What is lap band surgery
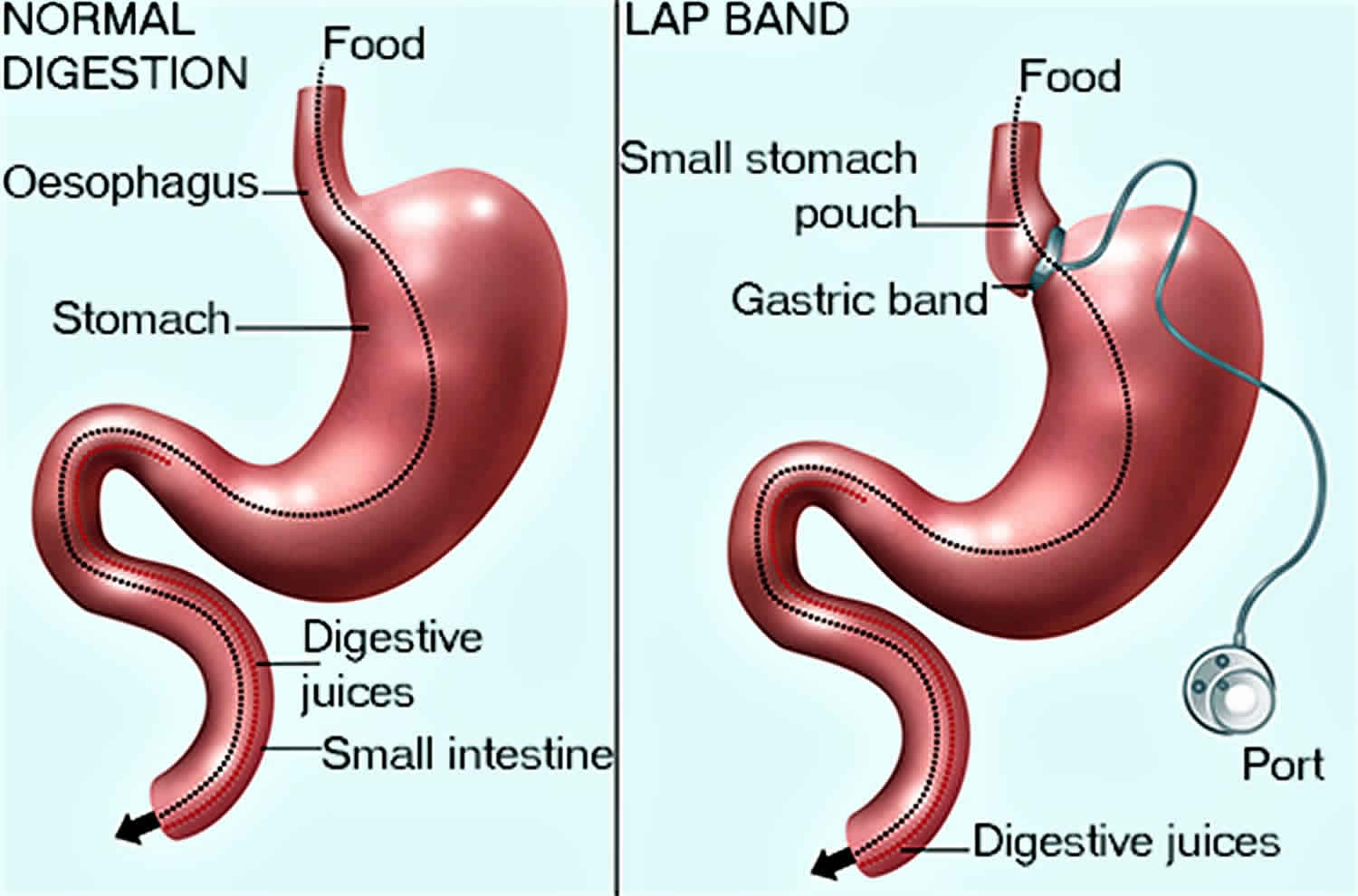
Lap band surgery is also called laparoscopic adjustable gastric banding, gastric banding or the LAP-BAND system, is used to help someone lose weight. Lap band surgery involves putting a ring called a “lap band” around the top part of your stomach. This creates a small stomach pouch above the band with a very narrow opening to the rest of the stomach. The ring slows the entry of food to the main part of your stomach and you’ll feel full after eating only a small amount of food, but it doesn’t reduce the absorption of calories and nutrients.
A lap band is a small inflatable balloon ring that contains salt water. The lap band can be made larger or smaller by the injection or removal of salt water.
A port is then placed under the skin of the abdomen. A tube connects the port to the band. By injecting or removing fluid through the port, the balloon can be inflated or deflated to adjust the size of the band.
Lap band surgery restricts the amount of food that your stomach can hold, so you feel full sooner. Lap band surgery is used for weight loss in severely obese adults who have been obese for at least five years and for whom non-surgical weight loss methods have not been successful. The patients must be willing to make major changes in their eating habits and lifestyle. Patients must have a Body Mass Index (BMI) of at least 40, a BMI of at least 35 with one or more severe morbid (unhealthy) conditions, or be at least 100 pounds over their estimated ideal weight. Updates to these criteria have included patients with a BMI of 30 to 35 with obesity-related comorbidities as an indication for laparoscopic adjusted gastric banding 1.
Lap band surgery has been shown to effectively cause weight loss in morbidly obese patients. The average patient will lose 87% of their excess weight after having the LAP-BAND System inserted. This should be compared to a person trying to lose weight by diet, exercise and medication therapy – where the average person will only lose 21% of their excess weight.
Large studies have shown that the average person will lose 23 kg following this surgery at 2 years, and up to 43 kg at 5 years post-operatively.
Losing weight after lap band surgery can help reduce problems with type 2 diabetes, asthma episodes and blood pressure, and can help improve heart health.
Lap band surgery has the lowest mortality of all the bariatric procedures, ranging from 0.02% to 0.1% 2. Lap band surgery carries a 3% 30 day morbidity 3 and a 12% rate of late complications, though this varies among the literature 4.
How does gastric banding work?
In a surgical procedure, the band is placed around the upper part of your stomach, creating a small pouch that can hold only a small amount of food. The narrowed opening between the stomach pouch and the rest of the stomach controls how quickly food passes from the pouch to the lower part of the stomach. The system helps the patient eat less by limiting the amount of food that can be eaten at one time and increasing the time it takes for food to be digested.
Depending on the patient’s needs, after the device is implanted the narrowed opening between the pouch and the lower part of the stomach can be adjusted in size by inflating or deflating the hollow band. Inflating the band makes the opening smaller, causing food to pass more slowly. Deflating the band makes it wider, causes food to pass more quickly. This adjustment is made by adding or removing fluid inside the hollow band. The doctor does this by injecting or removing the fluid through a small button-like part called the access port. This access port is placed under the skin in a muscle in the chest wall. The port is connected to the band by the tubing.
What are the benefits of lap band surgery?
The major benefit of the lap band surgery is weight loss. The operation to insert the LAP-BAND System is called gastric banding surgery. Lap band surgery is the simplest of all types of surgery performed for obesity. It is also considered the safest surgery for weight loss. In most cases, patients who have this surgery will only be in hospital for 24 hours.
Following the lap band surgery, a number of other medical problems will be improved in conjunction with weight loss. Studies of patients who have received gastric banding surgery show improvements in the following diseases after 2 years:
- Blood pressure
- Cholesterol
- Asthma
- Diabetes
- Gastro-esophageal reflux
- Heart failure
- Sleep apnoea
- Depression
- Infertility
- Blood clots
When should lap band surgery not be used?
Lap band surgery should not be used for people who are poor candidates for surgery, have certain stomach or intestinal disorders, have an infection, have to take aspirin frequently, or are addicted to alcohol or drugs. Lap band surgery should not be used on patients who are not able or willing to follow the rules for eating and exercise that are recommended by the doctor after surgery.
Lap band surgery contraindications
Lap band surgery is contraindicated for patients unable to tolerate general anesthesia. It is also contraindicated for those with uncontrollable coagulopathy or those at a prohibitive operative risk 5.
Relative contraindications include Prader-Willi syndrome, malignant hyperphagia, untreated severe psychiatric illness, pregnancy, cirrhotics with portal hypertension, autoimmune connective tissue disorders, chronic inflammatory conditions, and the need for chronic corticosteroid use 1.
Lap band surgery requirements or qualifications
Lap band weight-loss surgery may be an option if you are severely obese and have not been able to lose weight through diet and exercise.
The U.S. Food and Drug Administration (FDA) has approved use of the lap band surgery or gastric banding for people with a BMI of 30 or more who also have at least one health problem linked to obesity, such as heart disease or diabetes 6.
Lap band surgery is not a “quick fix” for obesity. Lap band surgery will greatly change your lifestyle. You must diet and exercise after this surgery. If you do not, you may have complications or poor weight loss.
People who have this lap band surgery should be mentally stable and not be dependent on alcohol or illegal drugs.
Doctors often use the following body mass index (BMI) measures to identify people who may be most likely to benefit from lap band weight-loss surgery. A normal BMI is between 18.5 and 25. Lap band weight-loss surgery procedure may be recommended for you if you have:
- A BMI of 40 or more. This most often means that men are 100 pounds (45 kg) overweight and women are 80 pounds (36 kg) over their ideal weight.
- A BMI of 35 or more and a serious medical condition that might improve with weight loss. Some of these conditions are sleep apnea, high cholesterol, heart attacks or stroke, type 2 diabetes, high blood pressure, heart disease, depression, and osteoarthritis.
The following are some of the main criteria are used to assess if the lap band surgery is appropriate:
- Have been very overweight for at least 5 years.
- Multiple, previous attempts to lose weight.
- Motivation to lose weight.
- Willingness to change current exercise and eating patterns.
- Understanding of what the surgery involves. (See page on laparoscopic surgery).
- Able to attend regular follow-up appointments.
Before the lap band surgery procedure
Your surgeon will ask you to have tests and visits with your other health care providers before you have lap band surgery. Some of these are:
- Blood tests and other tests to make sure you are healthy enough to have surgery.
- Classes to help you learn what happens during the surgery, what you should expect afterward, and what risks or problems may occur.
- Complete physical exam.
- Nutritional counseling.
- Visit with a mental health provider to make sure you are emotionally ready for major surgery. You must be able to make major changes in your lifestyle after surgery.
- Visits with your provider to make sure other medical problems you may have, such as diabetes, high blood pressure, and heart or lung problems, are under control.
If you are a smoker, you should stop smoking several weeks before surgery and not start smoking again after surgery. Smoking slows recovery and increases the risk of problems. Tell your provider if you need help quitting.
Always tell your doctor:
- If you are or might be pregnant
- What medicines, vitamins, herbs, and other supplements you are taking, even ones you bought without a prescription
During the week before your lap band surgery:
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), and any other medicines that make it hard for your blood to clot.
- Ask which medicines to take on the day of your surgery.
On the day of your lap band surgery:
- DO NOT eat or drink anything for 6 hours before your surgery.
- Take the medicines your doctor told you to take with a small sip of water.
Your doctor will tell you when to arrive at the hospital.
Lap band surgery procedure
You will receive general anesthesia before your lap band surgery. You will be asleep and unable to feel pain.
The lap band surgery is done using a tiny camera that is placed in your belly. This type of surgery is called laparoscopy. The camera is called a laparoscope. It allows your surgeon to see inside your belly. In this surgery:
- Your surgeon will make 1 to 5 small surgical cuts in your abdomen. Through these small cuts, the surgeon will place a camera and the instruments needed to perform the surgery.
- Your surgeon will place a band around the upper part of your stomach to separate it from the lower part. This creates a small pouch that has a narrow opening that goes into the larger, lower part of your stomach.
- The surgery does not involve any cutting or stapling inside your belly.
- Your surgery may take only 30 to 60 minutes if your surgeon has done a lot of these procedures.
When you eat after having lap band surgery, the small pouch will fill up quickly. You will feel full after eating just a small amount of food. The food in the small upper pouch will slowly empty into the main part of your stomach.
Lap band surgery recovery
You will probably go home the day of lap band surgery. Many people are able to begin their normal activities 1 or 2 days after going home. Most people take 1 week off from work.
You will stay on liquids or mashed-up foods for 2 or 3 weeks after your lap band surgery. You will slowly add soft foods, then regular foods, to your diet. By 6 weeks after lap band surgery, you will probably be able to eat regular foods.
The band is made of a special rubber (silastic rubber). The inside of the band has an inflatable balloon. This allows the band to be adjusted. You and your doctor can decide to loosen or tighten it in the future so you can eat more or less food.
The band is connected to an access port that is under the skin on your belly. The band can be tightened by placing a needle into the port and filling the balloon (band) with water.
Your surgeon can make the band tighter or looser any time after you have this surgery. It may be tightened or loosened if you are:
- Having problems eating
- Not losing enough weight
- Vomiting after you eat
Lap band surgery recovery at home
You may lose weight quickly over the first 3 to 6 months. During this time, you may have:
- Body aches
- Feel tired and cold
- Dry skin
- Mood changes
- Hair loss or hair thinning
These problems should go away as your body gets used to your weight loss and your weight becomes stable. Weight loss may be slower after this.
Wound care
Keep your dressings (bandage) on your wounds clean and dry. If you have sutures (stitches) or staples, they will be removed about 7 to 10 days after surgery. Some stitches can dissolve on their own. Your provider will tell if you have this kind.
Change the dressings (bandages) every day if you were told to do so. Be sure to change them more often if they get dirty or wet.
You may have bruising around your wound. This is normal. It will go away on its own. The skin around your incisions may be a little red. This is normal, too.
DO NOT wear tight clothing that rubs against your incisions while they heal.
Unless you are told otherwise, DO NOT shower until after your follow-up appointment with your provider. When you can shower, let water run over your incision, but DO NOT scrub it or let the water beat down on it.
DO NOT soak in a bathtub, swimming pool, or hot tub until your doctor tells you it is OK.
Activity
Being active soon after surgery will help you recover more quickly. During the first week:
Take short walks and going up and down stairs.
Try getting up and moving around if you are having some pain in your belly. It may help the pain.
If it hurts when you do something, stop doing that activity.
If you have laparoscopic surgery, you should be able to do most of your regular activities in 2 to 4 weeks.
Lap band surgery diet
Laparoscopic gastric banding made your stomach smaller by closing off part of your stomach with an adjustable band. After surgery you will eat less food, and you will not be able to eat quickly.
Your health care provider will teach you about foods you can eat and foods you should avoid. It is very important to follow these diet guidelines.
You will eat only liquid or puréed food for 2 to 3 weeks after your lap band surgery. You will slowly add in soft foods, and then regular foods.
A dietitian will advise you on how to change your eating habits to keep healthy while losing weight after lap band surgery.
You’ll need to visit your doctor to have the band adjusted, possibly several times, to the size that works for you for both weight loss and how you feel. You don’t need any anesthesia for the adjustment.
Follow-up care
By the time you leave the hospital, you will likely have a follow-up appointment scheduled with your surgeon within a few weeks. You will see your surgeon several more times in the first year after your surgery.
You may also have appointments with:
- A nutritionist or dietitian, who will teach you how to eat correctly with your smaller stomach. You will also learn about what foods and drinks you should have after surgery.
- A psychologist, who can help you follow your eating and exercise guidelines and deal with the feelings or concerns you may have after surgery.
The band around your stomach is filled with saline (saltwater). It is connected to a container (access port) that is placed under your skin in your upper belly. Your surgeon can make the band tighter or looser by increasing or decreasing the amount of saline in the band. To do this, your surgeon will insert a needle through your skin into the access port.
Your surgeon can make the band tighter or looser any time after you have this surgery. It may be tightened or loosened if you are:
- Not losing enough weight
- Having problems eating
- Vomiting after you eat
Lap band surgery risks
Lap band surgery is a very safe procedure. Sometimes infection or bleeding occurs at the wound. Very rarely, the ring can slip out of place or damage your stomach.
Risks for anesthesia and any surgery includes:
- Allergic reactions to medicines
- Breathing problems
- Blood clots in the legs that may travel to your lungs
- Blood loss
- Infection, including in the surgery site, lungs (pneumonia), or bladder or kidney
- Heart attack or stroke during or after surgery
Risks for lap band surgery are:
- Gastric band erodes through the stomach (if this happens, it must be removed).
- Stomach may slip up through the band. (If this happens, you may need urgent surgery.)
- Gastritis (inflamed stomach lining), heartburn, or stomach ulcers.
- Infection in the port, which may need antibiotics or surgery.
- Injury to your stomach, intestines, or other organs during surgery.
- Poor nutrition.
- Scarring inside your belly, which could lead to a blockage in your bowel.
- Your surgeon may not be able to reach the access port to tighten or loosen the band. You would need minor surgery to fix this problem.
- The access port may flip upside down, making it impossible to access. You would need minor surgery to fix this problem.
- The tubing near the access port can be accidentally punctured during a needle access. If this happens, the band cannot be tightened. You would need minor surgery to fix this problem.
- Vomiting from eating more than your stomach pouch can hold.
Call your doctor if:
- Your temperature is above 101°F (38.3°C).
- Your incisions are bleeding, red, warm to the touch, or have a thick, yellow, green, or milky drainage.
- You have pain that your pain medicine is not helping.
- You have trouble breathing.
- You have a cough that does not go away.
- You cannot drink or eat.
- Your skin or the white part of your eyes turns yellow.
- Your stools are loose, or you have diarrhea.
- You are vomiting after eating.
Lap band surgery side effects
Most patients experienced at least one side effect after lap band surgery. Common lap band surgery side effects include nausea and vomiting, heartburn, abdominal pain, and slippage of the band. The most serious side effects required either another operation or hospitalization.
Early complications include:
- Deep vein thrombosis (DVT): Pulmonary embolism is the leading cause of death following laparoscopic adjusted gastric band surgery in many series 7. These patients should receive appropriate venous thromboembolism prophylaxis.
- Esophageal or gastric perforation: The most common location for this is the retrogastric space. It is usually associated with an undiagnosed hiatal hernia. If a perforation occurs and is in close proximity to where the band will be placed, the procedure should be aborted.
- Esophagogastric obstruction: This can be an immediate postoperative obstruction caused by a tight gastric band. It is not typically seen due to the larger diameter of later band designs. This can be prevented by removing the perigastric fat pads to allow for adequate room for the gastric band 8.
Late complications include:
- Gastric prolapse, or a “slipped band”: This is characterized by the lower stomach herniating superiorly through the device. It can be classified as an anterior or posterior slippage of the fundus past the band; anterior is more common. The patient will experience sudden-onset food intolerance or reflux symptoms. Diagnosis begins with a plain abdominal radiograph. Normally the band is oriented diagonally from 2 to 8 o’clock and points towards the left shoulder. A slipped band will appear oriented more horizontally from a 10 to 4 o’ clock position and will point towards the left hip. Confirmation is generally done with an esophagram. Treatment should be initial deflation of the band to temporarily alleviate the patient’s symptoms. Definitive management includes a reoperation and one of the following techniques: laparoscopic band repositioning, removal with or without replacement of the band, and conversion to another bariatric procedure such as a sleeve gastrectomy or Roux-en-Y gastric bypass 9. Rarely, gastric ischemia and necrosis may ensue. Gastric prolapse had a much higher prevalence in the 1990s secondary to the laparoscopic adjusted gastric band procedure being done with the perigastric technique. This procedure involved a retro-gastric tunnel that entered the lesser sac, resulting in much more freedom and movement of the stomach. This freedom of movement allowed for posterior fundal herniation through the band. With the advent of the pars flaccida technique, the rate of prolapse has decreased from 15% to 4% 10.
- Band erosion: Incidence of band erosion into the stomach wall increases with time but remains between 1% and 2% in the literature 11. These are typically manifested by delayed port site infections, abdominal pain, or failure to suppress the appetite despite band adjustment. The diagnosis is confirmed with endoscopy. Treatment involves an operation, removal of the band, repair of the gastric wall, and drainage. Delayed replacement of the gastric band should be done in three months.
- Device malfunctions: These can be characterized by a variety of complications including device leak leading to failure of band adjustment, tube kinking, port dislodgment, and port site infection. Leaks can occur via tubing disconnection, port puncture, or band puncture. The port may become dislodged from the fascia and flip, rendering the port inaccessible.
- Band obstruction: This can be secondary to an overinflated band, which is most common, or a low placement of the band due to technical errors or a missed hiatal hernia. This will lead to the gastric pouch and esophageal dilation with esophagitis that can result in esophageal dysmotility, such as megaesophagus or pseudo-achalasia, in chronic cases 12. Diagnosis is with an esophagram demonstrating esophageal and gastric pouch dilation. Treatment is the deflation of the band and imaging to monitor for the resolution of the gastroesophageal dilatation. If conservative management fails, an operation to revise or remove the band is required 13.
Lap band surgery results
The final weight loss with gastric banding is not as large as with other weight loss surgery. The average weight loss is about one-third to one-half of the extra weight you are carrying. This may be enough for many people. Talk with your surgeon about which procedure is best for you.
In most cases, the weight will come off more slowly than with other weight loss surgery. You should keep losing weight for up to 3 years.
In the U.S. study, the average weight loss was 36% of a patient’s excess weight three years after the device was implanted. More than half of the patients lost at least 25% of their excess weight; some patients lost over 75%, but some lost no weight 14. Many publications demonstrate a low risk of reoperation and band removal, ranging from 1.2% to 3.7%, when evaluating long-term data for laparoscopic adjusted gastric banding 15. These results may be attributed to surgeon experience and advances in techniques that limit complications. However, other studies showed extremely high long-term reoperation rates requiring gastric band removal, ranging from 8% to 60% 16.
Losing enough weight after lap band surgery can improve many medical conditions you might also have, such as:
- Asthma
- Gastroesophageal reflux disease (GERD)
- High blood pressure
- High cholesterol
- Sleep apnea
- Type 2 diabetes
Weighing less should also make it much easier for you to move around and do your everyday activities.
This surgery alone is not a solution to losing weight. It can train you to eat less, but you still have to do much of the work. To lose weight and avoid complications from the procedure, you will need to follow the exercise and eating guidelines that your provider and dietitian gave you.
References- Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM, Heinberg LJ, Kushner R, Adams TD, Shikora S, Dixon JB, Brethauer S., American Association of Clinical Endocrinologists. Obesity Society. American Society for Metabolic & Bariatric Surgery. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013 Mar;21 Suppl 1:S1-27.
- Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Flum DR, Belle SH, King WC, Wahed AS, Berk P, Chapman W, Pories W, Courcoulas A, McCloskey C, Mitchell J, Patterson E, Pomp A, Staten MA, Yanovski SZ, Thirlby R, Wolfe B. Perioperative safety in the longitudinal assessment of bariatric surgery. N. Engl. J. Med. 2009 Jul 30;361(5):445-54.
- Nguyen NT, Hohmann S, Nguyen XM, Elliott C, Masoomi H. Outcome of laparoscopic adjustable gastric banding and prevalence of band revision and explantation at academic centers: 2007-2009. Surg Obes Relat Dis. 2012 Nov-Dec;8(6):724-7
- Carelli AM, Youn HA, Kurian MS, Ren CJ, Fielding GA. Safety of the laparoscopic adjustable gastric band: 7-year data from a U.S. center of excellence. Surg Endosc. 2010 Aug;24(8):1819-23
- Seeras K, Prakash S. Laparoscopic Lap Band Placement. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526062
- Obesity Treatment Devices. https://www.fda.gov/medicaldevices/productsandmedicalprocedures/obesitydevices/default.htm
- Gagner M, Milone L, Yung E, Broseus A, Gumbs AA. Causes of early mortality after laparoscopic adjustable gastric banding. J. Am. Coll. Surg. 2008 Apr;206(4):664-9.
- Shen R, Ren CJ. Removal of peri-gastric fat prevents acute obstruction after Lap-Band surgery. Obes Surg. 2004 Feb;14(2):224-9.
- Weiner R, Blanco-Engert R, Weiner S, Matkowitz R, Schaefer L, Pomhoff I. Outcome after laparoscopic adjustable gastric banding – 8 years experience. Obes Surg. 2003 Jun;13(3):427-34
- Di Lorenzo N, Furbetta F, Favretti F, Segato G, De Luca M, Micheletto G, Zappa M, De Meis P, Lattuada E, Paganelli M, Lucchese M, Basso N, Capizzi FD, Di Cosmo L, Mancuso V, Civitelli S, Gardinazzi A, Giardiello C, Veneziani A, Boni M, Borrelli V, Schettino A, Forestieri P, Pilone V, Camperchioli I, Lorenzo M. Laparoscopic adjustable gastric banding via pars flaccida versus perigastric positioning: technique, complications, and results in 2,549 patients. Surg Endosc. 2010 Jul;24(7):1519-23
- Egberts K, Brown WA, O’Brien PE. Systematic review of erosion after laparoscopic adjustable gastric banding. Obes Surg. 2011 Aug;21(8):1272-9.
- Khan A, Ren-Fielding C, Traube M. Potentially reversible pseudoachalasia after laparoscopic adjustable gastric banding. J. Clin. Gastroenterol. 2011 Oct;45(9):775-9.
- Arias IE, Radulescu M, Stiegeler R, Singh JP, Martinez P, Ramirez A, Szomstein S, Rosenthal RJ. Diagnosis and treatment of megaesophagus after adjustable gastric banding for morbid obesity. Surg Obes Relat Dis. 2009 Mar-Apr;5(2):156-9.
- LAP-BAND® Adjustable Gastric Banding (LAGB®) System – P000008. http://wayback.archive-it.org/7993/20170112093341/http:/www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DeviceApprovalsandClearances/Recently-ApprovedDevices/ucm088965.htm
- Giet L, Baker J, Favretti F, Segato G, Super P, Singhal R, Ashton D. Medium and long-term results of gastric banding: outcomes from a large private clinic in UK. BMC Obes. 2018;5:12.
- Carandina S, Tabbara M, Galiay L, Polliand C, Azoulay D, Barrat C, Lazzati A. Long-Term Outcomes of the Laparoscopic Adjustable Gastric Banding: Weight Loss and Removal Rate. A Single Center Experience on 301 Patients with a Minimum Follow-Up of 10 years. Obes Surg. 2017 Apr;27(4):889-895