What is leukemoid reaction
Leukemoid reaction is defined as a reactive, excessive leukocytosis with white blood cell counts exceeding 50,000/mm³ outside the bone marrow in the absence of hematological malignancy 1. There is a significant increase in mature neutrophils in the peripheral blood and a differential count showing neutrophilia with varying degree immature lineage of myeloid cells. The underlying mechanism for leukemoid reaction is attributed to increased cytokines and interleukins production 2. Leukemoid reaction is an inflammatory reaction that may be mistaken for leukemia, especially chronic myeloid leukemia (CML). Due to increased count of more immature lineage of myeloid cells in the blood the peripheral blood finding shows shift to the left. Differential of leukemoid reaction is chronic myelogenous leukemia (CML) and chronic neutrophil leukemia.
Differentiating leukemoid reaction from leukemia
- In the leukemoid reaction, the neutrophils are mature and not clonally derived.
- There is a persistent increase in total leucocyte (white blood cell) count above 50,000/mm³ and no evidence of leukemia.
- Blood count comes to normal after treating the cause.
- Increased blast cells are not seen in the leukemoid reaction.
- A count above 100,000/mm³ is more suggestive of the myeloproliferative disorder with very few exceptions.
The major causes of leukemoid reaction are severe infections, intoxications, malignancies, severe hemorrhage or acute hemolysis 3.
Leukemoid reaction has been described in response to inflammation, severe infection, malignancies, hemorrhage, acute hemolysis, or bone marrow stimulants 4. Leukemoid reaction may also be a paraneoplastic manifestation of various malignant tumors 5. Tumor-related leukemoid reaction is a kind of neoplastic syndrome, unrelated to an infection or other diseases. White blood cell counts often return to normal when the underlying condition is treated.
Leukemoid reaction vs CML
CML is short for chronic myelogenous leukemia or chronic myeloid leukemia, is a type of blood cancer or leukemia, that starts from cells in the bone marrow that are supposed to grow into different types of blood cells. Most of the time CML grows slowly, but over time the leukemia cells can spill out into the blood and spread to other parts of the body, like the spleen.
Table 1. Difference between leukemoid reaction and CML (chronic myeloid leukemia)
| Test | Leukemoid reaction | Chronic myeloid leukemia (CML) |
| WBC count | usually <50,000/mm³ | usually >50,000/mm³ |
| Basophils | absent | usually increased count |
| platelets | normal | Increased |
| Eosinophil | normal | Increased |
| Hemoglobin | usually normal | usually low |
| Band form | these are prominent | all stages (myelocytes) |
| Toxic granules and Dohle bodies | these are present | toxic granules ± to 0 |
| Spleen | usually not present | usually enlarged |
| Philadelphia chromosome | absent | present in 90% of the cases |
| Leukocyte Alkaline Phosphatase (LAP) score | > 100 | < 10 |
| History | short | long |
Many people with CML don’t have any symptoms. The leukemia is found when blood tests are done for some other health problem or during a routine check-up. Even when there are symptoms, they may be very general and unclear.
Some signs of CML include feeling tired or weak, losing weight, having a fever, or sweating a lot at night. The doctor will ask you questions about your health and do a physical exam.
If signs are pointing to CML, more tests will be done. Here are some of the tests you may have:
Tests for CML
- Blood cell counts: This blood test is often the first test done. Most people with CML have too many white blood cells with many early (not mature) cells, called blasts. Sometimes people with CML have low numbers of other types of blood cells. Even though these results may point to leukemia, most of the time you’ll need other blood tests or a test of the bone marrow to make sure.
- Bone marrow aspiration and biopsy: For these tests, a doctor uses thin, hollow needles to take out small amounts of bone marrow, usually from the back of your hip bone. The area around the bone is numbed, and you may be given a drug to make you sleepy during the test. The samples are sent to a lab to see if there are leukemia cells in the bone marrow. These tests may also be done after treatment to see if the treatment is working.
- Gene tests: If you might have CML, tests will be done on samples of your blood and/or bone marrow to look for certain gene changes in the cells. CML cells nearly always have certain changes.
- Other blood tests: If you have leukemia, other blood tests will be done to see how well your liver, kidneys, and other body parts are working.
- Imaging tests: These tests take pictures of the inside of your body. There are many kinds of imaging tests, like CT and MRI scans. They’re sometimes done to see if the leukemia has spread to other parts of your body, like the spleen or liver. Ask your doctor what imaging tests you may need.
The kind of treatment you will need depends on the phase of your CML, your age and how healthy you are, and whether a stem cell donor can be found.
The most common kinds of treatment for CML are:
- Targeted drugs
- Interferon
- Chemotherapy
- Stem cell transplant
Targeted drugs
The main treatment for CML is drugs that go after proteins in the leukemia cells that aren’t normal. These drugs mainly affect cancer cells and not normal cells. They’re pills you take every day. Most of the time, targeted drugs are very good at treating CML. If one targeted drug doesn’t work, others may be tried. These drugs can have side effects, but they’re often not the same as those of chemo drugs. Ask your doctor which drug you will have and what to expect.
Interferon
Interferons are made by immune system cells in the body. Man-made types of interferon drugs attack the leukemia and slow its growth. They’re given as a shot under the skin. Interferon might be tried if targeted drugs don’t work or you can’t take them. Side effects can include flu-like symptoms, feeling very tired, fever, and weight loss. Ask your doctor what to expect.
Chemotherapy
Chemotherapy or chemo, is the use of drugs to fight cancer. Most of the time chemo drugs are given into a vein or taken as pills. These drugs go into the blood and spread through the body. In CML, chemo is not usually used unless other treatments are no longer working. Chemo is given in cycles or rounds. Each round of treatment is followed by a rest break. Treatment often lasts for many months.
Chemotherapy can have many side effects like:
- Hair loss
- Mouth sores
- Not feeling like eating
- Diarrhea
- Being sick to your stomach and throwing up
- More risk of infections
- Black and blue marks and bleeding easily
- Tiredness
But these problems tend to go away after treatment ends. There are ways to treat most chemo side effects. Be sure to talk to your cancer care team so they can help.
Stem cell transplant
A stem cell transplant also called bone marrow transplant, lets doctors use very high doses of chemotherapy drug to kill the leukemia cells. The high doses destroy the bone marrow, which means new blood cells can’t be made. Although the drugs destroy the bone marrow, the stem cells given after chemo bring back the blood-making bone marrow stem cells. You may get an stem cell transplant if you haven’t been helped by other treatments. There are different kinds of stem cell transplant, each of which can have bad side effects. Ask your doctor which type you will have and what to expect.
Leukemoid reaction causes
The major causes of leukemoid reaction are severe infections, intoxications, malignancies, severe hemorrhage or acute hemolysis 3.
Infections
- Septicemia
- Brucellosis
- Shigellosis
- Salmonellosis
- Clostridium difficile colitis
- Cryptogenic abscess
- Miliary or acute necrotizing tuberculosis
- Disseminated candidiasis, cryptococcosis
Malignancies
- Carcinomas (lung, oropharyngeal, gastrointestinal, genitourinary)
- Hodgkin’s lymphoma
- Melanoma, Sarcoma
Drugs
- Corticosteroids
- Minocycline
- Recombinant hematopoietic growth factors
Leukemoid reaction is most often caused by serious infection 6, but can also be a paraneoplastic manifestation of several cancers, including lung, gastrointestinal, genitourinary, ovarian, and head and neck cancers, and hepatocellular carcinoma 7. Hughes and Charles 8 first reported a case of leukemoid reaction resulting from a carcinoma of the suprarenal gland in 1952. Since then, great efforts have been made to elucidate the mechanism of leukemoid reaction. Paraneoplastic syndromes, such as tumor fever and leukemoid reaction, have been described in literature 9. However, studies on the incidence and course of leukemoid reaction in solid tumors are scarce 10. One study reported that the occurrence of leukemoid reaction in solid tumors is approximately 1–4% 11. However, owing to few accounts in medical literature, the causes of this occurrence are not well understood.
Leukemoid reaction symptoms
Leukemoid reaction is defined as a reactive, excessive leukocytosis with white blood cell counts exceeding 50,000/mm³ outside the bone marrow in the absence of hematological malignancy 1. Symptoms depend entirely of the underlying cause of the leukemoid reaction. The only way to truly determine if your white blood cells are too high is to get your blood tested. People with high (above normal) white blood cell count, a condition called leukocytosis, typically don’t have any specific symptoms, but may have a medical condition that is responsible for raising white blood cell levels. The specific number for high (above normal) white blood cell count varies from one lab testing facility to another, but a general rule of thumb is that a count of more than 10,500 leukocytes in a microliter of blood in adults is generally considered to be high, while 4,500-10,500 is considered within the normal range. If there is a persistent increase in the neutrophils with a count of 30,000 to 50,000/mm³, with the presence of immature and mature white cells is called leukemoid reaction. Since a high (above normal) white blood cell count can be a symptom of another underlying problem, you might experience symptoms that are associated with that condition. However, people with leukocytosis may also experience a combination of these symptoms: fever, fainting, bleeding, bruising, weight loss, and general pain.
Leukemoid reaction diagnosis
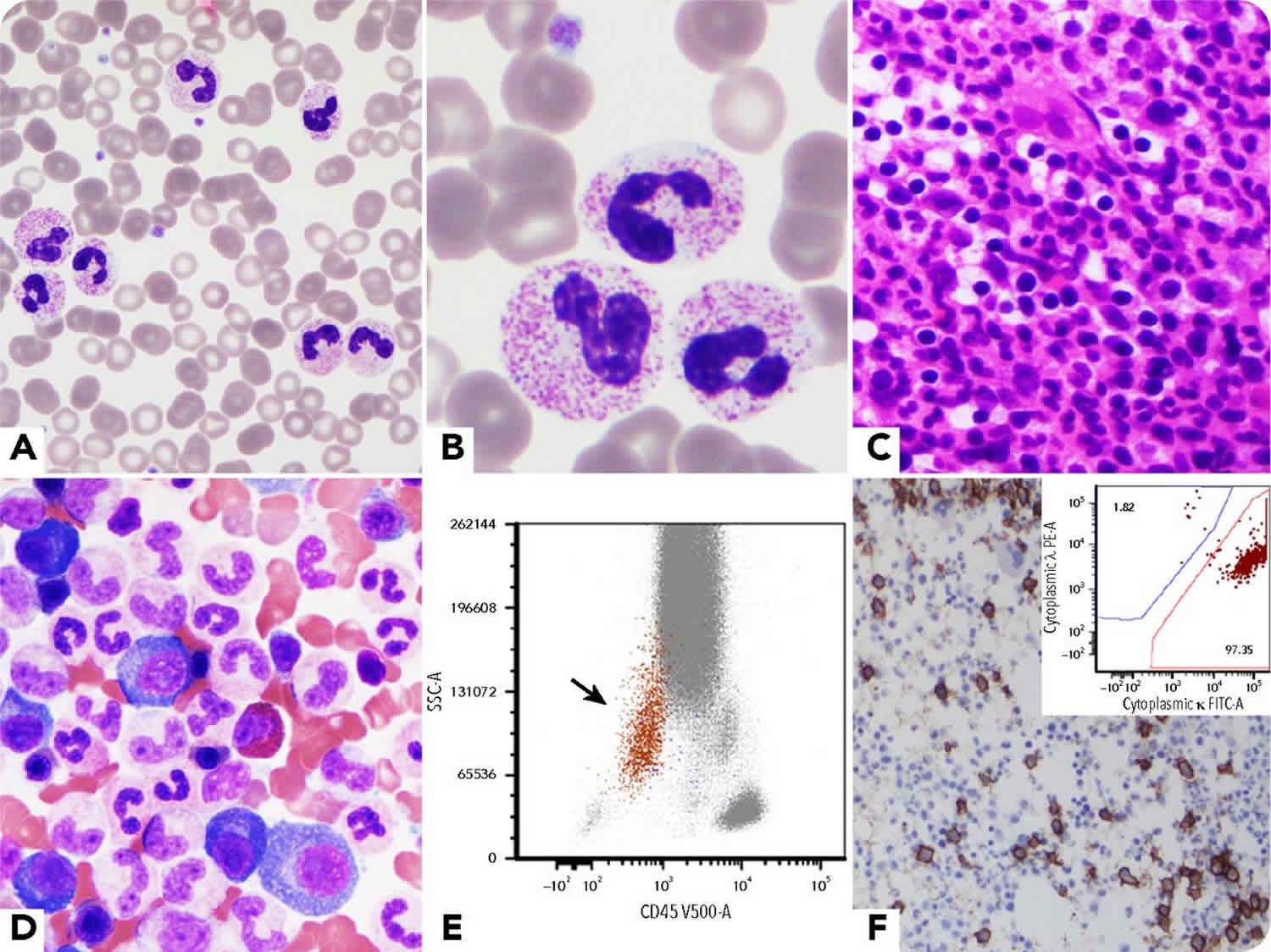
For establishing the diagnosis detailed history including exposure to toxins or drugs, laboratory investigation as total and differential blood counts, peripheral smear, leukocyte alkaline phosphatase (LAP) score, bone marrow examination can determine the underlying cause, there are cases where the clinician may not be able to exclude other significant causes of a leukemoid reaction without specific testing required for exclusion 12.
These include cytogenetic testing of chromosome 20 abnormalities seen in some cases of chronic neutrophil leukemia and molecular analysis of bcr –abl gene with t 9:22 translocation in CML. Immuno-phenotyping is useful in detecting surface antigens like CD13 and CD15 which are found in mature neutrophils in leukemoid reaction and CD34 in acute leukemia or myelodysplastic syndromes. It may also rule out CML in blast crisis by the presence of HLA-DR. Clonality studies demonstrate monoclonal cells in myeloproliferative syndromes and polyclonal neutrophils in leukemoid reaction 13. Imaging studies and biopsies
are useful when solid tumors are suspected.
In leukemoid reaction the differential count shows leukocyte consist mostly of mature neutrophils. Along with left shift, with the presence of myelocytes and metamyelocytes. In addition the smear shows Doëhle bodies, toxic granulation and cytoplasmic vacuoles in the neutrophils and absence of basophils, with increase or normal leukocyte alkaline phosphatase (LAP) score in leukemoid reaction so review of the peripheral smear can be helpful for differentiating between leukemoid reaction and CML in which there are more immature cells, basophils, and eosinophils are seen.
In chronic neutrophil leukemia, there is marked neutrophilia with no immature cells and, in contrast to an leukemoid reaction, myelocytes, metamyelocytes, and nucleated red cells are not seen. The peripheral smear in addition shows Doëhle bodies, toxic granulation and cytoplasmic vacuoles in the neutrophils and absence of basophils, with increase or normal LAP score in leukemoid reaction.
Serum levels of hematopoietic growth factors in leukemoid reaction due to GM-CSF-producing tumor is characterized by marked eosinophilia 14. CML and chronic neutrophil leukemia patients have significantly low G-CSF levels, suggesting that the neoplastic granulopoiesis can exert a suppressor effect on G-CSF synthesis 15. Searching for an underlying infection includes taking cultures of blood, sputum and bone marrow. Stool cultures should not be overlooked since colitis due to Shigella spp. or Clostridium difficile is one of the classic examples of an infection-associated leukemoid reaction.
Thus leukemoid reaction is a rare but challenging condition that may require a careful diagnostic work-up made by a combination of high leucocyte count, marked mature neutrophilia with a left shift, high LAP score. Rarely, it may require higher investigation as an absence of cytogenetic abnormalities, mature granulocyte pattern by immunophenotyping and polyclonal neutrophils the absence of high levels of hemopoietic growth factors. With all these findings there must be pathologist mind to make the differential and lead the physician tom exact diagnosis 12.
Leukemoid reaction treatment
Leukemoid reaction involves treating the cause of the leukemoid reaction.
References- Paraneoplastic leukemoid reaction in solid tumors. Chakraborty S, Keenportz B, Woodward S, Anderson J, Colan D. Am J Clin Oncol. 2015 Jun; 38(3):326-30.
- Pahadiya HR, Lakhotia M, Choudhary A, Choudhary S. (2017) Leukemoid reaction in megaloblastic anemia of the puerperium: An unusual cause. J Family Med Prim Care 6(3): 698-699.
- Aylin Canbolat Ayhan, Cetin Timur, Seyma Sonmez, Ebru Zemheri, Asım Yoruk (2014) Myeloid Sarcoma Presenting with Leukemoid Reaction in a Child Treated for Acute Lymphoblastic Leukemia Case Reports in Hematology 1-5.
- Pathol, Clin & Gn, Gupta & Sareen, Rateesh & Kapil, Menka. (2019). Clinical Pathology & Research Journal Leukemoid Reaction-An Update Leukemoid Reaction-An Update. 3.
- Yu G, Ji H, Meng C, et al. Esophageal adenocarcinoma with leukemoid reaction: a case report. J Cardiothorac Surg. 2019;14(1):66. Published 2019 Apr 8. doi:10.1186/s13019-019-0893-z https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6454710
- Next-generation sequencing discriminates myelodysplastic/myeloproliferative neoplasms from paraneoplastic leukemoid reaction in cancer patients with hyperleukocytosis. Sakr R, Renneville A, Saada V, Cotteret S, Martin JE, Droin N, Selimoglu-Buet D, Besse B, Hollebecque A, Marzac C, Pasquier F, Micol JB, De Botton S, Mir O, Solary E, Willekens C. Leuk Lymphoma. 2018 Jul; 59(7):1742-1745.
- Hepatocellular carcinoma manifesting as cavitary lung metastases and leukemoid reaction. Jain P, Roop Rai R, Jha A. J Gastrointestin Liver Dis. 2008 Sep; 17(3):355-6.
- Marked leukocytosis resulting from carcinomatosis. HUGHES WF, HIGLEY CS. Ann Intern Med. 1952 Nov; 37(5):1085-8.
- Leukemoid reaction associated with pediatric nasopharyngeal carcinoma: An unusual presentation. Kuş AB, Şahin P, Uğuz AH, Tanyeli A, Küpeli S. Int J Pediatr Otorhinolaryngol. 2014 May; 78(5):885-7.
- Extreme leucocytosis: not always leukaemia. Halkes CJ, Dijstelbloem HM, Eelkman Rooda SJ, Kramer MH. Neth J Med. 2007 Jul-Aug; 65(7):248-51.
- Rapid onset lung squamous cell carcinoma with prominent peritoneal carcinomatosis and an eosinophilic leukemoid reaction, with coexistence of the BRAF V600E and oncogenic KRAS G12A mutations: A case report. Li B, Lu JC, He D, Wang J, Zhou H, Shen L, Zhang C, Duan C. Oncol Lett. 2014 Aug; 8(2):589-593.
- Pathol, Clin & Gn, Gupta & Sareen, Rateesh & Kapil, Menka. (2019). Clinical Pathology & Research Journal Leukemoid Reaction-An Update Leukemoid Reaction-An Update. 3.
- Bohm J, Kock S, Schaefer HE, Fisch P (2003) Evidence of clonality in chronic neutrophilic leukaemia. J Clin Pathol 56(4): 292-295.
- Watanabe M, Ono K, Ozeki Y, Tanaka S, Aida S, et al. (1998) Production of granulocyte-macrophage colony-stimulating factor in a patient with metastatic chest wall large cell carcinoma. Jpn J Clin Oncol 28(9): 559-562.
- Endo K, Kohnoe S, Okamura T, Haraguchi M, Adachi E, et al. (2005) Gastric adenosquamous carcinoma producing granulocyte-colony stimulating factor. Gastric Cancer 8(3): 173-177.