Liddle syndrome
Liddle syndrome is a rare inherited form of resistant high blood pressure (resistant hypertension). Resistant hypertension is a condition in which blood pressure continues to be greater than 140/90 mm Hg despite compliance with a regimen of 3 antihypertensive agents including a diuretic 1. Liddle syndrome is characterized by resistant hypertension that begins unusually early in life, often in childhood, although some affected individuals are not diagnosed until adulthood. Some people with Liddle syndrome have no additional signs or symptoms, especially in childhood. Over time, however, untreated hypertension can lead to heart disease or stroke, which may be fatal.
In addition to hypertension, affected individuals can have low levels of potassium in the blood (hypokalemia). Signs and symptoms of hypokalemia include muscle weakness or pain, fatigue, constipation, or heart palpitations. The shortage of potassium can also raise the pH of the blood, a condition known as metabolic alkalosis.
Liddle syndrome is a rare condition, although its prevalence is unknown. Liddle syndrome has been found in populations worldwide. Lin-Ping Wang et al. 2 and Liu and his team 3 studied the prevalence of Liddle syndrome. According to them, it was 0.92% to 1.52% in the Chinese population. In these studies, the study population was a group of hypokalemic patients, but Liddle syndrome can be seen in patients with normal potassium levels. Therefore, if researchers studied the incidence of Lidle syndrome in normal potassium patients with hypertension, it would likely be much higher 4. There is no gender or race predisposition.
Researchers of one study of US veterans concluded that there was approximately a 6% prevalence of symptomatic Liddle syndrome 5.
Liddle syndrome is caused by mutations in either the SCNN1B or SCNN1G genes and is inherited in an autosomal dominant manner. Treatment may include a low sodium diet and potassium-sparing diuretics to reduce blood pressure and normalize potassium levels. Conventional anti-hypertensive therapies are not effective 6.
Liddle syndrome causes
Liddle syndrome is caused by mutations in the SCNN1B or SCNN1G gene. Each of these genes provides instructions for making a piece (subunit) of a protein complex called the epithelial sodium channel (ENaC). These channels are found at the surface of certain cells called epithelial cells in many tissues of the body, including the kidneys, where the channels transport sodium into cells.
In the kidney, epithelial sodium channels open in response to signals that sodium levels in the blood are too low, which allows sodium to flow into cells. From the kidney cells, this sodium is returned to the bloodstream (a process called reabsorption) rather than being removed from the body in urine.
Mutations in the SCNN1B or SCNN1G gene change the structure of the respective epithelial sodium channel subunit. The changes alter a region of the subunit that is involved in signaling for its breakdown (degradation) when it is no longer needed. As a result of the mutations, the subunit proteins are not degraded, and more epithelial sodium channels remain at the cell surface. The increase in channels at the cell surface abnormally increases the reabsorption of sodium (followed by water), which leads to hypertension. Reabsorption of sodium into the blood is linked with removal of potassium from the blood, so excess sodium reabsorption leads to hypokalemia.
Epithelial sodium channel (ENaC) is present in the distal colon, ducts of exocrine glands, lungs, and apical surface of the epithelial surface of distal nephron 7. Patients with Liddle syndrome have an abnormality in the epithelial sodium channels in distal nephrons due to mutations in 1 of the 3 subunits. Due to this mutation, the degradation of the sodium channels has been impaired; therefore, the quantity of these channels on the apical surface of distal nephron increases inappropriately 8. The sodium feedback inhibition system is also impaired in patients with Liddle syndrome 9. Typically, increased intracellular sodium in distal nephron cells inhibit apical epithelial sodium channels, but in patients with Liddle syndrome, they become insensitive to sodium concentration. Increased sodium channels cause increased sodium retention which results in chronic volume retention and a hypertension state and suppressed renin and aldosterone levels 10. In this population, renal biopsy showed atrophy of juxtaglomerular cells due to chronically suppressed renin and aldosterone levels.
Liddle syndrome inheritance pattern
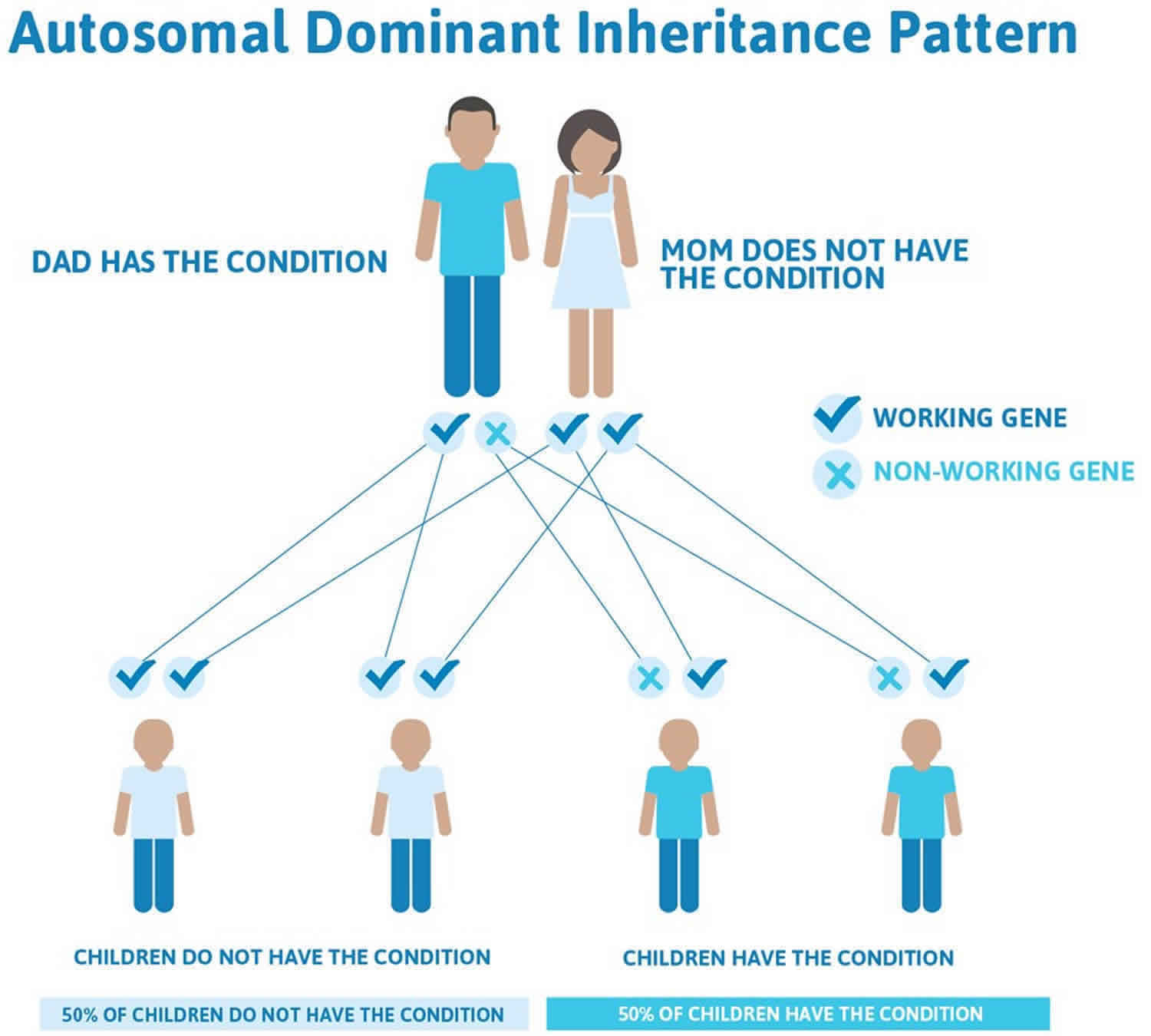
Liddle syndrome is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder.
Often autosomal dominant conditions can be seen in multiple generations within the family. If one looks back through their family history they notice their mother, grandfather, aunt/uncle, etc., all had the same condition. In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
Figure 1 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 1. Liddle syndrome autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Liddle syndrome symptoms
Patients with Liddle syndrome can be symptomatic or asymptomatic. It presents with early onset of hypertension between the age of 11 and 31 and resistant hypertension due to sodium reabsorption at the level of distal nephron. The healthcare provider may take years or decades to diagnose it. Providers often misdiagnose the symptoms. Hypertension due to Liddle syndrome is sensitive to a salt-restricted diet 4. Hypertension presents with a headache, dizziness, retinopathy, chronic kidney disease, left ventricular hypertrophy, and sudden death. Due to resistant hypertension, hypokalemia, and ventricular hypertrophy, a patient can develop lethal arrhythmias which can lead to sudden death.
Untreated resistant hypertension can eventually lead to heart disease and stroke.
Hypokalemia and metabolic alkalosis happen due to excessive loss of potassium in the urine at the expense of sodium reabsorption 11. Symptoms of hypokalemia can include weakness, fatigue, muscle pain (myalgia), constipation or heart palpitations.
The incidence of hypertension and hypokalemia in patients with Liddle syndrome is about 92.4% and 71.8% respectively 12. Healthcare providers can order genetic testing to diagnose patients with Liddle syndrome who do not have hypertension or hypokalemia. In these individuals, genetic testing is usually done because of family history.
Liddle syndrome complications
Liddle syndrome complications include hypokalemia, metabolic alkalosis, and resistant hypertension. The resistant hypertension patients can develop end-organ damage that includes myocardial infarction, transient ischemic attack/cerebrovascular accident, pulmonary edema, ventricular hypertrophy.
Liddle syndrome diagnosis
A diagnosis of Liddle syndrome is often suspected based the presence of early-onset hypertension (high blood pressure), especially in people with a family history of the condition. Additional testing can then be ordered to confirm the diagnosis. This may include 13:
- Blood tests which can detect low levels of potassium, renin and aldosterone.
- Urine tests to identify low levels of sodium (< 20 mEq or <20 mmol/L) and aldosterone.
- Genetic testing to look for a change (mutation) in the SCNN1B or SCNN1G gene.
Laboratory investigation may reveal hypokalemia and metabolic alkalosis 12. Hyperaldosteronism can also present with same features and biochemical abnormalities. Renin and aldosterone levels should be checked to differentiate between hyperaldosteronism and pseudo-hyperaldosteronism (Liddle syndrome). In patients with Liddle syndrome, renin and aldosterone levels are low in contrast to patients with hyperaldosteronism in whom aldosterone levels are high. Due to normal levels of aldosterone, spironolactone does not work for patients with Liddle syndrome 14.
Once a patient diagnosed with low-renin and low-aldosterone levels, a patient should take aldosterone for two months under the healthcare providers observation. Some conditions like glucocorticoid resistance syndrome, apparent mineralocorticoid excess syndrome, and congenital adrenal hyperplasia also respond well to this drug. If the patient does not respond to aldosterone, then the clinician should be suspicious for Liddle syndrome.
Ultimate the diagnosis made by genetic analysis of the gene that regulates epithelial sodium channel (ENaC).
Liddle syndrome treatment
Treatment for Liddle syndrome consists of following a low sodium diet and taking potassium-sparing diuretics, which reduce blood pressure and correct hypokalemia and metabolic alkalosis. Conventional anti-hypertensive therapies are not effective for this condition 13. The drug of choice is amiloride. It works well in Liddle syndrome as it directly inhibits epithelial sodium channel (ENaC). Amiloride is prescribed daily with a dose ranges from 5 to 20 mg. Triamterene, another potassium-sparing diuretic, similar to amiloride can also be used to manage Liddle syndrome. A sodium-restricted diet showed a cumulative effect with these drugs 15. However, excessive sodium accumulation on the receptor makes is unavailable for the medication 16. If renal function is normal, then the incidence of hyperkalemia is very rare. Avoidance of excessive potassium in the diet is suggested along with the use of potassium-sparing diuretics. Amiloride is safe in pregnancy 17.
Liddle syndrome prognosis
With treatment, the long-term outlook (prognosis) for people with Liddle syndrome is good. However, untreated hypertension may lead to stroke, heart disease and/or kidney problems which can be fatal 13. No researchers have investigated long-term mortality of Liddle syndrome. Clinicians often under treat and misdiagnose these patients. Further studies are needed to establish mortality in the population suffering from secondary hypertension due to Liddle syndrome.
References- Mubarik A, Aeddula NR. Liddle Syndrome. [Updated 2020 Jan 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536911
- Wang LP, Yang KQ, Jiang XJ, Wu HY, Zhang HM, Zou YB, Song L, Bian J, Hui RT, Liu YX, Zhou XL. Prevalence of Liddle Syndrome Among Young Hypertension Patients of Undetermined Cause in a Chinese Population. J Clin Hypertens (Greenwich). 2015 Nov;17(11):902-7.
- Liu K, Qin F, Sun X, Zhang Y, Wang J, Wu Y, Ma W, Wang W, Wu X, Qin Y, Zhang H, Zhou X, Wu H, Hui R, Zou Y, Jiang X, Song L. Analysis of the genes involved in Mendelian forms of low-renin hypertension in Chinese early-onset hypertensive patients. J. Hypertens. 2018 Mar;36(3):502-509.
- Pagani L, Diekmann Y, Sazzini M, De Fanti S, Rondinelli M, Farnetti E, Casali B, Caretto A, Novara F, Zuffardi O, Garagnani P, Mantero F, Thomas MG, Luiselli D, Rossi E. Three Reportedly Unrelated Families With Liddle Syndrome Inherited From a Common Ancestor. Hypertension. 2018 Feb;71(2):273-279.
- Tapolyai M, Uysal A, Dossabhoy NR, Zsom L, Szarvas T, Lengvárszky Z, Fülöp T. High prevalence of liddle syndrome phenotype among hypertensive US Veterans in Northwest Louisiana. J Clin Hypertens (Greenwich). 2010 Nov;12(11):856-60.
- Liddle syndrome. https://ghr.nlm.nih.gov/condition/liddle-syndrome
- Canessa CM, Schild L, Buell G, Thorens B, Gautschi I, Horisberger JD, Rossier BC. Amiloride-sensitive epithelial Na+ channel is made of three homologous subunits. Nature. 1994 Feb 03;367(6462):463-7.
- Lu C, Pribanic S, Debonneville A, Jiang C, Rotin D. The PY motif of ENaC, mutated in Liddle syndrome, regulates channel internalization, sorting and mobilization from subapical pool. Traffic. 2007 Sep;8(9):1246-64.
- Kellenberger S, Gautschi I, Rossier BC, Schild L. Mutations causing Liddle syndrome reduce sodium-dependent downregulation of the epithelial sodium channel in the Xenopus oocyte expression system. J. Clin. Invest. 1998 Jun 15;101(12):2741-50.
- Nakada T, Koike H, Akiya T, Katayama T, Kawamata S, Takaya K, Shigematsu H. Liddle’s syndrome, an uncommon form of hyporeninemic hypoaldosteronism: functional and histopathological studies. J. Urol. 1987 Apr;137(4):636-40.
- Unwin RJ, Luft FC, Shirley DG. Pathophysiology and management of hypokalemia: a clinical perspective. Nat Rev Nephrol. 2011 Feb;7(2):75-84.
- Monticone S, Buffolo F, Tetti M, Veglio F, Pasini B, Mulatero P. GENETICS IN ENDOCRINOLOGY: The expanding genetic horizon of primary aldosteronism. Eur. J. Endocrinol. 2018 Mar;178(3):R101-R111.
- Liddle syndrome. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=526
- Mulatero P, Verhovez A, Morello F, Veglio F. Diagnosis and treatment of low-renin hypertension. Clin. Endocrinol. (Oxf). 2007 Sep;67(3):324-34.
- Yang KQ, Lu CX, Fan P, Zhang Y, Meng X, Dong XQ, Luo F, Liu YX, Zhang HM, Wu HY, Cai J, Zhang X, Zhou XL. Genetic screening of SCNN1B and SCNN1G genes in early-onset hypertensive patients helps to identify Liddle syndrome. Clin. Exp. Hypertens. 2018;40(2):107-111.
- Warnock DG. Liddle syndrome: an autosomal dominant form of human hypertension. Kidney Int. 1998 Jan;53(1):18-24.
- Awadalla M, Patwardhan M, Alsamsam A, Imran N. Management of Liddle Syndrome in Pregnancy: A Case Report and Literature Review. Case Rep Obstet Gynecol. 2017;2017:6279460.