Liver metastases
Liver metastasis also called secondary liver cancer or metastatic liver disease, is cancer that started in another part of your body and spread to the liver. Liver metastasis is not the same as cancer that starts in the liver, which is called primary liver cancer. Liver metastasis is much more common than primary liver cancer.
For many types of cancer, liver metastasis is also called stage IV (four) cancer. The process by which cancer cells spread to other parts of the body is called metastasis. Liver metastases are sometimes present when the original (primary) cancer is diagnosed, or it may occur months or years after the primary tumor is removed.
When observed under a microscope and tested in other ways, metastatic liver cancer cells have features like that of the primary cancer and not like the cells in the place where the cancer is found. This is how doctors can tell that liver metastasis is cancer that has spread from another part of the body.
Liver metastatic cancer has the same name as the primary cancer. For example, breast cancer that spreads to the liver is called metastatic breast cancer, not liver cancer. It is treated as stage IV breast cancer, not as liver cancer.
Some kinds of cancer are more likely to spread to the liver than others. The most common types of cancer that spread to the liver are:
- Colorectal
- Lung
- Breast
- Pancreatic
- Stomach
- Melanoma
- Neuroendocrine
The risk of cancer spreading to the liver depends on the site of the original cancer. For example, cancers of the gastrointestinal tract often spread to the liver because their blood drains directly through the liver. Melanoma usually spreads through the body’s blood vessels to the liver.
After the lymph nodes, the liver is the most common site of metastatic spread. Most liver metastases originate from the colon, rectum, pancreas, stomach, esophagus, breast, lung, melanoma and some less common sites.
Cancer can spread to any part of the liver. Most people develop many liver metastases or multiple tumors in both lobes of the liver. The majority of liver metastases present as multiple tumors. Only 10% of all cases present with a solitary metastatic lesion (only one liver metastasis). Moreover, in more than three-quarters (3/4) of patients with liver metastases, there is involvement of both lobes of the liver.
Several factors influence the incidence and pattern of liver metastases. These include the patient’s age and sex, the primary site, the histologic type, and the duration of the tumor. In a few tumor types, such as colonic carcinoma, carcinoid, and hepatocellular carcinoma, metastasis is confined to the liver. Most tumors that metastasize to the liver, such as breast and lung cancers, spread to other sites at the same time.
Colorectal cancer frequently metastasizes to the liver. Patients presenting with operable liver metastases often receive chemotherapy followed by surgery to remove all visible disease, and then additional chemotherapy to eliminate non-visible microscopic disease. Patients with advanced colorectal cancer whose liver metastases are not amendable to surgery may still benefit from Radiofrequency Ablation (RFA) and microwave ablation and other therapeutic options.
Sometimes when people are diagnosed with metastatic cancer, doctors cannot tell where it started. This type of cancer is called cancer of unknown primary origin, or CUP.
Liver metastases symptoms
Liver metastases may not cause any symptoms at first because the liver is large and can work normally even if it contains cancer. Symptoms of liver metastases vary depending on the number of tumors and where they are in the liver. Other health conditions can cause the same symptoms as liver metastases.
See your doctor if you have these symptoms, especially if they are getting worse:
- loss of appetite
- nausea
- fatigue
- weight loss
- fever
- yellow skin and eyes and dark colored urine (called jaundice)
- itchy skin
- discomfort or pain in the abdomen
- swelling of the abdomen caused by a buildup of fluid (called ascites)
- swelling of the ankles.
Liver metastases possible complications
Complications are generally the result of tumors spreading to a large area of the liver. They can include:
- Blockage of the flow of bile
- Decreased appetite
- Fever
- Liver failure (usually only in the late stages of disease)
- Pain
- Weight loss
Liver metastases diagnosis
The following tests may be used to diagnose liver metastases. Many of the same tests can help your healthcare team plan treatment and monitor liver metastases.
Your health history is a record of your symptoms, risk factors and all the medical events and problems you have had in the past. In taking a health history, your doctor will ask questions about a personal history of symptoms that suggest liver metastases.
A physical exam allows your doctor to look for any signs of liver metastases. During a physical exam, your doctor may feel the abdomen to see if the liver is enlarged or sore when touched.
Blood tests
Blood tests are usually done to check your general health and find out how well the liver is working. The most common blood tests used to help diagnose liver metastases are liver function tests. Other blood tests that may be abnormal include a complete blood count (CBC), blood glucose (sugar) and blood clotting tests.
Sometimes tumor marker tests are done if you have had cancer before. These tests measure the amount of a specific protein in the body. For example, carcinoembryonic antigen (CEA) is a tumour marker measured in the blood. It is usually checked during follow-up after treatment for colorectal cancer. An increase in CEA (carcinoembryonic antigen) levels over time could mean the cancer has come back and it may have spread to the liver.
Imaging tests
Imaging tests are an important part of diagnosing liver metastases. It is common for people to have one or more imaging tests when the doctor thinks the cancer may have spread to the liver. The imaging tests used to diagnose liver metastases include the following.
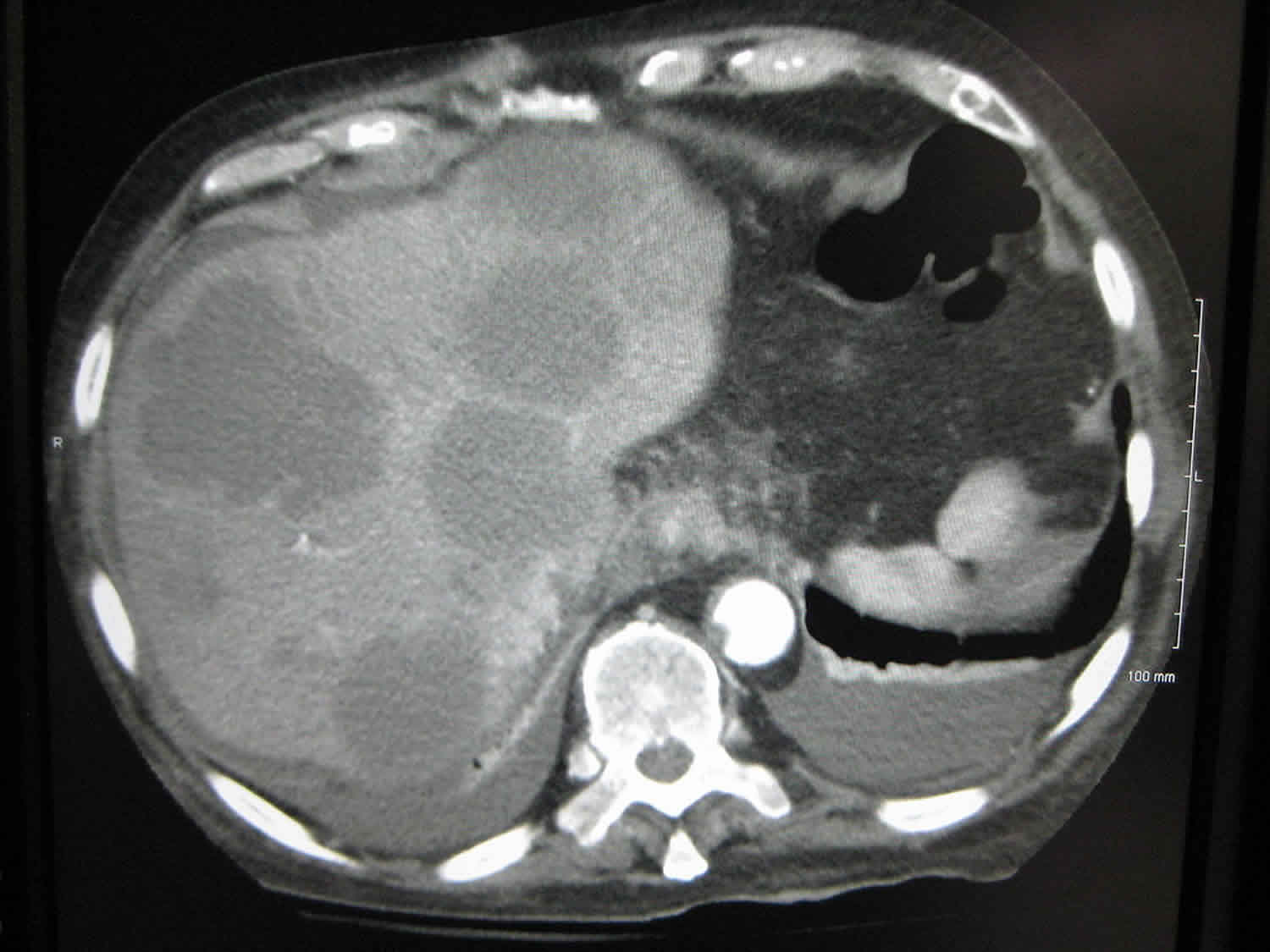
Computed tomography (CT) scan is a common imaging test to check for liver metastases. It can also check for metastases in organs and tissues around the liver. The CT scan is usually done with contrast medium to show areas more clearly.
Ultrasound is used to check for an enlarged liver or changes in its shape or texture. It is also used to guide a biopsy needle or laparoscope to a specific area of the liver.
Magnetic resonance imaging (MRI) may be used to find small metastatic tumors in the liver. It is usually used when doctors are not certain about the results of other imaging tests such as CT scan or ultrasound.
Positron emission tomography (PET) scan may be used to check for metastases in organs and tissues around the liver. It is often used when there is a history of colorectal or stomach cancer.
Biopsy
A biopsy is the removal of cells or tissues so they can be examined under a microscope. It may be needed to diagnose liver metastases. It is done when the doctor can’t tell if there is liver metastasis based on imaging tests or if there is no history of cancer. A biopsy may also be done to check tumor markers that help guide treatment. A percutaneous needle biopsy or endoscopic biopsy during laparoscopy may be used.
Other tests
If liver metastases are found before the primary cancer is diagnosed, the doctor may order tests to find out where the cancer started. These tests may include:
- CT scan of the chest to check for lung cancer
- Colonoscopy to check for colorectal cancer
- Laparoscopy to examine organs in the abdomen and pelvis
Liver metastases treatment
If you have liver metastases, your healthcare team will create a treatment plan just for you. It will be based on your needs and usually includes a combination of different treatments. Treatments can control and slow the growth of liver metastases, but most metastases don’t go away completely unless they can be removed by surgery. Treatments can also manage or prevent problems caused by liver metastases. These are sometimes called supportive therapies.
When deciding which treatments and supportive therapies to offer for liver metastases, your healthcare team will consider:
- where the cancer started
- where cancer is in the liver
- how many metastases there are
- the size of the metastatic tumors
- if there is metastatic cancer in other parts of the body
- cancer treatments you’ve already received
- how well the liver is working
- your personal preferences
You may be offered the following treatments and supportive therapies for liver metastases.
Chemotherapy
Chemotherapy is the most common treatment for liver metastases. It is used to help stop or slow the growth of cancer and relieve symptoms. Chemotherapy may also be used to shrink the cancer so surgery can be done, or it may be given after surgery to lower the risk of the cancer coming back. Chemotherapy is sometimes used along with other treatments such as targeted therapy.
Systemic chemotherapy means that the drugs circulate throughout the body to destroy cancer cells. It is usually given intravenously (through a needle into a vein) or orally (as a pill by mouth). The drugs, dose and schedule will vary for each person. The type of chemotherapy drug or combination of drugs used depends on where the cancer started.
Hepatic arterial infusion (HAI) is a procedure that delivers chemotherapy directly to liver tumors. The chemotherapy is supplied through a pump to the main artery of the liver called the hepatic artery. Floxuridine (FUDR) is the most common chemotherapy drug used in hepatic arterial infusion. Hepatic arterial infusion is not used as often as systemic chemotherapy because it is a complex and labor-intensive technique. It requires many medical experts, including surgeons, oncologists and radiologists, who all have experience in giving hepatic arterial infusion. It may be used to treat liver metastases when cancer has only spread to the liver and the tumors can’t be removed by surgery.
Chemoembolization, or transarterial chemoembolization (TACE), is a procedure that delivers chemotherapy directly to liver tumors. A catheter is placed in the hepatic artery, which is the main blood vessel that goes to the liver. The chemotherapy and a special substance that blocks the blood supply to the tumor called an embolic agent are given through the catheter. Once the blood supply is blocked, the cancer does not receive the oxygen and nutrients it needs to grow. Also, the tumor is exposed to the chemotherapy longer. Chemoembolization may be used to stop or slow the growth of liver metastases when the cancer has only spread to the liver.
Side effects of chemotherapy will depend mainly on the type of drug, the dose and how it’s given. Common side effects of many chemotherapy drugs are bone marrow suppression (low blood cell counts), nausea and vomiting, mouth problems and bowel problems. Hepatic arterial infusion (HAI) and transarterial chemoembolization (TACE) tend to have fewer side effects than systemic chemotherapy.
Targeted therapy
Targeted therapy uses drugs that find and attach to specific substances (such as proteins) on the surface of or inside cancer cells. These substances help send signals that tell cells to grow or divide. The targeted therapy drugs block the substances to stop or slow the growth and spread of cancer cells.
Targeted therapy may be used to control the growth of liver metastases from some types of cancer, such as:
- bevacizumab (Avastin) or cetuximab (Erbitux) is used for colorectal cancer
- erlotinib (Tarceva) is used for pancreatic cancer
Targeted therapy is given intravenously (through a needle into a vein) or orally (as a pill by mouth). It is most often used along with chemotherapy.
Side effects of targeted therapy depend mainly on the type and dose of the drug. Common side effects of many targeted therapy drugs include flu-like symptoms and fatigue. Most side effects go away on their own or can be treated. Tell your healthcare team if you have these side effects or others you think might be from targeted therapy.
Surgery
Surgery may be used to treat liver metastasis when only one area or a few areas of cancer are found. The surgery, called liver resection, removes the part of the liver that contains cancer. It is most often used for colorectal cancer that has spread to the liver.
A surgeon who specializes in liver surgery (called a hepatobiliary surgeon) will do the liver resection. This surgery is usually done by making a cut, or incision, in the abdomen (called open liver resection). The surgeon can also do a liver resection by making several small cuts in the abdomen and then inserting a laparoscope (a thin, tube-like instrument with a light and lens) and tools to do the surgery (called laparoscopic liver resection). A laparoscopic liver resection may not be available at all treatment centers. Liver resection takes several hours to complete.
Side effects of surgery will depend mainly on the amount of liver removed and your overall health. Some side effects include pain, bleeding, wound infection and pleural effusion.
Ablation therapy
Ablation therapy is a procedure that removes or destroys cells or tissues with heat, chemicals or other techniques. Different types of ablation therapy may be used to treat liver metastases. They are mainly used to treat small liver tumors when surgery can’t be done because it’s not safe or possible.
Ablation therapies for liver metastases are done by surgeons with specialized experience. They may not be available at all treatment centers.
The following ablation therapies may be used to treat liver metastases. Side effects will depend mainly on the procedure done and how much of the liver is treated.
Radiofrequency ablation (RFA) uses electrical currents to create heat that destroys cancer cells. A needle is placed directly into a liver tumor. The surgeon will use an imaging test, such as ultrasound or CT scan, to guide the needle into the tumor. Electrical currents are passed through the needle. These currents heat and destroy the tumor.
Cryotherapy uses extreme cold to freeze and destroy abnormal and cancerous cells or tissue. It is also called cryosurgery or cryoablation. The doctor uses an imaging test (such as ultrasound) to find the liver tumor that will be treated. Then the doctor places a probe directly into a liver tumor through a small cut, or incision, made in the skin. An extremely cold gas, such as liquid nitrogen, is passed through the probe to the tumor. The gas freezes and destroys the cancer. Sometimes the freezing process is repeated.
Percutaneous ethanol injection uses a needle to inject ethyl alcohol directly into a liver tumor. The doctor uses ultrasound or CT scan to guide the needle through the skin and into the tumour. The ethyl alcohol kills cancer cells and shrinks the tumor.
Radiation therapy
Radiation therapy also called radiotherapy, is not used that often to treat liver metastases. This is because radiation can damage the liver called radiation-induced liver disease. In rare cases, external beam radiation may be given to the whole liver to relieve symptoms called palliative treatment. Newer radiation therapy techniques can deliver more targeted doses of radiation to the liver tumors and lower the risk of liver damage.
Radioembolization or selective internal radiation therapy, is a procedure that delivers radiation directly to liver tumors. It uses tiny radioactive beads called microspheres. A catheter carries the radioactive beads through the hepatic artery to the liver. The beads deliver radiation only to the tumor and not to healthy liver tissue. They also block the blood supply to the tumor so the cancer can’t get the oxygen and nutrients it needs to grow. Radioembolization may be used to slow the growth of liver metastases and relieve symptoms when other treatments can’t be used.
Stereotactic body radiation therapy may be used when there are 1–3 small liver metastases. This is a type of external beam radiation therapy that delivers a high dose of radiation directly to a tumor. It avoids treating healthy liver tissue around the tumor with radiation. How many sessions of stereotactic radiation therapy are used depend on the size, location and number of metastases being treated, as well as other factors.
Side effects of radiation therapy will depend mainly on the type of radiation therapy and how much of the liver is treated. Common side effects of radiation therapy include fatigue and skin problems.
Hormonal therapy
Hormonal therapy is a treatment that adds, blocks or removes certain hormones to slow or stop the growth of cancer cells that need hormones to grow. Drugs, surgery or radiation therapy can be used as hormonal therapy.
Hormonal therapy may be used to help slow the growth of tumors in the liver and relieve symptoms. It is given for some types of cancer that have spread to the liver, especially breast cancer.
Side effects of hormone therapy will depend mainly on the type of hormonal therapy. Common side effects of many types of hormonal therapy are hot flashes, weight gain and less interest in sex.
Pain medicines
Not everyone with liver metastases will have pain. Pain can happen when the capsule around the liver is stretched. Pain medicines may be used. They are often given because other treatments may take a while to relieve pain or may not stop pain completely.
Pain medicines can be given different ways. They are usually given orally or intravenously. The most common pain medicines used for liver metastases are:
- opioids such as morphine (MS Contin, Statex, MOS) and codeine
- corticosteroids such as dexamethasone (Decadron, Dexasone)
- nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Motrin, Advil, Nuprin)
Side effects of pain medicines will depend mainly on the type of drug, the dose and the length of treatment. Common side effects of pain medicines like opioids are upset stomach, drowsiness and constipation. Corticosteroids can cause sleep problems, increased appetite, fluid buildup in the legs, arms or face, weight gain, high blood sugar levels, infection, mood changes and skin problems (such as a rash or acne). NSAIDs can upset the stomach.
Liver metastases prognosis
How well patients with metastatic liver cancer do depends on the location of the original cancer and how much it has spread to the liver. In a small number of cases, surgery to remove the liver tumors may lead to a cure. This is usually only possible in patients with certain tumor types (for example, colorectal cancer), and when there are a limited number of tumors in the liver.
In most cases, cancer that has spread to the liver is not curable. However, the treatments discussed above may help shrink tumors, improve life expectancy, and relieve symptoms.
Living with liver metastases
In many cases, liver metastasis is a chronic condition. Adjusting to life with liver metastases often takes time. A person with liver metastases may have concerns about the following.
Loss of appetite
Loss of appetite, or anorexia, is a common symptom of liver metastases. It can be caused by the cancer, the liver not working properly, treatments or other symptoms such as pain and ascites. Not eating enough because of loss of appetite can lead to problems like weight loss, a weakened immune system and fatigue.
There are several ways to manage loss of appetite and make sure you are getting enough nutrition. You can try to eat small meals and snacks at regular times throughout the day. Serve food cold or at room temperature to reduce strong tastes and smells. Eat foods high in calories and protein such as ice cream, nuts and eggs. Try commercial nutrition products when your appetite is poor. Ask your doctor about medicines that you could take to help improve appetite.
Fatigue
Many people with liver metastases have fatigue. Fatigue is when you feel tired and don’t have energy to do normal activities. It can greatly affect your quality of life.
Fatigue can be caused by many factors, including cancer treatments, loss of appetite, poor nutrition, pain and pain medicines. It can become a chronic problem. Talk to your healthcare team about ways to treat the causes and learn how to cope with fatigue.
Metastatic liver cancer life expectancy
A diagnosis of advanced cancer can lead to questions about survival. There is no way of knowing exactly how long someone will live with liver metastases. It depends on many factors, including where the cancer started, the number of tumors in your liver and the treatments used.
Survival with liver metastases depends on the type of cancer that has spread to the liver and whether or not surgery is possible. For example, survival with liver metastases from prostate or breast cancer is often measured in years. Survival with lung cancer that has spread to the liver is often measured in months. Some people may live much longer than expected, while others may die sooner than expected.
The best person to talk to about survival is the doctor. The doctor may be able to estimate survival based on what they know about a person and the type of cancer, but it’s not an exact science.
When metastatic liver cancer can no longer be controlled
If you have been told you have metastatic liver cancer that can no longer be controlled, you and your loved ones may want to discuss end-of-life care. Even if you choose to continue receiving treatment to try to shrink the cancer or control its growth, you can always receive palliative care to control the symptoms of cancer and the side effects of treatment.
Choices for care when treatment may not be an option
When dealing with advanced cancer, patients have different goals for their care. These goals may change over time. Some patients want to keep trying aggressive treatments. Others decide to choose other paths for care, such as controlling the symptoms of the disease.
Decisions for care are very personal and it’s natural to want to do all you can. But you should weigh these feelings against the risks and benefits of available treatments as well as your own feelings about life and death. You should ask all the questions you need to. If you choose not to go through active cancer treatment, you will continue to receive care and be made comfortable.
Palliative care
Palliative care is care that makes patients feel better but doesn’t treat the disease itself. Palliative care should begin when the cancer is diagnosed. It continues through treatment and beyond. Research shows that palliative care improves the quality of life of patients and family members. All patients have a right to comfort and quality of life throughout their care.
Palliative care is especially important if you choose to stop treating your cancer. It includes:
- Treating or preventing cancer symptoms and the side effects caused by treatment
- Getting help with emotional and spiritual problems
- Addressing the practical concerns of patients and families
Palliative treatment: Many of the same methods that are used to treat cancer, such as medicines and certain treatments, can also be used to reduce pain or other symptoms, and help a patient feel more comfortable. In advanced cancer, palliative treatment may be given to help a person feel better, even if it isn’t intended to treat the cancer. For example, doctors may give chemotherapy to slow the growth of a tumor that is causing pain. Or surgery may be performed to remove a mass that is pressing on certain nerves and causing pain.
To receive palliative care, members of your health care team may be able to help. However a palliative care specialist may be the best person to treat problems. Ask your doctor or nurse if there is a specialist you can see.
Hospice care
Hospice is a special type of care in which medical, psychological, and spiritual support are given to patients and their loved ones when cancer therapies are no longer controlling the disease. Although both hospice and palliative care provide comfort and support for patients, palliative care is available throughout a patient’s experience with cancer. A person’s cancer treatment continues while one is receiving palliative care, but with hospice care, the focus has shifted to just relieving symptoms and providing support at the end of life.
The goal of hospice care is to help you live each day to the fullest by controlling pain and other symptoms, making you as comfortable as possible. It is not intended to either hasten or postpone death. The focus is on caring, not curing. If your condition improves or your cancer goes into remission, hospice care can stop and active treatment can resume.
Choosing hospice care doesn’t mean that you’ve given up hope. Instead, hospice care means you’re changing what you hope for. This could be hoping for good quality of remaining life, including more time with loved ones and friends.
Hospice care can be given in different places. Hospice care most often takes place at home, but it can also be provided in special inpatient facilities, hospitals, and nursing homes. It can also take place along with professional home care if necessary. Hospice services may include:
- Doctor and nursing services
- Medical supplies and equipment
- Drugs for managing cancer-related symptoms and pain
- Short-term inpatient care
- Volunteers to give caregivers a break
- Counseling and spiritual care
- Social work services
- Grief counseling and support
Hospice professionals and volunteers are specially trained. They are committed to supporting the emotional needs of both patients and their families, and are trained to deal with medical symptoms. The hospice team usually includes doctors, nurses, home health aides, social workers, clergy or other counselors, and trained volunteers. The team may also include speech, physical, and occupational therapists, if needed. The hospice team will focus on your goals for end-of-life care, basing your care plan on your needs and desires.
Hospice can provide support for months. Even though many people believe that hospice is only available in the last days or weeks of life, it can provide support for months. Many people have said that they wished hospice care had begun earlier. They were surprised by the expert care and understanding that they got from hospice caregivers.
Your doctor must certify that you are eligible for hospice care. Most insurance plans, including Medicare, will cover hospice care once they receive a statement by both your attending doctor and the hospice medical director that states you have a life expectancy of 6 months or less. You would also sign a statement saying that you’re choosing hospice care. Hospice care can be continued if you live longer than 6 months, as long as your hospice doctor (and regular doctor if you still have one) recertifies your condition.
The hospice team or insurance provider can answer questions about whether certain care decisions, such as getting a second opinion or taking part in a clinical trial while in hospice care, would affect eligibility for hospice services.
Medicare and most Medicaid and private insurance plans pay for hospice services. Medicare is a government health insurance program for the elderly and disabled that is overseen by the Centers for Medicare and Medicaid Services (CMS).
- The Medicare hotline can answer your questions about hospice benefits and Medicare-certified hospice programs. Call 1–800–MEDICARE (1–800–633–4227); callers with TTY equipment can call 1–877–486–2048.
- The Medicare website has other tips and resources about coverage for hospice, including the booklet Medicare Hospice Benefits.
Medicaid, a federal–state partnership program that is part of the Centers for Medicare and Medicaid Services (CMS) and is administered by each state, is designed for people who need financial help for medical expenses. Information about coverage is available from local state welfare offices, state public health departments, state social services agencies, or the state Medicaid office. Information about specifc state locations can be found online (https://www.benefits.gov/categories/Healthcare%20and%20Medical%20Assistance).
Information about the types of costs covered by a particular private health policy is available from your hospital business office or hospice social worker, or from your insurance company.
Local civic, charitable, or religious organizations may also be able to help patients and their families with hospice expenses.
The following organizations can provide more information about hospice.
- National Hospice and Palliative Care Organization
- 1–800–658–8898 (helpline)
- 1–877–658–8896 (multilingual line)
- [email protected]
- https://www.nhpco.org
The National Hospice and Palliative Care Organization’s Caring Connections website offers information and publications focused on improving end-of-life care for adults and children. The site includes a database of national hospice programs. Some Spanish-language publications are available.
- National Association for Home Care & Hospice
- 202-547-7424
- https://www.nahc.org
The National Association for Home Care & Hospice has a home care and hospice agency locator in its information for consumers.