Lupus headaches
People who have lupus have an increased chance of having headaches compared to the rest of the population, occurring in up to 72% of systemic lupus erythematosus (SLE) patients. It is worth noting that in the vast majority of patients, headaches are not considered to be due to the lupus itself, but most likely have a separate cause. The most common type of headaches seen in lupus patients are migraine headaches and tension headaches. It is also not uncommon for people who have lupus to have headaches as a result of fibromyalgia (around 1-in-5 people with lupus will have this as an overlapping condition).
Lupus is a chronic, autoimmune disease. People with lupus have an overactive and misdirected immune system. Lupus is systemic, meaning that it affects a wide part of the body, including the joints, kidneys, skin, blood, brain and other organs.
Systemic lupus erythematosus (SLE) accounts for about 70 percent of all lupus cases. While SLE generally is considered the most serious form of lupus, cases range from very mild to severe. SLE affects various parts of the body and can cause joint pain, fatigue, hair loss, sensitivity to light, fever, rash and kidney problems.
Other types of lupus include:
- Cutaneous lupus erythematosus. It affects the skin.
- Drug-induced lupus. This is caused by the use of certain medications. Symptoms go away once the medicine is discontinued.
- Neonatal lupus. This type affects babies of women who have lupus. It typically disappears after about 6 months.
Lupus headaches causes
There are many different types and causes of headache, so it is helpful to understand which you have in order to manage your symptoms effectively.
Most headaches will go away on their own and aren’t a sign of something more serious. The most common reasons for having a headache are:
- Having a cold or the flu
- Stress
- Drinking too much alcohol
- Bad posture
- Problems with eyesight
- Not eating regular meals
- Not drinking enough fluids (dehydration)
- Taking too many painkillers
- Menstruation or the menopause
Around 15% of people with systemic lupus erythematosus (SLE) may experience headaches during a severe flare of their lupus. The exact cause of these lupus-related headaches is not understood and the diagnosis of “lupus headaches” involved a careful consideration and ruling out of the other possible causes.
Migraine
A migraine is usually a moderate or severe headache felt as a throbbing pain on one side of the head. Many people also have symptoms such as nausea, vomiting and increased sensitivity to light or sound. Some people have migraines frequently (up to several times a week) while other people only have a migraine occasionally. It’s possible for years to pass between migraine attacks. There are several types of migraine, including:
- Migraine with aura – where there are specific warning signs just before the migraine begins, such as seeing flashing lights.
- Migraine without aura – the most common type, where the migraine occurs without the specific warning signs.
- Migraine aura without headache, also known as silent migraine – where an aura or other migraine symptoms are experienced, but a headache doesn’t develop.
About 20% of the population suffers from migraine at some stage in their lives. Migraine often first appears in childhood, adolescence or early adulthood, but affects the greatest number of people between 35 and 45 years of age. Migraine is less common in children (about 2-5%) and affects girls and boys about equally. However, in adolescents and adults the disease disproportionately affects women (22% vs 10% lifetime prevalence).
In women, migraine frequency and severity are affected by hormones and, as a result, often change during adolescence, pregnancy and menopause. Beginning around menarche (the first menstrual cycle), its prevalence increases during reproductive years and then decreases around menopause. In women the symptoms of migraine tend also to be more severe and longer lasting. Women often experience an improvement in migraine during pregnancy, however, unfortunately it typically reappears following birth. After about 70 years of age the prevalence of migraine decreases to that of the middle teen years. At this stage there are less women suffering from migraine, but those who are may experience them more frequently, though accompanying symptoms such as nausea and photophobia are usually less pronounced.
The exact cause of migraines is unknown, although they’re thought to be the result of temporary changes in the chemicals, nerves and blood vessels in the brain. Some people find migraine attacks are associated with certain triggers, which can include:
- starting their period
- stress
- tiredness
- certain foods or drinks
- certain medications
- environmental triggers
‘Susceptibility to migraine is normally inherited. Certain parts of the brain employing monoamines, such as serotonin and noradrenaline, appear to be in a hypersensitive state, reacting promptly and excessively to stimuli such as emotion, bombardment with sensory impulses, or any sudden change in the internal or external environment. If the brainstem systems controlling the cerebral cortex become active, the brain starts to shut down, a process starting at the back of the brain in the visual cortex and working slowly forward. The pain nucleus of the trigeminal nerve becomes spontaneously active; pain is felt in the head or upper neck and blood flow in the face and scalp increases reflexly. Noradrenaline is released from the adrenal gland and causes the platelets to release serotonin. Serotonin in the circulation is thought to reflect levels of this neurotransmitter in the brain.
The brainstem nuclei of one side have a reciprocal effect on those of the other side; their effects may alternate, causing cortical changes on one side and headache on the other, or causing the headache itself to change from side to side.
Essentially, migraine is caused by the interaction between the brain and the cranial blood vessels. Treatment can be aimed at constriction of dilated arteries to abort each headache as it comes or at the brain itself in an attempt to prevent the headaches altogether.
This is the present hypothesis for the mechanism by which migrainous symptoms are produced 1.
Migraine triggers
Triggers are many and varied, not the same for everyone and not necessarily the same for different attacks in the same person. Identifying triggers may be complicated by the fact that it often takes a combination of triggers to set off a headache.
Dietary triggers
Common, well-recognized dietary triggers include:
- missed, delayed or inadequate meals
- caffeine (coffee and tea) withdrawal
- certain wines, beers and spirits
- chocolate, citrus fruits, aged cheeses and cultured products (chocolate and other sugar cravings may be prodomal not triggers)
- monosodium glutamate (MSG)
- dehydration.
Environmental triggers
Environmental triggers include:
- bright or flickering lights, bright sunlight
- strong smells, e.g. perfume, gasoline, chemicals, smoke-filled rooms, various food odors
- travel, travel-related stress, high altitude, flying
- weather changes, changes in barometric pressure (likewise, decompression after deep-sea diving)
- loud sounds
- going to the movies
- computers (overuse, incorrect use).
Hormonal triggers
Hormonal fluctuations are implicated as a significant trigger for women as three times as many women suffer from migraine headaches as men, this difference being most apparent during the reproductive years,. Hormonal triggers may be:
- Climacteric (final menstrual period)
- Menstruation (a UK study found 50% of women more likely to have migraine around menstruation)
- Ovulation
- Oral contraceptives
- Pregnancy (may worsen for first few months but in two thirds of women improves in latter part)
- Hormone replacement therapy (HRT)
- Menopause.
Physical and emotional triggers
Physical and emotional factors include:
- lack of sleep or oversleeping (even as little as half hour difference in routine, e.g. sleeping in on weekends)
- illness such as a viral infection or a cold (if taken cold and migraine medication, remember that many cold remedies contain pain-killers)
- back and neck pain, stiff and painful muscles, especially in scalp, jaw, neck, shoulders, and upper back
- sudden, excessive or vigorous exercise (regular exercise can however prevent migraine, if migraine is triggered by a blow to the head a doctor should be consulted)
- emotional triggers such as arguments, excitement, stress and muscle tension
- relaxation after stress (weekend headache).
Antiphospholipid syndrome
Antiphospholipid syndrome (APS) sometimes known as Hughes syndrome or ‘sticky blood’, is an autoimmune disease which affects the blood and its ability to clot. Between 30% and 50% of people who have SLE will be positive for antiphospholipid antibodies.
One of the most common features of antiphospholipid syndrome is recurrent headaches – often migrainous and sometimes accompanied by flashing lights, zigzag patterns, nausea and vomiting. If untreated, the migraines can become increasingly severe and frequent, and sometimes result in hemiplegic migraines which can mimic a transient ischemic attack (TIA) or stroke.
Pseudotumour cerebri
Pseudotumour cerebri also called benign intracranial hypertension, occurs in around 1% of people who have systemic lupus erythematosus (SLE). It is due to an increase in the pressure of fluid around the brain and spinal cord, causing headaches that are often severe, as well as blurred and double vision. “Pseudo-“ means “false” and “cerebri” means of the brain”. So “pseudotumour cerebri” means “a false tumour of the brain.” In other words, it is a condition that causes some symptoms that are similar to those of a brain tumour, but there is no tumour. Some people who have SLE develop pseduotumour cerebri caused by a blood clot due to antiphospholipid antibodies.
Aseptic meningitis
When the meninges (tissues and membranes that envelop the brain and spinal cord) are inflamed it is called meningitis. Meningitis is most commonly the result of an infection (which can be deadly if not identified and treated swiftly). If no bacteria or other microorganisms are found to be the cause of the inflammation then this is called aseptic meningitis (“a-“ means “not” and “septic” means “infectious”). Lupus is one of the possible causes of aseptic meningitis, although it appears to be a very rare manifestation. It can also be caused by medications including non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen. It is not known why, but people who have lupus are at an increased risk of this particular side effect from NSAIDs. Many types of viruses can cause aseptic meningitis but fortunately, the vast majority of these are mild infections that resolve on their own.
Meningitis typically causes headaches, fever, stiffness of the neck, and intolerance of light shining in the eyes. When severe, it can cause difficulty with thinking. It may be difficult to keep the hips and knees straightened while lying down, and patients may find it more comfortable to keep the hips and knees bent. On physical examination, the classic finding is nuchal rigidity (“nuchal” refers to the neck).
Lupus headaches prevention
One of the best ways of preventing migraines is recognizing the things that trigger an attack and trying to avoid them. You may find you tend to have a migraine after eating certain foods or when you’re stressed; by avoiding this trigger you may prevent a migraine.
Keeping a headache/migraine diary can help you identify possible triggers and monitor how well any medication you’re taking is working.
Here are some foods that people reported as triggers for their headaches/migraines:
- Monosodium glutamate (MSG)
- Dark chocolate and red wine
- Strong cheeses
- Anything with aspartame
- Anything with a lot of citrus
- Coffee
- Alcohol
- Skipping meals
Here are a few dos that may help to prevent some headaches.
DO
- Drink plenty of water
- Get plenty of rest if you have a cold or the flu
- Try to relax – stress can make headaches worse
- Exercise when you can
- Take paracetamol or ibuprofen (unless you have been indicated otherwise)
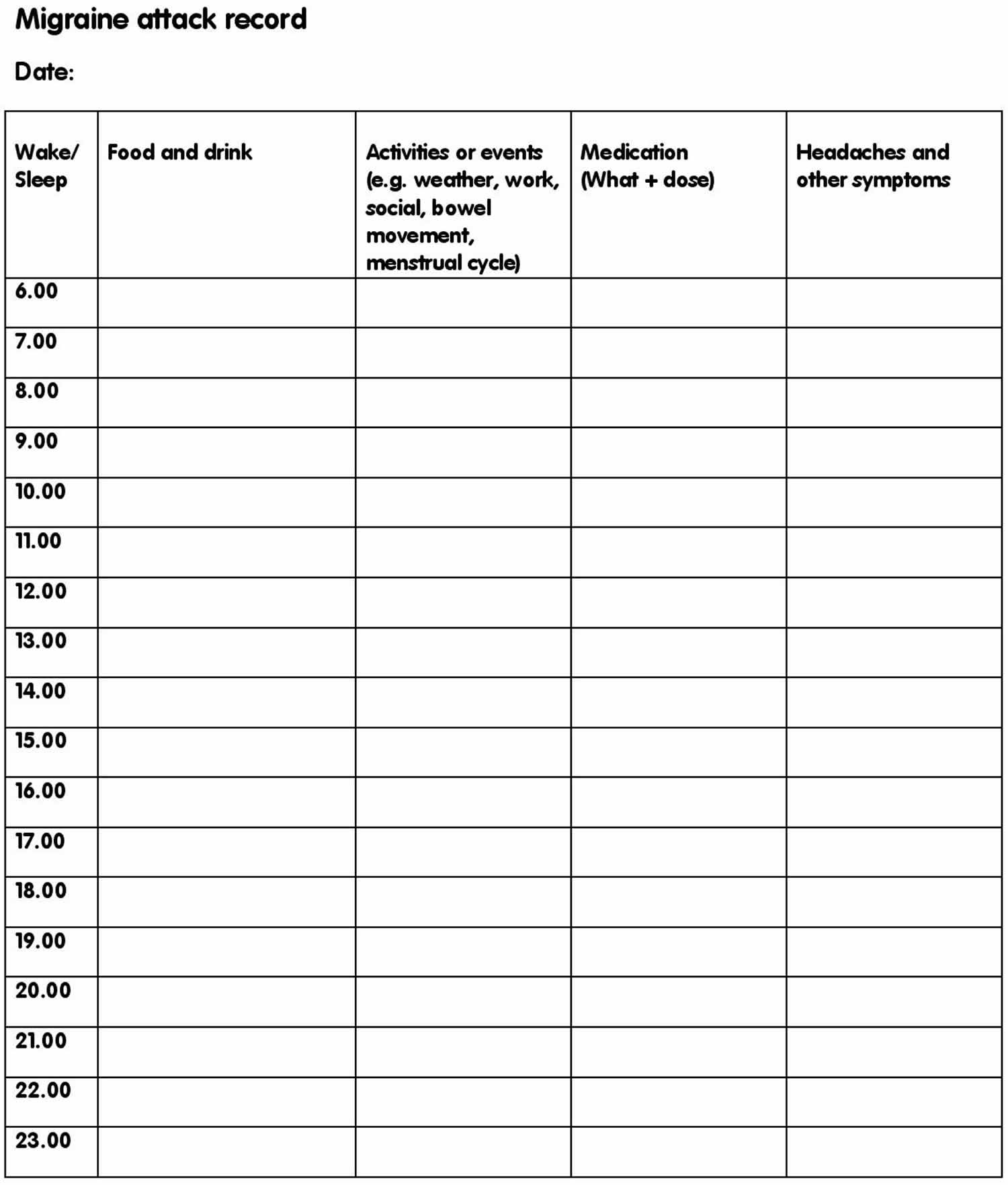
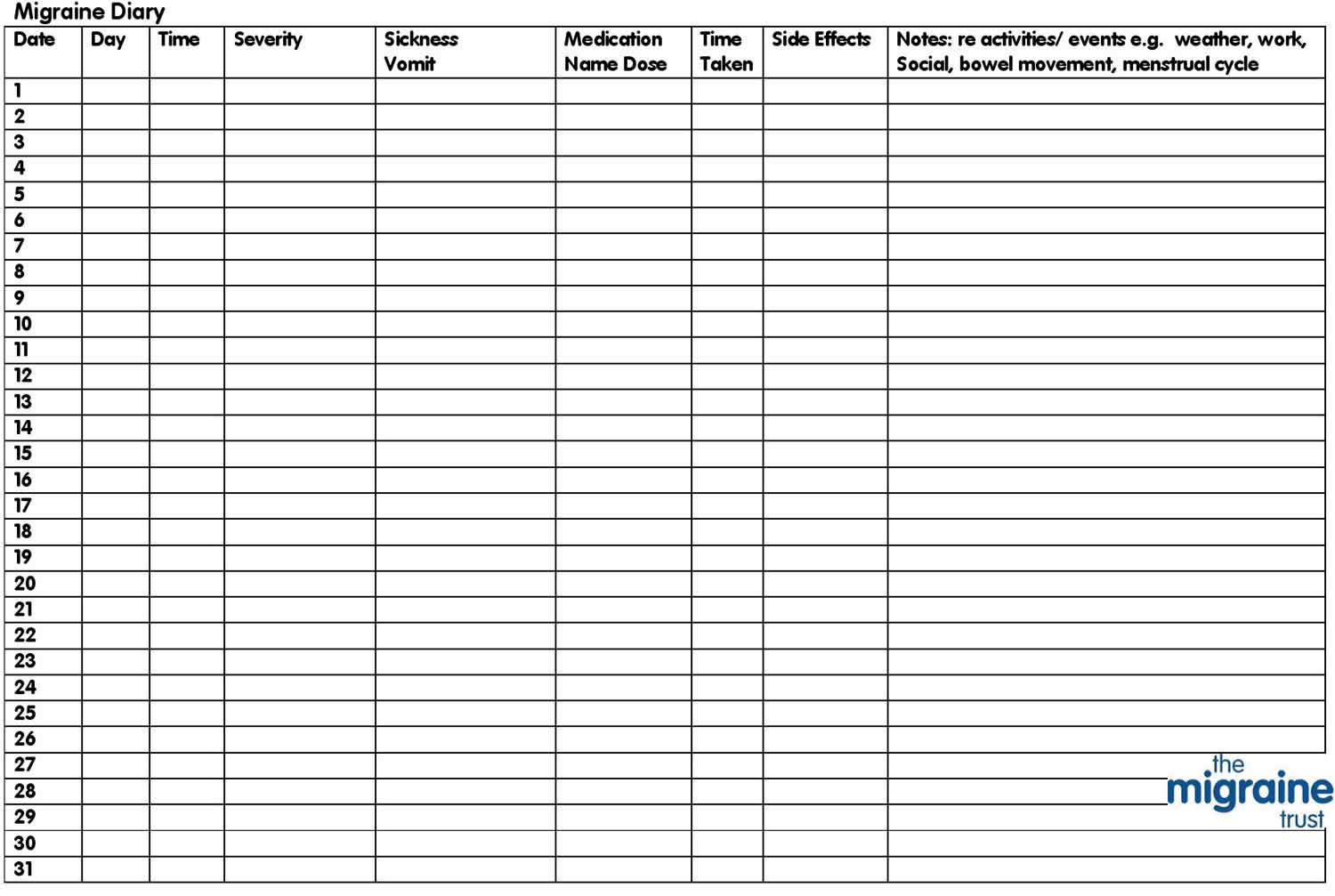
Migraine diary
To help with the diagnosis, it can be useful to keep a diary of your migraine attacks for a few weeks.
Note down details including (see Figure 1 below):
- the date
- time
- what you were doing when the migraine began
- how long the attack lasted
- what symptoms you experienced
- what medicines you took (if any)
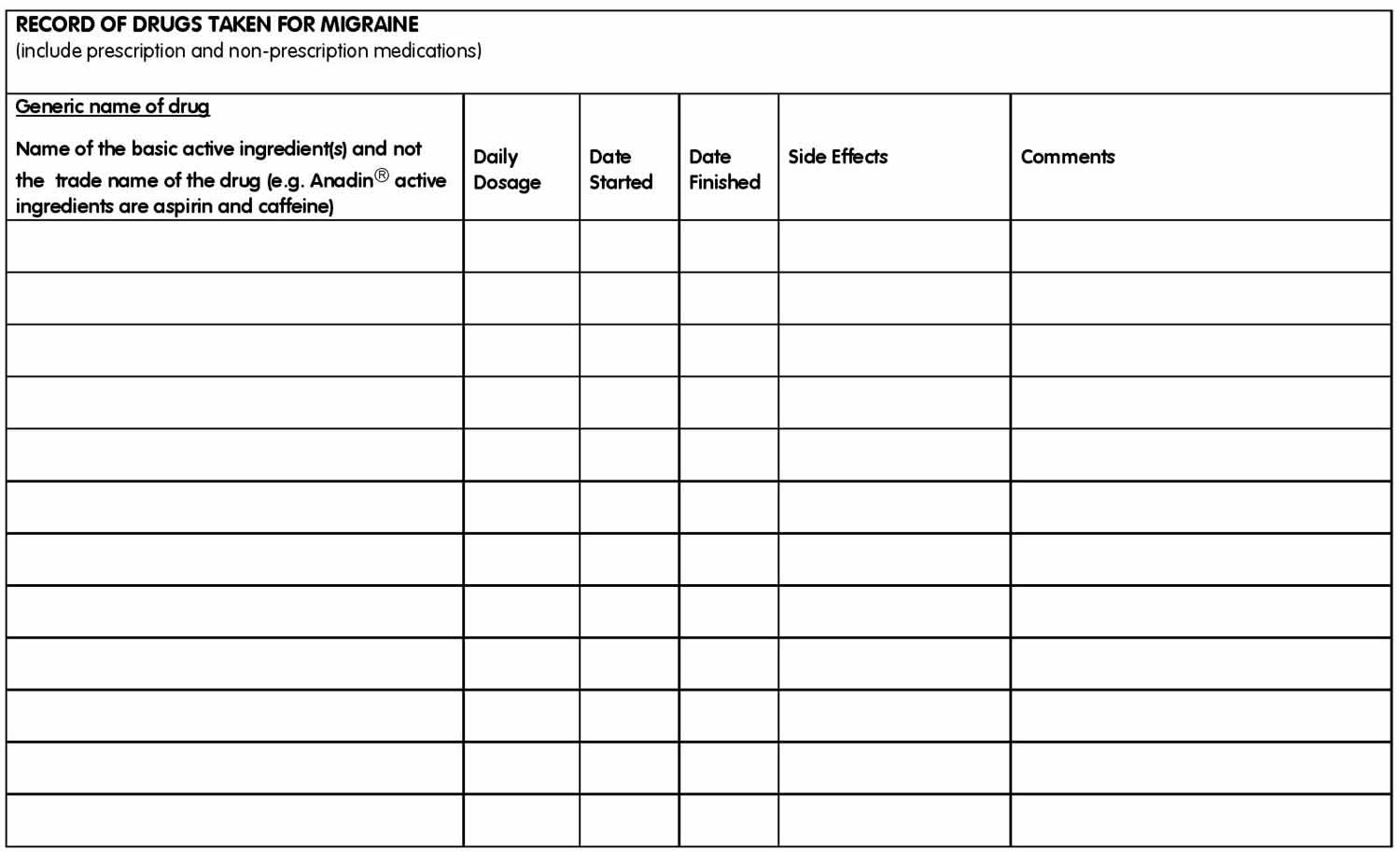
Regularly taking frequent doses of painkillers is an important reason why migraines can become difficult to treat. Doing so can cause a medication overuse headache.
Overuse headaches are usually caused by taking painkillers on a long-term basis and not because of exceeding, or just sticking to, the recommended dose.
It’ll be very helpful to keep a record of what painkillers you take and how often you take them.
You should not take painkillers on more than 10 days every month in the long term.
It may also be helpful for women to make a note when they start their period, as this can help your doctor identify potential triggers.
Figure 1. Headache diary
Lupus headache symptoms
The International Headache Society classifies a headache as a migraine when:
(a) the pain can be classified by at least two of the following:
- one sided
- moderate to severe
- throbbing
- aggravated by movement
(b) there is at least one of the following associated symptoms:
- nausea
- vomiting
- photophobia (sensitivity to light)
- phonophobia (sensitivity to noise)
(c) the headache lasts for between 4 and 72 hours.
Other migraine symptoms that may be experienced include:
- osmophobia (sensitivity to smell)
- aura (visual disturbances such as bright zigzag lines, flashing lights, difficulty in focusing or blind spots lasting 20-45 minutes)
- difficulty in concentrating, confusion
- a feeling of being generally extremely unwell
- problems with articulation or co-ordination
- diarrhea
- stiffness of the neck and shoulders
- tingling, pins and needles or numbness or even one-sided limb weakness
- speech disturbance
- paralysis or loss of consciousness (rare).
Migraine may occur recurrently over many years or even decades. Frequency may vary greatly in the same person over time, from a few a year up to several a week.
Stages of migraine
Migraine can be divided into five distinct phases:
1. Early Warning Symptoms (prodromol)
A significant number of migraineurs experience warning symptoms for up to 24 hours before the attacks start but may not recognize these signs until they know what to look for. These symptoms include:
- changes in mood, varying from feeling elated, on top of the world and full of energy, flying through the day’s work and accomplishing twice as much as usual, to feeling depressed and irritable
- gut symptoms, nausea, changes in appetite (intense hunger or sugar craving: may consume a whole packet of biscuits or chocolates), lack of appetite, constipation, diarrhea
- neurological changes, drowsiness, incessant yawning, difficulty finding the right words (dysphasia), dislike of light and sound, difficulty in eye focus
- changes in behavior, hyperactive, obsessional, clumsy, lethargic
- muscular symptoms, general aches and pains
- fluid balance changes, thirst, passing more fluid, fluid retention.
All these symptoms arise in the hypothalamus, the deep-seated part of the brain.
2. Aura
Aura accompanies migraine attacks for about 20 – 30% of migraineurs. The most common aura symptoms are visual disturbances such as bright zigzag lines, flashing lights, difficulty in focusing or blind spots. Aura affects the visual field of both eyes despite often seeming to affect one only and lasts 5-60 minutes then the vision normally restores itself. Less commonly aura affects sensation or speech. When several aura symptoms are present, they usually follow in succession.
3. Headache
Those experiencing classical migraine (migraine with aura) may or may not have a gap of up to an hour between the end of the aura and the onset of the head pain and may feel a bit ‘spaced out’ during the gap. Regardless of whether one experiences migraine with aura, or common migraine (migraine without aura), the headaches are similar. The headache phase can last up to three days. It is often throbbing and on one side of the head, but can affect both. It can be on the same or opposite side to the aura. Movement makes it worse. The most common accompanying symptoms in this phase are nausea, vomiting and sensitivity to light, sound and smell. Eating can help especially starchy foods. The symptoms can be more distressing than the headache itself.
4. Resolution
The way an attack ends varies greatly. Sleep is restorative for some. Being sick can make children feel much better. For others effective medication can improve attacks. For a few nothing works except the headache burning itself out.
5. Recovery (postdromol)
A feeling of being drained may exist for about 24 hours, others may feel energetic or even euphoric.
Most headaches will go away on their own and aren’t a sign of something more serious but you should make an appointment with your your doctor if:
- your headache keeps coming back.
- painkillers don’t help and your headache gets worse.
- you have a bad throbbing pain at the front or side of your head – this could be a migraine or, more rarely, a cluster headache.
- you feel sick, vomit and find light or noise painful.
- you get other symptoms – for example, your arms or legs feel numb or weak.
In some cases when severe headaches are experienced alongside other symptoms it can be a sign of something serious. You should see your doctor urgently if you have a severe headache and:
- your jaw hurts when eating.
- you have blurred or double vision.
- your scalp feels sore.
These could be signs that the arteries in your head and neck are inflamed. This needs urgent treatment.
You should call your local emergency number or go to emergency room if:
- The headache came on suddenly and is extremely painful.
- You have an extremely painful headache and:
- sudden problems speaking or remembering things.
- loss of vision.
- you’re feeling drowsy or confused.
- you have a very high temperature, feel hot and shivery, and have a stiff neck or a rash.
- the white part of your eye is red.
Lupus headaches diagnosis
Any patient with lupus who suffers from headaches should receive a systematic search for known causes including blood pressure checking, an examination of the blood for antiphospholipid antibodies and ultimately, if indicated, a brain scan.
The diagnosis of lupus headache involves a careful consideration and ruling out of other causes of headache by taking a history, performing a physical examination and blood tests, and, if necessary, ordering an MRI scan of the brain.
There’s no specific test to diagnose migraines. For an accurate diagnosis to be made, a doctor must identify a pattern of recurring headaches along with the associated symptoms.
Migraines can be unpredictable, sometimes occurring without the other symptoms. Obtaining an accurate diagnosis can sometimes take time.
Lupus headache treatment
If your headaches/migraines are severe or you’ve tried avoiding possible triggers and are still experiencing symptoms, your doctor may prescribe medication to help prevent further attacks.
Medication
Some people can manage their migraines with medications available from a pharmacy. For many others, these are not sufficiently effective. If this is the case, or you are unsure about the cause or nature of your headache, or if your headaches change, it is important you consult a doctor. Studies show that 50% of migraine sufferers have not been diagnosed. Even if you have previously consulted a doctor and the prescribed treatment has not been successful it is worth going again. Migraines can be managed, effective migraine management involves a partnership between you and your doctor. Some medications are given once the headache has begun (acute treatment) and others taken daily to reduce the frequency of attacks (preventative treatment).
Acute treatment
Infrequent, less severe migraine may respond to over-the counter medications such as:
- aspirin (not recommended for young children, some adults respond well to three tablets)
- acetaminophen (paracetamol)
- non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Nurofen, Brufen), naproxen (Naprosyn).
Medications that may be prescribed for more severe migraine include:
- triptans such as sumatriptan (Imigran), naratriptan (Naramig), zolmitriptan (Zomig) that are based on the serotonin molecule
- ergotamine compounds (Cafergot) that appear to provide relief by constricting cranial blood vessels
- stronger non-steroidal anti-inflammatory drugs
- stronger narcotic-type analgesics.
Anti-emetic medications often prescribed with other forms of acute therapy to minimize the nausea that often accompanies migraine include:
- metoclopramide (Maxolon), prochlorperazine (Stemetil) or domperidone (Motilium) to increase absorption and reduce nausea.
Combination medicines
You can buy a number of combination medicines for migraine without a prescription at your local pharmacy. These medicines contain both painkillers and anti-sickness medicines. If you’re not sure which one is best for you, ask your pharmacist.
It can also be very effective to combine a triptan with another painkiller, such as ibuprofen. Many people find combination medicines convenient. But the dose of painkillers or anti-sickness medicine may not be high enough to relieve your symptoms.
If this is the case, it may be better to take painkillers and anti-sickness medicines separately. This allows you to easily control the doses of each.
Preventive treatment
Prophylactic/preventive medication is taken daily, monthly or at regular intervals, regardless of whether a headache is present, to reduce the incidence of severe or frequent headaches. These include:
- beta blockers such as propranolol (Inderal), timolol (Blocadren), atenolol (Tenormin) and metoprolol (Lopresor, Betaloc) that block the beta-receptors on which adrenaline works in the nervous system as well as on blood vessels
- serotonin antagonists such as methysergide (Deseril), pizotifen (Sandomigran) and cyproheptadine (Periactin)
- sodium valproate or valproic acid (eg Epilim), an anti-epileptic drug shown to reduce the intensity of migraine
- calcium-channel blockers such as verapamil (Isoptin) that stop the constriction of blood vessels by preventing the use of calcium necessary for this reaction
- antidepressants such as amitriptyline (eg. Tryptanol) have an action on headache that is independent of their antidepressant action
- onabotulinumtoxin A (eg. Botox) is not just a beauty treatment. It has been proven to help those with chronic migraine.
- feverfew, a herbal remedy
- riboflavin 200mg twice daily has been reported as useful.
All are effective. All have side effects and, except feverfew and riboflavin, are prescription drugs. Many were initially introduced for some other problem and were also observed to reduce headache.
Treatment for pregnant and breastfeeding women
In general, migraine treatment with medicines should be limited as much as possible when you’re pregnant or breastfeeding.
Instead, trying to identify and avoid potential migraine triggers is often recommended.
If medicine is essential, your doctor may prescribe you a low-dose painkiller, such as paracetamol.
In some cases, anti-inflammatory medicine or triptans may be prescribed.
Speak to a doctor or your midwife before taking medicine when you’re pregnant or breastfeeding.
Complementary and alternative therapy
- Acupuncture: Stimulating acupoints may ease pain by encouraging production of endorphins (natural painkillers).
- Alexander technique: Can help prevent tension headaches by relieving poor posture and pressure that results from it.
- Aromatherapy: Combines various scented oils and promotes relaxation and eases tension.
- Biofeedback: Can be used to treat tension-type and migraine headaches – patient learns to control blood pressure, heart rate, and spasms in the arteries supplying the brain through a sensory device.
- Chiropractic therapy: Based on the theory that most diseases of the body are a result of a misalignment of the vertebral column with pressure on the adjacent nerves that may affect blood vessel and muscle function. Manual techniques purport to adjust the misalignment.
- Homeopathy: Uses active substances found in certain medications highly diluted.
- Hydrotherapy: Splashing your face with cold water before lying down for an hour can ease headache. Alternating hot and cold showers dilates then constricts the blood vessels, stimulating circulation. Ice pack on head is another option.
- Hypnotherapy: Can help sufferer deal with headache by altering the way the body interprets messages of pain.
- Massage: Can reduce muscle tension throughout the body, thereby reducing headache.
- Meditation: A recent study on migraine prevention through meditation has had very promising results, all participants reported less severe migraines.
- Naturopathy: Uses only natural substances in small amounts and aims to provide a healthier balance of bodily processes.
- Osteopathy: Manipulation of the neck or cranial, osteopathy may be used to correct misalignments of the vertebrae that can cause migraines.
- Physiotherapy: Treating muscle tension can release pressure that may lead to headache.
- Relaxation techniques: Geared towards reducing pressure in the body and the level of stress chemicals that may worsen headache.
- Shiatsu: Combination of massage and pressure can restore the “energy balance” and induce relaxation.
- Yoga: Can relieve muscle tension in the back of the neck and correct posture.
Transcranial magnetic stimulation
If the treatments above are not effectively controlling your migraines, your doctor may refer you to a specialist migraine clinic for further investigation and treatment.
In addition to the medicines mentioned above, a specialist may recommend other treatments, such as transcranial magnetic stimulation.
Transcranial magnetic stimulation
In January 2014, the National Institute for Health and Care Excellence 2 approved the use of a treatment called transcranial magnetic stimulation (TMS) for the treatment and prevention of migraines.
Transcranial magnetic stimulation involves holding a small electrical device to your head that delivers magnetic pulses through your skin.
It’s not clear exactly how transcranial magnetic stimulation works in treating migraines, but studies have shown that using it at the start of a migraine can reduce its severity.
It can also be used in combination with the medicines mentioned above without interfering with them.
But transcranial magnetic stimulation is not a cure for migraines and does not work for everyone.
The evidence for its effectiveness is not strong and is limited to people who have migraine with aura.
There’s also little evidence about the potential long-term effects of the treatment, although studies into the treatment have so far only reported minor and temporary side effects.
Side effects include:
- slight dizziness
- drowsiness and tiredness
- a muscle tremor that can make it difficult to stand
- irritability
National Institute for Health and Care Excellence 2 recommends that transcranial magnetic stimulation should only be provided by headache specialists in specialist centres because of the uncertainty about the potential long-term side effects.
The specialist will keep a record of your experiences using the treatment.
Pseudotumour cerebri
Draining some of the cerebrospinal fluid (CSF) from the spinal canal (which also decreases the amount around the brain) is a way to treat and lessen the symptoms of pseudotumour cerebri. Other therapies include treating lupus with steroids and other immunomodulating therapies. In addition, diuretics may be helpful in decreasing the fluid pressure. In more resistant cases, surgery of the eyes can relieve the amount of increased pressure around the brain, usually providing a more permanent treatment. If the pseudotumour cerebri is caused by a blood clot in the brain due to antiphospholipid antibodies it is treated with blood thinners such as warfarin.
Aseptic meningitis
If a person who has lupus develops meningitis, in addition to being treated with antibiotics (in case of bacterial infection), it is also important that any NSAIDs be discontinued in case they are the cause. Fortunately, this cause of meningitis resolves when the NSAID is stopped. The drugs azathioprine and intravenous immunoglobulin (IVIG for short) may also rarely cause aseptic meningitis in people who have lupus. If all other potential causes have been ruled out then it is presumed that the aseptic meningitis is directly due to inflammation from SLE. In that case, the doctor will usually treat it with high doses of steroids.
References