What is malabsorption
Malabsorption is a condition when you are unable to absorb nutrients from your digestive system into the bloodstream. Malabsorption syndrome refers to a number of disorders in which nutrients from food are not absorbed properly in your small intestine. Your small intestine does most of the digesting of the foods you eat. If you have a malabsorption syndrome, your small intestine cannot absorb nutrients from foods. Although digestion and absorption of nutrients primarily happens in the small bowel, other areas of the body provide additional enzymes involved. The salivary glands, stomach, pancreas, and small intestine interact with each other to facilitate digestion and absorption. Due to the involvement of these other organs, malabsorption issues and clinical diagnoses may stem from regions other than the small intestine. For example, pancreatic insufficiency, pernicious anemia, and cystic fibrosis are all diseases involving malabsorption, yet they do not originate in the small intestine.
Normally, foods are digested and nutrients (proteins, carbohydrates, fats, vitamins, and minerals) are absorbed into the bloodstream mainly in the small intestine.
Malabsorption may occur if a disorder:
- Interferes with the digestion of food
- Interferes with the absorption of nutrients
Your body digests foods in three stages: first proteins, fats, and carbohydrates are broken down, in the stomach by acid and enzymes and in the small intestines by enzymes produced by the pancreas and bile from the liver, into their component parts. They are then absorbed, primarily in the small intestines. Finally, the nutrients are transported throughout the body and used or stored.
If there are not enough pancreatic enzymes or bile available, then fat and other foods cannot be properly digested. If a condition prevents the intestines from absorbing nutrients, then they are “lost” by excretion in the stool. In both cases – improper digestion or absorption – the affected person can experience symptoms associated with malabsorption and in severe cases, symptoms of malnutrition and vitamin deficiency. If the condition prevents the digestion and/or absorption of fats from the diet, then excess fat is present in the stool and the person may experience prolonged diarrhea with stomach pain, cramps, bloating, gas, and weight loss.
Malabsorption can be classified as either global, involving the entire mucosa of the small intestine or partial, dealing with malabsorption of specific nutrients 1. Clinical features of malabsorption are relatively specific to the type of nutrient that is deficient, yet weight loss and fatty, greasy stools are classical findings of global malabsorption 1. Stools are typically voluminous and pale. Most patients present with nonspecific gastrointestinal symptoms: abdominal pain, flatulence, anorexia, and distension. Patients with malabsorption issues may also be asymptomatic 2.
During instances of isolated malabsorption, such as celiac disease, specific manifestations such as bone thinning or iron deficiency anemia may be the only presentation 3. Malabsorption of carbohydrates can cause milk intolerance and watery diarrhea, protein can lead to muscle atrophy, and menstrual irregularities, folic acid, and iron deficiency lead to anemia, vitamin A deficiency causes night blindness, and vitamin K deficiency can cause bleeding disorders 1. It is also important to note that some causes of malabsorption, such as the malabsorption of fats from celiac disease or pancreatic insufficiency, can cause the malabsorption of other substances such as vitamin D, which needs chylomicrons to be effectively absorbed 1.
Symptoms of different malabsorption syndromes can vary. They often include chronic diarrhea, abnormal stools, weight loss, and gas. Your doctor may use lab, imaging, or other tests to make a diagnosis.
Causes of malabsorption syndromes include:
- Celiac disease
- Lactose intolerance
- Short bowel syndrome. This happens after surgery to remove half or more of the small intestine. You might need the surgery if you have a problem with the small intestine from a disease, injury, or birth defect.
- Whipple disease, a rare bacterial infection
- Genetic diseases
- Certain medicines
Long-term malabsorption can result in:
- Anemia
- Gallstones
- Kidney stones
- Thin and weakened bones
Your health care provider will do an exam. Tests that may be done include:
- Blood and urine tests
- CT scan of the abdomen
- Hydrogen breath test
- MR or CT enterography
- Schilling test for vitamin B12 deficiency
- Secretin stimulation test
- Small bowel biopsy
- Stool culture or culture of small intestine aspirate
- Stool fat testing
- X-rays of the small bowel or other imaging tests
Treatment of malabsorption syndromes depends on the cause. See your healthcare provider if you have symptoms of malabsorption.
Small intestine role in digestion and absorption of nutrients
Carbohydrates, proteins, and lipids are digested and absorbed by the small intestine 1. Dietary carbohydrates begin as polysaccharides, such as amylose, or disaccharides, such as lactose, sucrose, maltose, or trehalose. Each disaccharide is made up of 2 monosaccharides. The monosaccharides are glucose, fructose, and galactose. For the small bowel enterocytes to absorb carbohydrates, they must be broken down into monosaccharides. The enzyme responsible for carb digestion is amylase, which is found in the saliva and pancreas. Alpha-amylase is found in the mouth and begins the digestion of carbohydrates, but the pancreatic amylase is primarily responsible for hydrolyzing starches. Along with amylase, the small intestine brush border contains enzymes that digest carbohydrates, including maltase, isomaltase, sucrase, beta-galactosidase, and trehalase complex. The monosaccharides are absorbed on the apical membrane via carrier-mediated transporters, SGLT1 and GLUT5. Glucose and galactose use SGLT1 (fueled by sodium), while GLUT5 transports fructose 4.
Protein digestion occurs via the breaking of peptide bonds through hydrolysis by proteolytic enzymes. Proteins are broken down into their amino acids. Pepsin is a proteolytic enzyme in the stomach, which is where protein digestion is started. Chief cells secrete pepsinogen, an inactive precursor of pepsin, which can activate itself. Although pepsin helps digestion in the stomach, it is not completely necessary for protein digestion and must have an environment with a pH of 1 to 3 to work properly. Pepsin is not found in the small intestine, as the pancreatic fluids cause the duodenum to be a more basic environment. The pancreas secretes trypsin, chymotrypsin, elastase, and carboxypeptidase A and B. These proteases from the pancreas are released once the duodenum releases cholecystokinin (CCK) in the presence of proteins. The inactive forms of these pancreatic proteases are released first, and enteropeptidase (also called enterokinase) turns them into their active forms. Once Trypsin is activated, it can activate more of itself to hasten digestion. Protein digestion yields free amino acids, dipeptides, tripeptides, and oligopeptides. Dipeptides and tripeptides are transported via Pept-1, which requires a hydrogen ion gradient. Amino acid absorption involves many carrier-mediated active and facilitated transport proteins 4.
Dietary fats come in the form of triglycerides and are acquired mostly from animal sources. Triglycerides are broken down into 2-monoglycerides and fatty acids. Lipid digestion enzymes come from many areas prior to the duodenum, including lingual, gastric, and pancreatic lipases. Cholecystokinin (CCK) release from the duodenum causes sluggish gastric emptying, allowing for more time for lipid digestion by the lingual and gastric lipases. There are also lipases within foods, termed food-bearing lipases, that can begin auto-digesting themselves. Colipase, lipase, phospholipase A2, and cholesterol ester hydrolase are pancreatic enzymes that break down fats. Bile salts cause the inactivation of lipases. Colipase prevents lipase inactivation. Emulsification is important in fat digestion, as it breaks fat globules into smaller droplets, increasing the surface area for pancreatic lipases. Absorption of lipids was thought to be passive, yet discovery of fatty acid binding proteins supports an active course. Fatty acids are relocated to the endoplasmic reticulum of enterocytes and reformed. Free fatty acids are most commonly absorbed in the jejunum of the small intestine 4.
Vitamins and minerals are also absorbed by the small intestine. Folate goes through hydrolysis, is absorbed in the duodenum and upper part of the jejunum, and is actively transported into portal circulation. Vitamin B12, or Cobalamin, is absorbed in the terminal ileum. B12 must bind to R protein in the stomach. Once the B12-R complex reaches the duodenum, R protein is hydrolyzed, and B12 binds to intrinsic factor (IF), which is secreted by the gastric parietal cells. The B12-IF complex travels to the terminal ileum and enters the enterocyte via ileal receptors. Vitamins A, D, E, and K are fat-soluble and may be passively absorbed in the small bowel. Approximately 9 liters of water travels to the gastrointestinal tract per day, and the small intestine absorbs 7 to 8 liters, while the colon absorbs the remaining 1 to 2 liters. Water absorption is thought to occur via osmotic gradients and aquaporins on intestinal membranes 4.
What causes malabsorption
Diarrhea is defined as the abnormal passage of loose or liquid stools more than three times per day, and/or stool volume >200 g/day 5. Chronic diarrhea is defined as an increase in stool frequency and/or volume that persists for longer than three to four weeks. Chronic symptoms generally do not suggest an infectious cause, although patients may report that symptoms are preceded by gastrointestinal infection or food poisoning. The most common causes in clinical practice are inflammatory syndromes of the small bowel or colon (e.g., Crohn disease, celiac disease); functional bowel disorders (e.g., irritable bowel syndrome [IBS]); neoplasia; pancreatic insufficiency resulting in maldigestion; intestinal dysmotility; and small bowel malabsorption (e.g., postgastrointestinal surgery) (see Table 1).
A common but frequently underinvestigated cause of chronic diarrhea is bile acid malabsorption resulting from dysregulation of the enterohepatic recycling of bile acids and of bile acid production 6.
Causes of malabsorption syndromes include:
Digestion problems
- Digestion of food can be affected by
- Disorders that prevent adequate mixing of food with digestive enzymes and stomach acid
- Insufficient production of digestive enzymes
- Decreased production of bile
- Too much stomach acid
- The wrong kinds of bacteria growing in the small intestine
Inadequate mixing may occur in a person who has had part of the stomach surgically removed.
In some disorders, the body produces inadequate amounts or types of digestive enzymes, which are necessary for the breakdown of food. For example, a common cause of malabsorption is insufficient production of digestive enzymes by the pancreas, which occurs with some pancreatic diseases, or by the small intestine, which occurs in lactase deficiency (lactose intolerance).
Decreased production of bile, too much acid in the stomach, or too many of the wrong kinds of bacteria growing in the small intestine (bacterial overgrowth syndrome) may also interfere with digestion.
Absorption problems
- Absorption of nutrients into the bloodstream can be affected by:
- Disorders that injure the lining of the small intestine
- Surgical removal of a large section of the small intestine
- Disorders that affect the flow of lymphatic fluid from the bowel
The normal lining consists of small projections called villi and even smaller projections called microvilli, which create an enormous surface area for absorption. Infections (bacterial, viral, or parasitic) and disorders such as celiac disease and Crohn disease all may injure the intestinal lining.
Surgical removal of a large section of the small intestine substantially reduces the surface area for absorption (short bowel syndrome).
Disorders that affect the flow of lymphatic fluid from the bowel into the bloodstream (the path that fats must take to enter the bloodstream), such as malformation of intestinal lymph vessels (intestinal lymphangiectasia), blockage of lymph vessels due to lymphoma (cancer of the lymphatic system), or impaired entry of lymph fluid into the bloodstream due to some heart disorders, also reduce absorption.
Causes of malabsorption
Many diseases can cause malabsorption. Most often, malabsorption involves problems absorbing certain sugars, fats, proteins, or vitamins. It can also involve an overall problem with absorbing food.
Problems or damage to the small intestine that may lead to problems absorbing important nutrients. These include:
- Celiac disease
- Crohn disease
- Damage from radiation treatments
- Overgrowth of bacteria in the small bowel
- Parasite or tapeworm infection
- Surgery that removes all or part of the small intestine
Enzymes produced by the pancreas help absorb fats and other nutrients. A decrease of these enzymes makes it harder to absorb fats and certain nutrients. Problems with the pancreas may be caused by:
- Cystic fibrosis
- Infections or swelling of the pancreas
- Trauma to the pancreas
- Surgery to remove part of the pancreas
Some of the other causes of malabsorption include:
- AIDS and HIV
- Certain medicines (tetracycline, some antacids, some medicines used to treat obesity, colchicine, acarbose, phenytoin)
- Gastrectomy and surgical treatments for obesity
- Cholestasis
- Chronic liver disease
- Cow’s milk protein intolerance
- Soy milk protein intolerance
Table 1. Potential causes of chronic diarrhea in clinical practice
| Colon (large intestine) | Colonic neoplasia |
| Inflammatory bowel disease (ulcerative colitis, Crohn’s colitis) | |
| Microscopic colitis | |
| Small intestine | Celiac disease |
| Crohn disease | |
| Other small bowel enteropathies | |
| Bile acid malabsorption | |
| Disaccharidase deficiency | |
| Small bowel bacterial overgrowth | |
| Mesenteric ischemia | |
| Radiation enteritis | |
| Lymphoma | |
| Chronic infection (e.g., giardiasis) | |
| Pancreas | Chronic pancreatitis |
| Pancreatic carcinoma | |
| Cystic fibrosis | |
| Endocrine | Hyperthyroidism |
| Diabetes | |
| Hypoparathyroidism | |
| Addison disease | |
| Hormone-secreting tumours (e.g., VIPoma, carcinoid, gastrinoma) | |
| Other | Factitious diarrhea |
| Surgery (eg, small bowel resection, internal fistulas) | |
| Drugs (eg, nonsteroidal anti-inflammatory drugs, antihypertensives, antibiotics, antiarrhythmics, antineoplastics, drugs containing magnesium) | |
| Food additives (e.g., sorbitol, fructose) | |
| Alcohol abuse | |
| Autonomic neuropathy |
Bile acid malabsorption
Bile acid malabsorption is a common but frequently under-recognized cause of chronic diarrhea, with an estimated prevalence of 4% to 5% 6. Excessive levels of bile acids in the lower gastrointestinal tract may cause diarrhea via one or more mechanisms: altering water and sodium transport; increasing lower gastrointestinal motility; damaging the mucosa; inducing mucus secretion; or stimulating defecation 7. One-third of new patients presented with chronic diarrhea. Bile acid malabsorption is classified as type 1 (secondary to ileal dysfunction), type 2 (idiopathic) or type 3 (secondary to gastrointestinal disorders not associated with ileal dysfunction) 6.
Three subtypes of bile acid malabsorption have been categorized. Type 1 includes patients with terminal ileal disease (eg, Crohn disease, resection) or radiation injury resulting in impaired bile acid reabsorption; type 2 is idiopathic; and type 3 comprises conditions unrelated to ileal disease (eg, celiac disease, cholecystectomy, bacterial overgrowth) that alter intestinal motility or bile acid absorption (Table 2) 8.
Table 2. Classification of bile acid malabsorption
| Classification of bile acid malabsorption | Cause |
|---|---|
| Type 1 Ileal dysfunction (secondary bile acid malabsorption) | Ileal Crohn disease, ileal resection
|
| Type 2 Idiopathic bile acid malabsorption/primary bile acid diarrhea | Unknown cause
|
| Type 3 Other conditions | Postcholecystectomy, postvagotomy, celiac disease, bacterial overgrowth, pancreatic insufficiency (chronic pancreatitis and cystic fibrosis)
|
The estimated prevalence of bile acid malabsorption is >90% in patients with resected Crohn disease (Crohn’s disease) and 11% to 52% of unresected Crohn disease patients (type 1); 33% in diarrhea-predominant irritable bowel syndrome (type 2); and is a frequent finding postcholecystectomy or postvagotomy (type 3) 6.
Bile acid malabsorption was considered in the diagnostic workup in 22% of chronic diarrhea cases. Overall, only 1% of all new cases and 3% of chronic diarrhea cases were diagnosed with bile acid malabsorption; among bile acid malabsorption cases, 61% were type 1, 22% were type 2 and 15% were type 3. Thirty-nine per cent of clinicians investigated only a selected group of patients, and 22% reported they investigated bile acid malabsorption rarely or not at all.
Often under-recognized in practice is type 2 bile acid malabsorption (idiopathic bile acid malabsorption), which potentially affects a wide range of patients with chronic diarrhea. While the etiology of idiopathic bile acid malabsorption is unclear, several underlying pathophysiological mechanisms have been proposed. Some 9, but not all 10, studies have suggested that idiopathic bile acid malabsorption is associated with more rapid small-bowel and colonic transit times. Genetic variants in the FGF19-FGFR4-Klothoβ pathway, which affects colonic transit times, have been reported in diarrhea-predominant irritable bowel syndrome (IBS-D) 11. However, these variants may play a more important role in dysregulation of the bile acid pool. A recent study reported that 38% of diarrhea-predominant irritable bowel syndrome (IBS-D) patients exhibited increased bile acid synthesis, as measured by serum levels of 7α-hydroxy-4-cholesten-3-one (C4), and higher body mass index 12.
Similar results were found in a study comparing idiopathic bile acid malabsorption patients with diarrhea versus healthy controls 13. Fasting C4 levels were significantly higher in patients with idiopathic bile acid malabsorption compared with controls (51 ng/mL versus 18 ng/mL), suggesting dysregulation of bile acid synthesis. Moreover, median fibroblast growth factor 19 (FGF19) levels were significantly lower in idiopathic bile acid malabsorption versus controls (120 pg/mL versus 231 pg/mL), indicating that a deficiency in FGF19 feedback inhibition of bile acid synthesis may contribute to an overproduction of bile acids that cannot be accommodated by ileal reabsorption. FGF19 levels were also found to be low in patients postcholecystectomy (type 3 bile acid malabsorption).
Investigations include bile acid malabsorption fecal bile acid assay, 23-seleno-25-homo-tauro-cholic acid (SeHCAT) testing and high-performance liquid chromatography of serum 7-α-OH-4-cholesten-3-one (C4), to determine the level of bile acid synthesis. A less time-consuming and expensive alternative in practice is an empirical trial of the bile acid sequestering agent cholestyramine. An estimated 70% to 96% of chronic diarrhea patients with bile acid malabsorption respond to short-course cholestyramine. Adverse effects include constipation, nausea, borborygmi, flatulence, bloating and abdominal pain. Other bile acid sequestering agents, such as colestipol and colesevelam, are currently being investigated for the treatment of bile acid malabsorption-associated diarrhea 6.
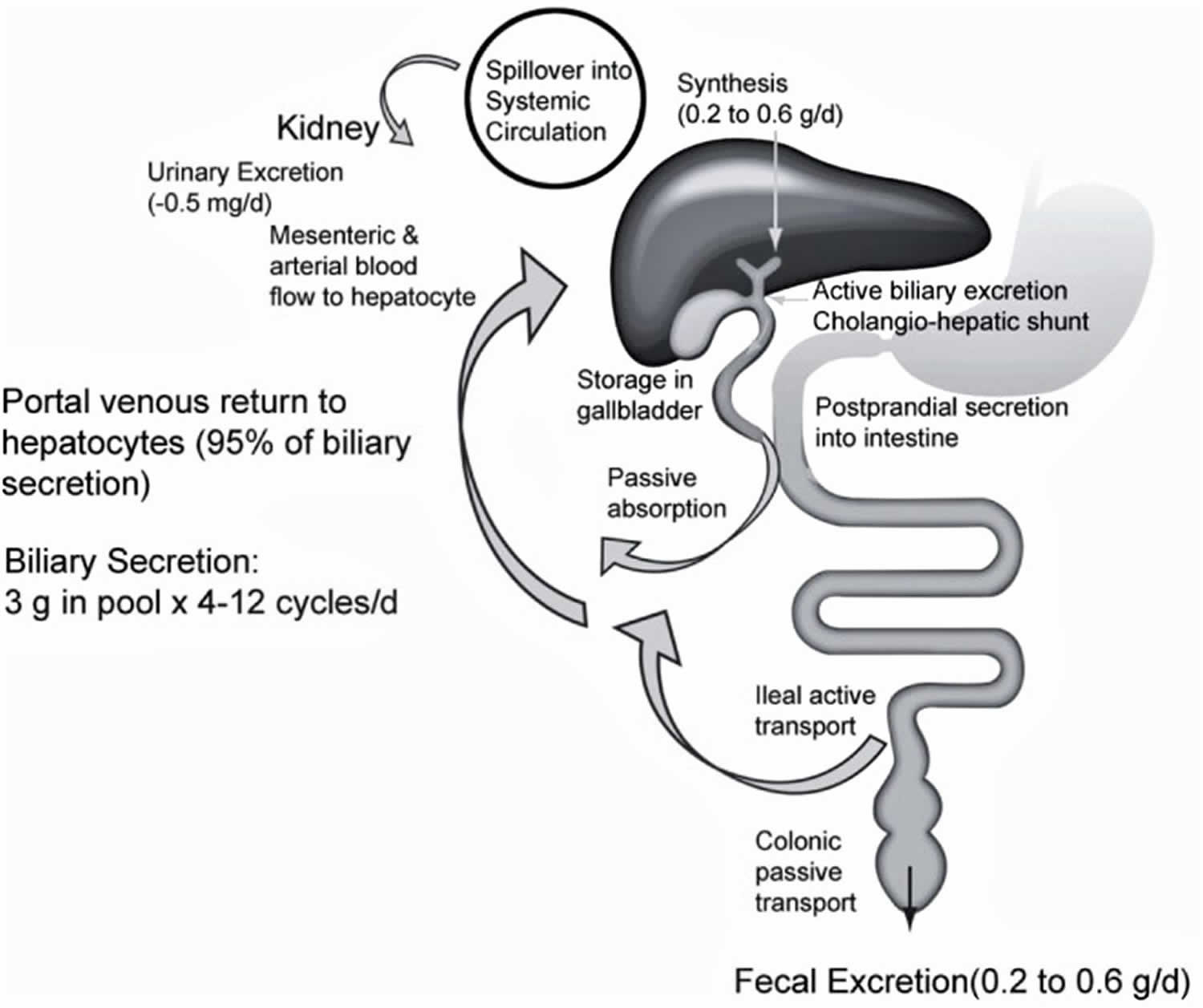
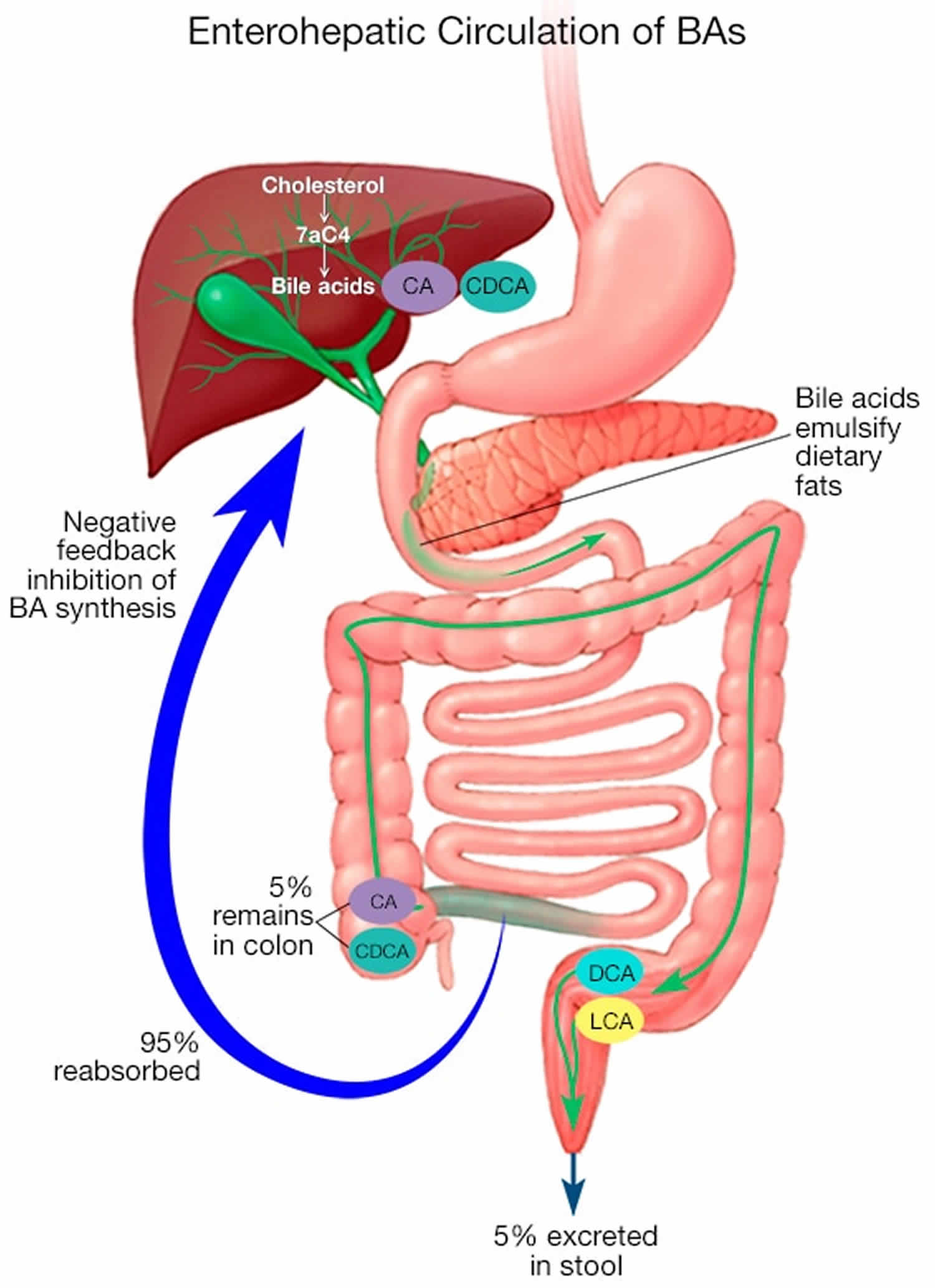
Bile acid production and the enterohepatic circulation
An estimated 0.5 g of bile acids are synthesized in the liver per day 14. The total bile acid pool is approximately 3 g, of which 95% is reclaimed from the ileum and a small amount of unconjugated bile acids is recaptured in the colon via passive nonionic diffusion 15. This cycle is repeated four to 12 times per day, resulting in an estimated daily loss of 0.2 g/day to 0.6 g/day in the feces, which must be replaced by new bile acid synthesis in hepatocytes 14.
The enterohepatic circulation of bile acids was first described by Small et al 16 four decades ago (Figure 1). Primary bile acids, principally cholic acid and chenodeoxycholic acid, are synthesized from cholesterol in the liver, conjugated with glycine or taurine to increase their water solubility and secreted to bile. Secondary bile acids, primarily deoxycholic acid and lithocholic acid, are derived from primary bile acids as a result of modifications (e.g., deconjugation, 7-dehydroxylation) by intestinal bacteria. These modifications increase passive absorption of secondary bile acids in the colon.
The main pathway for cholesterol conversion to cholic acid and chenodeoxycholic acid is the neutral pathway, in which the rate-limiting enzyme is the cytochrome P450 enzyme cholesterol 7α-hydroxylase (CYP7A1) 17. In the alternative (acidic) pathway, 27-hydroxylation of bile acid intermediates of the CYP7A1 pathway primarily results in chenodeoxycholic acid synthesis; this pathway accounts for <20% of total bile acid production 18. Other minor pathways involve cholesterol 25-hydroxylase, which is not part of the CYP450 system; and cholesterol 24-hydroxylase (CYP46), which converts 24S-cholesterol in the brain to bile acids 17.
Approximately 95% of primary bile acids are reabsorbed by the distal ileum through active uptake by the apical sodium-dependent bile acid transporter, returned to the liver via the portal circulation and taken up by hepatocytes. A small percentage of bile acids entering the colon can be passively absorbed, resulting in an overall net loss of 1% to 3% 19. The conservation of the bile acid pool is altered by more rapid intestinal transit and changes in gut flora due to diet, medications or other factors.
Cholesterol and bile acid levels are tightly regulated. Of particular interest are the liver X receptor and the farnesoid X receptor (FXR), both of which act as transcription factors regulating enzyme expression. The dimerized liver X receptor/retinoid X receptor (RXR) binds to oxidized cholesterol metabolites and induces the expression of CYP7A1, resulting in increased bile acid synthesis 20.
Bile acid production is regulated by farnesoid X receptor (FXR), which is expressed primarily in ileal enterocytes and hepatocytes. Bile acids activate FXR, which forms a dimerized FXR/retinoid X receptor (RXR) complex. In the liver, farnesoid X receptor (FXR)/retinoid X receptor (RXR) downregulates CYP7A1 expression, resulting in decreased bile acid synthesis and increased expression of the bile salt export pump, and downregulates CYP8B1, which is necessary for cholic acid synthesis 21. The result is a decrease in bile acid synthesis and uptake, and increased export to bile 20. In enterocytes, FXR/RXR acts on apical sodium-dependent bile acid transporter to reduce ileal uptake of bile acids 22. High intracellular bile acid levels in enterocytes also stimulate the release of fibroblast growth factor 19 (FGF19), which feeds back to the FGF receptor-4 (FGFR4) and its coreceptor Klothoβ on hepatocytes to downregulate CYP7A1 and reduce bile acid production 23. This decreases intestinal bile acid absorption and prevents the intracellular accumulation of bile acids. Thus, bile acid production is regulated through negative feedback mechanisms in the liver and remotely in the ileum.
The composition of the bile acid pool is influenced by various factors. The principal constituents are the primary bile acids (cholic acid, chenodeoxycholic acid) and the secondary bile acid deoxycholic acid; deoxycholic acid accumulates in the bile pool because 7-dehydroxylation cannot be reversed 20. Deoxycholic acid formation from cholic acid is increased by diet (eg, high fat) and other factors that slow colonic transit times 20, as well as increased Gram-positive anaerobes and 7-alpha-dehydroxylase activity 24. Absorption and bioavailability of deoxycholic acid are influenced by colonic transit time and pH in the distal colon 24.
Diets high in taurine (e.g., seafood), or high in fat or low in fiber will increase the amount of taurine-conjugated bile acids 25. The apical sodium-dependent bile acid transporter is also more effective at transporting dihydroxy bile acids (ie, deoxycholic acid, chenodeoxycholic acid) 22, which influence the bile acid pool.
Medications also play a role. Glucocorticoids upregulate apical sodium-dependent bile acid transporter 26, suggesting an alternative mechanism of symptom control in patients with inflammatory bowel disease. Cholestyramine has been shown to preferentially reduce dihydroxy (chenodeoxycholic acid acid, deoxycholic acid) bile acids (eg, cholic acid) and reduce the secondary bile acid pool 27. Cholestyramine also elevates the ratio of glycine- versus taurine-conjugated bile acids in bile. Because glycine conjugates are more subject to passive absorption, this may be an alternative mechanism by which cholestyramine reduces malabsorption 27.
Some bile acids (eg, cholic acid, ursodeoxycholic acid) do not appear to contribute to diarrhea 20. Dihydroxy bile acids (eg, deoxycholic acid, chenodeoxycholic acid) are more active, causing mucosal damage and demonstrating prosecretory effects in the colon 28.
Figure 1. Enterohepatic circulation of bile acids
Abbreviations: BA = bile acid; CA = cholic acid; CDCA = chenodeoxycholic acid; DCA = deoxycholic acid; LCA = lithocholic acid
[Source 6 ]Bile acid malabsorption investigations
Traditional investigations of bile acid malabsorption, such as direct testing of bile acid content in fecal samples 29 or 14C cholylglycine testing of 14C in expired air and stool, are difficult and unpleasant to perform 30. Another method to assess bile acid malabsorption is 23-seleno-25-homo-tauro-cholic acid (SeHCAT) testing (sensitivity >80%, specificity >98%) 31, in which 23-selena-25-homo-tauro-cholic acid is radiolabelled with 75Selenium homotaurocholic acid 32. This orally administered synthetic conjugated bile acid is secreted in bile, reabsorbed in the terminal ileum and resecreted. A noncollimated gamma camera measures abdominal radioactivity on day 7. Early studies indicated that retention of <12% of 23-selena-25-homotaurocholic acid was abnormal 33. A cut-off value <10% to 15% retention at day 7 is now generally established. SeHCAT (23-seleno-25-homo-tauro-cholic acid) testing has proven invaluable in the research setting, but is not routinely available in practice. This is unfortunate because the cost of the test is comparable with other, more routine, studies. SeHCAT costs $250 per capsule while an octreotide scan costs $1,028 per dose, and a 99m Tc-methylene diphosphonate bone scan costs $28 6. SeHCAT values are stable during long-term follow-up in patients with chronic diarrhea, suggesting that repeat testing is not required 34.
Determining the serum levels of 7-α-OH-4-cholesten-3-one (C4), which are markedly elevated when bile acid synthesis is increased 35, is a potentially useful measure but is not widely used at present; further standardization is needed 36. ELISA of serum fibroblast growth factor 19 (FGF19) levels, which are inversely correlated with 7-α-OH-4-cholesten-3-one (C4) levels, has been proposed 13 but is not generally available.
It should be noted that pathophysiological mechanisms other than bile acid malabsorption may contribute to diarrhea in some patients (e.g., postcholecystectomy) with abnormal SeHCAT or C4 findings 37, and that abnormal SeHCAT/C4 may occur in patients without clinically relevant symptoms. The association among SeHCAT, bile acid malabsorption and symptom frequency/severity requires further study.
A practical alternative to SeHCAT/C4 testing of bile acid malabsorption in patients with chronic diarrhea is to use a bile acid sequestering agent, which binds with high affinity to organic anions such as bile acids. American Gastroenterology Association guidelines recommend an empirical trial with an agent, such as cholestyramine, to diagnose bile acid malabsorption 38. British Society of Gastroenterology guidelines state that in the absence of diagnostic tests, an empirical trial of cholestyramine can be used 39, with the caveat that this approach has not been prospectively studied.
Bile acid malabsorption treatment
A large proportion of patients with severe bile acid malabsorption (SeHCAT <5%) will respond to an empirical trial of cholestyramine 6. In the case series reported by Nyhlin et al 40, response rates were 88% in resected Crohn’s disease and 28% in unresected Crohn’s disease. A total of 37 of 40 patients with severe bile acid malabsorption (all types) responded to cholestyramine 1 g/day to 8 g/day in the series by Ford et al 41. A large series demonstrated a response in 71% of patients taking cholestyramine; treatment with a bile acid sequestering agent was effective regardless of bile acid malabsorption type 38.
In addition, a substantial proportion of patients with diarrhea-predominant irritable bowel syndrome (IBS-D) will respond to cholestyramine. In their systematic review of 15 treatment studies, Wedlake et al 42 found that clinical response was correlated with bile acid malabsorption severity. The overall response to empirical therapy with cholestyramine was 96% for severe bile acid malabsorption (SeHCAT <5% of baseline), 80% for moderate or severe bile acid malabsorption (SeHCAT <10%), and 70% for any degree of bile acid malabsorption (SeHCAT <15%). Because one-quarter of diarrhea-predominant irritable bowel syndrome (IBS-D) patients have some degree of bile acid malabsorption, it would be expected that a large proportion of patients would respond to empirical use of cholestyramine. Wedlake et al 42 concluded that bile acid malabsorption is not a rare finding in diarrhea-predominant irritable bowel syndrome (IBS-D) patients and speculated that as many as 500,000 adults in the United Kingdom could benefit from therapeutic intervention for bile acid malabsorption. A similar number of Canadians would be expected to benefit from treatment due to the higher prevalence of diarrhea-predominant irritable bowel syndrome (IBS-D) in Canada 43.
A long-term follow-up (mean 99 months) of 14 patients with chronic diarrhea 44 found that seven of 14 experienced resolution of symptoms and no longer required cholestyramine. Of the remaining seven symptomatic patients, diarrhea was well controlled in five using cholestyramine and in two using antidiarrheal medications.
Cholestyramine is the only agent approved by Health Canada for the symptomatic control of bile acid-induced diarrhea due to short bowel syndrome to help reduce fecal bile acid loss 45. Cholestyramine powder is usually administered at a starting dose of 4 g/day, increased as needed to 4 g one to six times/day; in clinical practice, less frequent dosing (eg, 4 g twice/day) is often effective in relieving bile acid malabsorption-associated diarrhea. Lower doses (eg, 4 g twice/day) are generally used in patients with short-bowel syndrome. Adverse effects may include constipation, nausea, borborygmi, flatulence, bloating and abdominal pain.
The bile acid sequestering agents colestipol and colesevelam would also be expected to be clinically useful based on their mode of action; however, neither is indicated for the treatment of bile acid malabsorption-associated diarrhea in Canada 46. There are no published reports of colestipol in bile acid malabsorption. Dosing for hyperlipidemia is 2 g/day to 16 g/day administered either once-daily or in divided doses, or one to six packets (5 g/packet or 7.5 g/packet) of colestipol given once-daily or in divided doses. The most common adverse effects are constipation, abdominal pain/cramping, bloating/flatulence, heartburn, diarrhea and nausea/vomiting.
Colesevelam, a water-insoluble polymer, has been shown to have modest effects on intestinal transit time. A study randomly assigned 24 patients with diarrhea-predominant irritable bowel syndrome (IBS-D) to colesevelam 1.875 g twice/day or placebo for 12 to 14 days. Colesevelam eased stool passage and had a nonsignificant effect on 24 h colonic transit time. There was no effect on the number of bowel movements per day; however, there was a tendency to improved stool consistency 47. A retrospective study in cancer patients with bile acid malabsorption symptoms receiving colesevelam reported improvements in diarrhea (83%), urgency of defecation (74%), frequency of defecation (72%), steatorrhea (71%), abdominal pain (68%) and fecal incontinence (62%) 48. The optimal dosing of colesevelam for bile acid malabsorption has not been established. The dosing for hyperlipidemia is six 625 mg tablets/day (or three tablets twice per day), or one 3.75 g packet/day (or 1.875 g packet twice/day). The most common adverse effects are constipation, dyspepsia and nausea.
All bile acid sequestering agents have the potential to bind other drugs. Interactions may occur with drugs such as glyburide, glimepiride, glipizide, tetracycline, penicillin G, levothyroxine, cyclosporine, olmesartan, phenobarbital, warfarin, digitalis, and oral contraceptives containing ethinyl estradiol and norethindrone 45. Patients should generally be advised to take medications either 1 hour before or 4 hours to 6 hours after the bile acid sequestering agent 49.
In addition, bile sequestering agents may interfere with the absorption of fat-soluble vitamins 50. During long-term use, periodic monitoring of serum vitamin A and E levels and prothrombin time are advised.
Fat malabsorption
Fat malabsorption results from impaired digestion or absorption of dietary fats causing fatty stools (steatorrhea). There is currently no precise standardized definition of the amount of fat excretion necessary to make the diagnosis of steatorrhoea, however fat excretion of more than 6g per day is considered abnormal. Fat malabsorption can be caused by multiple diseases including cystic fibrosis, chronic pancreatitis, cholestatic liver disease, celiac disease, and inflammatory bowel disease 51. If untreated, fat malabsorption may result in malnutrition, growth failure, and deficiencies of fat-soluble vitamins A, E, D, and K with resultant skin and visual changes, neurologic deficits, osteoporosis/rickets and coagulopathy 52.
Fat in stool may be detected with the qualitative fecal fat test, which generally determines the presence or absence of excess fat. This is the simplest test for fecal fat and is performed by placing a suspension of treated or untreated stool onto a glass slide, adding a fat stain, and observing the number and size of fat globules that are present.
Currently the gold standard test to diagnose fat malabsorption remains the 72 hour fat balance method, which is based on the premise that fat intake minus fat output equals fat absorbed 53. A coefficient of fat absorption, calculated from the intake/output data, is the standard value used to indicate malabsorption. This test is very time consuming and logistically difficult as it requires a three to five day stool collection and a complete dietary intake record. Additionally, most patients with fat malabsorption have diarrhea and therefore accurate and complete collection is difficult, particularly in infants and children. These limitations make the 72 hour fat balance method impractical in the clinical setting and stress the need for a facile, accurate test of fat malabsorption. Despite previous attempts to develop simpler methods than the 72 hour fat balance method, none have proven to be easier than and as reliable as the gold standard.
Fat malabsorption causes
Fat malabsorption can result due to both digestive and absorptive disorders.
Normally dietary fat (a mixture of cholesterol and triglycerides) gets broken down partially in the stomach by a process called emulsification and then further in the duodenum (first segment of the small intestine) by certain pancreatic enzymes.
Bile (a yellow-green substance synthesised in the liver and stored in the gallbladder) also helps in the digestive and absorption process. This enters the duodenum and helps divide fat into very small globules coated with bile acids, called micelles. This aids the absorption and transport of the fats across the lining of the small intestine so the fats can enter the lymphatics.
Disruption in any of these processes can lead to malabsorption of fats which means dietary fat stays within the bowel to be later excreted in the stools in increased amounts.
Possible causes of steatorrhoea include:
- Celiac disease (gluten-sensitive enteropathy) – when foods containing gluten are eaten, a reaction occurs that damages the lining of the small intestine. This impairs absorption of fat and other substances
- Tropical sprue is the most common cause of steatorrhoea worldwide. Tropical sprue occurs in many parts of Asia and may be seen in travellers to these areas. The exact cause of this disorder is not known but it is thought to result in damage to intestinal villi which leads to malabsorption.
- Chronic pancreatitis – This causes a reduction in the production of the pancreatic enzymes which are required for adequate fat digestion.
- Liver disease and obstruction of bile ducts (e.g. Choledocholithiasis inhibit bile entering the duodenum so lipids cannot be digested or absorbed.
- Bacterial overgrowth – This can occur spontaneously in elderly patients or in patients with diverticular disease. The abnormal bacteria can breakdown bile salts.
- Parasites – e.g. Giardiasis.
- Pancreatic cancer – This can cause malabsorption by inhibiting pancreatic function or b obstruction of biliary outflow.
- Short bowel syndrome – Removal of segments of bowel inhibits the capacity for absorption.
- Crohn’s disease causes damage to the ileum (final portion of the small intestine) that has important roles in absorption of bile acids and other substances.
- Cystic fibrosis – This is a genetic condition that causes abnormal secretions in various organs throughout the body. In the pancreas, mucus plugs block some of the ducts and inhibit the secretion of digestive juices by the pancreas.
Fat malabsorption symptoms
You may notice the following symptoms if you suffer steatorrhoea:
- Foul-smelling feces.
- Bulky stool.
- Pale stools.
- Loose stools.
- Greasy stools.
Fat malabsorption diagnosis
Your doctor will take a thorough history regarding your symptoms and past medical history that may give the doctor a clue to the possible cause of your malabsorption. They will also perform a general examination and more specifically examine the abdomen.
When malabsorption occurs it is not uncommon for the doctor to perform several tests. These may include:
- Fecal fat determination – Stool samples are collected over three days whilst you follow a strict diet regarding fat content. The total fat content in the stool is measured and compared to normal values
- Spot stool sample – The doctor can use special stains and techniques on a single stool sample to determine the likely fat content. This is much easier than the above method but not as reliable.
- Breath test – The amount of carbon dioxide in the breath is measured after you ingest a radio-labeled fat sample. This gives an indication of fat absorption.
- Imaging tests such as Upper gastrointestinal endoscopy and biopsy, Barium studies and Wireless capsule enteroscopy can help identify abnormalities in the intestinal tract that may be the cause of the malabsorption.
Fat malabsorption treatment
Treatment of fat malabsorption (steatorrhea) largely depends on the underlying cause. A gluten-free diet helps treat coeliac disease. Pancreatic enzyme supplements can be used in cases of pancreatic insufficiency and antibiotics are helpful if bacterial overgrowth is present. If inflammatory bowel disease is identified corticosteroids and other anti-inflammatory agents such as sulfasalazine are the treatments of choice. In addition, you may require nutritional supplements such as vitamins and minerals as absorption of these may be diminished.
Malabsorption symptoms
Symptoms of malabsorption are caused by the increased passage of unabsorbed nutrients through the digestive tract or by the nutritional deficiencies that result from inadequate absorption.
The most common symptom of malabsorption is:
- Chronic diarrhea
- In children, current weight or rate of weight gain is often much lower than that of other children of similar age and gender. This is called failure to thrive. The child may not grow and develop normally.
Possible signs and symptoms of chronic malabsorption include the following:
- Persistent abdominal pain and vomiting
- Frequent, loose, bulky, foul- smelling stools
- Increased susceptibility to infection
- Weight loss with the loss of fat and muscle
- Increase in bruises
- Bone fractures
- Dry, scaly skin rashes
- Personality changes
- Slowing of growth and weight gain (may not be noticeable for several months)
When there is inadequate absorption of fats in the digestive tract, stool is light-colored, soft, bulky, greasy, and unusually foul-smelling (such stool is called steatorrhea). The stool may float or stick to the side of the toilet bowl and may be difficult to flush away. The inadequate absorption of certain sugars can cause explosive diarrhea, abdominal bloating, and flatulence.
Malabsorption can cause deficiencies of all nutrients or selective deficiencies of proteins, fats, sugars, vitamins, or minerals. People with malabsorption usually lose weight or have difficulty maintaining their weight despite adequate consumption of food. Women may stop menstruating. The symptoms vary depending on the specific deficiencies. For example, a protein deficiency can cause swelling and accumulation of fluid (edema) anywhere throughout the body, dry skin, and hair loss. Anemia (caused by vitamin or iron deficiency) may cause fatigue and weakness.
Symptoms of nutrient deficiencies:
- Calcium: Bone pain and deformities, greater likelihood of fractures (due to bone thinning or osteoporosis), muscle spasms, tooth discoloration, and greater susceptibility to painful tooth decay
- Folate (folic acid): Fatigue and weakness (due to anemia)
- Iron: Fatigue and weakness (due to anemia)
- Magnesium: Muscle spasms
- Niacin: Diarrhea, skin disorders, confusion (pellagra), and sore tongue
- Protein: Swelling (edema), usually in the legs; dry skin; and hair loss
- Vitamin A: Night blindness
- Vitamin B1 (Thiamin): Pins-and-needles sensation, especially in the feet, and heart failure
- Vitamin B2: Sore tongue and cracks at the edges of the mouth
- Vitamin B12: Fatigue and weakness (due to anemia), pins-and-needles sensation, and confusion
- Vitamin C: Weakness and bleeding gums
- Vitamin D: Bone thinning and bone pain
- Vitamin K: Tendency to bruise and bleed
Malabsorption diagnosis
A doctor suspects malabsorption when a person has chronic diarrhea, weight loss, anemia, and other signs of nutritional deficiencies. Malabsorption is less obvious and often more difficult to recognize in older people than in children.
Your health care provider will take you medical history and do a physical exam.
Your doctor will also order tests to confirm the diagnosis (such as blood and stool tests) and tests to diagnose the cause (such as biopsy and imaging).
Laboratory tests can help confirm the diagnosis:
- Tests to measure fat in stool
- Visual examination of stool
- Blood tests
A stool test that directly measures the amount of fat in stool that has been collected over 3 days is the most reliable one for diagnosing malabsorption of fat, which is present in almost all malabsorption disorders. A finding of more than 7 grams of fat in the stool daily is the hallmark of malabsorption. Also available are a few other tests that measure fat in the stool but do not require the 3-day collection of stool.
Stool samples are examined with the unaided eye as well as under the microscope. Undigested food fragments may mean that food passes through the intestine too rapidly. In a person with jaundice, stool with excess fat indicates decreased production or secretion of bile. Sometimes parasites or their eggs are seen under the microscope, suggesting that malabsorption is caused by a parasitic infection.
Blood tests and other laboratory tests can be done to detect malabsorption of other specific substances, such as lactose or vitamin B12.
Once a doctor confirms a person has a malabsorption disorder, tests are done to diagnose the cause:
- Biopsy
- Imaging tests
- Pancreatic function tests
A biopsy may be needed to detect abnormalities in the lining of the small intestine. The tissue is removed through an endoscope (a flexible viewing tube equipped with a light source and a camera through which a small clipper can be inserted) passed through the mouth and into the small intestine.
Imaging tests, such as video capsule endoscopy, computed tomography, or barium x-rays, and other diagnostic tests (culture of digestive bacteria, certain blood tests, or breath tests) may also be done.
Pancreatic function tests are done if the doctor thinks that the cause of malabsorption may be the insufficient production of digestive enzymes by the pancreas. However, some of these tests are complex, time-consuming, and invasive. In one test, a tube is passed through the mouth and guided into the small intestine, where intestinal fluids containing pancreatic secretions can be collected and measured. In another test, the person swallows a substance that requires pancreatic enzymes for its digestion. The products of digestion are then measured in the urine. Recently, doctors have been doing simpler and easier tests that measure levels of certain pancreatic enzymes in the stool.
Malabsorption treatment
Treatment depends on the cause and is aimed at relieving symptoms and ensuring the body receives enough nutrients.
A high-calorie diet may be tried. It should supply:
- Key vitamins and minerals, such as iron, folic acid, and vitamin B12
- Enough carbohydrates, proteins, and fats
If needed, injections of some vitamins and minerals or special growth factors will be given. Those with damage to the pancreas may need to take pancreatic enzymes. Your provider will prescribe these if necessary.
Medicines to slow down the normal movement of the intestine can be tried. This may allow food to remain in the intestine longer
If the body is not able to absorb enough nutrients, total parenteral nutrition (TPN) is tried. It will help you or your child get nutrition from a special formula through a vein in the body. Your provider will select the right amount of calories and total parenteral nutrition (TPN) solution. Sometimes, you can also eat and drink while getting nutrition from total parenteral nutrition (TPN).
References- Fish EM, Bhimji SS. Physiology, Small Bowel. [Updated 2018 Oct 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532263
- American Gastroenterological Association medical position statement: guidelines for the evaluation and management of chronic diarrhea. Gastroenterology. 1999 Jun;116(6):1461-3.
- Mustalahti K, Collin P, Sievänen H, Salmi J, Mäki M. Osteopenia in patients with clinically silent coeliac disease warrants screening. Lancet. 1999 Aug 28;354(9180):744-5.
- Anatomy and Physiology of the Small Bowel. Gastrointest Endosc Clin N Am. 2017 Jan;27(1):1-13. doi: 10.1016/j.giec.2016.08.001. https://www.ncbi.nlm.nih.gov/pubmed/27908510
- Thomas PD, Forbes A, Green J, et al. Guidelines for the investigation of chronic diarrhoea, 2nd edn. Gut. 2003;52(Suppl V):v1–v15
- Barkun AN, Love J, Gould M, Pluta H, Steinhart H. Bile acid malabsorption in chronic diarrhea: pathophysiology and treatment. Can J Gastroenterol. 2013;27(11):653-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3816948/
- Pattni S, Walters JRF. Recent advances in the understanding of bile acid malabsorption. Br Med Bull. 2009;92:79–93.
- McJunkin B, Fromm H, Sarva RP, Amin P. Factors in the mechanism of diarrhea in bile acid malabsorption: Fecal pH – a key determinant. Gastroenterology. 1981;80:1454–1464.
- Törnblom H, Van Oudenhove L, Sadik R, Abrahamsson H, Tack J, Simrén M. Colonic transit time and IBS symptoms: What’s the link? Am J Gastroenterol. 2012;107:754–60.
- Sciarretta G, Fagioli G, Furno A, et al. 75Se HCAT test in the detection of bile acid malabsorption in functional diarrhoea and its correlation with small bowel transit. Gut. 1987;28:970–5.
- Wong BS, Camilleri M, Carlson PJ, et al. A Klothoβ variant mediates protein stability and associates with colon transit in irritable bowel syndrome with diarrhea. Gastroenterology. 2011;140:1934–42.
- Wong BS, Camilleri M, Carlson P, et al. Increased bile acid biosynthesis is associated with irritable bowel syndrome with diarrhea. Clin Gastroenterol Hepatol. 2012;10:1009–15.
- Walters JR, Tasleem AM, Omer OS, Brydon WG, Dew T, le Roux CW. A new mechanism for bile acid diarrhea: Defective feedback inhibition of bile acid biosynthesis. Clin Gastroenterol Hepatol. 2009;7:1189–94.
- Chiang JY. Bile acids: Regulation of synthesis. J Lipid Res. 2009;50:1955–66.
- Mekhjian HS, Phillips SF, Hofmann AF. Colonic absorption of unconjugated bile acids: Perfusion studies in man. Dig Dis Sci. 1979;24:545–50.
- Small DM, Dowling RH, Redinger RN. The enterohepatic circulation of bile salts. Arch Intern Med. 1972;130:552–73.
- Redinger RN. The role of the enterohepatic circulation of bile salts and nuclear hormone receptors in the regulation of cholesterol homeostasis: Bile salts as ligands for nuclear hormone receptors. Can J Gastroenterol. 2003;17:265–71.
- Fuchs M. Bile acid regulation of hepatic physiology: III. Regulation of bile acid synthesis: Past progress and future challenges. Am J Physiol Gastrointest Liver Physiol. 2003;284:G551–7
- Swell L, Gustafsson J, Schwartz CC, Halloran LG, Danielsson H, Vlahcevic ZR. An in vivo evaluation of the quantitative significance of several potential pathways to cholic and chenodeoxycholic acids from cholesterol in man. J Lipid Res. 1980;21:455–66.
- Martínez-Augustin O, Sánchez de Medina F. Intestinal bile acid physiology and pathophysiology. World J Gastroenterol. 2008;14:5630–40.
- Kim I, Ahn SH, Inagaki T, et al. Differential regulation of bile acid homeostasis by the farnesoid X receptor in liver and intestine. J Lipid Res. 2007;48:2664–72.
- Craddock AL, Love MW, Daniel RW, et al. Expression and transport properties of the human ileal and renal sodium-dependent bile acid transporter. Am J Physiol. 1998;274:G157–69
- Zweers SJ, Booij KA, Komuta M, et al. The human gallbladder secretes fibroblast growth factor 19 into bile: Towards defining the role of fibroblast growth factor 19 in the enterobiliary tract. Hepatology. 2012;55:575–83.
- Thomas LA, Veysey MJ, Bathgate T, et al. Mechanism for the transit-induced increase in colonic deoxycholic acid formation in cholesterol cholelithiasis. Gastroenterology. 2000;119:806–15.
- Stadler J, Stern HS, Yeung KS, et al. Effect of high fat consumption on cell proliferation activity of colorectal mucosa and on soluble faecal bile acids. Gut. 1988;29:1326–31
- Jung D, Fantin AC, Scheurer U, Fried M, Kullak-Ublick GA. Human ileal bile acid transporter gene ASBT (SLC10A2) is transactivated by the glucocorticoid receptor. Gut. 2004;53:78–84
- Garbutt JT, Kenney TJ. Effect of cholestyramine on bile acid metabolism in normal man. J Clin Invest. 1972;51:2781–9
- Bajor A, Gillberg PG, Abrahamsson H. Bile acids: Short and long term effects in the intestine. Scand J Gastroenterol. 2010;45:645–64
- Porter JL, Fordtran JS, Santa Ana CA, et al. A simple and accurate enzymatic method for measurement of total fecal bile acids in patients with severe fat malabsorption. J Lab Clin Med. 2003;141:411–8.
- Fromm H, Hofmann AF. Breath test for altered bile acid metabolism. Lancet. 1971;ii:621–5.
- Balzer K, Breuer N, Quebe-Fehling E. [Postprandial serum bile acid level and 75SeHCAT retention in diagnosis of bile acid malabsorption syndrome. A comparative study] Med Klin (Munich) 1993;88(Suppl 1):23–8.
- Boyd GS, Merrick MV, Monks R, et al. Se-75-labelled bile acid analogs, new radiopharmaceuticals for investigating the enterohepatic circulation. J Nuci Med. 1981;22:720–5.
- Nyhlin H, Merrick MV, Eastwood MA, Brydon WG. Evaluation of ileal function using 23-selena-25-homotaurocholate, a γ-labelled conjugated bile acid. Gastroenterology. 1983;84:63–8.
- Bajor A, Kilander A, Sjövall H, Rudling M, Ung KA. The bile acid turnover rate assessed with the (75)SeHCAT test is stable in chronic diarrhoea but slightly decreased in healthy subjects after a long period of time. Dig Dis Sci. 2008;53:2935–40.
- Gälman C, Arvidsson T, Angelin B, Rudling M. Monitoring hepatic cholesterol 7 alpha-hydroxylase activity by assay of the stable bile acid intermediate 7 alpha-hydroxy-4-cholesten-3-one in peripheral blood. J Lipid Res. 2003;44:859–66.
- Brydon WG, Culbert P, Kingstone K, et al. An evaluation of the use of serum 7-alpha-hydroxycholestenone as a diagnostic test of bile acid malabsorption causing watery diarrhea. Can J Gastroenterol. 2011;25:319–23.
- American Gastroenterological Association medical position statement: Guidelines for the evaluation and management of chronic diarrhea. Gastroenterology. 1999;116:1461–3.
- Borghede MK, Schlütter JM, Agnholt JS, Christensen LA, Gormsen LC, Dahlerup JF. Bile acid malabsorption investigated by selenium-75-homocholic acid taurine ((75)SeHCAT) scans: Causes and treatment responses to cholestyramine in 298 patients with chronic watery diarrhoea. Eur J Intern Med. 2011;22:e137–40.
- Thomas PD, Forbes A, Green J, et al. Guidelines for the investigation of chronic diarrhoea, 2nd edn. Gut. 2003;52(Suppl V):v1–v15.
- Nyhlin H, Merrick MV, Eastwood MA. Bile acid malabsorption in Crohn’s disease and indications for its assessment using SeHCAT. Gut. 1994;35:90–3.
- Ford GA, Preece JD, Davies IH, Wilkinson SP. Use of the SeHCAT test in the investigation of diarrhea. Postgrad Med J. 1992;68:272–6.
- Wedlake L, A’Hern R, Russell D, Thomas K, Walters JR, Andreyev HJ. Systematic review: The prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2009;30:707–17.
- Canadian Digestive Health Foundation Irritable bowel syndrome. http://cdhf.ca//
- Luman W, Williams AJ, Merrick MV, Eastwood MA. Idiopathic bile acid malabsorption: Long-term outcome. Eur J Gastroenterol Hepatol. 1995;7:641–5.
- Olestyr (cholestyramine) Product Monograph. Pendopharm, Division of Pharmascience Inc; Feb 20, 2012.
- Colestid (colestipol) Product Monograph. Pfizer Canada Inc; Nov 6, 2012.
- Odunsi-Shiyanbade ST, Camilleri M, McKinzie S, et al. Effects of chenodeoxycholate and a bile acid sequestrant, colesevelam, on intestinal transit and bowel function. Clin Gastroenterol Hepatol. 2010;8:159–65.
- Wedlake L, Thomas K, Lalji A, Anagnostopoulos C, Andreyev HJ. Effectiveness and tolerability of colesevelam hydrochloride for bile-acid malabsorption in patients with cancer: A retrospective chart review and patient questionnaire. Clin Ther. 2009;31:2549–58.
- Walters JRF, Pattni SS. Managing bile acid diarrhea. Ther Adv Gastroenterol. 2010;3:349–57.
- Jacobson TA, Armani A, McKenney JM, Guyton JR. Safety considerations with gastrointestinally active lipid-lowering drugs. Am J Cardiol. 2007;99:47C–55C.
- Schmitz J. Maldigestion and Malabsorption. In: Walker WA, et al., editors. Pediatric Gastrointestinal Disease. New York: Mosby; 2000. pp. 48–55.
- Dorsey J, Buckley D, Summer S, et al. Fat malabsorption in cystic fibrosis: comparison of quantitative fat assay and a novel assay using fecal lauric/behenic acid. J Pediatr Gastroenterol Nutr. 2010;50(4):441-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2847657/
- Van de Kamer JH, Huinink H, Weyers HA. Rapid method for the determination of fat in feces. J Biol Chem. 1949;177:349–355.