What is mesenteric ischemia
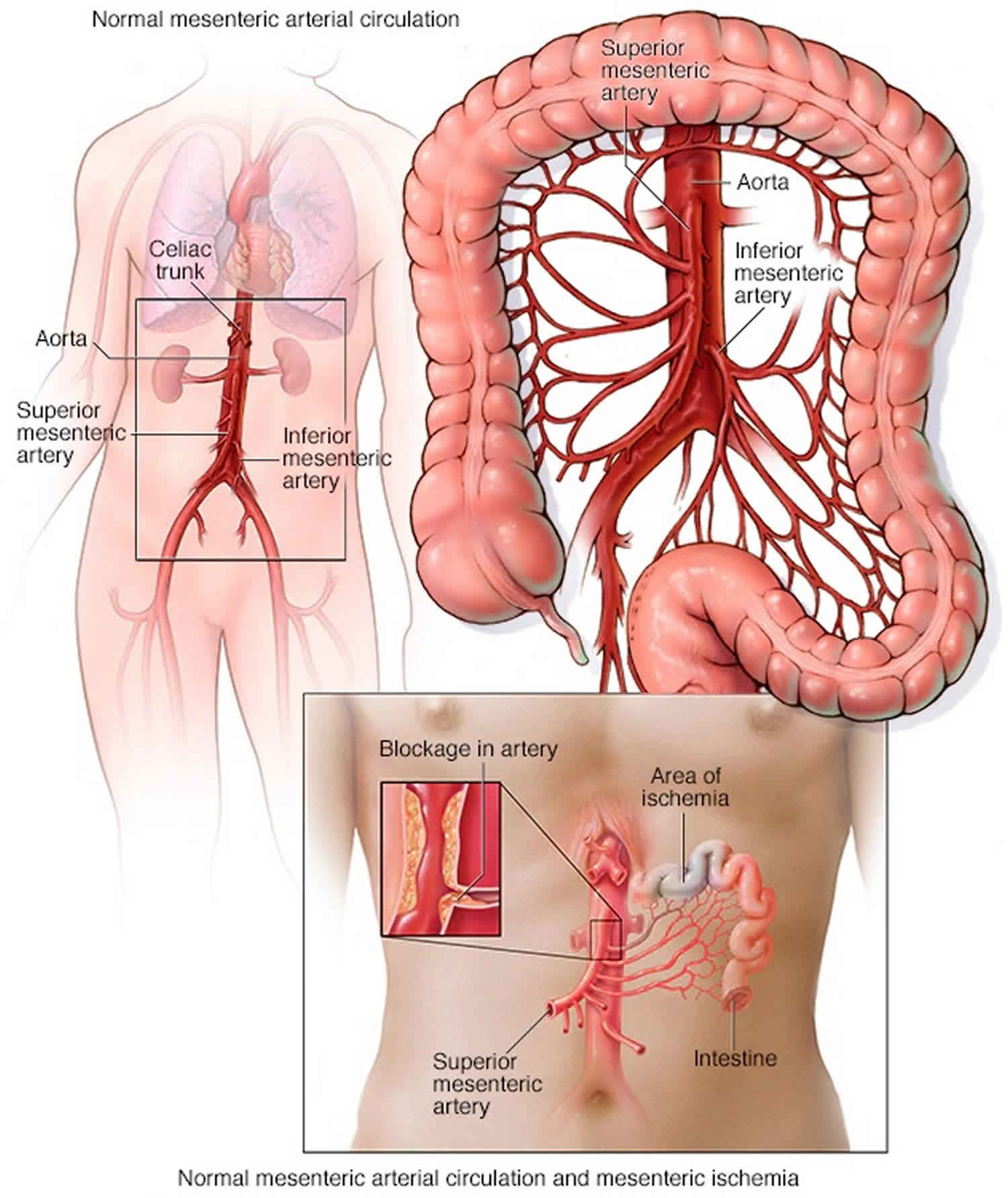
Mesenteric ischemia is sudden blockage of blood flow to part of your small and large intestines, which may lead to gangrene and perforation (puncture). Mesenteric ischemia occurs when there is a narrowing or blockage of one or more of the three mesenteric arteries that supply the small and large intestines. Sudden loss of blood flow to the intestines (acute mesenteric ischemia) from a blood clot requires immediate surgery. Mesenteric ischemia that develops over time (chronic mesenteric ischemia) is treated with angioplasty or open surgery. Untreated, chronic mesenteric ischemia can become acute or lead to severe weight loss and malnutrition.
Figure 1. Mesenteric artery
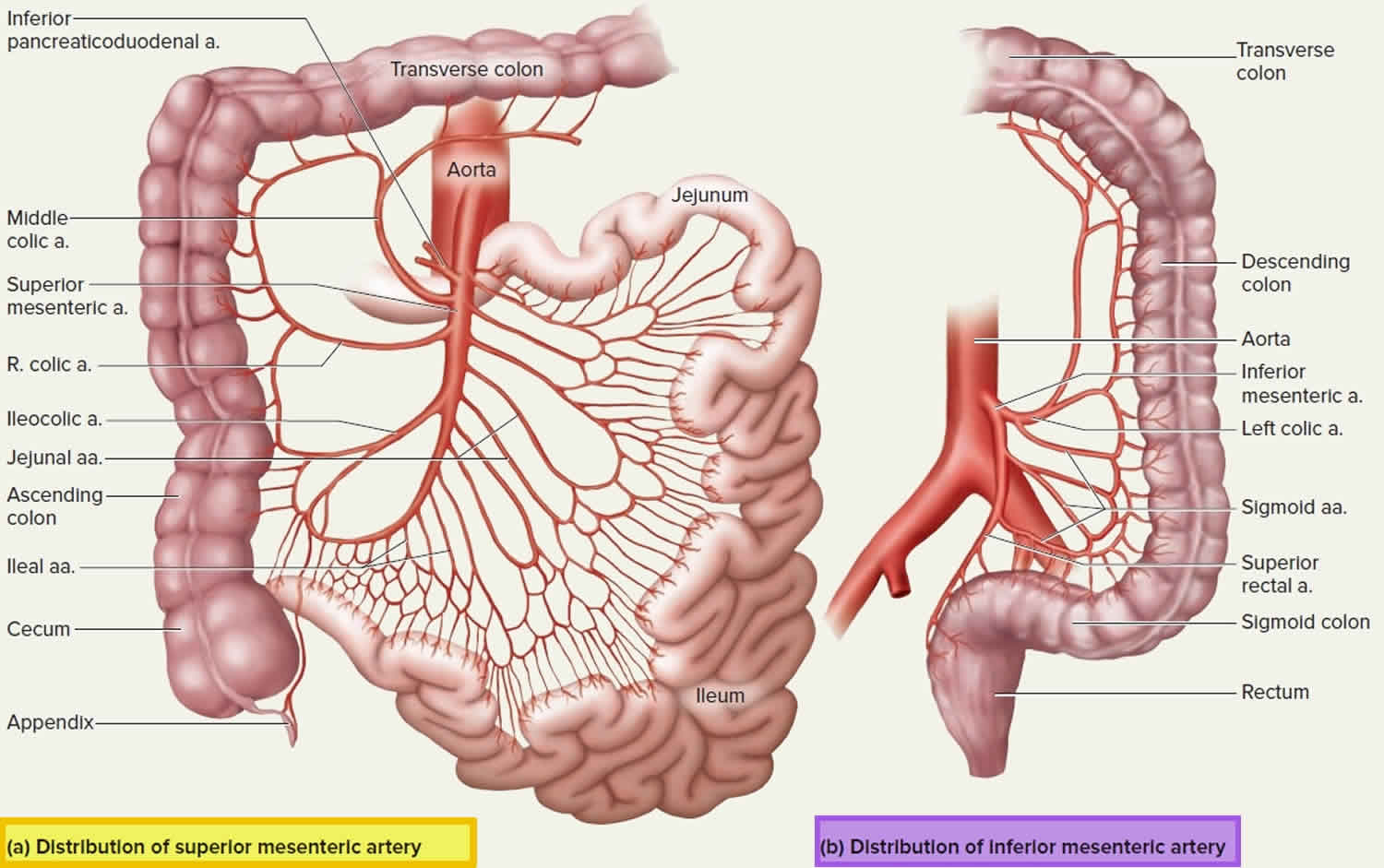
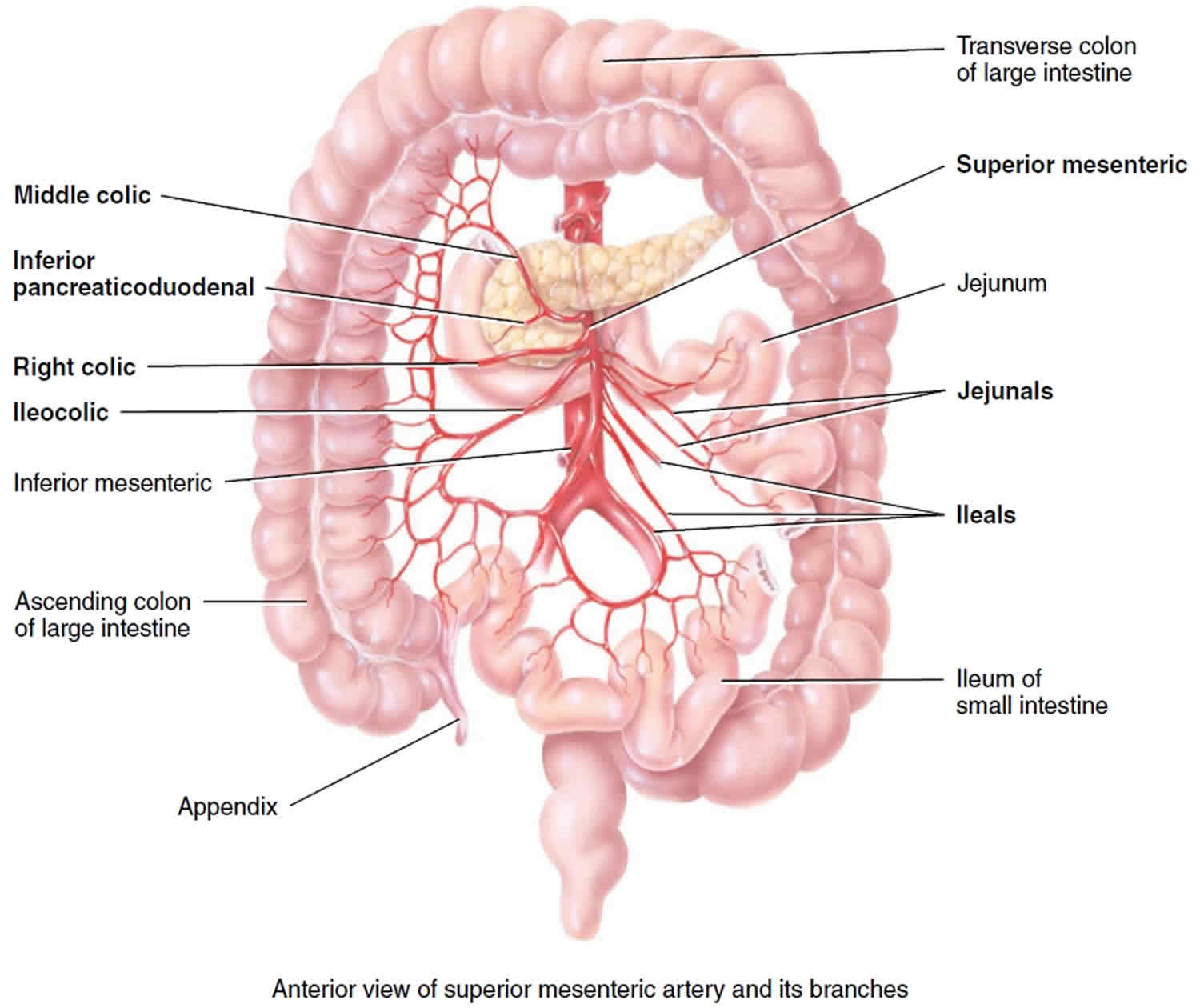
Figure 2. Superior mesenteric artery and its branches
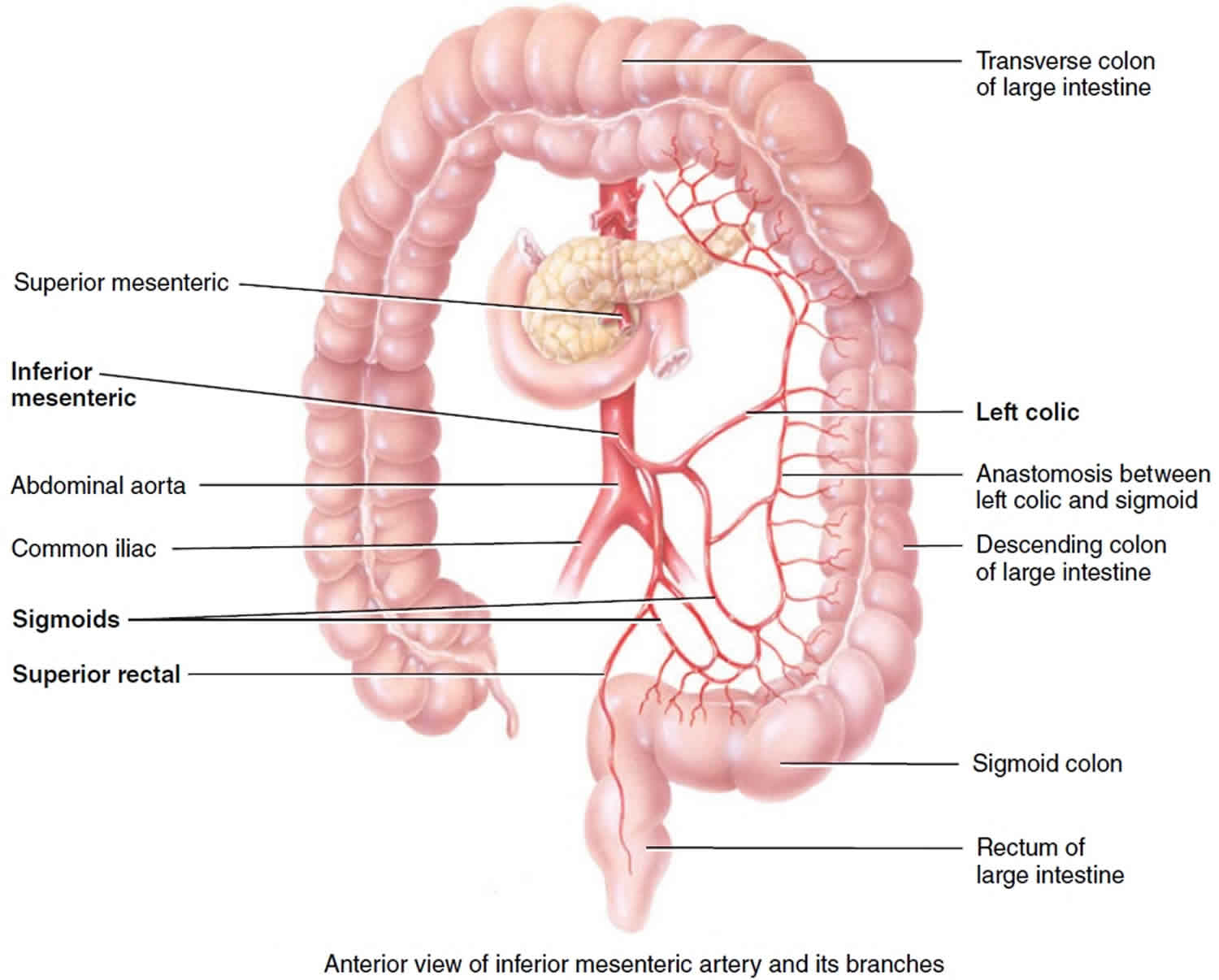
Figure 3. Inferior mesenteric artery and its branches
Mesenteric ischemia causes
The arteries that supply blood to the intestines run directly from the aorta. The aorta is the main artery from your heart. Hardening of the arteries occurs when fat, cholesterol, and other substances build up in the walls of arteries. This is more common in smokers and in people with high blood pressure or high blood cholesterol. This narrows the blood vessels and reduces blood flow to the intestines. Like every other part of the body, blood brings oxygen to the intestines. When the oxygen supply is slowed, symptoms may occur.
Three major vessels serve the abdominal contents:
- Celiac trunk: Supplies the esophagus, stomach, proximal duodenum, liver, gallbladder, pancreas, and spleen
- Superior mesenteric artery (SMA): Supplies the distal duodenum, jejunum, ileum, and colon to the splenic flexure (see Figures 1 and 2)
- Inferior mesenteric artery (IMA): Supplies the descending colon, sigmoid colon, and rectum (see Figures 1 and 3)
Collateral vessels are abundant in the stomach, duodenum, and rectum; these areas rarely develop ischemia. The splenic flexure is a watershed between the superior mesenteric artery and inferior mesenteric artery and is at particular risk of ischemia. Note that acute mesenteric ischemia is distinct from ischemic colitis, which involves only small vessels and causes mainly mucosal necrosis and bleeding.
Mesenteric blood flow may be disrupted on either the venous or arterial sides. In general, patients > 50 are at greatest risk and have the types of occlusions and risk factors. However, many patients have no identifiable risk factors.
The blood supply to the intestines may be suddenly blocked by a blood clot (embolus). The clots most often come from the heart or aorta. These clots are more commonly seen in people with abnormal heart rhythm.
Both acute and chronic mesenteric ischemia are caused by a decrease in blood flow to your intestines. Acute mesenteric ischemia is most commonly caused by a blood clot in the main mesenteric artery. The blood clot often originates in the heart. The chronic form is most commonly caused by a buildup of plaque that narrows the mesenteric arteries.
Mesenteric ischemia has multiple causes. The most common are:
- Arterial embolus (> 40%): Arterial embolism is a blood clot or piece of atherosclerotic plaque material (the buildup of cholesterol and other fatty materials in an artery) that travels from its origin in the heart or aorta to lodge in the smaller arteries (in this case those of the intestines).
- Arterial thrombosis (30%): Arterial thrombus is a blood clot that forms spontaneously in the arteries or veins, including those of the intestines, blocking flow.
- Venous thrombosis (15%)
- Nonocclusive ischemia (15%): Sometimes flow is not blocked completely but is simply too low because of low heart output (as in heart failure or shock) or because certain drugs (such as cocaine) narrow the blood vessels. In general, people older than 50 years are at greatest risk.
Blockage of blood flow for more than 6 hours can cause the affected area of intestine to die, allowing intestinal bacteria to invade the person’s system. Shock, organ failure, and death are likely if intestinal death occurs.
Risk factors for mesenteric ischemia
- Arterial embolus (> 40%): Coronary artery disease, heart failure, valvular heart disease, atrial fibrillation, history of arterial emboli
- Arterial thrombosis (30%): Generalized atherosclerosis
- Venous thrombosis (15%): Hypercoagulable states, inflammatory conditions (eg, pancreatitis, diverticulitis), trauma, heart failure, renal failure, portal hypertension, decompression sickness
- Nonocclusive ischemia (15%): Low-flow states (eg, heart failure, shock, cardiopulmonary bypass), splanchnic vasoconstriction (eg, vasopressors, cocaine)
Mesenteric ischemia prevention
The following lifestyle changes can reduce your risk for narrowing of the arteries:
- Get regular exercise.
- Follow a healthy diet.
- Get heart rhythm problems treated.
- Keep your blood cholesterol and blood sugar under control.
- Quit smoking.
Mesenteric ischemia symptoms
At first, the person has severe abdominal pain, usually developing suddenly, but only mild pain occurs when the doctor presses on the abdomen during the examination (unlike in disorders such as appendicitis or diverticulitis, in which pressing makes the pain much worse). Later, as the intestine starts to die, the doctor’s examination of the abdomen causes more severe pain.
Acute mesenteric ischemia symptoms
Symptoms of sudden acute mesenteric ischemia due to a traveling blood clot include:
- Sudden severe abdominal pain
- Diarrhea
- Nausea and vomiting
- Urgent need to have a bowel movement
- Fever
Chronic mesenteric ischemia symptoms
Symptoms caused by chronic mesenteric ischemia due to gradual hardening of the mesenteric arteries include:
- Abdominal pain that starts about 30 minutes after eating
- Pain that worsens over an hour
- Pain that goes away within one to three hours
- Diarrhea
Mesenteric ischemia complications
If not treated promptly, acute mesenteric ischemia can lead to:
- Sepsis. This potentially life-threatening condition is caused by the body releasing chemicals into the bloodstream to fight infection. In sepsis, the body overreacts to the chemicals, triggering changes that can lead to multiple organ failure.
- Irreversible bowel damage. Insufficient blood flow to the bowel can cause parts of the bowel to die.
- Death. Both of the above complications can lead to death.
People with chronic mesenteric ischemia can develop:
- Fear of eating. This occurs because of the after-meal pain associated with the condition.
- Unintentional weight loss. This can occur as a result of the fear of eating.
- Acute-on-chronic mesenteric ischemia. Symptoms of chronic mesenteric ischemia can progress, leading to the acute form of the condition.
Mesenteric ischemia diagnosis
If the person has typical symptoms of acute mesenteric ischemia or if the abdomen is very tender, doctors usually take the person right to surgery.
If the diagnosis of acute mesenteric ischemia is not clear, doctors do CT angiography (a special CT scan using radiopaque dye injected in an arm vein to produce images of blood vessels) to look for swelling of the intestines or blockages in the arteries that supply blood to the intestines.
Mesenteric ischemia treatment
If mesenteric ischemia is diagnosed during surgery, the blood vessel blockage can sometimes be removed or bypassed, but other times the affected intestine must be removed.
If mesenteric ischemia is diagnosed during CT angiography, doctors may try to relieve the blockage in the blood vessels using angiography. In angiography, a small flexible tube (catheter) is threaded through the artery in the groin and into the arteries of the intestines. If a blockage is seen during angiography, sometimes it can be opened by injecting certain drugs, suctioning out a blood clot using a special angiography catheter, or inflating a small balloon within the artery to widen it and then placing a small tube or manufactured mesh (stent) to keep it open. If doctors cannot successfully open the blockage using these procedures, the person needs surgery to open the blockage or to remove the affected portion of the intestine.
After recovery, many people need to take a drug to help prevent blood clotting.
Mesenteric ischemia prognosis
If the doctor can make the diagnosis and begin treatment early, people usually recover well. People with acute mesenteric ischemia often do poorly because parts of the intestine may die before surgery can be done. This can be fatal. However, with prompt diagnosis and treatment, acute mesenteric ischemia can be treated successfully. The prognosis for chronic mesenteric ischemia is good after a successful surgery. However, it is important to make lifestyle changes to prevent hardening of the arteries from getting worse.
If the diagnosis is not made or if treatment is not started until some of the affected intestine has died, 70 to 90% of people die. A person cannot survive if almost all the small intestine dies or is removed.
People with hardening of the arteries that supply the intestines often have the same problems in blood vessels that supply the heart, brain, kidneys, or legs.