What is methylene blue
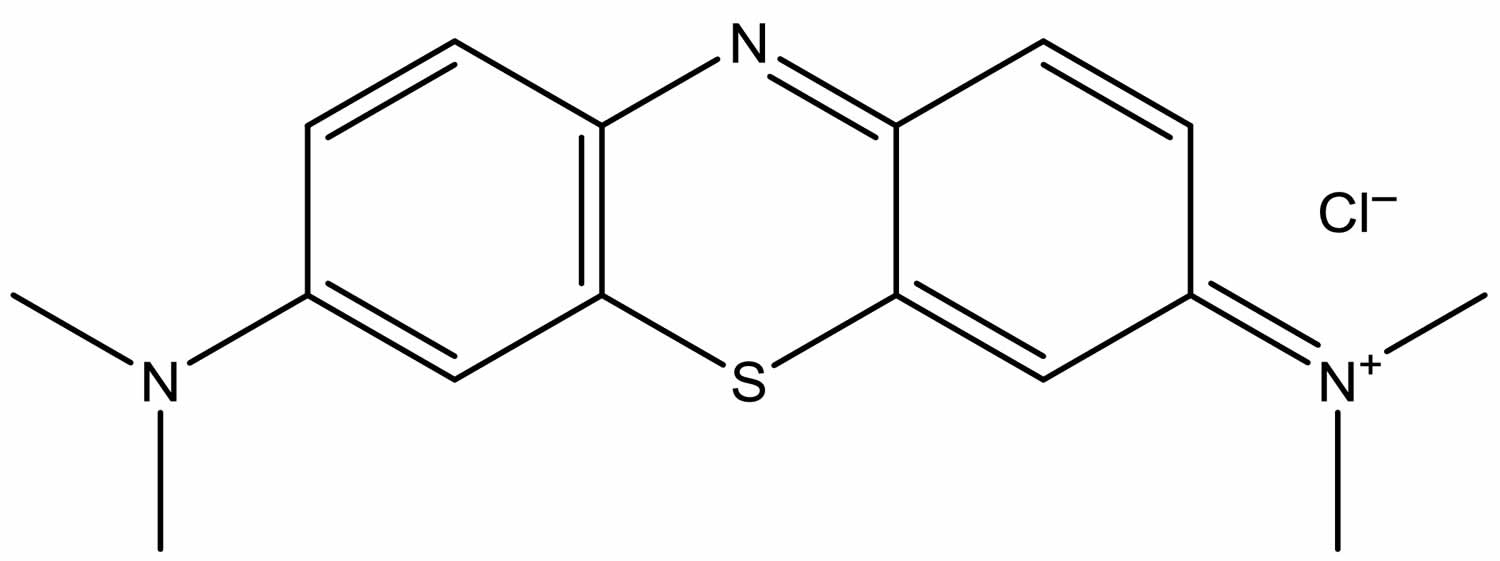
Methylene blue (C16H18ClN3S), also known as methylthioninium chloride, is a medication and is a synthetic basic dye consisting of dark green crystals or crystalline powder, having a bronze-like luster. Methylene blue in water or alcohol have a deep blue color. Methylene blue is used as a bacteriologic stain and as an indicator. Methylene blue stains to negatively charged cell components like nucleic acids; when administered in the lymphatic bed of a tumor during oncologic surgery, methylene blue may stain lymph nodes draining from the tumor, thereby aiding in the visual localization of tumor sentinel lymph nodes. As a medication, when administered intravenously in low doses, methylene blue may convert methemoglobin to hemoglobin and it is mainly used to treat methemoglobinemia 1. Specifically, methylene blue is used to treat methemoglobin levels that are greater than 30% or in which there are symptoms despite oxygen therapy. Methylene blue is typically given by injection into a vein. Methylene blue inhibits guanylate cyclase and has been used to treat cyanide poisoning, but this use is no longer recommended.
Methylene blue is a diaminophenothiazine drug that at low doses (0.5 – 4 mg/kg body weight) has neurometabolic-enhancing properties 2. Preclinical research with rodents has shown that at low doses, methylene blue is a metabolic and cognitive enhancer that improves brain oxygen consumption, brain glucose uptake, cerebral blood flow, fMRI responses and memory consolidation by induction of cytochrome oxidase, the respiratory enzyme found within nerve cells 2. By enhancing cytochrome oxidase activity, methylene blue increases oxygen consumption and amount of ATP available in neurons during memory consolidation. Although methylene blue has the potential to enter any nerve cell, it preferentially accumulates in neurons with higher energy demand, such as those involved in memory consolidation after extinction training 3. Hence, by acting as a mitochondrial electron cycler and antioxidant, low-dose methylene blue increases cellular energy production and support enhanced memory consolidation in key brain regions associated with memory processing 2. Based on the findings of this study 4, patients who continue to show moderate to high levels of fear at the conclusion of an exposure therapy session may have their fear inadvertently strengthened by methylene blue administration, thus leading to a less favorable therapeutic outcome.
Methylene blue common side effects include headache, vomiting, confusion, shortness of breath, and high blood pressure. Other side effects include serotonin syndrome, red blood cell breakdown, and allergic reactions. Use often turns the urine, sweat, and stool blue to green in color. Methylene blue is a thiazine dye. It works by converting the ferric iron (Fe+++) in hemoglobin to ferrous iron (Fe++). While use during pregnancy may harm the baby, not using it in methemoglobinemia is likely more dangerous.
Methylene blue is a monoamine oxidase (MAO) inhibitor and therefore can interact with selective serotonin reuptake inhibitor (SSRI) and monoamine oxidase (MAO) inhibitors to cause serious serotonin toxicity 5.
Methylene blue also interacts with dapsone and forms hydroxylamine which oxidizes hemoglobin causing hemolysis 6.
A few very rare case reports regarding methylene blue‐induced anaphylactic reactions upon injection in surgery patients were identified in the scientific literature 7. These reactions were IgE mediated and probably caused by a conjugation of methylene blue as hapten to a protein.
As no food or respiratory allergy nor skin allergy was identified in the literature search for methylene blue, and concern for anaphylactic reactions upon oral exposure is low, there are no safety concerns with respect to allergenicity of methylene blue 8.
Methylene blue contraindications
Methylene blue is contraindicated in patients who have developed hypersensitivity reactions to it and in severe renal insufficiency. It is relatively contraindicated in G6PD deficient patients as it can cause severe hemolysis and also in patients with Heinz body anemia 9.
What is methylene blue used for
Methylene blue, an inhibitor of nitric oxide synthase and guanylate cyclase has many uses in medicine. It has been found to improve the hypotension associated with various clinical states 10. It also improves hypoxia and hyper dynamic circulation in cirrhosis of liver and severe hepatopulmonary syndrome 11. It also results in transient and reproducible improvement in blood pressure and cardiac function in septic shock 12.
Methemoglobinemia
Methemoglobinemia (MetHb) is a blood disorder in which an abnormal amount of methemoglobin (MetHb) is produced. Hemoglobin is the protein in red blood cells that carries and distributes oxygen to the body. Methemoglobin is a form of hemoglobin. Methemoglobin normally exists in small amounts in the blood. However, when methemoglobin levels increase with methemoglobinemia, the blood is not able to release oxygen effectively to body tissues. The resulting lack of oxygen throughout the body can cause symptoms such as pale or blue-colored skin.
Methylene blue may be unsafe in people who have or may be at risk for a blood disease called G6PD deficiency. They should not take this medicine. If you or your child has G6PD deficiency, always tell your provider before getting treatment.
Causes of methemoglobinemia
Methemoglobinemia condition can be:
- Passed down through families (inherited or congenital)
- Caused by exposure to certain drugs, chemicals, or foods (acquired)
There are two forms of inherited methemoglobinemia. The first form is passed on by both parents. The parents usually do not have the condition themselves. They carry the gene that causes the condition. It occurs when there is a problem with an enzyme called cytochrome b5 reductase.
There are two types of inherited methemoglobinemia:
- Type 1 (also called erythrocyte reductase deficiency) occurs when red blood cells lack the enzyme.
- Type 2 (also called generalized reductase deficiency) occurs when the enzyme doesn’t work in the body.
The second form of inherited methemoglobinemia is called hemoglobin M disease. It is caused by defects in the hemoglobin protein itself. Only one parent needs to pass on the abnormal gene for the child to inherit the disease.
Acquired methemoglobinemia is more common than the inherited forms. Acquired methemoglobinemia occurs in some people after they are exposed to certain chemicals and drugs, including:
- Anesthetics such as benzocaine
- Nitrobenzene
- Certain antibiotics (including dapsone and chloroquine)
- Nitrites (used as additives to prevent meat from spoiling)
Certain foods, such as spinach, beets or carrots contain natural nitrates in large amounts. These foods should not be given to children younger than 6 months of age.
Methemoglobinemia symptoms
Symptoms of type 1 methemoglobinemia include:
- Bluish coloring of the skin
Symptoms of type 2 methemoglobinemia include:
- Developmental delay
- Failure to thrive
- Intellectual disability
- Seizures
Symptoms of hemoglobin M disease include:
- Bluish coloring of the skin
Symptoms of acquired methemoglobinemia include:
- Bluish coloring of the skin
- Headache
- Fatigue
- Shortness of breath
- Lack of energy
Methemoglobinemia prognosis
People with type 1 methemoglobinemia and hemoglobin M disease often do well. Type 2 methemoglobinemia is more serious. It often causes death within the first few years of life.
People with acquired methemoglobinemia often do very well once the drug, food, or chemical that caused the problem is identified and avoided.
Methemoglobinemia possible complications
Complications of methemoglobinemia include:
- Shock
- Seizures
- Death
Methemoglobinemia diagnosis and test
A baby with this condition will have a bluish skin color (cyanosis) at birth or shortly afterward. The health care provider will perform blood tests to diagnose the condition. Tests may include:
- Checking the oxygen level in the blood (pulse oximetry)
- Blood test to check levels of gases in the blood (arterial blood gas analysis)
Methemoglobinemia treatment
People with hemoglobin M disease don’t have symptoms. So, they may not need treatment.
Methylene blue is used to treat severe methemoglobinemia.
Methylene blue acts by reacting within red blood cell to form leukomethylene blue, which is a reducing agent of oxidized hemoglobin converting the ferric ion (Fe+++) back to its oxygen carrying ferrous state (Fe++) 13.
Ascorbic acid may also be used to reduce the level of methemoglobin.
Alternative treatments include hyperbaric oxygen therapy, red blood cell transfusion and exchange transfusions.
In most cases of mild acquired methemoglobinemia, no treatment is needed. But you should avoid the medicine or chemical that caused the problem. Severe cases may need a blood transfusion.
How is methylene blue given?
Methylene blue is injected into a vein through an IV. A healthcare provider will give you this injection. The IV infusion can take up to 30 minutes to complete.
Your breathing, blood pressure, oxygen levels, kidney function, and other vital signs will be watched closely while you are receiving methylene blue. Your blood will also need to be tested to help your doctor determine that the medicine is working.
You may only need to receive one dose of methylene blue. If you do need a second dose, it can be given 1 hour after your first dose.
Methylene blue will most likely cause your urine or stools to appear blue or green in color. This is a normal side effect of the medication and will not cause any harm. However, this effect may cause unusual results with certain urine tests.
Vasoplegic syndrome
Vasoplegic syndrome is generally defined as an arterial pressure <50 mm Hg, cardiac index >2.5 L /min/m², right atrial pressure <5 mm Hg, left atrial pressure <10 mm Hg and low systemic vascular resistance <800 dyne/sec/cm 14.
Risk factors for vasoplegia
Recent studies have established various risk factors for postoperative vasoplegia. These include preoperative use of heparin, ACE inhibitors, congestive heart failure, poor left ventricular function, duration of cardiopulmonary bypass, re-operation, age of the patient and opiod anesthesia 15.
Mechanism of action of methylene blue in vasoplegia
It has been suggested that refractory vasoplegia may reflect a dysregulation of nitric oxide synthesis and vascular smooth cell guanylate cyclase activation. Based on recent pathophysiologic findings it appears that the soluble intracellular enzyme guanylate cyclase is activated to produce cyclic guanosine monophosphate (C-GMP) presumably under the influence of several mediators including nitric oxide 16.
Methylene blue acts by inhibiting guanylate cyclase, thus decreasing C-GMP and vascular smooth muscle relaxation 17.
Preoperative use in cardiac surgery
Methylene blue (1%) has been used IV over 30 min in ICU 1hour before surgery and found decreased incidence and severity of vasoplegic syndrome in high risk patients 14.
Intraoperative use in cardiac surgery
It has also been successfully added to cardiopulmonary bypass prime (2 mg/ kg) and continued as infusion (.25- 2mg/kg/hr) during cardiopulmonary bypass to treat refractory hypotension in septic endocarditis 18.
Postoperative use in cardiac surgery
It can also be used to treat severe vasoplegia in post operative transplant patient 19. Hence studies have concluded decreased mortality in vasoplegic patients after cardiac surgery with methylene blue as compared to placebo 20.
Methylene blue in septic shock
A release of nitric oxide has been incriminated in the cardiovascular alterations of septic shock. Since guanylate cyclase is the target enzyme in the endothelium dependent relaxation mediated by nitric oxide, Methylene blue- a potent inhibitor of guanylate cyclase has been found very effective in improving the arterial pressure and cardiac function in septic shock 12.
Studies have found improvement in mean arterial pressure and systemic vascular resistance while decreasing vasopressor requirements in septic shock 21.
Methylene blue and hepatopulmonary syndrome
The hypoxemia in hepatopulmonary syndrome results from widespread pulmonary vasodilatation due to increased C-GMP. Methylene blue is found to ↑PaO2 and ↓alveolar-arterial difference for partial pressure of oxygen in all pts with hepatopulmonary syndrome. This was due to ↓C-GMP levels by Methylene Blue-a potent inhibitor of guanylate cyclase 22.
Methylene blue as antimalarial
Methylene blue has already been used some 100 years ago against malaria, but it disappeared when chloroquine and other drugs entered the market. However recent studies has shown the efficacy of Methylene blue as an effective and cheap antimalarial agent especially in countries with increasing resistance of P. falciparum to existing 1st line antimalarial agents-chloroquine and pyrimethamine-sulfadoxine.
Methylene blue, a specific inhibitor of P.falciparum glutathione reductase has the potential to reverse chloroquine resistance and it prevents the polymerization of haem into haemozoin similar to 4-amino-quinoline antimalarials.
A dose of 36-72mg/kg over 3 days is the most effective schedule 23.
Apart from the intrinsic antimalarial activity and chloroquine sensitizing action it was also considered to prevent methemoglobinemia- a serious complication of malarial anemia 24.
Methylene blue and cancer
Recent research suggests that Methylene Blue and other redox cyclers induce selective cancer cell apoptosis by NAD (P) H: quinine oxidoreductase (NQO1)-dependent bioreductive generation of cellular oxidative stress. Hence methylene blue is being investigated for the photodynamic treatment of cancer 25.
Methylene blue and ifosfamide neurotoxicity
Another, less well known use of methylene blue is its utility for treating ifosfamide neurotoxicity. A toxic metabolite of ifosfamide, chloroacetaldehyde, disrupts the mitochondrial respiratory chain, leading to accumulation of nicotinamide adenine dinucleotide hydrogen (NADH).
Methylene blue acts as an alternative electron acceptor, and reverses the NADH inhibition of hepatic gluconeogenesis while also inhibiting the transformation of chloroethylamine into Chloroacetaldehyde, and also inhibits multiple amine oxidase activities, preventing the formation of Chloroacetaldehyde 26.
Hence it has prophylactic and therapeutic role in ifosfamide – induced encephalopathy 27.
Methylene blue as dye and stain
Methylene blue infusion was found as a safe and effective method of localizing abnormal parathyroid glands 28.
Methylene blue has also been used for intraoperative endoscopic marking of intestinal lumen for location of lesions 29.
Methylene blue was also found as an effective and cheap alternative to isosulfan blue dye for sentinel lymph node localization in pt with breast cancer 30.
Methylene blue also has been used in diagnostic microbiology as a stain. It is an inexpensive and rapid method for detection of Helicobacter pylori (H.pylori) 31.
Methylene blue neutralization of heparin
Methylene blue effectively neutralizes heparin especially in pts with protamine allergy. However work still needs to be done to determine the safety of the drug at the higher doses necessary to neutralize heparin levels achieved in bypass patients 32.
Methylene blue and priapism
Methylene blue has been used to treat high flow priapism by intra-cavernous injection which is known to antagonize endothelial derived relaxation factor 33.
Methylene blue and Alzheimer’s disease
The relationship between Methylene blue and Alzheimer’s disease has recently attracted increasing scientific attention. It has been shown to attenuate the formations of amyloid plaques and neurofibrillary tangles and partial repair of impairments in mitochondrial function and cellular metabolism 34.
Methylene blue photodynamic therapy
Photodynamic therapy using the light activated anti-microbial agent, Methylene blue kills methicillin resistant staphylococcus aureus (MRSA) in superficial and deep excisional wounds 35. Methylene blue in combination with light also inactivates viral nucleic acid of hepatitis-C and human immunodeficiency virus (HIV-1) and treats cases of resistant plaque psoriasis 36.
Methylene blue dose
Methemoglobinemia: Dose commonly used is 1-2mg/kg of 1% Methylene blue solution 13.
Vasoplegic syndrome: Methylene blue is used as a single dose of 1.5 -2 mg /kg IV over 20 min to 1 hour for rescue treatment 14.
Antimalarial: A methylene blue dose of 36-72 mg/kg over 3 days is the most effective schedule 23.
Methylene blue side effects
Methylene blue turns urine greenish blue and bluish discoloration of skin and mucosa which is self limiting 37. Methylene blue may also cause blurred vision and may impair your thinking or reactions. Be careful if you drive or do anything that requires you to be alert and able to see clearly.
For at least 24 hours after treatment with methylene blue, avoid exposure to sunlight or tanning beds. This medicine can make you sunburn more easily. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Methylene blue also interferes with the pulse oximeter’s light emission resulting in falsely depressed oxygen saturation reading 6.
Check with your doctor or nurse immediately if any of the following side effects occur:
Incidence not known
- agitation
- bluish-colored lips, fingernails, or palms
- confusion
- cough
- dark urine
- diarrhea
- difficulty breathing
- difficulty swallowing
- dizziness or lightheadedness
- fast heartbeat
- fever
- headache
- hives or welts, itching, or skin rash
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- overactive reflexes
- pale skin
- poor coordination
- rapid heart rate
- redness of the skin
- restlessness
- shivering
- sore throat
- sweating
- talking or acting with excitement you cannot control
- tightness in the chest
- trembling or shaking
- twitching
- unusual bleeding or bruising
- unusual tiredness or weakness
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of methylene blue overdose
- abdominal or stomach pain
- bigger, dilated, or enlarged pupils (black part of the eye)
- blue staining of the urine, skin, and mucous membranes
- bluish-colored lips, fingernails, or palms
- blurred vision
- burning, crawling, itching, numbness, prickling, “pins and needles”, or tingling feelings
- confusion
- dark urine
- difficulty breathing
- dizziness or lightheadedness
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fear
- fever
- headache
- increased sensitivity of the eyes to light
- nausea
- pale skin
- rapid heart rate
- rapid shallow breathing
- shakiness in the legs, arms, hands, or feet
- sore throat
- tightness in the chest
- unusual bleeding or bruising
- unusual tiredness or weakness
- vomiting
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- change in taste
- changes in skin color
- feeling hot or cold
- increased sweating
- loss of taste
- muscle or joint pain
- pain at the infusion site
- pain in the arms or legs
Less common
- back pain
- bruising
- chills
- general feeling of discomfort or illness
- large, flat, blue or purplish patches in the skin
- loss of appetite
- muscle aches and pains
- muscle spasm
- runny nose
- trouble sleeping
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects.
Methylene blue toxicity
Methylene blue is a safe drug when used in therapeutic doses (<2mg/kg) 38. But methylene blue can cause toxicity in high doses. The features of toxicity being cardiac arrhythmias, coronary vasoconstriction, decreased cardiac output, renal blood flow and mesenteric blood flow; increased pulmonary vascular pressure and pulmonary vascular resistance and gas exchange deterioration 38.
Due to methylene blue tissue reactive properties, a case of skin and fat necrosis followed by a dry gangrene of the skin in a female patient with breast cancer who underwent sentinel lymph node biopsy localization using peri-tumoral injection of methylene blue dye has been reported 39.
Methylene blue can also cause hemolytic anemia characterized by Heinz body formation especially in people with severe renal insufficiency and glucose-6-phosphate dehydrogenase (G6PD) deficiency 6.
Neonates are particularly prone to adverse effects of methylene blue. It causes hyperbilirubinemia, meth-Hemoglobin formation, hemolytic anemia, respiratory distress, pulmonary edema, photo toxicity and bluish discoloration of tracheal secretions and urine 40.
Methylene blue due to its monoamine oxidase (MAO) inhibiting property may precipitate potentially fatal serotonin toxicity at doses >5mg/kg 41 and rarely can cause severe anaphylactic shock 42.
You can develop serotonin syndrome if you take methylene blue together with antidepressants called selective serotonin reuptake inhibitors (SSRIs), selective serotonin/norepinephrine reuptake inhibitors (SSNRIs) and monoamine oxidase inhibitors.
Common selective serotonin reuptake inhibitors (SSRIs) include citalopram (Celexa), sertraline (Zoloft), fluoxetine (Prozac), paroxetine (Paxil), and escitalopram (Lexapro). Selective serotonin/norepinephrine reuptake inhibitors (SSNRIs) include duloxetine (Cymbalta) and venlafaxine (Effexor). Common monoamine oxidase inhibitors include isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Emsam) and tranylcypromine (Parnate).
If you take these medicines, be sure to read the warning on the packaging. It tells you about the potential risk of serotonin syndrome. However, do not stop taking your medicine. Talk to your doctor about your concerns first.
People with serotonin syndrome will likely stay in the hospital for at least 24 hours for close observation.
Serotonin syndrome treatment may include:
- Benzodiazepine medicines, such as diazepam (Valium) or lorazepam (Ativan) to decrease agitation, seizure-like movements, and muscle stiffness
- Cyproheptadine (Periactin), a drug that blocks serotonin production
- Intravenous (through the vein) fluids
- Withdrawal of medicines that caused the syndrome
In life-threatening cases, medicines that keep the muscles still (paralyze them), and a temporary breathing tube and breathing machine will be needed to prevent further muscle damage.
Serotonin syndrome prognosis
People may get slowly worse and can become severely ill if not quickly treated. Untreated, serotonin syndrome can be deadly. With treatment, symptoms usually go away in less than 24 hours.
Uncontrolled muscle spasms can cause severe muscle breakdown. The products produced when the muscles break down are released into the blood and eventually go through the kidneys. This can cause severe kidney damage if serotonin syndrome isn’t recognized and treated properly.
Serotonin syndrome symptoms occur within minutes to hours, and may include 43:
- Agitation or restlessness
- Diarrhea
- Fast heartbeat and high blood pressure
- Hallucinations
- Increased body temperature
- Loss of coordination
- Nausea and vomiting
- Overactive reflexes
- Rapid changes in blood pressure.
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 34. ISBN 9780857111562.
- Rojas JC, Bruchey AK, Gonzalez-Lima F. Neurometabolic mechanisms for memory enhancement and neuroprotection of methylene blue. Progress in Neurobiology. 2012;96(1):32-45. doi:10.1016/j.pneurobio.2011.10.007. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3265679/
- Gonzalez-Lima F, Bruchey AK. Extinction memory improvement by the metabolic enhancer methylene blue. Learn Mem. 2004;11:633–640 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC523083/
- Telch MJ, Bruchey AK, Rosenfield D, et al. Post-Session Administration of USP Methylene Blue Facilitates the Retention of Pathological Fear Extinction and Contextual Memory in Phobic Adults. The American journal of psychiatry. 2014;171(10):1091-1098. doi:10.1176/appi.ajp.2014.13101407. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4467026/
- Gillman P K. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia. 2006;61:1013–4 https://www.ncbi.nlm.nih.gov/pubmed/16978328
- Clifton, Jack II, Leikin, Jerrold Methylene blue. American Journal of Therapeutics. 2003;10:289–91.
- Dewachter P, Castro S, Nicaise‐Roland P, Chollet‐Martin S, Le Beller C, Lillo‐le‐Louet A and Mouton‐Faivre C, 2011. Anaphylactic reaction after methylene blue‐treated plasma transfusion. British Journal of Anaesthesia, 106, 687–689. https://doi.org/10.1093/bja/aer009
- Dyes in aquaculture and reference points for action. EFSA Journal 29 June 2017. https://efsa.onlinelibrary.wiley.com/doi/10.2903/j.efsa.2017.4920
- Clifton, Jack II, Leikin, Jerrold Methylene blue. American Journal of Therapeutics. 2003;10:289–91. https://www.ncbi.nlm.nih.gov/pubmed/12845393
- Bosoy , Dimitry , Axelband , et al. Utilization of methylene blue in the setting of hypotension associated with concurrent renal and hepatic failure: a concise review. OPUS 12 Scientist. 2008;2:21–9.
- Peter schenk, Christian Madl, Shahrzad Rezaie-Majd, Stephen Lehr, Christian Muller. Methylene blue improves the hepatopulmonary syndrome. Ann Intern Med. 2000;133:701–6.
- Preiser, Jean-Charles, Lejeune, et al. Methylene blue administration in septic shock: A Clinical Trial. Critical Care Medicine. 1995;23:259–64.
- Methemoglobinemia: a case study. Boylston M, Beer D. Crit Care Nurse. 2002 Aug; 22(4):50-5. http://ccn.aacnjournals.org/content/22/4/50.long
- Ertugrul Ozal, Erkan Kuralay, Vedat Yildirim, et al. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery. Ann Thorac Surg. 2005;79:1615–9. https://www.ncbi.nlm.nih.gov/pubmed/15854942
- Armand Mekontso-Dessap, Remi Houel, Celine Soustelle, Matthias Kirsch, Dominique Thebert, Daniel Y. Loisance.Risk factors for post-cardiopulmonary bypass vasoplegia in patients with preserved left ventricular function. Ann Thorac Surg. 2001;71:1428–32. https://www.ncbi.nlm.nih.gov/pubmed/11383777
- Levin Ricardo L, Degrange Marcela A, Bruno Gustavo F, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77:496–9. https://www.ncbi.nlm.nih.gov/pubmed/14759425
- Gachot B, Bedos J.P, Veber B, Wolff M, Regnier B. Short-term effects of methylene blue on hemodynamics and gas exchange in humans with septic shock. Intensive Care Medicine. 1995;21:1027–31 https://www.ncbi.nlm.nih.gov/pubmed/8750129
- Grayling M, Deakin C D. Methylene blue during cardiopulmonary bypass to treat refractory hypotension in septic endocarditis. J Thorac Cardiovasc Surg. 2003;125:426–7.
- Kofidis T, Struber M, Wilhelmi M, et al. Reversal of severe vasoplegia with single-dose methylene blue after heart transplantation. J Thoracic Cardiovasc Surg. 2001;122:823–4.
- Levin Ricardo L, Degrange Marcela A, Bruno Gustavo F, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77:496–9.
- Edmund S, Kwok H, Howers Daniel. Use of methylene blue in sepsis: A Systematic Review. Journal of Intensive Care Medicine. 2006;21:359–63.
- Peter schenk, Christian Madl, Shahrzad Rezaie-Majd, Stephen Lehr, Christian Muller. Methylene blue improves the hepatopulmonary syndrome. Ann Intern Med. 2000;133:701–6
- Meissner Peter E, Germain Mandi, Boubacar Coulibaly, et al. Methylene blue for malaria in Africa: results from a dose-finding study in combination with chloroquine. Malaria Journal. 2006;5:84. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1617109/
- Schirmer R.H, Coulibaly B, Stich A, et al. Methylene blue as an antimalarial agent. Redox rep. 2003;8:272–5. https://www.ncbi.nlm.nih.gov/pubmed/14962363
- Wondrak GT. NQO1-activated phenothiazinium redox cyclers for the targeted bioreductive induction of cancer cell apoptosis. Free Radic Biol Med. 2007;43:178–90 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705808/
- Alici-Evcimen Y, Breitbart WS. Ifosfamide neuropsychiatric toxicity in patients with cancer. Psychooncology. 2007;16:956–60.
- Pelgrims J, De Vos F, Van den Brande J, Schrijvers D, Prové, Vermorken JB. Methylene blue in the treatment and prevention of ifosfamide-induced encephalopathy: report of 12 cases and a review of the literature. British Journal of Cancer. 2000;82:291–4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2363270/pdf/82-6690917a.pdf
- Gordan Donald L, Airan Mohan C, Thomas William, Seidman Leon H. Parathyroid identification by methylene blue infusion. British Journal of Surgery. 2005;62:747–9.
- Beretvas RI, Ponsky J. Endoscopic marking: an adjunct to laparoscopic gastrointestinal surgery. Surgical endoscopy. 2001;15:1202–3.
- Simmons RM, Smith SM, Osborne MP. Methylene blue dye as an alternative to isosulfan blue dye for sentinel lymph node localization. Breast J. 2001;7:181–3.
- Misra V, Misra SP, Dwivedi M, Gupta SC. The Loeffler’s methylene blue stain: An inexpensive and rapid method for detection of helicobacter pylori. Journal of Gastroenterology and Hepatology. 2008;9:512–3.
- Sloand EM, Kessler CM, Mcintosh CL, Klein HG. Methylene blue for neutralization of heparin. Thromb Res. 1989;54:677–86
- Steers WD, Selby JB. Use of methylene blue and selective embolization of the pudendal artery for high flow priapism refractory to medical and surgical treatments. J Urol. 1991;146:1361–3.
- Murat Oz, Lorke Dietrich E, Petroianu George A. Methylene blue and Alzheimer’s disease. Biochemical pharmacology. 2009;78:927–32
- Zolfaghari Parjam S, Samantha Packer, Mervyn Singer, et al. In vivo killing of Staphylococcus aureus using light-activated antimicrobial agent. BMC Microbiology. 2009;9:27.
- Salah M, Samy N, Fadel M. Methylene blue mediated photodynamic therapy for resistant plaque psoriasis. J Drugs Dermatol. 2009;8:42–9
- Ertugrul Ozal, Erkan Kuralay, Vedat Yildirim, et al. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery. Ann Thorac Surg. 2005;79:1615–9.
- Ginimuge PR, Jyothi SD. Methylene Blue: Revisited. Journal of Anaesthesiology, Clinical Pharmacology. 2010;26(4):517-520. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3087269/
- Salhab M, Al sarakbi W, Mokbel K. Skin and fat necrosis of the breast following methylene blue dye injection for sentinel node biopsy in a patient with breast cancer. Int Semin Surg Oncol. 2005;2:26.
- Cowett RM, Hakanson DO, Kocon RW, Oh W. Untoward neonatal effect of intraamniotic administration of methylene blue. Obstet Gynecol. 1976;48:74–5.
- Gillman P K. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia. 2006;61:1013–4. https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1365-2044.2006.04808.x
- Pascale Dewachter, Claudie Moutan-Faivre, Philippe Trechot, Jean-Claude Lleu, Paul Michel Mertes. Severe anaphylactic shock with methylene blue instillation. Anesth Analg. 2005;101:149–50. https://www.ncbi.nlm.nih.gov/pubmed/15976222
- Serotonin syndrome. https://medlineplus.gov/ency/article/007272.htm