Microfracture surgery
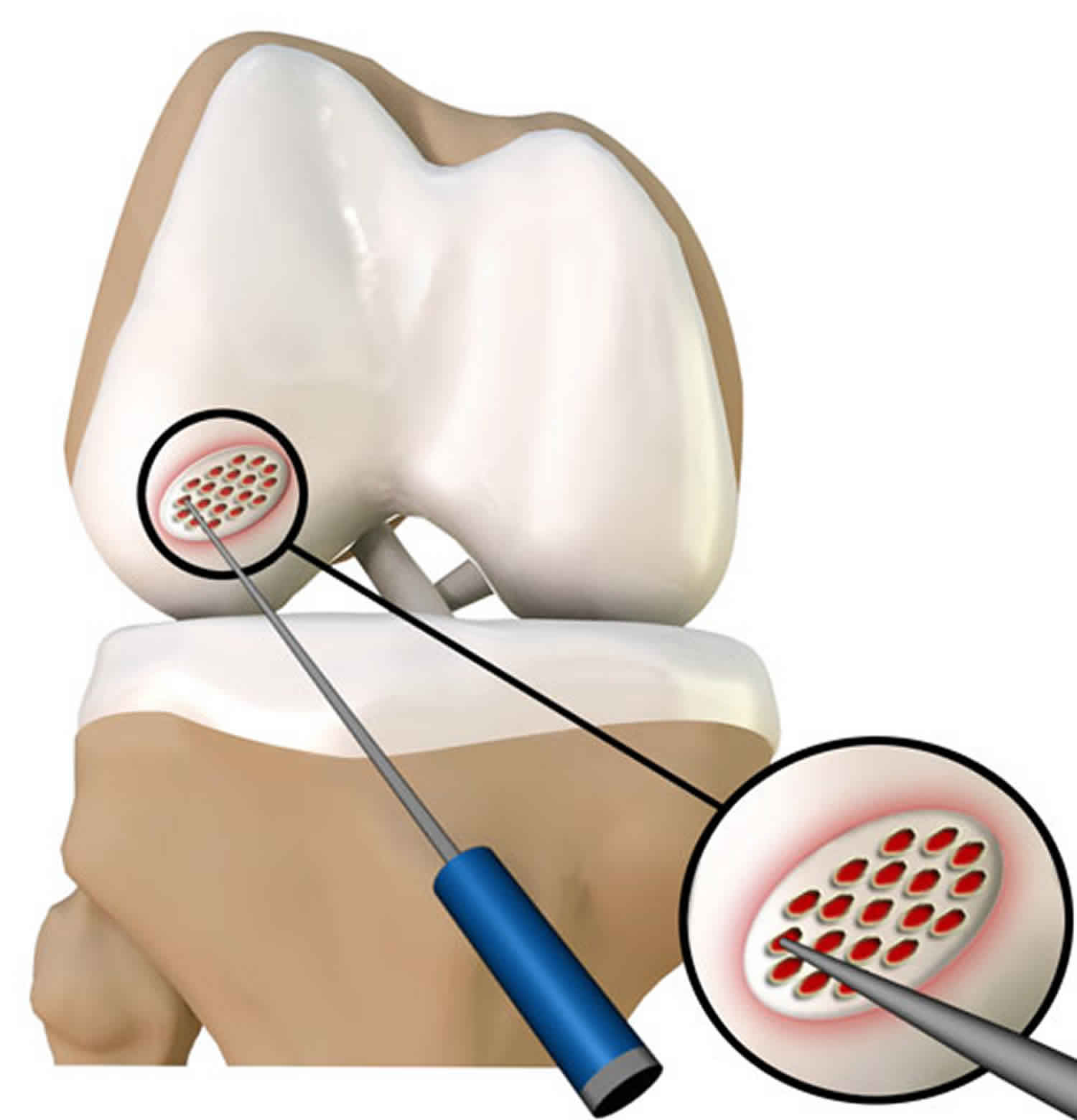
Microfracture also called microfracture surgery, is a articular cartilage repair surgical technique performed to promote the healing of damaged cartilage with the use of stem cells (progenitor cells of the body) that works by creating tiny fractures in the underlying bone. This causes new cartilage to develop from a so-called super-clot. The goal of microfracture is to stimulate the growth of new articular cartilage by creating a new blood supply. Technically, microfracture surgery is a bone marrow stimulation procedure and is based on the puncturing of the subchondral bone plate into the bone marrow, the generation of a blood clot containing precursor cell populations derived from the subchondral bone marrow, and the spontaneous transformation of the repair clot into a fibrocartilaginous repair tissue. A sharp tool called an awl is used to make multiple holes in the joint surface. The holes are made in the bone beneath the cartilage, called subchondral bone. This action creates a healing response. New blood supply can reach the joint surface, bringing with it new cells that will form the new cartilage.
The treatment of chondral lesions of the knee remains, even today, a dilemma for the orthopaedic surgeon or sports medicine physician. Symptoms and levels of impairment from articular cartilage lesions of the knee vary greatly between individuals. For those lesions that cause symptoms in patients, several lines of treatment have been developed. Of these treatment strategies, the most common and most useful is microfracture – an arthroscopic procedure and rehabilitation programme that was developed in the early 1980s by Dr J. Richard Steadman 1. Today, microfracture is still the most commonly utilised articular cartilage repair procedure throughout the world.
Since its development, the microfracture procedure has been used by its originator to treat more than 2000 patients. Of these patients, 75 to 80% experienced significant pain relief and improvement in the ability to perform daily activities and participate in sports. Fifteen percent noticed no change, and five percent continued to have joint deterioration.
Microfracture surgery is considered the best procedure to treat cartilage injuries less than ½ inch or 15 mm. Microfracture is widely used to treat hip and knee injuries.
Microfracture can be done with an arthroscope. The best candidates are young patients with single lesions and healthy subchondral bone.
Microfracture surgery is quick (typically lasting between 30–90 minutes), minimally invasive, and can have a significantly shorter recovery time than an arthroplasty (knee replacement).
Microfracture may be indicated for the following:
- Cartilage lesions
- Young patients who have a single injury and healthy subchondral bone (bone underlying the articular cartilage)
Contraindication for microfracture surgery of the hip will be defects larger than 4 cm² as well as in cases of more advanced osteoarthritis (extensive acetabular lesions, equivalent lesions of the femoral head) 2. Age (e.g. over 60 years) is also considered a relative contraindication as well as the impossibility of undergoing an adequate rehabilitation regime 3.
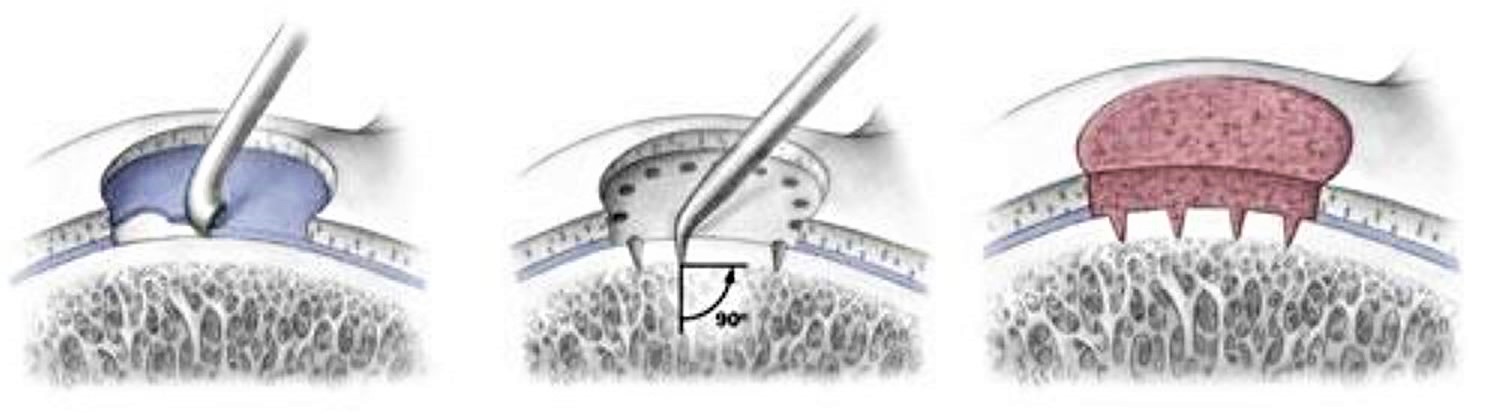
The microfracture surgery is usually performed as an arthroscopic procedure (arthroscope is an instrument consisting of a small camera to view the area of injury) under local, spinal or general anesthesia. Three small incisions are made to insert the arthroscope and other instruments. Any loose or unstable cartilage is removed. Your surgeon will insert a sharp tool known as an awl to make several holes on the surface of the ankle joint. These holes penetrate into the subchondral bone and open up new blood supply to the area. This new blood supply from within the bone marrow, supplies the damaged joint surface with new stem cells to form fibrocartilage, which fills the damaged area and promotes the formation of new tissue. The incisions will then be covered.
Figure 1. Microfracture surgery technique
Footnote: Steps of the microfracture technique. (Left) Damaged cartilage is removed. (Center) Awl is used to make holes in the subchondral bone. (Right) Healing response brings new, healthy cartilage cells.
Is microfracture a “cure” for osteoarthritis?
No, microfracture is a technique to help form a new surface to cover chondral defects. If successful, it minimizes pain and swelling, and helps the joint function more normally.
Is the new tissue that forms after the microfracture identical to the original articular cartilage?
No, the new tissue is a “hybrid” of articular-like cartilage plus fibrocartilage. Experience shows that this hybrid repair tissue is durable and functions similarly to articular cartilage.
Can microfracture be used in joints other than the knee?
Yes, there are reports of microfracture being used in the shoulder, the hip, and the ankle. The long-term effectiveness of the technique in these other joints is unknown. This is because there are no long-term studies available similar to those that have been done to evaluate the procedure in the knee.
Microfracture surgery indications
Several factors to take into consideration for use of the microfracture procedure include patient age, acceptable bio-mechanical alignment of the knee, activity level, the patient’s willingness to accept the extensive rehabilitation protocol and the individual’s expectations. If all of these criteria are met, then microfracture may be a suitable treatment option for the patient.
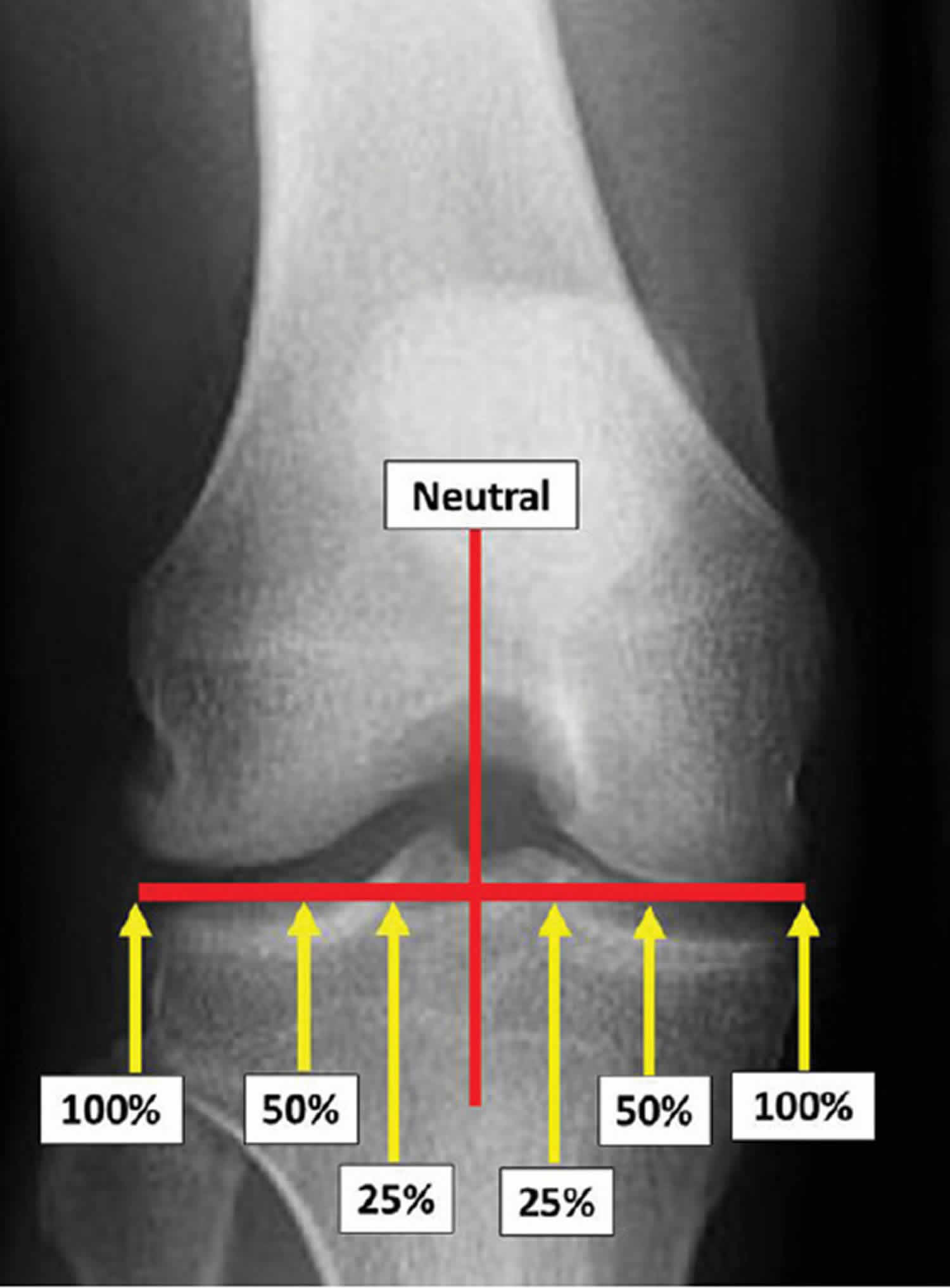
In addition, it is extremely important to manage the patient’s expectations. Patient-centered questionnaires are important to understand the patient’s symptoms and limitations in function. Imaging is also necessary for proper patient selection. To determine angular deformity, a long-standing hip to ankle image radiograph is taken. Axial alignment is measured by drawing a line from the center of the head of the femur to the centre of the tibiotarsal joint and assessing the load-bearing line within the knee joint 4. With the center of the joint being 0% or neutral alignment and 100% being the outside edge of the condyles, alignment outside of 25% on the medial or lateral side may result in inferior results following microfracture (Figure 2). The patellofemoral joint is also evaluated by way of radiographic patellar views. Standard anteriorposterior and lateral images are also reviewed. Images with both knees flexed to 30 or 45 degrees in a weightbearing position are also included. In the case of a suspected chondral defect, a magnetic resonance image (MRI) allows for confirmation of the articular cartilage defect and allows for analysis of co-pathologies.
The original description and regimen for microfracture was a combination of surgery and rehabilitation which would allow cartilage repair tissue to form in the articular cartilage defect. The surgical goal was to create fractures in the subchondral bone perpendicular to the surface. Through these fractures, blood and marrow elements would be released and form a ‘super’ clot. To reach all areas of the knee joint, various angled picks were developed. Previous work had been done with drills, but drills could not reach all areas of the joint and produced heat when used, which could limit the development of new tissue
Several peer-reviewed basic science studies proved the concepts behind microfracture in the 1990s and 2000s 5. The first study evaluated the percentage of fill and the collagen content in the repair tissue 1. At 4 and 12 months following microfracture, there was more repair tissue in defects that were treated with microfracture compared to untreated lesions. In addition, type II collagen was increased, with 74% type II collagen at 12 months. Earlier bone remodelling was noted by changes in porosity 1. The next basic science study proved that the removal of the calcified cartilage layer improved the grade of the repair tissue and the filling of the lesion 6.
To further understand the composition of the repair tissue, Frisbie et al 7 looked at key matrix component expression in early cartilage healing following microfracture. Samples were collected at 2, 4, 6 and 8 weeks. The study showed that over the 8 week period, mRNA levels for type II collagen, as well as aggrecan, gradually increased in the microfracture group. These findings supported non-weightbearing for 8 weeks in patients with microfracture on weightbearing surfaces. The basic science study showed that the repair cartilage was not adequately mature until 8 weeks 7.
One of the first studies on outcomes compared patients who used continuous passive motion (CPM) following microfracture 8. Based on second-look arthroscopies, the study concluded that patients who used CPM (continuous passive motion) had improved cartilage healing. This study supported the use of CPM for 8 weeks following microfracture, in addition to non-weightbearing 8.
Figure 2. Assessing alignment, the line between the hip and knee crosses through the knee joint. If the line lands outside of the 25% line, microfracture on the weightbearing condyles maybe contraindicated.
Microfracture surgical procedure
The microfracture procedure is done arthroscopically. The surgeon visually assesses the defect and performs the procedure using special instruments that are inserted through three small incisions on the knee. After assessing the cartilage damage, any unstable cartilage is removed from the exposed bone. The surrounding rim of remaining articular cartilage is also checked for loose or marginally attached cartilage. This loose cartilage is also removed so that there is a stable edge of cartilage surrounding the defect. The process of thoroughly cleaning and preparing the defect is essential for optimum results.
Multiple holes, or microfractures are made in the articular cartilage lesion with the awls in the exposed bone about 3 to 4 mm apart. The awl should be perpendicular to the bone as it is advanced. A 90° awl is used for the patella if an angle cannot be created to accommodate the 45° awl. It is important that the 90° awl only be advanced manually, with no use of a mallet. Microfracture holes are made around the edge of the defect and then continued to the center. When all of the holes have been made, the fluid pressure is reduced to verify the release of fat droplets and blood from the microfracture holes. Microfracture creates a rough surface on the subchondral bone. This surface allows the marrow clot to adhere more easily, while the integrity of the subchondral plate is maintained for joint surface shape.
Bone marrow cells and blood from the holes combine to form a “super clot” that completely covers the damaged area. This marrow-rich clot is the basis for the new tissue formation. The microfracture technique produces a rough bone surface that the clot adheres to more easily. This clot eventually matures into firm repair tissue that becomes smooth and durable. Since this maturing process is gradual, it usually takes two to six months after the procedure for the patient to experience improvement in the pain and function of the knee. Improvement is likely to continue for about 2 to 3 years.
For successful outcomes, the joint environment must be corrected if indicated. It is critical that there is adequate space in the knee and no limitations in full motion. Arthrofibrosis, infrapatellar or suprapatellar plica and anterior interval scarring can all limit the joint space 9. In most cases, these can be corrected at the same time as the microfracture procedure.
Complementary biological treatments
Although microfracture treatment is clearly suggested for the management of full-thickness chondral lesions, there are still deficiencies of neoformed tissue in the lesion. Various complementary biological treatments have been suggested, but they will always be complementary to the microfractures 10. Options for complementary biological treatments include the use of growth factors (Plasma Rich Protein), collagen membranes, stem cells, chondrocyte grafts or, in case of open surgery, osteochondral grafts. All these complementary options are surgically more demanding, especially the stable fixation of the respective membranes in the area of the microfractures. They also have additional surgery costs. Recent publications confirmed the formation of a more stable tissue, with higher cellularity and good short-term clinical outcomes but there are insufficient long-term clinical results supporting the routine use of some of these surgical techniques 11.
Microfracture surgery risks and complications
As with any procedure, microfracture involves some of the following risks and complications:
- Bleeding
- Infections
- Blood clots
- The newly formed cartilage is not as strong as the body’s original cartilage, and thus, there is a risk of it breaking overtime.
Most patients progress through the postoperative period with little or no difficulty. Some patients may develop mild transient pain, most frequently after microfracture has been performed on the patella (kneecap) and trochlear groove (the groove on the femur in which the patella glides during motion). Small changes in the articular surface of this patellofemoral joint may produce a grating or “gritty” sensation, particularly when a patient discontinues use of the knee brace and begins normal weightbearing through a full range of motion. Patients rarely have pain at this time, and this grating sensation typically resolves on its own in a few days or weeks.
Similarly, if a steep perpendicular rim was made in the trochlear groove, patients may notice “catching” or “locking” as the ridge of the patella rides over this area during joint motion. Some patients may even notice these symptoms while using the continuous passive motion machine (CPM), a device that gently moves the joint while the patient is lying down. If this locking sensation is painful, the patient is advised to limit weightbearing and avoid the bothersome joint angle for an additional period. These symptoms usually dissipate within 3 months.
Typically, swelling and joint effusion (fluid in the joint) disappear within 8 weeks after a microfracture procedure. Occasionally, a recurrent effusion develops between 6 and 8 weeks after surgery for a defect on the femur; usually when a patient begins to put weight on the injured leg. This effusion may mimic the preoperative or immediate postoperative effusion, although it is usually painless. It usually resolves within several weeks. Rarely is a second arthroscopy required for recurring effusions.
Microfracture surgery post-operative protocol
When developing the microfracture procedure, Dr Steadman recognised that development of a post-operative protocol was needed to protect the repair and facilitate cartilage regrowth. Most prior cartilage procedures had little to no emphasis on the post-operative period. The goal of the protocol was to create an environment which allows maximum differentiation of repair tissue. The size and location of the treated lesion determines specifics of the rehabilitation plan. The particular protocol of the rehabilitation programme should be tailored to the procedures that have been performed on the patient to ensure the best possible outcomes.
When microfracture is performed on the weightbearing surfaces of the femoral condyles or tibial plateaus, mobilisation begins immediately after surgery, with a CPM machine in the recovery room. Initially, range of motion is roughly 30 to 70 degrees and the machine will cycle once per minute. This will be increased as tolerated by the patient. The goal is to have the patient on the machine for 6 to 8 hours in a 24 hour period. The ultimate goal here is for the patient to gain complete passive range of motion as soon as possible post-surgery. In addition, there is an emphasis on range of motion of the patella and patellar tendon motion. Patellar mobilisation exercises are taught to the patient on the first day following surgery. All patients receive cold therapy after surgery to reduce inflammation as well as pain. Cold therapy is usually implemented for 1 to 7 days after surgery.
Crutch-assisted touch-down weight-bearing ambulation is prescribed for up 8 weeks based on the size of the lesion. In patients with smaller lesions, less than 1 cm, this prescription may be shorter. For this, patients will place about 10% to 30% of their body weight on the injured leg. Between 1 and 2 weeks after surgery the patient will be placed on a stationary bike without resistance and begin a deep-water exercise programme that involves running. Flotation will be used so that the injured leg does not touch the bottom of the pool. This is an imperative step and must be followed.
At roughly 8 weeks the patient progresses to full weightbearing. On occasion, an unloader brace prescribed for the appropriate compartment, is used as weightbearing is progressed to normal to protect the healing lesion. Then, a period of dynamic biking with increasing resistance. Biking is the fundamental exercise to rebuild strength between 8 and 16 weeks post-surgery. Elastic resistance band programmes are added at 12 weeks following the detailed description that has been published 12.
All patients treated by microfracture for patellofemoral lesions will be put in a brace with motion limited to 0° to 20° for at least 8 weeks. This range of motion limits compression of the regenerating surfaces of the trochlea or patella or both. Passive motion is allowed with the brace removed, but otherwise the brace must be worn at all times. The brace is removed for CPM usage and replaced following CPM usage. For patients with patellofemoral joint lesions, joint angles are carefully observed at the time of arthroscopy to determine where the defect comes into contact with the patellar facet or the trochlear groove. These angles are avoided during strength training for approximately 4 months. This avoidance allows for immediate training in the 0° to 20° range postoperatively because there is minimal compression of these chondral surfaces with such limited motion.
Patients with lesions of the patellofe-moral joint treated with microfracture are allowed weightbearing as tolerated in their brace 2 weeks after surgery. After 8 weeks, the brace is gradually opened and then discontinued. When the brace is discontinued, patients are allowed to advance their training progressively. Starting 12 weeks after microfracture, the exercise programme is the same one used for femorotibial lesions.
Improvement in knee function may not occur for at least 6 months after microfracture, so patients are counselled preoperatively so they understand what to expect after surgery. Improvement has been shown to occur slowly and steadily for at least 2 years, which has been supported by a clinical research data 13. The repair tissue matures, pain and swelling resolve and patients regain confidence and comfort in their knees during increased levels of activity during this time period.
Microfracture surgery recovery
Following the microfracture surgical procedure, the rehabilitation program after microfracture is crucial to optimize the success of the surgical technique. The rehabilitation program is designed to promote the ideal physical environment in which the bone marrow cells can transition into the appropriate cartilage-like cell lines. When the ideal physical environment is combined with the ideal chemical environment produced by the marrow clot, a repair cartilage can develop that fills the original defect. Your physical therapist will teach you exercises during the rehabilitation program to regain muscle strength, promote healing and gain normal range of motion of the joint.
The specific rehabilitation program for each patient following a microfracture will vary depending upon the following factors:
- The location of the defect
- The size of the defect
- Whether any other surgical procedure, such as an anterior cruciate ligament reconstruction, was done at the same time as microfracture
Following are examples of some rehabilitation programs.
Rehabilitation protocol for patients with chondral defects on the femur or tibia
- The patient is started on a continuous passive motion (CPM) machine immediately in the recovery room. Ideally, the patient should use the machine for 6 to 8 hours every 24 hours. Range of motion is increased as tolerated until full range of motion is achieved with the machine.
- If a continuous passive motion (CPM) machine is not used, the patient begins passive flexion/extension (straightening and bending) of the knee with 500 repetitions three times a day.
- The use of crutches, with only light touch-down weight allowed on the involved leg, is prescribed for 6 to 8 weeks. Patients with small defect areas (less than 1cm in diameter) may be allowed to put weight on the leg a few weeks sooner.
- Brace use is rarely recommended for patients with chondral defects on the femur or tibia.
Limited strength training also begins immediately after microfracture surgery.
- Standing one-third knee bends with a great deal of the weight on the uninjured leg begin the day after surgery.
- Stationary biking without resistance and a deep-water exercise program begin 1 to 2 weeks after surgery.
- After 8 weeks the patient progresses to full weight bearing and begins a more vigorous program of active knee motion.
- Elastic resistance cord exercises can begin about 8 weeks following surgery.
- Free weights or machine weights can be started when the early goals of the rehabilitation program have been met, but no sooner than 16 weeks after surgery.
- Patients must not resume sports that involve pivoting, cutting, and jumping for 4 to 6 months after a microfracture procedure. Full activity may be resumed once the physician has examined the knee and given approval for the patient to return to sports activity.
Rehabilitation protocol for patients with patellofemoral chondral defects
- All patients treated with microfracture for patellofemoral defects must use a brace set for 0° to 20° of flexion for at least 8 weeks. It is essential to limit compression of the new surfaces in the early postoperative period, so that the maturing marrow clot will not be disturbed. The brace should be worn at all times except when passive motion is allowed.
- Patients are placed into a continuous passive motion (CPM) machine immediately following surgery. The goal is to obtain a pain-free and full passive range of motion soon after surgery during those periods when the brace is removed.
- When the patient wears a brace, strength training is allowed, but only in the 0° to 20° range immediately after surgery in order to limit compression of the affected chondral surfaces. The joint angles of these patients are observed carefully at the time of surgery to determine where the defect makes contact with the opposing surface, either on the patella or on the trochlear groove of the femur. These areas are avoided during strength training for approximately 4 months.
- Patients are allowed to put weight on the involved leg as tolerated, but it must be limited to the angles of flexion that do not compress the treated surfaces. For this reason the patient must wear a brace locked in limited flexion.
- After 8 weeks, the knee brace is gradually opened to allow increased flexion of the knee, a process that takes about a month. Brace use is generally discontinued at about 12 weeks. Some patients, however, like to continue to wear the brace for strenuous exercise for a few more months up to about 6 months.
- After brace use is discontinued, strength training advances progressively.
- The doctor must examine the knee before the patient is released to full activity.
Microfracture knee surgery success rate
Microfracture surgery is suitable for patients of any age, but microfracture does not work for everyone. It is used less frequently in patients over 65 years of age. In older patients with more diffuse articular cartilage loss, joint replacement is usually more appropriate treatment.
In degenerative knees it has been found to have about a 75% success rate. Twenty two percent of the patients remain unchanged and about three percent are made worse. One study has shown a success rate of 75 to 80 percent among patients 45 years of age or younger 14. Even a partially successful procedure can greatly enhance function and delay or eliminate the need for more aggressive surgery such as total joint replacement or cartilage transplantation. Three percent of patients may be made worse. Rarely a patient may become stiff and require a further procedure to restore motion. Infection is rare but may occur in about one in every few hundred procedures. Other very rare complications may also occur.
The first long-term outcomes paper was published on the microfracture technique in 2003 13. This study followed 72 patients with acute chondral lesions at an average of 11 years after microfracture, with the longest follow-up being 17 years. The results showed a decrease in symptoms and improved function. The study identified age as the only independent predictor of Lysholm improvement. Patients over 35 years of age improved less than patients under 35; nonetheless both groups showed improvement 13.
Recently, a study compared the outcomes of autologous chondrocyte implantation with microfracture treatment in a randomized trial 15. Forty patients were treated in each group. At 2 years, both groups showed significant improvement on the Lysholm scale and, particularly, pain, with no difference between the groups. However, the microfracture group had more improvement in the Short Form-36 physical component score 15. A follow-up to this study showed no differences at 5 years 16.
Cartilage injuries are common in high-impact sports. In American football, 25 active National Football League players were treated with microfracture between 1986 and 1997. By the next season, 76% of the players returned to play and continued to play for an additional 4 seasons. All players showed decreased symptoms and improvement in function. Of those players who did not return to play, most had pre-existing degenerative changes of the knee 17. In a group of professional skiers who underwent microfracture, excellent patient-centered outcomes were seen at an average of 77 months follow-up13. The median postoperative Tegner activity scale was 10 (range 4 to 10), even 7 years after professional skiing. One patient did not return to skiing. The average time from surgery to return to competition was 13.4 months (range 0.5 to 25.3 months). Among skiers with a World Cup ranking, improved ranking was seen in the majority. The study showed that microfracture, with the recommended post-operative protocol, is an acceptable treatment option for elite skiers who have full thickness articular cartilage lesions of the knee. Microfracture has also been successful in young patients 18. In patients between 12 and 18 years old, excellent outcomes and high patient satisfaction was found at an average of 5.8 years following microfracture 19. Only one patient required a revision microfracture of a trochlear defect. These young patients returned to full activity with no disability from their knee injury. Many other studies have documented varied results following microfracture. Most of these studies did not follow the post-opreative protocol. For optimal results it is critical to follow the surgical technique and post-operative protocol as originally described.
Microfracture hip surgery success rate
One of the first publications about short-term clinical results in patients treated with microfractures for grade 4 chondral lesions of the hip was by Philippon et al. 20. In 2008, he published a series of nine patients who underwent revision arthroscopy after previous arthroscopic treatment with microfractures for a full-thickness chondral lesion. He describes filling an average of 91% with a tissue described as stable 20. However, no clinical results of these series were published.
In 2009, Byrd and Jones 21 published a series of micro perforations in 58 patients with grade 4 lesions with good functional results and an increase of 20 points (rise from 65 preop. to 85 postoperative) in the Modified Harris Hip Score. In 2012, Karthikeyan et al. 22 published a series of 20 patients who underwent microfractures in acetabular chondral defects. Revision arthroscopy was performed in all of them (17 ± 11 months of follow-up). An average filling of the chondral defect of 93% (±17%) was found, defining the cartilage as macroscopically stable. The results in functional
scores showed an increase of the non-arthritic hip score from 54.5 to 78 in an average period of 21 months.
In 2014, Domb et al. 23 published a series of 30 patients with femoroacetabular impingement and grade 4 chondral lesions. In all of the patients the femoroacetabular impingement was corrected, the full-thickness chondral lesions were treated with microfractures. The clinical assessment was performed with a minimum period of two years of follow-up, considering several functional scores (Modified Harris Hip Score, non-arthritic hip score, HOS-ADL). All measured functional scores had significant improvements; however, there was no comparative group in this study. In 2015, Domb et al. 24 published a new series of patients with a femoroacetabular impingement and chondral lesions treated by hip arthroscopy. Two comparative groups with and without microfractures were defined. The aforementioned functional scores were assessed after a minimum follow-up period of two years. Although all patients showed a significant improvement in all measured scores, there was no significant difference in the two studied groups 24.
In 2012, McDonald et al. 25 also published a comparative series of elite athletes treated with and without microfractures during the arthroscopic treatment of femoroacetabular impingement. The two study groups presented no significant differences when resuming their sports activities.
In 2016, Marquez-Lara et al. 26 published a systematic review of indications, outcomes and postoperative-treatment rehabilitation protocols using microfractures in patients with chondral
lesions secondary to femoroacetabular impingement. Twelve studies (11 out of 12 studies) showed good post-microfracture results in 267 patients (except one publication of a case report with one clinical case). As an indication for microfractures, the vast majority considered full-thickness focal chondral lesions. Most publications also recommend some degree of weight-bearing protection in postoperative rehabilitation, nevertheless rehabilitation protocols vary significantly.
In 2015 Fontana and de Girolamo 27 published a study comparing the clinical results after five-year follow-up of microfracture with a technique of enhanced microfracture autologous matrix-induced chondrogenesis (autologous matrix-induced chondrogenesis) for acetabular chondral lesions grades 3 and 4. The outcome in both groups was significantly improved at six months and one year postoperatively. During the subsequent four years the outcome in the microfracture autologous matrix-induced chondrogenesis group deteriorated slowly, whereas that in the autologous matrix-induced chondrogenesis group remained stable. They conclude that at the short term clinical outcomes improve in both microfracture autologous matrix-induced chondrogenesis and autologous matrix-induced chondrogenesis groups. However, the autologous matrix-induced chondrogenesis group had better and more durable improvement.
In summary, studies confirm good short- and medium-term results in full-thickness chondral lesions treated with microfracture, in the absence of osteoarthritis 28. However, it is difficult to determine if these results are only due to the microfractures, as this treatment is always related to several other factors and surgical procedures, such as labrum repair, correction of underlying bone deformity or change in postoperative activity (Impact sports reduction) of operated patients.
References- Frisbie DD, Trotter GW, Powers BE, Rodkey WG, Steadman JR, Howard RD et al. Arthroscopic subchondral bone plate microfracture technique augments healing of large osteochondral defects in the radial carpal bone and medial femoral condyle of horses. J Vet Surg 1999; 28:242-255.
- Mella, C., Núñez, A., & Villalón, I.E. (2017). Treatment of acetabular chondral lesions with microfracture technique. SICOT-J. https://pdfs.semanticscholar.org/b729/1ccd704e1a90191f0ca30f6840d05545d428.pdf
- El Bitar Y, Lindner D, Jackson T, Domb B (2014) Joint-preserving surgical options for management of chondralinjuries of the hip. J Am Acad Orthop Surg 22(1), 46–56.
- Steadman JR. The microfracture technique. In: The crucial principles in care of the knee. Philadelphia: Lippincott Williams & Wilkins 2007.
- Steadman JR, Rodkey WG, Briggs KK. Microfracture: its history and experience of the developing surgeon. Cartilage 2010; 1:78-86.
- Frisbie DD, Morisset S, Ho CP, Rodkey WG, Steadman JR, McIlwraith CW. Effects of calcified cartilage on healing of chondral defects treated with microfracture in horses. Am J Sports Med 2006; 34:24-31.
- Frisbie DD, Oxford JT, Southwood L, Trotter GW, Rodkey WG, Steadman JR et al. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop 2003; 407:215-227.
- Rodrigo JJ, Steadman JR, Silliman JF, Fulstone HA. Improvement of full-thickness chondral defect healing in the human knee after debridement and microfracture using continuous passive motion. Am J Knee Surg 1994; 7:109-116.
- Steadman JR, Dragoo J, Hines S, Briggs KK. Arthroscopic release for symptomatic scarring of the anterior interval of the knee. Am J Sports Med 2008; 36:1763-1769.
- Fontana A, Bistolfi A, Crova M, Rosso F, Massazza G (2012)Arthroscopic treatment of hip chondral defects: autologouschondrocyte transplantation versus simple debridement, a pilotstudy. Arthroscopy 28, 322–329.
- Mancini D, Fontana A (2014) Five-year results of arthroscopictechniques for the treatment of acetabular chondral lesions infemoroacetabular impingement. Int Orthop 38(10), 2057–2064.
- Hurst JM, Steadman JR, O’Brien L, Rodkey WG, Briggs KK. Rehabilitation following microfracture for chondral injury in the knee. Clin Sports Med 2010; 29:257-265.
- Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 2003; 19:477-484.10. Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grøntvedt T, Solheim E. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am 2004; 86:455-464.
- Outcomes of microfracture for traumatic chondral defects of the knee: Average 11-year follow-up”, Steadman et al., Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 19, No 5 (May–June), 2003: pp 477–484
- Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grøntvedt T, Solheim E. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am 2004; 86:455-464.
- Knutsen G, Drogset JO, Engebretsen L, Grøntvedt T, Isaksen V, Ludvigsen TC, et al. A randomised trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 2007; 89:2105-2112.
- Steadman JR, Miller BS, Karas SG, Schlegel TF, Briggs KK, Hawkins RJ. The microfracture technique in the treatment of full-thickness chondral lesions of the knee in National Football League players. J Knee Surg 2003; 16:83-8
- Steadman JR, Hanson CM, Briggs KK, Matheny LM, James EW, Guillet A. Outcomes after knee microfracture of chondral defects in alpine ski racers. J Knee Surg 2014; 27:407-410.
- Steadman JR, Briggs KK, Matheny LM, Guillet A, Hanson CM, Willimon SC. Outcomes following microfracture of full-thickness articular cartilage lesions of the knee in adolescent patients. J Knee Surg 2015; 28:145-150.
- Philippon MJ, Schenker ML, Briggs KK, Maxwell RB (2008)Can microfracture produce repair tissue in acetabular chondraldefects? Arthroscopy 24(1), 46–50.
- Byrd JW, Jones KS (2009) Arthroscopic femoroplasty in themanagement of cam type femoroacetabular impingement. ClinOrthop Relat Res 467(3), 739–746.
- Karthikeyan S, Roberts S, Griffin D (2012) Microfracture foracetabular chondral defects in patients with femoroacetabularimpingement: results at second-look arthroscopic surgery. Am JSports Med 40(12), 2725–2730.
- Domb BG, El Bitar YF, Lindner D, Jackson TJ, Stake CE(2014) Arthroscopic hip surgery with a microfracture proce-dure of the hip: clinical outcomes with two-year follow-up. HipInt 24(5), 448–456.
- Domb BG, Redmond JM, Dunne KF, Stake CE, Gupta A(2015) A matched-pair controlled study of microfracture of thehip with average 2-year follow-up: do full-thickness chondraldefects portend an inferior prognosis in hip arthroscopy?Arthroscopy 31(4), 628–634.
- McDonald JE, Herzog MM, Philippon MJ (2013) Return toplay after hip arthroscopy with microfracture in elite athletes.Arthroscopy 29(2), 330–335.
- Marquez-Lara A, Mannava S, Howse E, Stone A, Stubbs A(2016) Arthroscopic management of hip chondral defects: Asystematic review of the literature. Arthroscopy 32(7), 1435–1443.
- Fontana A, de Girolamo L (2015) Sustained five-year benefit ofautologous matrix-induced chondrogenesis for femoral acetab-ular impingement-induced chondral lesions compared withmicrofracture treatment. Bone Joint J 97-B(5), 628–635
- Mella C, Nuñez A & Villalón I (2017) Treatment of acetabular chondral lesions with microfracture technique. SICOT J,3,45. https://pdfs.semanticscholar.org/b729/1ccd704e1a90191f0ca30f6840d05545d428.pdf