What is Mondor’s disease
Mondor’s disease also known as Mondor’s cord, is a rare self-limited, benign sclerosing superficial thrombophlebitis (vein inflammation caused by a blood clot) of the veins of the anterior thoracic wall that usually resolves in four to eight weeks without any specific treatment 1. Almost all cases of Mondor’s disease are reported to be thrombophlebitis of the superficial vein, although some are reported to be lymphangitis and/or a combination of both the causes 2. Mondor’s disease manifests with a palpable cord-like induration beneath the skin. Cases with cord-like lesions on the chest wall were first reported in the early 1850s, and Henri Mondor, a French surgeon, reported a case series and described them in detail in 1939 3. Subsequently, similar cord-like indurations occurring at the abdominal wall, groin, axilla, and penis were also reported. Although no formal classification has yet been established, Mondor’s disease on the anterolateral thoracoabdominal wall is generally recognized as original Mondor’s disease, while similar abnormalities on other sites, such as the penis and axilla, are recognized as variants of Mondor’s disease. The former is called penile Mondor’s disease with dorsum and dorsolateral aspects of the penis – first reported by Helm et al. in 1958 4 and the latter is called axillary web syndrome of mid-upper arm, first reported as a complication of axillary surgery by Moskovitz et al. in 2001 5. The diagnosis of Mondor’s disease is rather straightforward and based on a physical examinations. However, some case occur “secondary” with another underlying disease, including malignancy, a hypercoagulative state, and vasculitis. The potential link of Mondor’s disease with underlying malignancy, hypercoagulable state or systemic vasculitis warrants a greater vigilance on the part of your health care providers.
A recent literature review by Amano et al. 6 revealed 45% of cases to be idiopathic, 20% iatrogenic, 22% traumatic and 5% about breast cancer. The most commonly involved vessel is the superior epigastric vein producing a palpable cord in the inferior outer quadrant of the breast 6. Mondor’s disease on the chest wall is often diagnosed in women at breast clinics, penile Mondor’s disease at urology clinics, and axillary web syndrome at surgery or breast clinics 1.
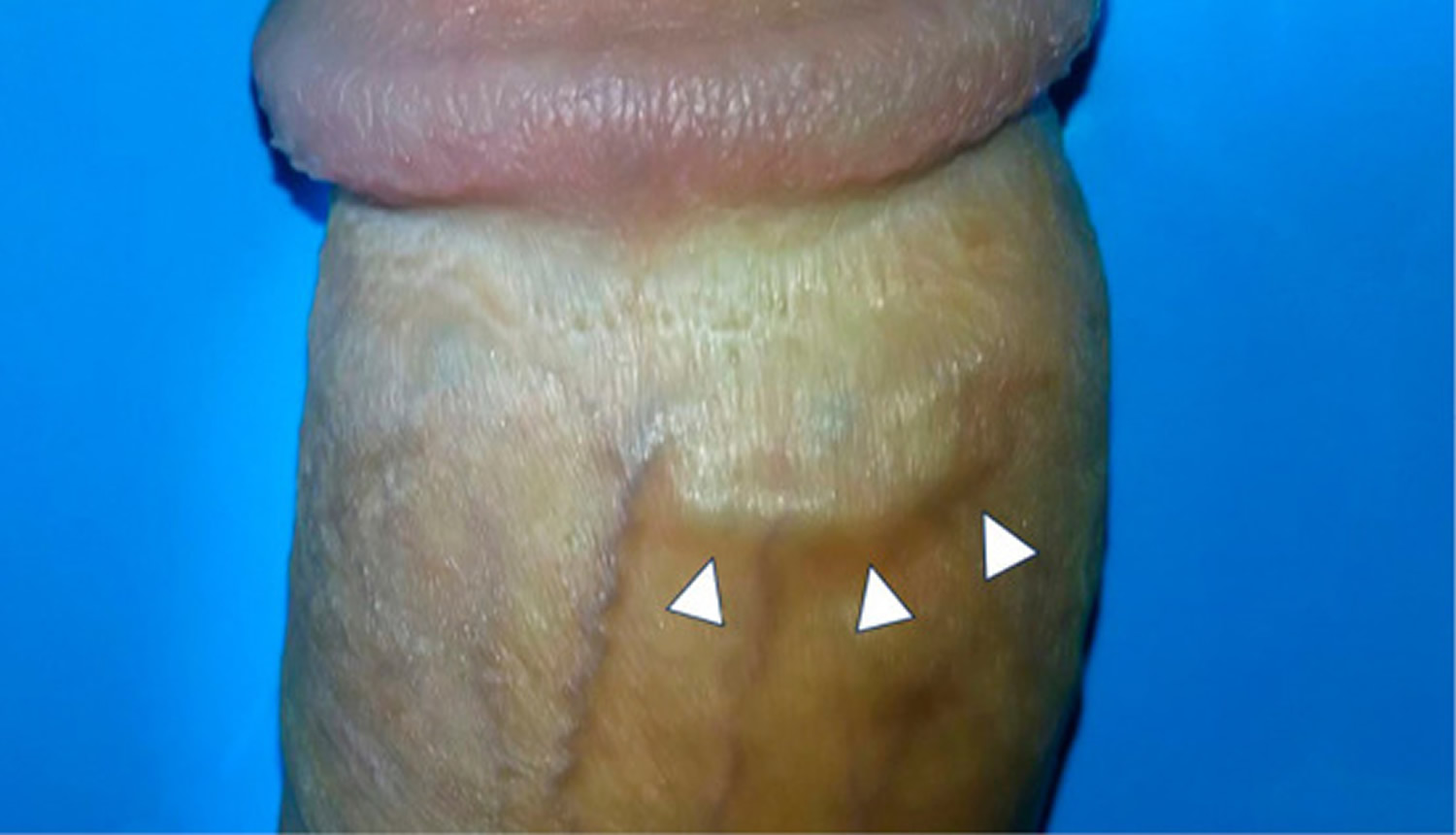
Figure 1. Penile Mondor’s disease
Footnote: A 28-year-old man with no significant past medical history presented with a 2-day history of cord like lesion on his penis. He said that he had vigorous sex with his wife 7 days before presentation; he denied fever, trauma, nor discharge from urethra. Physical examination revealed a 15-millimeter hard subcutaneous cord like lesion on his penis. Blood test detected no abnormality suggesting underlying diseases. Diagnosis of penile Mondor’s disease was made, and the lesion resolved within 2 weeks only with sexual abstinence. No recurrence nor erectile dysfunction was observed during 2-year follow up period.
[Source 1 ]Figure 2. Mondor’s disease breast
Mondor’s disease causes
Despite many years having lapsed since its first report, the details of Mondor’s disease remain unclear due to its rarity. There are less than 400 reported cases of Mondor Disease in medical literature 7. Many case reports have linked sclerosing superficial thrombophlebitis and the resulting palpable cord to local trauma including such repetition injury as a tight brassier, strenuous exercise in the case of bodybuilders or direct injury associated with surgery 8. Other causes include direct damage to the veins, stagnation of blood, or extrinsic pressure on veins. Cases of Mondor Disease have been reported after cosmetic mammoplasty, mastectomy and breast-conserving surgery for breast cancer and after core needle biopsy 9. Prior authors have highlighted an association between Mondor’s Cord as a sign of underlying breast pathology and recommend ruling out breast cancer through appropriate imaging before expectant management, however, no direct correlation has been proven.
Mondor disease can affect several different venous drainage systems. However, it never involves in the inner, upper portion of the breast. Symptoms may be found in the groin, abdomen, arm or axilla. Axillary disease, also known as axillary web syndrome, has been well documented following axillary lymph node dissection and sentinel lymph node biopsy for breast cancer 10. Penile Mondor disease has also been described, while its pathogenesis is incompletely understood, this rare entity involves near-painless cords on the dorsal aspect of the penis 11.
Mondor’s disease pathophysiology
The pathogenesis of Mondor’s disease has been unclear for some time. It was previously difficult to distinguish obstructed small blood vessels from damaged small lymph vessels using conventional histopathological methods. The application of recently developed immunohistochemical markers revealed that almost all Mondor’s diseases appeared to be thrombophlebitis of the superficial vein, while some cases occurred due to lymphangitis 2. The combination of polyclonal antibody against human lymphatic vessel endothelial hyaluronan receptor-1 (LYVE-1)-a marker for the lymph vessel-and von Willebrand factor antibody-a conventional marker of the blood vessels-can clearly distinguish between these two vessels. In addition, sclerosing lymphangitis of the penis, which is clinically identical to penile Mondor’s disease, was found to be thrombophlebitis in most cases using monoclonal antibodies against CD31 and CD34 12.
The pathophysiology of axillary web syndrome is unestablished. It was originally reported to be a combination of thrombosed vein and lymphatics 13. Some authors believe it to be a lymphatic pathogenesis with superficial fascia 14, while others argue that it is a microlymphatic stasis or binding of fibrin or other proteins in the interstitial space, based on their ultrasonographic findings 15. The detailed analysis of axillary web syndrome with immunohistochemical method has not yet been reported.
The progression of phlebitis includes some pathophysiological steps in developing Mondor’s disease. At the initial stages, thrombotic events occur in the affected veins. As a result, the lumen often becomes occluded with fibrin and inflammatory cells. Subsequently, the connective tissue gathering in the vessel forms a hard, cord-like induration. Thereafter, recanalization proceeds for several weeks until establishment 16.
Mondor’s disease symptoms
As Mondor’s disease lesions are composed of an occluded subcutaneous veins, acutely arising cord-like palpable indurations on the body surface are its only clinical manifestation. The skin itself shows ample elasticity and limited inflammatory changes. Indurations commonly appear longitudinally on the anterolateral thoracoabdominal wall because of its rich, vertically oriented superficial vein network 16. As such, a transverse surgical incision during breast augmentation or wearing tight bras can affect this system, resulting in induration at the inframammary site 17.
In penile Mondor’s disease, the induration appears on the dorsal and dorsolateral aspects of the penis due to the involvement of an inferior part of the superficial vein system of the abdominal wall (Figure 1) 18. The circumflex vein can also be affected, which some authors claim to be a case of atypical penile Mondor’s disease 19.
In axillary web syndrome, induration arises at the distal parts of the axially surgical scar and extends for any length from the mid-upper arm to the base of the thumb 20. Pain was experienced in approximately 40% of patients with restriction of the shoulder abduction 21.
Some Mondor’s disease patients suffer from pain, tightness, erythematous skin change, a fever, and discomfort during movement 22. In addition, some patients experience anxiety because of its unfamiliar appearance, especially when the lesion occurs on the penis 23. When Mondor’s disease occurs secondary to an underlying cause, such as giant-cell arteritis or other vasculitis, concomitant symptoms, including a high-grade fever or malaise, may be present 24.
Mondor’s disease diagnosis
The diagnosis of Mondor disease is a clinical one confirmed by history and physical alone. With so few cases represented in the medical literature, there is no accepted consensus on evaluation or management. While some authors have suggested a link between underlying breast cancer and Mondor disease, others have denied this link and attribute the coexistence of disease to the direct or indirect trauma associated with the diagnosis and treatment of the underlying malignancy 25. In patients with a classic story and no other systemic complaints and otherwise regular physical exam, it is reasonable to proceed without a laboratory, radiographic or another invasive testing for diagnosis. In those patients with signs or symptoms suggestive of underlying pathology further evaluation with either mammography of the breast or ultrasound of the breast or penis is warranted 26.
In cases where the clinical picture is not definitive, ultrasound is considered the first line in the imaging evaluation of Mondor’s disease. Ultrasound in the location of the patient’s area of palpable concern will show a non-compressible, hypoechoic tubular structure which is the superficial vein. An area of intraluminal thrombus may or may not be visible 27. Color Doppler should be used to confirm the diagnosis by demonstrating the absence of flow within the vein 28. Mammography may be inconclusive, or it may reveal a linear density in the breast in patients with superficial thrombophlebitis. MRI and other advanced imaging techniques are generally not indicated in the evaluation of Mondor’s disease 29.
Mondor’s disease treatment
Supportive care and expectant management are sufficient in most cases of Mondor’s disease. Warm compresses, nonsteroidal anti-inflammatory medications, and abstinence from irritating clothing or activities are first-line therapy 30. Most lesions will resolve with cessation of discomfort and dissolution of the palpable cord 31. Treatment with low molecular weight heparin or aspirin has been reported in some case series; this is not recommended in patients without an underlying hypercoagulable state inciting superficial thrombophlebitis and associated Mondor’s Cord. intralesional triamcinolone injections for a Mondor’s cord after breat augmentation has been successful in shortening Mondor’s disease 32.
Mondor’s disease prognosis
Mondor’s disease is usually a self-limited condition resolving in six to eight weeks. The prognosis of secondary Mondor’s disease where the situation is secondary to a hypercoagulable state, the prognosis is directly linked to the prognosis of the underlying disease. As with any thromboembolic disease there is a small chance of the development of a deep venous thrombosis (DVT).
The long-term prognosis of Mondor’s disease has not yet been reported. A previous study noted that 4 patients with chest Mondor’s disease showed a good clinical course without recurrence for almost 3 years, while another reported 3 of 23 chest Mondor’s disease patients continued to suffer from recurrence for 9 years 33. However, only a few patients with PMondor’s disease experience chronic pain and priapism, and almost all are free from symptoms 34. With regard to the functional prognosis of PMondor’s disease, which is a considerable concern among young patients, a study on 30 PMondor’s disease patients reported no permanent deformity of the penis or erectile dysfunction after 2 months of follow-up 35. The relationship between Mondor’s disease and other sites of superficial thrombophlebitis remains unclear, but such lesions are considered an initial manifestation of generalized thrombophlebitis 36.
References- Amano M, Shimizu T. Mondor’s Disease: A Review of the Literature. Intern Med. 2018;57(18):2607–2612. doi:10.2169/internalmedicine.0495-17 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6191595
- Ichinose A, Fukunaga A, Terashi H, et al. Objective recognition of vascular lesions in Mondor’s disease by immunohistochemistry. J Eur Acad Dermatol Venereol 22: 168-173, 2008.
- Hokama A, Fujita J. Mondor disease: an unusual cause of chest pain. South Med J 103: 1189, 2010.
- Helm JD Jr, Hodge IG. Thrombophlebitis of a dorsal vein of the penis: report of a case treated by phenylbutazone (Butazolidin). J Urol 79: 306-307, 1958
- Moskovitz AH, Anderson BO, Yeung RS, Byrd DR, Lawton TJ, Moe RE. Axillary web syndrome after axillary dissection. Am J Surg 181: 434-439, 2001
- Amano M, Shimizu T. Mondor’s Disease: A Review of the Literature. Intern. Med. 2018 Sep 15;57(18):2607-2612.
- Quéhé P, Saliou AH, Guias B, Bressollette L. [Mondor’s disease, report on three cases and literature review]. J Mal Vasc. 2009 Feb;34(1):54-60.
- Tröbinger C, Wiedermann CJ. Bodybuilding-induced Mondor’s disease of the chest wall. Phys Ther Sport. 2017 Jan;23:133-135.
- Goldman A, Wollina U. Mondor’s Disease after Aesthetic Breast Surgery: A Case Series and Literature Review. J Cutan Aesthet Surg. 2018 Jul-Sep;11(3):132-135.
- Koehler LA, Haddad TC, Hunter DW, Tuttle TM. Axillary web syndrome following breast cancer surgery: symptoms, complications, and management strategies. Breast Cancer (Dove Med Press). 2019;11:13-19.
- Marsaudon E, Legal C, Gayoux D, Weber O. [Mondor’s disease of penis: A case report]. Rev Med Interne. 2016 Sep;37(9):636-8.
- Kumar B, Narang T, Radotra BD, Gupta S. Mondor’s disease of penis: a forgotten disease. Sex Transm Infect 81: 480-482, 2005.
- Moskovitz AH, Anderson BO, Yeung RS, Byrd DR, Lawton TJ, Moe RE. Axillary web syndrome after axillary dissection. Am J Surg 181: 434-439, 2001.
- Salmon RJ, Berry M, Hamelin JP. A novel treatment for postoperative mondor’s disease: manual axial distraction. Breast J 15: 381-384, 2009.
- Koehler LA, Hunter DW, Haddad TC, et al. Characterizing axillary web syndrome: ultrasonographic efficacy. Lymphology 47: 156-163, 2014.
- Alvarez-Garrido H, Garrido-Ríos AA, Sanz-Muñoz C, Miranda-Romero A. Mondor’s disease. Clin Exp Dermatol 34: 753-756, 2009.
- Khan UD. Incidence of mondor disease in breast augmentation: a retrospective study of 2052 breasts using inframammary incision. Plast Reconstr Surg 122: 88-89, 2008.
- Mayor M, Buro´n I, Calvo-Mora J, et al. Mondor’s disease. Int J Dermatol 39: 922-925, 2000.
- Arora R, Sonthalia S, Gera T, Sarkar R. A typical penile Mondor’s disease – involvement of the circumflex vein. Int J STD AIDS 26: 360-363, 2015.
- Schuitevoerder D, White I, Fortino J, Vetto J. Axillary web syndrome: an underappreciated complication of sentinel node biopsy in melanoma. Am J Surg 211: 846-849, 2016.
- Figueira PVG, Haddad CAS, de Almeida Rizzi SKL, Facina G, Nazario ACP. Diagnosis of axillary web syndrome in patients after breast cancer surgery: epidemiology, risk factors, and clinical aspects: a prospective study. Am J Clin Oncol 2017(Epub ahead of print).
- Belleflamme M, Penaloza A, Thoma M, Hainaut P, Thys F. Mondor disease: a case report in ED. Am J Emerg Med 30: 1-3, 2012.
- Polat H, Yucel MO, Gok A, Benlioglu C, Cift A, Sarica MA. Penile Mondor’s disease: primum non nocere! Urol J 12: 2096-2098, 2015.
- Diamantopoulos EJ, Yfanti G, Andreadis E. Giant-cell arteritis presenting as Mondor disease. Ann Intern Med 130: 78-79, 1999.
- Halkier E, Bødker A. Mondor’s disease: a review of five cases. Acta Chir Scand. 1983;149(3):333-4.
- Nazir SS, Khan M. Thrombosis of the dorsal vein of the penis (Mondor’s Disease): A case report and review of the literature. Indian J Urol. 2010 Jul;26(3):431-3.
- Salemis NS, Merkouris S, Kimpouri K. Mondor’s disease of the breast. A retrospective review. Breast Dis. 2011;33(3):103-7
- Kim HS, Cha ES, Kim HH, Yoo JY. Spectrum of sonographic findings in superficial breast masses. J Ultrasound Med. 2005 May;24(5):663-80.
- Adeniji-Sofoluwe A, Afolabi O. Mondor’s disease: classical imaging findings in the breast. BMJ Case Rep. 2011 Aug 19;2011
- Rountree KM, Barazi H, Aulick NF. Mondor Disease. [Updated 2019 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538282
- Pasta V, D’Orazi V, Sottile D, Del Vecchio L, Panunzi A, Urciuoli P. Breast Mondor’s disease: Diagnosis and management of six new cases of this underestimated pathology. Phlebology. 2015 Sep;30(8):564-8.
- Shah NA, Gryskiewicz J, Crutchfield CE. Successful Treatment of a Recalcitrant Mondor’s Cord Following Breast Augmentation. J Clin Aesthet Dermatol. 2014 Apr;7(4):50-1.
- Salemis NS, Merkouris S, Kimpouri K. Mondor’s disease of the breast. A retrospective review. Breast Dis 33: 103-107, 2011.
- Zidani H, Foughali M, Laroche JP. Superficial venous thrombosis of the penis: Penile Mondor’s disease? A case report and literature review. J Mal Vasc 35: 352-354, 2010.
- Özkan B, Coskuner ER, Turk A, Akkus E, Yalçın V. Penile Mondor disease and its effect on erectile function: results of 30 patients. Urology 85: 113-117, 2015.
- José Luis RP, Rosario C, Belén R, Yolanda RG. Superficial thrombophlebitis. Semin Cutan Med Surg 26: 71-76, 2007