Morvan syndrome
Morvan syndrome or Morvan’s fibrillary chorea, is a rare constellation of neurological symptoms, consisting of peripheral nerve hyperexcitability, autonomic instability, and encephalopathy often associated with autoantibodies to voltage-gated potassium channel complexes (anti – VGKC-Ab) 1. Contactin associated protein-like 2 antibodies (CASPR2-Ab) and leucine-rich glioma inactivated protein 1 antibodies (LGI1-Ab) were previously known for the potential association with Morvan syndrome 2.
The occurrence of Morvan syndrome is quite rare. Based on the published literature, Morvan syndrome is almost exclusively seen in males. This male preponderance is quite intriguing. One report has shown CASPR2 protein-coding mRNA in the prostate gland, which supports the possibility that the male reproductive system may also harbor these antigens besides brain tissue. This finding was consistent with the onset of Morvan syndrome in a few patients after scrotal drainage as reported by Irani et al. 3.
Morvan’s syndrome causes
Initially, a precise cause of Morvan syndrome was not completely understood. Occasional reports of heavy metal poisoning like gold 4, manganese 5, and mercury 6 were implicated in its etiology and pathogenesis. Association with elevated cerebrospinal fluid (CSF) IgG and oligoclonal bands 7, thyrotoxicosis 8 and autoimmune hypothyroidism 9, clinical or subclinical myasthenia, certain neoplasms like thymoma 10, small-cell lung cancer, teratoma, prostate adenoma, and carcinoma in situ of the colon 11, have also been implicated in its etiopathogenesis. Neuromyotonia alone occurring without any suggestion of central nervous system (CNS) or autonomic nervous system (ANS) involvement has been reported in association with Staphylococcus aureus infection in one case 12. Another case following Legionnaire disease 13 and one associated with antibodies to N-type calcium channel has also been published 11. Older reports have implicated lesions in the diencephalon, basal ganglia and raphe nuclei in the brain and abnormalities in central serotonin metabolism 10.
However, presently, there is overwhelming evidence that strongly supports an autoimmune basis in its etiology where strong association with autoantibodies to voltage-gated potassium channel complex (VGKCs) 14 are identified. It has become reasonably clear that voltage-gated potassium channel complex antibodies are mainly directed against proteins that are an integral part of VGKC complexes in brain tissue. Proteins such as contactin-associated protein 2 (CASPR2) and leucine-rich glioma inactivated (1LGI1) were identified as primary targets for autoantibodies 15.
The first identified antibody target within the voltage-gated potassium channel complex was CASPR2 in patients with Morvan syndrome. Subsequently, LGI1 was also recognized as an additional and significant target in a few cases with Morvan syndrome and also limbic encephalitis. In addition, a minority of patients have antibodies directed against the third identified antigenic component of the voltage-gated potassium channel complex, namely contactin-2 10.
Morvan syndrome pathophysiology
As mentioned earlier antibodies against VGKC complex proteins, CASPR2, and LGI1 are now strongly implicated in the pathogenesis of Morvan syndrome[11][23]. There is experimental evidence that these antibodies can cause neuronal hyperexcitability by suppressing voltage-gated potassium outward currents needed for the repolarization of the motor nerve. Immunostaining of brain tissue showed that these antibodies target subtly different regions of the brain that is likely to be involved in the localization of the distinctive clinical features seen in Morvan syndrome.
CASPR2 antibodies are predominantly seen in Morvan syndrome and were often found in association with thymoma cases also. Furthermore, thymectomy and thymoma chemotherapy are likely to trigger the onset of Morvan syndrome which supports the possibility that thymic tumors shelter antigenic targets, particularly CASPR2, and become somehow exposed and potentially vulnerable to antibody attack following thymectomy or thymoma chemotherapy.
The various combinations of LGI1 and CASPR2 antibody binding in Morvan syndrome could contribute to the distinctive multifocal phenotype.
Monoaminergic diencephalic and brainstem nuclei are known to be involved in arousal, and autonomic homeostasis. A disturbance in this homeostasis can cause insomnia, dysautonomia, and less frequently hyponatremia.
Dysfunction in the neurons anywhere in the thalamus, hypothalamus, locus coeruleus, and raphe nuclei could produce insomnia.
The dysautonomia noted in Morvan syndrome is likely generated within the hypothalamus and raphe nuclei.
However, syndrome of inappropriate antidiuretic hormone secretion (SIADH) related hyponatremia was sometimes found in patients with LGI1 antibodies. The LGI1 antibody binds to hypothalamic paraventricular neurons that produce antidiuretic hormone secretion (ADH), which mediates water retention. This suggests that LGI1 antibody binding may increase ADH secretion which in turn causes hyponatremia, although some patients with CASPR2 antibodies do have low plasma sodium due to some unknown mechanism.
It was found that LGI1 or CASPR2 antibodies bind to all these regions and possibly have variable specificities at subcellular level that may determine the relative functional significance of each antibody. Besides the target antigen distribution, other factors, including the accessibility to circulating antibodies and physiological properties of neuronal populations, may also determine the clinical manifestations.
As mentioned earlier in etiology some patients did also have anti contactin-2 antibodies, which are only rarely found in limbic encephalitis; contactin-2 is expressed in cardiac conduction tissue and some reports that found anti contactin-2 antibodies had had cardiovascular instability. Some other patients had reactivities to antigenic targets that were not consistent with LGI1, CASPR2, or contactin-2, leading to the suspicion that different antibody reactivities are present in, at least, some of these patients. Therefore, to facilitate further understanding, more research and data are needed.
Morvan’s syndrome symptoms
Morvan syndrome or Morvan’s fibrillary chorea, is a rare constellation of neurological symptoms, consisting of peripheral nerve hyperexcitability, autonomic instability, and encephalopathy often associated with autoantibodies to voltage-gated potassium channel complexes (anti – VGKC-Ab) 1.
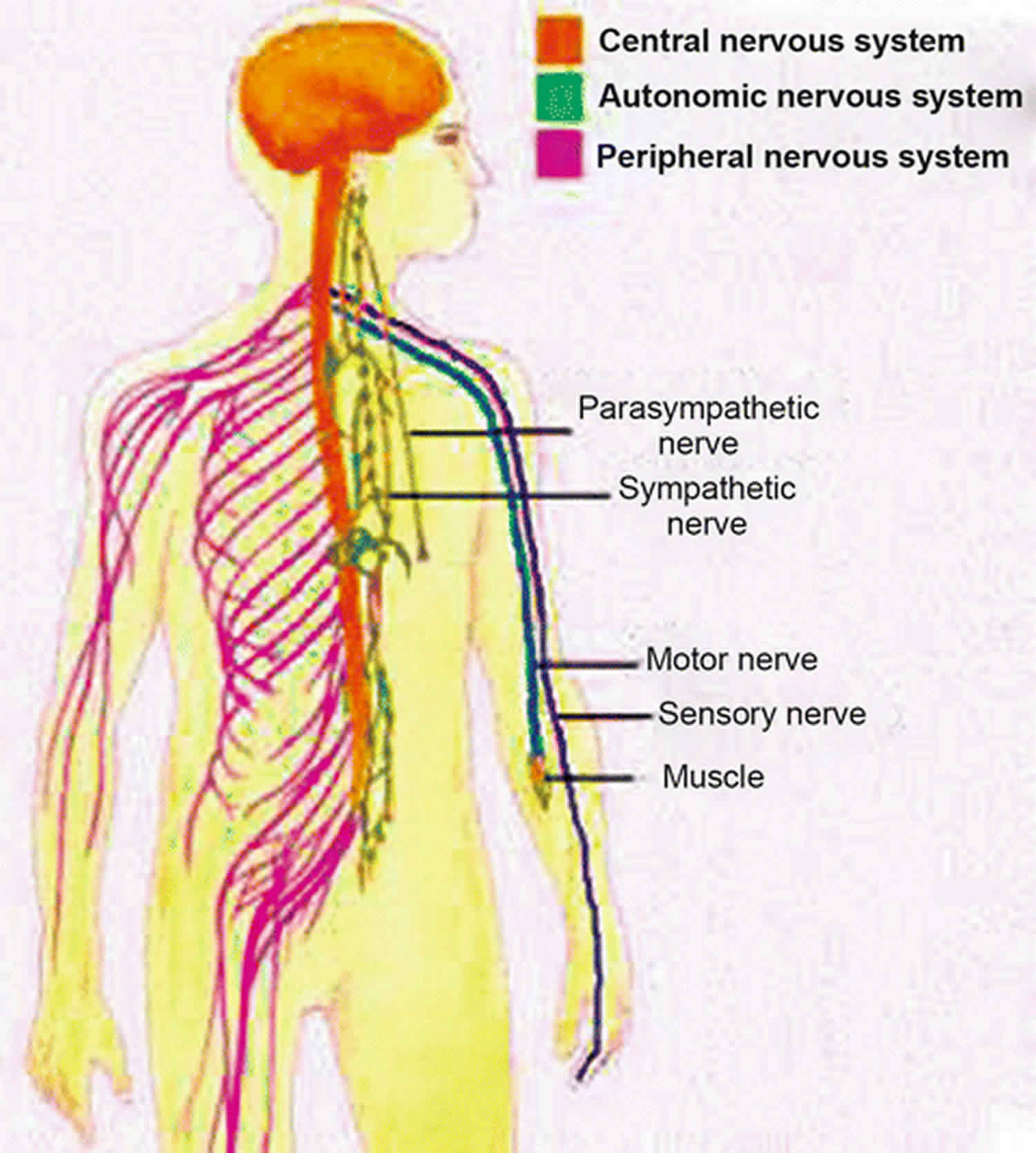
Morvan syndrome is mainly a clinical diagnosis 9. Morvan syndrome is characterized by features caused by central, autonomic and peripheral nervous system hyperactivity 16.
- The central nervous system (CNS) features include encephalopathy, severe insomnia, vivid complex hallucinations, delirium, spatial and temporal disorientation, confusion, amnesia, agitation, and belligerence.
- The autonomic nervous system (ANS) features, due to autonomic instability, are excessive sweating, fever, palmoplantar erythema, pruritus, drooling, severe constipation, excessive lacrimation, arrhythmias, hypertension, weight loss, skin and rarely hyponatremia due to the syndrome of inappropriate antidiuretic hormone secretion 17.
- The peripheral nervous system (PNS) features are peripheral nerve hyperexcitability resulting in continuous muscle fiber activity, neuropathic pain, areflexia (loss of deep tendon reflexes), and a stocking-type sensory loss. Continuous muscle fiber activity is manifested as neuromyotonia which is clinically seen as myokymia 18.
These comprise most of the possible symptoms of Morvan syndrome. However, it is less likely for an individual patient to manifest all the above clinical features. The varied occurrence of the clinical features of the syndrome may depend on the type of antibody detected either anti-CASPR2 or anti-LGI1 or both or some other antibodies.
The presence of tumors (especially thymoma), weight loss, and additional antibodies directed toward the acetylcholine receptor are found in association with CASPR2 antibodies. Whereas, serum hyponatremia and delusions, as well as myoclonus, are more common in the presence of LGI1 antibodies.
Morvan’s syndrome diagnosis
Morvan syndrome is a clinical diagnosis. A high index of clinical suspicion is needed to diagnose Morvan syndrome when a patient presents with a combination of above mentioned diverse clinical features. Most of the investigations that are usually performed in such patients, such as CSF analysis, brain MRI, EEG, PET scan, are typically unyielding. EMG studies can confirm myokymia. However, the detection of VGKC-complex antibodies is quite diagnostic. Although these antibodies are directed against CASPR2, LGI1, or more commonly both, CASPR2 antibodies predominance is found in association with thymoma cases.
Morvan syndrome treatment
Clinicians have tried several treatment modalities with variable clinical response (see also table 1). These include gold therapy, antiepileptic agents such as carbamazepine, valproate, phenobarbital, phenytoin, and procedures such as thymectomy.
However, plasma exchange appears to be the most effective treatment available for Morvan syndrome as seen in several cases, besides immunosuppression 9. Immunosuppression is a patient response based, and it is usually the initial treatment modality tried before plasma exchange. Due to unclear reasons, clinical response to plasma exchange and immunosuppression is also variable. It is probably related to the varied serum factors responsible for causing symptoms in mixed patient populations. Some authors postulate that with Morvan syndrome associated with other autoimmune conditions like myasthenia and autoimmune thyroid disorders, immunosuppression is more effective.
Morvan syndrome prognosis
The natural history of Morvan syndrome is variable. Some cases have been reported to remit spontaneously, and some required extensive treatment, mainly in the form of immunotherapy including plasma exchange and long-term immunosuppression. Some cases were fatal. The overall prognosis of Morvan syndrome was particularly poor when associated with thymoma.
References- Masood W, Sitammagari KK. Morvan Syndrome (Morvan Fibrillary Chorea, MFC) [Updated 2019 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507887
- Demirbas S, Aykan MB, Zengin H, Mazman S, Saglam K. Morvan syndrome: a rare cause of syndrome of inappropriate antidiuretic hormone secretion. Clujul Med. 2017;90(3):353–355. doi:10.15386/cjmed-755 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5536216
- Morvan syndrome: clinical and serological observations in 29 cases. Ann Neurol. 2012 Aug;72(2):241-55. doi: 10.1002/ana.23577. Epub 2012 Apr 4. https://doi.org/10.1002/ana.23577
- Vernay D, Dubost JJ, Thevenet JP, Sauvezie B, Rampon S. “Chorée fibrillaire de Morvan” followed by Guillain-Barré syndrome in a patient receiving gold therapy. Arthritis Rheum. 1986 Nov;29(11):1413-4.
- Haug BA, Schoenle PW, Karch BJ, Bardosi A, Holzgraefe M. Morvan’s fibrillary chorea. A case with possible manganese poisoning. Clin Neurol Neurosurg. 1989;91(1):53-9.
- Gil R, Lefèvre JP, Neau JP, Guillard O, Hulin A. [Morvan’s fibrillary chorea and acrodynic syndrome following mercury treatment]. Rev. Neurol. (Paris). 1984;140(12):728-33.
- Liguori R, Vincent A, Clover L, Avoni P, Plazzi G, Cortelli P, Baruzzi A, Carey T, Gambetti P, Lugaresi E, Montagna P. Morvan’s syndrome: peripheral and central nervous system and cardiac involvement with antibodies to voltage-gated potassium channels. Brain. 2001 Dec;124(Pt 12):2417-26.
- HARMAN JB, RICHARDSON AT. Generalised myokymia in thyrotoxicosis report of a case. Lancet. 1954 Sep 04;267(6836):473-4.
- Josephs KA, Silber MH, Fealey RD, Nippoldt TB, Auger RG, Vernino S. Neurophysiologic studies in Morvan syndrome. J Clin Neurophysiol. 2004 Nov-Dec;21(6):440-5.
- Galié E, Renna R, Plantone D, Pace A, Marino M, Jandolo B, Koudriavtseva T. Paraneoplastic Morvan’s syndrome following surgical treatment of recurrent thymoma: A case report. Oncol Lett. 2016 Oct;12(4):2716-2719.
- Lee EK, Maselli RA, Ellis WG, Agius MA. Morvan’s fibrillary chorea: a paraneoplastic manifestation of thymoma. J. Neurol. Neurosurg. Psychiatry. 1998 Dec;65(6):857-62.
- Maddison P, Lawn N, Mills KR, Vincent A, Donaghy M. Acquired neuromyotonia in a patient with spinal epidural abscess. Muscle Nerve. 1998 May;21(5):672-4.
- Barber PA, Anderson NE, Vincent A. Morvan’s syndrome associated with voltage-gated K+ channel antibodies. Neurology. 2000 Feb 08;54(3):771-2.
- Cottrell DA, Blackmore KJ, Fawcett PR, Birchall D, Vincent A, Barnard S, Walls TJ. Sub-acute presentation of Morvan’s syndrome after thymectomy. J. Neurol. Neurosurg. Psychiatry. 2004 Oct;75(10):1504-5.
- Irani SR, Pettingill P, Kleopa KA, Schiza N, Waters P, Mazia C, Zuliani L, Watanabe O, Lang B, Buckley C, Vincent A. Morvan syndrome: clinical and serological observations in 29 cases. Ann. Neurol. 2012 Aug;72(2):241-55.
- Lotan I, Djaldetti R, Hellman MA, Benninger F. Atypical case of Morvan’s syndrome. J Clin Neurosci. 2016 Mar;25:132-4.
- Buckley C, Oger J, Clover L, Tüzün E, Carpenter K, Jackson M, Vincent A. Potassium channel antibodies in two patients with reversible limbic encephalitis. Ann. Neurol. 2001 Jul;50(1):73-8.
- Iwasaki Y, Kinoshita M, Ikeda K, Takamiya K, Shiojima T. Concurrence of myasthenia gravis and chorée fibrillaire de Morvan. Eur Arch Psychiatry Neurol Sci. 1990;239(5):335-6.