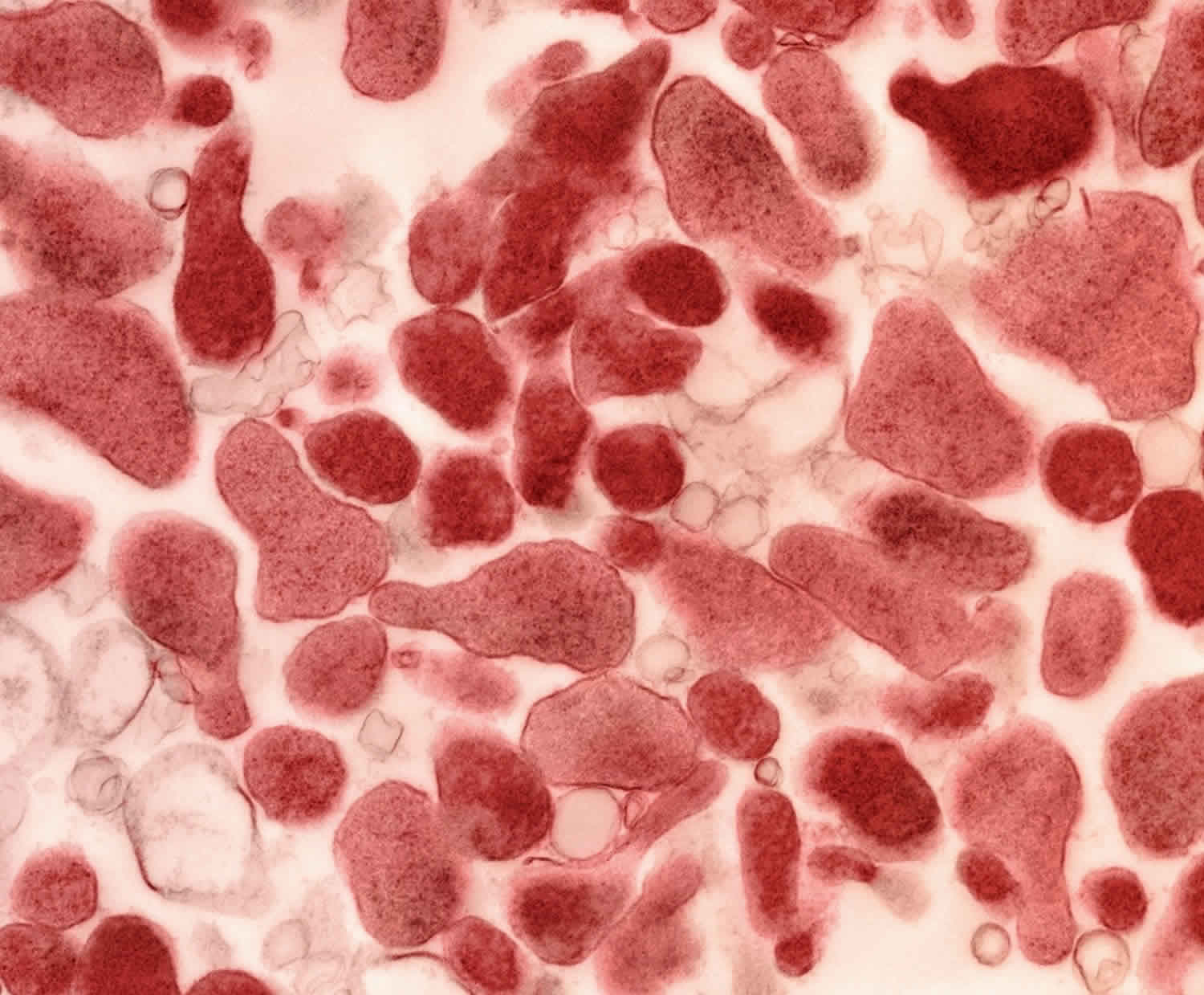
Mycoplasma genitalium
Mycoplasma genitalium or Mgen is a emerging sexually transmitted disease (STD) that can cause infections in both men and women 1, 2, 3. You can get mycoplasma genitalium by having vaginal, anal, and oral sex with someone who has the infection 4, 5. Mycoplasma genitalium can infect the cervix (opening to the uterus), inside the penis (the urethra), or the rectum.
According to the 2021 Guidelines for the Sexually Transmitted Infections Treatment issued by the United States Centers for Disease Control and Prevention, Mycoplasma genitalium infection can cause cervicitis (inflammation of the cervix) and pelvic inflammatory disease (PID) and 20%–30% of male urethritis cases (inflammation of the urethra) 6, 7, 8. A meta-analysis showed that M. genitalium infection was significantly associated with an increased risk of cervicitis, pelvic inflammatory disease, female infertility, preterm birth and spontaneous abortion 9. A recent meta-analysis from China showed that the infection rate of M. genitalium infection in pregnant women was 4.86%, and the M. genitalium infection rates in women with ectopic pregnancy, spontaneous abortion, induced abortion, and premature rupture of membranes were 13.01, 11.81, 6.11, and 12.63%, respectively 10. This suggests that the incidence of Mycoplasma genitalium infection in pregnant women with ectopic pregnancy, spontaneous abortion, and premature rupture of membranes is higher than that in other pregnant women 3.
Rectal infection with Mycoplasma genitalium has been reported among 1%–26% of men who have sex with men 11, 12, 13, 14 and among 3% of women 15. Rectal infections often are asymptomatic, although higher prevalence of M. genitalium has been reported among men with rectal symptoms. Similarly, although asymptomatic M. genitalium has been detected in the pharynx, no evidence exists of it causing oropharyngeal symptoms or systemic disease 8.
The recommended treatment for all cases of Mycoplasma genitalium infections includes a two-stage approach with doxycycline, followed by an additional agent (either moxifloxacin or azithromycin), ideally using resistance-guided therapy 16.
Recommended antibiotic regimens if M. genitalium resistance testing is available 16, 8:
- If macrolide sensitive: Doxycycline 100 mg orally 2 times/day for 7 days, followed by azithromycin 1 g orally initial dose, followed by 500 mg orally once daily for 3 additional days (2.5 g total)
- If macrolide resistant: Doxycycline 100 mg orally 2 times/day for 7 days followed by moxifloxacin 400 mg orally once daily for 7 days
Recommended antibiotic regimens if M. genitalium resistance testing is Not Available 16, 8:
- If M. genitalium is detected by an FDA-cleared NAAT: Doxycycline 100 mg orally 2 times/day for 7 days, followed by moxifloxacin 400 mg orally once daily for 7 days
Although cure rates with doxycycline monotherapy are low, using doxycycline as the initial agent may lower Mycoplasma genitalium organism load and facilitate organism clearance, thereby increasing likelihood of moxifloxacin success 17. Higher doses of azithromycin have not been effective for M. genitalium after azithromycin treatment failures. Men with persistent or recurrent urethritis after treatment for M. genitalium should be referred to an infectious disease or urology specialist 8.
Mycoplasma genitalium treatment failures can occur when using doxycycline, azithromycin, and moxifloxacin 18. Microbiologic cure rates are poor with either doxycycline or azithromycin monotherapy (~50% or less). Microbiologic cure rates for moxifloxacin were initially high (close to 100%) but have declined to 89% in studies conducted from 2010-2017 19.
For cases of suspected treatment failure, consult the STD Clinical Consultation Network here https://www.stdccn.org
Resistance to azithromycin, which has been recommended for treatment, is high across the globe 20, 21. Pharmacokinetic data indicate that changing azithromycin dosing from a single-dose strategy to a multiday strategy might protect against inducing resistance in M. genitalium infections 22, 23.
How do I know if I have Mycoplasma genitalium?
People with Mycoplasma genitalium often have no symptoms 18.
Someone with symptoms may notice:
- Vaginal discharge;
- A burning sensation when urinating;
- Discharge from the penis.
See your doctor if you notice any of these symptoms.
You should also see a doctor if your partner has an STD or symptoms of one. Symptoms of an STD can include an unusual sore, a smelly discharge, burning when peeing, pain/bleeding after sex, and bleeding between periods.
How common is Mycoplasma genitalium?
The 2017-2018 National Health and Nutrition Examination Survey (NHANES) estimates overall prevalence of urogenital Mycoplasma genitalium to be 1.7% among people aged 14-59 years in the United States. The survey reported similar prevalence between males at 1.8% and females at 1.7% 24.
Reported estimates of Mycoplasma genitalium prevalence among STD clinic-based populations are higher. Among men presenting with urethritis in select STD clinics, 28.7% were positive for Mycoplasma genitalium 25. Among women presenting in a STD clinic in Seattle, 26% had an Mycoplasma genitalium infection 26. A large U.S. prospective multicenter study of a nucleic acid amplification diagnostic test for Mycoplasma genitalium including male and female patients seeking care in diverse geographic regions found overall prevalence to be 10.3%. In this study, Mycoplasma genitalium was more common among people ages 15 to 24 years than in people ages 35 to 39 years. The risk for Mycoplasma genitalium was higher in Black participants than White participants and higher in non-Hispanic than in Hispanic participants 27. A meta-analysis of Mycoplasma genitalium prevalence among gay, bisexual, and other men who have sex with men (MSM) found that urethral (5.0%) and rectal (6.2%) Mycoplasma genitalium infections were more common than pharyngeal infections (1.0%) 27.
Is there a cure for Mycoplasma genitalium?
Yes, the right treatment with antibiotics can cure Mycoplasma genitalium. It is important that you take all of the medicine your doctor gives you to treat Mycoplasma genitalium infection. Do not share medicine for Mycoplasma genitalium with anyone. Your sex partner(s) should also see a doctor who can test and treat them if needed. When taken properly, treatment will stop the infection and can decrease your chances of having problems later. Although medicine will stop the infection, it will not undo any permanent damage caused by the disease.
It is becoming harder to treat some Mycoplasma genitalium infections, as drug-resistant strains of Mycoplasma genitalium are increasing. Return to your doctor if your symptoms continue for more than a few days after completing treatment.
When can I have sex again after my Mycoplasma genitalium treatment?
Wait until you and your sex partner(s) complete Mycoplasma genitalium treatment and symptoms are gone before you have sex again.
If you were treated for Mycoplasma genitalium in the past, you can still get it again. This can happen if you have vaginal or anal sex without a condom with a person who has Mycoplasma genitalium.
What happens if I don’t get Mycoplasma genitalium treated?
Left untreated, Mycoplasma genitalium can cause serious and permanent health problems in women, including pelvic inflammatory disease (PID). Some of the complications of PID are:
- Formation of scar tissue that blocks fallopian tubes;
- Ectopic pregnancy (pregnancy outside the uterus);
- Infertility (not being able to get pregnant); and
- Long-term pelvic or abdominal pain.
For people who are already pregnant, Mycoplasma genitalium may be associated with preterm (early) delivery or pregnancy loss.
Currently experts do not know if men develop long-term health problems from Mycoplasma genitalium.
Mycoplasma genitalium transmission
You can get mycoplasma genitalium by having vaginal or anal sex without a condom with someone who has the infection. Researchers are still determining whether sex partners can spread Mgen through oral sex.
A person with mycoplasma genitalium can pass the infection to someone even when they have no signs or symptoms.
How can I reduce my risk of getting Mycoplasma genitalium?
The only way to completely avoid STDs such as Mycoplasma genitalium is to not have vaginal or anal sex.
If you are sexually active, the following things can help lower your chances of getting Mycoplasma genitalium:
- Being in a long-term mutually monogamous relationship with a partner who does not have Mycoplasma genitalium; and
- Using condoms the right way every time you have vaginal or anal sex.
Mycoplasma genitalium signs and symptoms
Mycoplasma genitalium causes symptomatic and asymptomatic urethritis among men.
When present, the typical symptoms of Mycoplasma genitalium urethritis include:
- painful urination (dysuria),
- urethral itch, and
- purulent or mucopurulent urethral discharge.
On examination, urethral discharge is often present. However, the discharge may not be grossly evident, and urethral milking (placing pressure along the length of the penis to express discharge) may be necessary for detection.
Among women, Mycoplasma genitalium may cause cervicitis and pelvic inflammatory disease (PID), though individuals with cervicitis due to Mycoplasma genitalium often are asymptomatic.
When present, symptoms associated with Mycoplasma genitalium cervicitis include:
- vaginal discharge,
- vaginal itching,
- painful urination (dysuria), and
- pelvic discomfort.
Clinical findings associated with cervicitis include purulent or mucopurulent cervical discharge and cervical friability. Vaginal wet smear or cervical fluid Gram stain may show elevated numbers of polymorphonuclear leukocyte cells.
Symptoms of pelvic inflammatory disease (PID) due to Mycoplasma genitalium may include:
- mild to severe pelvic pain,
- abdominal pain,
- abnormal vaginal discharge, and/or
- bleeding.
Research shows that 1%-26% of men who have sex with men and 3% of women have rectal infections of Mycoplasma genitalium 28, 29, 30, 31, 32 Rectal infections often are asymptomatic, but not always.
Similarly, people may have asymptomatic Mycoplasma genitalium in the pharynx. However, no evidence exists of it causing oropharyngeal symptoms or systemic disease. At this time, more research is needed to determine whether oral sex can spread Mycoplasma genitalium.
Mycoplasma genitalium complications
Mycoplasma genitalium is consistently associated with urethritis in men. However, there is not enough data to implicate Mycoplasma genitalium infection with adverse reproductive consequences (e.g., epididymitis, prostatitis, or infertility). The consequences of asymptomatic infection with Mycoplasma genitalium among cisgender men are unknown.
While Mycoplasma genitalium is associated with cases of pelvic inflammatory disease (PID), there are conflicting data regarding the strength of the association 31, 9. There are no clinical trials examining treatment of Mycoplasma genitalium and prevention of PID. In vitro inoculation of Mycoplasma genitalium into fallopian tube tissue causes damage to cilia, and Mycoplasma genitalium is more common among cisgender women with infertility. However, data are conflicting regarding the association between Mycoplasma genitalium and tubal factor infertility. Data are also limited regarding the association of Mycoplasma genitalium with ectopic pregnancy or preterm delivery.
Mycoplasma genitalium diagnosis
Laboratory tests can diagnose Mycoplasma genitalium. Your doctor may ask you to provide a urine sample for testing. In some cases, they may use (or ask you to use) a swab to get a sample from the vagina or cervix.
Nucleic acid amplification testing (NAAT) also called polymerase chain reaction (PCR) is the preferred method of detection for Mycoplasma genitalium. To diagnose Mycoplasma genitalium in men using nucleic acid amplification testing (NAAT), urine samples are the optimal specimen. For females, urine or cervical or vaginal swab samples are acceptable, but the preferred specimen types are vaginal swabs 33. Several commercial laboratories in the U.S. have laboratory-developed tests which also utilize nucleic acid amplification (NAAT). There are not published data on the sensitivity and specificity of these tests compared to FDA-approved NAATs.
Mycoplasma genitalium is an extremely slow growing organism. Culture can take up to six months and only a few research settings in the U.S. have the technical capability to culture Mycoplasma genitalium 34.
Mycoplasma genitalium treatment
The recommended treatment for all cases of Mycoplasma genitalium infections includes a two-stage approach with doxycycline, followed by an additional agent (either moxifloxacin or azithromycin), ideally using resistance-guided therapy 16, 8.
Recommended antibiotic regimens if M. genitalium resistance testing is available 16, 8:
- If macrolide sensitive: Doxycycline 100 mg orally 2 times/day for 7 days, followed by azithromycin 1 g orally initial dose, followed by 500 mg orally once daily for 3 additional days (2.5 g total)
- If macrolide resistant: Doxycycline 100 mg orally 2 times/day for 7 days followed by moxifloxacin 400 mg orally once daily for 7 days
Recommended antibiotic regimens if M. genitalium resistance testing is Not Available 16, 8:
- If M. genitalium is detected by an FDA-cleared NAAT: Doxycycline 100 mg orally 2 times/day for 7 days, followed by moxifloxacin 400 mg orally once daily for 7 days
Although cure rates with doxycycline monotherapy are low, using doxycycline as the initial agent may lower Mycoplasma genitalium organism load and facilitate organism clearance, thereby increasing likelihood of moxifloxacin success 17. Higher doses of azithromycin have not been effective for M. genitalium after azithromycin treatment failures. Men with persistent or recurrent urethritis after treatment for M. genitalium should be referred to an infectious disease or urology specialist 8.
Mycoplasma genitalium treatment failures can occur when using doxycycline, azithromycin, and moxifloxacin 18. Microbiologic cure rates are poor with either doxycycline or azithromycin monotherapy (~50% or less). Microbiologic cure rates for moxifloxacin were initially high (close to 100%) but have declined to 89% in studies conducted from 2010-2017 19.
For cases of suspected treatment failure, consult the STD Clinical Consultation Network here https://www.stdccn.org
Resistance to azithromycin, which has been recommended for treatment, is high across the globe 20, 21. Pharmacokinetic data indicate that changing azithromycin dosing from a single-dose strategy to a multiday strategy might protect against inducing resistance in M. genitalium infections 22, 23.
Recommended PID treatment regimens are not effective against M. genitalium. Initial empiric therapy for PID, which includes doxycycline 100 mg orally 2 times/day for 14 days, should be provided at the time of presentation for care 16. If M. genitalium is detected, a regimen of moxifloxacin 400 mg orally once daily for 14 days has been effective in eradicating the organism 16. Nevertheless, no data have been published that assess the benefits of testing women with PID for M. genitalium, and the importance of directing treatment against this organism is unknown 16.
HIV infection
Persons who have M. genitalium and HIV infection should receive the same treatment regimen as those persons without HIV 16.
Follow-Up
Test of cure is not recommended for asymptomatic persons who received treatment with a recommended regimen 16. In settings in which M. genitalium testing is available, persons with persistent urethritis, cervicitis, or PID accompanied by detection of M. genitalium should be treated with moxifloxacin.
Management of Sex Partners
Recent studies report a high concordance of M. genitalium among partners of males, females, and men who have sex with men; however, no studies have determined whether reinfection is reduced with partner treatment 14, 35, 36. Sex partners of patients with symptomatic M. genitalium infection can be tested, and those with a positive test can be treated to possibly reduce the risk for reinfection 16. If testing the partner is not possible, the antimicrobial regimen that was provided to the patient can be provided 16.
References- Raj JS, Rawre J, Dhawan N, Khanna N, Dhawan B. Mycoplasma genitalium: A new superbug. Indian J Sex Transm Dis AIDS. 2022 Jan-Jun;43(1):1-12. doi: 10.4103/ijstd.ijstd_103_20
- Yueyue W, Feichen X, Yixuan X, Lu L, Yiwen C, Xiaoxing Y. Pathogenicity and virulence of Mycoplasma genitalium: Unraveling Ariadne’s Thread. Virulence. 2022 Dec;13(1):1161-1183. doi: 10.1080/21505594.2022.2095741
- Yu J, Zhou Y, Luo H, Su X, Gan T, Wang J, Ye Z, Deng Z, He J. Mycoplasma genitalium infection in the female reproductive system: Diseases and treatment. Front Microbiol. 2023 Feb 21;14:1098276. doi: 10.3389/fmicb.2023.1098276
- Horner PJ, Martin DH. Mycoplasma genitalium Infection in Men. J Infect Dis. 2017 Jul 15;216(suppl_2):S396-S405. doi: 10.1093/infdis/jix145
- Wiesenfeld HC, Manhart LE. Mycoplasma genitalium in Women: Current Knowledge and Research Priorities for This Recently Emerged Pathogen. J Infect Dis. 2017 Jul 15;216(suppl_2):S389-S395. doi: 10.1093/infdis/jix198
- Bachmann LH, Kirkcaldy RD, Geisler WM, Wiesenfeld HC, Manhart LE, Taylor SN, et al.; MAGNUM Laboratory Working Group. Prevalence of Mycoplasma genitalium infection, antimicrobial resistance mutations and symptom resolution following treatment of urethritis. Clin Infect Dis. 2020;71:e624–32. 10.1093/cid/ciaa293
- Chambers LC, Morgan JL, Lowens MS, Robinson TS, Romano SS, Leipertz GL, et al. Cross-sectional study of urethral exposures at last sexual episode associated with non-gonococcal urethritis among STD clinic patients. Sex Transm Infect. 2019;95:212–8. 10.1136/sextrans-2018-053634
- Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, Reno H, Zenilman JM, Bolan GA. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. doi: 10.15585/mmwr.rr7004a1
- Rebecca Lis, Ali Rowhani-Rahbar, Lisa E. Manhart, Mycoplasma genitalium Infection and Female Reproductive Tract Disease: A Meta-analysis, Clinical Infectious Diseases, Volume 61, Issue 3, 1 August 2015, Pages 418–426, https://doi.org/10.1093/cid/civ312
- Yan X., Xiang H., Tao Y., Xu Z., Xuelong S., Jinyan Q., et al.. (2022). Mycoplasma genitalium infection rate among pregnancy females in China: a meta-analysis. Chin. J. Evid. Med. 22, 90–95. doi: 10.7507/1672-2531.202111133
- Bissessor M, Tabrizi SN, Bradshaw CS, et al. The contribution of Mycoplasma genitalium to the aetiology of sexually acquired infectious proctitis in men who have sex with men. Clin Microbiol Infect 2016;22:260–5. 10.1016/j.cmi.2015.11.016
- Ong JJ, Aung E, Read TRH, et al. Clinical characteristics of anorectal Mycoplasma genitalium infection and microbial cure in men who have sex with men. Sex Transm Dis 2018;45:522–6. 10.1097/OLQ.0000000000000793
- Read TRH, Murray GL, Danielewski JA, et al. symptoms, sites, and significance of Mycoplasma genitalium in men who have sex with men. Emerg Infect Dis 2019;25:719–27. 10.3201/eid2504.181258
- Cina M, Baumann L, Egli-Gany D, et al. Mycoplasma genitalium incidence, persistence, concordance between partners and progression: systematic review and meta-analysis. Sex Transm Infect 2019;95:328–35. 10.1136/sextrans-2018-053823
- Baumann L, Cina M, Egli-Gany D, et al. Prevalence of Mycoplasma genitalium in different population groups: systematic review andmeta-analysis. Sex Transm Infect 2018;94:255–62. 10.1136/sextrans-2017-053384
- Mycoplasma genitalium. https://www.cdc.gov/std/treatment-guidelines/mycoplasmagenitalium.htm
- Read TRH, Fairley CK, Murray GL, et al. Outcomes of resistance-guided sequential treatment of Mycoplasma genitalium infections: a prospective evaluation. Clin Infect Dis 2019;68:554–60. 10.1093/cid/ciy477
- Mycoplasma genitalium – CDC Detailed Fact Sheet. https://www.cdc.gov/std/mgen/stdfact-Mgen-detailed.htm
- Li Y, Le WJ, Li S, Cao YP, Su XH. Meta-analysis of the efficacy of moxifloxacin in treating Mycoplasma genitalium infection. Int J STD AIDS. 2017 Oct;28(11):1106-1114. doi: 10.1177/0956462416688562
- Lau A, Bradshaw CS, Lewis D, Fairley CK, Chen MY, Kong FY, et al. The efficacy of azithromycin for the treatment of genital Mycoplasma genitalium: a systematic review and meta-analysis. Clin Infect Dis. 2015;61:1389–99. 10.1093/cid/civ644
- Li Y, Le WJ, Li S, Cao YP, Su XH. Meta-analysis of the efficacy of moxifloxacin in treating Mycoplasma genitalium infection. Int J STD AIDS. 2017;28:1106–14. 10.1177/0956462416688562
- Horner P, Blee K, O’Mahony C, Muir P, Evans C, Radcliffe K; Clinical Effectiveness Group of the British Association for Sexual Health and HIV. 2015 UK National Guideline on the management of non-gonococcal urethritis. Int J STD AIDS 2016;27:85–96. 10.1177/0956462415586675
- Horner P. Mycoplasma genitalium nongonococcal urethritis is likely to increase in men who have sex with men who practice unsafe sex: what should we do? Sex Transm Dis 2019;46:518–20. 10.1097/OLQ.0000000000001030
- Torrone EA, Kruszon-Moran D, Philips C, Morris MR, Bowden KE, Papp J, Bachmann LH, Weinstock H, Kersh EN. Prevalence of Urogenital Mycoplasma genitalium Infection, United States, 2017 to 2018. Sex Transm Dis. 2021 Nov 1;48(11):e160-e162. doi: 10.1097/OLQ.0000000000001394
- Bachmann LH, Kirkcaldy RD, Geisler WM, Wiesenfeld HC, Manhart LE, Taylor SN, Seña AC, McNeil CJ, Newman L, Myler N, Fuchs R, Bowden KE; MAGNUM Laboratory Working Group. Prevalence of Mycoplasma genitalium Infection, Antimicrobial Resistance Mutations, and Symptom Resolution Following Treatment of Urethritis. Clin Infect Dis. 2020 Dec 17;71(10):e624-e632. doi: 10.1093/cid/ciaa293
- Khosropour CM, Jensen JS, Soge OO, Leipertz G, Unutzer A, Pascual R, Barbee LA, Dombrowski JC, Golden MR, Manhart LE. High Prevalence of Vaginal and Rectal Mycoplasma genitalium Macrolide Resistance Among Female Sexually Transmitted Disease Clinic Patients in Seattle, Washington. Sex Transm Dis. 2020 May;47(5):321-325. doi: 10.1097/OLQ.0000000000001148
- Manhart LE, Gaydos CA, Taylor SN, Lillis RA, Hook EW 3rd, Klausner JD, Remillard CV, Love M, McKinney B, Getman DK. Characteristics of Mycoplasma genitalium Urogenital Infections in a Diverse Patient Sample from the United States: Results from the Aptima Mycoplasma genitalium Evaluation Study (AMES). J Clin Microbiol. 2020 Jun 24;58(7):e00165-20. doi: 10.1128/JCM.00165-20
- Ong JJ, Aung E, Read TRH, et al. Clinical characteristics of anorectal Mycoplasma genitalium infection and microbial cure in men who have sex with men. Sex Transm Dis 2018Aug;45(8):522–526. doi: 10.1097/OLQ.0000000000000793
- Tim R. H. Read, Christopher K. Fairley, Sepehr N. Tabrizi, Melanie Bissessor, Lenka Vodstrcil, Eric P. F. Chow, Mieken Grant, Jennifer Danielewski, Suzanne M. Garland, Jane S. Hocking, Marcus Y. Chen, Catriona S. Bradshaw, Azithromycin 1.5g Over 5 Days Compared to 1g Single Dose in Urethral Mycoplasma genitalium: Impact on Treatment Outcome and Resistance, Clinical Infectious Diseases, Volume 64, Issue 3, 1 February 2017, Pages 250–256, https://doi.org/10.1093/cid/ciw719
- Bissessor M, Tabrizi SN, Bradshaw CS, Fairley CK, Hocking JS, Garland SM, Twin J, Poljak M, Peel J, Chen MY. The contribution of Mycoplasma genitalium to the aetiology of sexually acquired infectious proctitis in men who have sex with men. Clin Microbiol Infect. 2016 Mar;22(3):260-5. doi: 10.1016/j.cmi.2015.11.016
- Cina M, Baumann L, Egli-Gany D, Halbeisen FS, Ali H, Scott P, Low N. Mycoplasma genitalium incidence, persistence, concordance between partners and progression: systematic review and meta-analysis. Sex Transm Infect. 2019 Aug;95(5):328-335. doi: 10.1136/sextrans-2018-053823
- Baumann L, Cina M, Egli-Gany D, Goutaki M, Halbeisen FS, Lohrer GR, Ali H, Scott P, Low N. Prevalence of Mycoplasma genitalium in different population groups: systematic review and meta-analysis. Sex Transm Infect. 2018 Jun;94(4):255-262. doi: 10.1136/sextrans-2017-053384
- Van Der Pol B, Waites KB, Xiao L, Taylor SN, Rao A, Nye M, Chavoustie S, Ermel A, Kaplan C, Eisenberg D, Chan PA, Mena L, Pacheco S, Krishnamurthy S, Mohan R, Bertuzis R, McGowin CL, Arcenas R, Marlowe EM. Mycoplasma genitalium Detection in Urogenital Specimens from Symptomatic and Asymptomatic Men and Women by Use of the cobas TV/MG Test. J Clin Microbiol. 2020 May 26;58(6):e02124-19. doi: 10.1128/JCM.02124-19
- Jensen JS, Hansen HT, Lind K. Isolation of Mycoplasma genitalium strains from the male urethra. J Clin Microbiol. 1996 Feb;34(2):286-91. doi: 10.1128/jcm.34.2.286-291.1996
- Xiao L, Waites KB, Van Der Pol B, Aaron KJ, Hook EW 3rd, Geisler WM. Mycoplasma genitalium infections with macrolide and fluoroquinolone resistance-associated mutations in heterosexual African American couples in Alabama. Sex Transm Dis 2019;46:18–24. 10.1097/OLQ.0000000000000891
- Slifirski JB, Vodstrcil LA, Fairley CK, et al. Mycoplasma genitalium infection in adults reporting sexual contact with infected partners, Australia, 2008–2016. Emerg Infect Dis 2017;23:1826–33. 10.3201/eid2311.170998