Neck cracking
The noise you hear from your neck is in most cases completely harmless. Crepitus or crepitation is the noise that may be heard during joint movements, such as a cracking, popping, snapping, or grinding. These sounds and sensations can occur in the neck as well. The cracking, clicking or popping noise is caused when the facet joints in the spine are opened up in the course of the manipulation. The process is just as it is when your knuckles or your knees click. It is not painful and afterwards the joints in the spine may move more freely giving a combination of pain relief and better mobility. Most people at some point have experienced neck crepitus. One example is feeling a cracking sensation in the neck when turning the head to back up a car.
Some people regularly crack their neck on purpose—either due to a nervous habit or perhaps to bring some therapeutic relief from neck tightness. As such, it is common for people to wonder whether repeatedly cracking the neck can wear down the joints and cause arthritis. A review of the current medical literature indicates that frequent, purposeful knuckle-cracking of the fingers does not increase the risk for arthritis in those joints 1, 2. Joint cracking in the neck has not been as thoroughly studied, but there is currently no evidence to suggest that purposefully cracking the neck increases the risk for arthritis.
Your joints can make a variety of sounds: popping, cracking, grinding, and snapping. The joints that “crack” are the knuckles, knees, ankles, back, and neck. There are different reasons why these joints “sound off”.
- Escaping gases: Scientists explain that synovial fluid present in your joints acts as a lubricant. The fluid contains the gases oxygen, nitrogen, and carbon dioxide. When you pop or crack a joint, you stretch the joint capsule. Gas is rapidly released, which forms bubbles. In order to crack the same knuckle again, you have to wait until the gases return to the synovial fluid.
- Movement of joints, tendons and ligaments: When a joint moves, the tendon’s position changes and moves slightly out of place. You may hear a snapping sound as the tendon returns to its original position. In addition, your ligaments may tighten as you move your joints. This commonly occurs in your knee or ankle, and can make a cracking sound.
- Rough surfaces: Arthritic joints make sounds caused by the loss of smooth cartilage and the roughness of the joint surface.
Neck crepitus is usually painless and typically does not represent anything serious. However, if crepitus occurs with other troubling symptoms such as pain or following trauma, it could indicate a more serious underlying medical condition is present.
Your neck contains synovial fluid, which lubricates the joints between the bones. When you stretch and roll your neck, you put negative pressure on the synovial fluid, which creates tiny gas bubbles and results in a popping sound. Think of it like opening a can of soda. It’s called ‘cavitation’, and unless you’re overdoing it, it’s usually safe.
If you have a history of neck stiffness so much so that you frequently have an overwhelming urge to crack it, or if you cracked it and have neck pain as a result, it might be time to consult a physician.
A medical professional should assess any pain, numbness in limbs, or loss of strength experienced by neck cracking. The last thing you want is for the issue to get progressively worse while you’re waiting for your doctor to have time to see you and send you to see a specialist. You can bypass the waiting period by coming to see one of the physicians at SpineOne. We offer same-day appointments for urgent relief, and you don’t need a referral from your doctor. If you’re experiencing excessive pain or discomfort after popping your neck, schedule an appointment today.
The signs and symptoms of potentially serious pathology in patients presenting with neck pain.
Red flag symptoms
- Significant preceding trauma or neck surgery
- Systemic upset (weight loss, night sweats, fevers)
- Severe pain
- Nocturnal pain
- Relatively young (<20) or old (>55)
- Signs of spinal cord compression
- Significant vertebral body tenderness
- History of TB, HIV, cancer or inflammatory arthritis
Although neck pain is often poorly defined and vague in presentation, it is important to avoid missing serious pathology.
It is worth mentioning that red flags in this scenario have a high negative predictive value (so if they are absent, the chances of a serious cause being present are quite low) but their positive predictive value for diagnosing serious pathology is low.
Possible causes
- Whiplash
- Cervical spondylosis/degenerative
- Vertebral disc prolapse
- Rheumatoid arthritis or seronegative arthropathies
- Malignancy
- Infection (TB, meningitis)
- Cervical rib
- Neck artery dissection or aneurysm
- Vertebral fracture
Is neck cracking harmful?
If you are feeling pain when your joints pop, then you should seek a health care professional.
In general, a doctor should be consulted if neck cracking, also called neck crepitus, accompanies any of the following:
- Pain or swelling. Neck crepitus with pain or swelling could indicate osteoarthritis or some other type of inflammatory process in the joints of the neck.
- Recent accident or injury. If the neck is making new cracking or grinding sounds after trauma, such as a car accident or a fall, then that could indicate a structural change that needs to be addressed by a qualified health professional.
- Frequent or constant. If the neck crepitus is constant, such as a sound that can be recreated every time or nearly every time the joint is moved, then that could signal a problem in joint function, especially when accompanied by pain.
- Recent surgery. Sometimes new neck sounds develop after surgery in the cervical spine. These sounds might show up weeks later, and while they could be normal and nothing to worry about, they should be mentioned to the surgeon just in case.
Otherwise, neck cracking and grinding sounds alone most likely do not indicate a health problem. If a person is excessively worried about frequent neck cracking sounds even though there is no pain or other troubling symptoms, it is worth seeing the doctor to rule out a serious underlying condition and regain peace of mind.
Can purposefully cracking your neck be dangerous?
While quite rare, there are reports of vertebral artery dissection in the neck resulting in a stroke after certain types of manipulation of the cervical spine 3, 4, 5, 6. There is debate whether vertebral artery damage is equally likely to occur in people who do not receive spinal manipulation in this subset of the population 7. A review of the medical literature indicates that spinal manipulation of the neck by a qualified medical professional does not appreciably stress or stretch the vertebral artery 8.
As a standard precaution, anyone experiencing concerning symptoms such as pain, dizziness, lightheadedness, numbness, tingling, or other troubling symptoms after neck cracking should consult a qualified health professional immediately.
When neck cracking should be a concern?
See red flag symptoms and causes.
There are signs to help indicate when neck cracking is more than benign crepitus:
- Cracking that repeats every time you move a certain way, or nearly every time
- Cracking that’s accompanied by pain or swelling
- Cracking that starts following an accident or surgery that affects the cervical spine
If you experience any of these types of neck cracking, make an appointment with your doctor so your symptoms can be properly diagnosed.
It’s good to err on the side of caution when you’re concerned. But keep in mind that most cases of neck cracking, when not accompanied by other symptoms, are harmless.
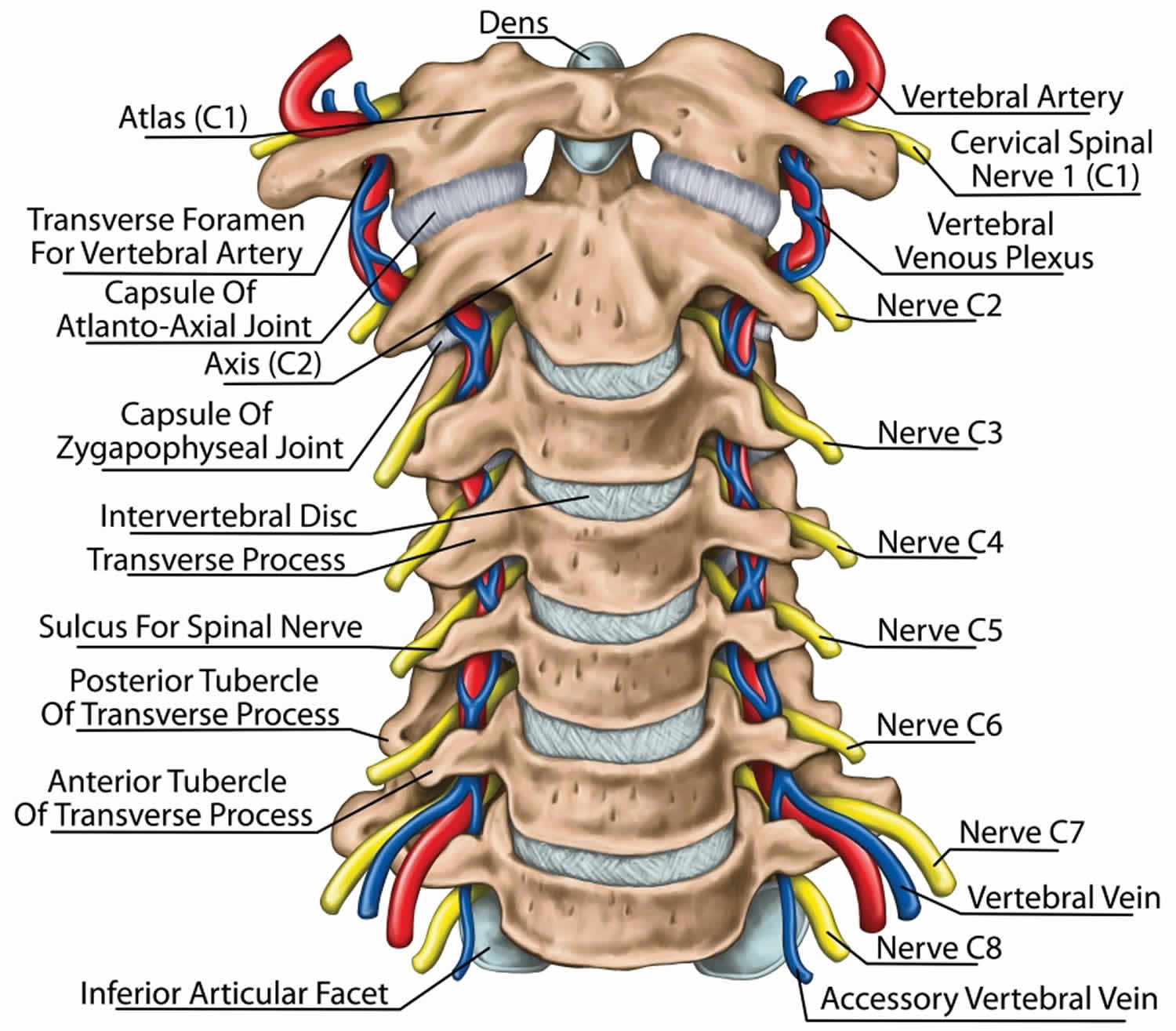
Cervical spine anatomy
The cervical spine is made up of the first 7 vertebrae and functions to provide mobility and stability to the head, while connecting it to the relative immobile thoracic spine (see the image below). The first 2 vertebral bodies are quite different from the rest of the cervical spine. The atlas, or C1, articulates superiorly with the occiput and inferiorly with the axis, or C2.
The atlas is ring-shaped and does not have a body, unlike the rest of the vertebrae. The body has become part of C2, and it is called the odontoid process, or dens. The atlas is made up of an anterior arch, a posterior arch, 2 lateral masses, and 2 transverse processes. The transverse foramen, through which the vertebral artery passes, is enclosed by the transverse process. On each lateral mass is a superior and inferior facet (zygapophyseal) joint. The superior articular facets are kidney-shaped, concave, and face upward and inward. These superior facets articulate with the occipital condyles, which face downward and outward. The relatively flat inferior articular facets face downward and inward to articulate with the superior facets of the axis.
The axis has a large vertebral body, which contains the fused remnant of the C1 body, the dens. The dens articulates with the anterior arch of the atlas via its anterior articular facet and is held in place by the transverse ligament. The axis is composed of a vertebral body, heavy pedicles, laminae, and transverse processes, which serve as attachment points for muscles. The axis articulates with the atlas by its superior articular facets, which are convex and face upward and outward.
The remaining cervical vertebrae, C3-C7, are similar to each other, but they are very different from C1 and C2. They each have a vertebral body, which is concave on its superior surface and convex on its inferior surface. On the superior surfaces of the bodies are raised processes or hooks called uncinate processes, which articulate with depressed areas on the inferior aspect of the superior vertebral bodies called the echancrure or anvil. These uncovertebral joints are most noticeable near the pedicles and are usually referred to as the joints of Luschka 9. These joints are believed to be the result of degenerative changes in the annulus, which leads to fissuring in the annulus and the creation of the joint. The spinous processes of C3-C5 are usually bifid, in comparison to the spinous processes of C6 and C7, which are usually tapered.
The facet joints in the cervical spine are diarthrodial synovial joints with fibrous capsules. The joint capsules in the lower cervical spine are more lax compared with other areas of the spine to allow for gliding movements of the facets. The joints are inclined at 45° from the horizontal plane and angled 85° from the sagittal plane. This alignment helps to prevent excessive anterior translation and is important in weight bearing 10.
The fibrous capsules are innervated by mechanoreceptors (types I, II, and III), and free nerve endings have been found in the subsynovial loose areolar and dense capsular tissues 11. In fact, there are more mechanoreceptors in the cervical spine than in the lumbar spine 12. This neural input from the facets may be important for proprioception and pain sensation and may modulate protective muscular reflexes that are important in preventing joint instability and degeneration.
The facet joints in the cervical spine are innervated by both the anterior and dorsal rami. The occipitoatlantal joint and atlantoaxial joint are innervated by the ventral rami of the first and second cervical spinal nerves. Two branches of the dorsal ramus of the third cervical spinal nerve innervate the C2-C3 facet joint, a communicating branch and a medial branch known as the third occipital nerve.
The remaining cervical facets, C3-C4 to C7-T1, are supplied by the dorsal rami medial branches that arise one level cephalad and caudad to the joint 13. Therefore, each joint from C3-C4 to C7-T1 is innervated by the medial branches above and below. These medial branches send off articular branches to the facet joints as they wrap around the waists of the articular pillars.
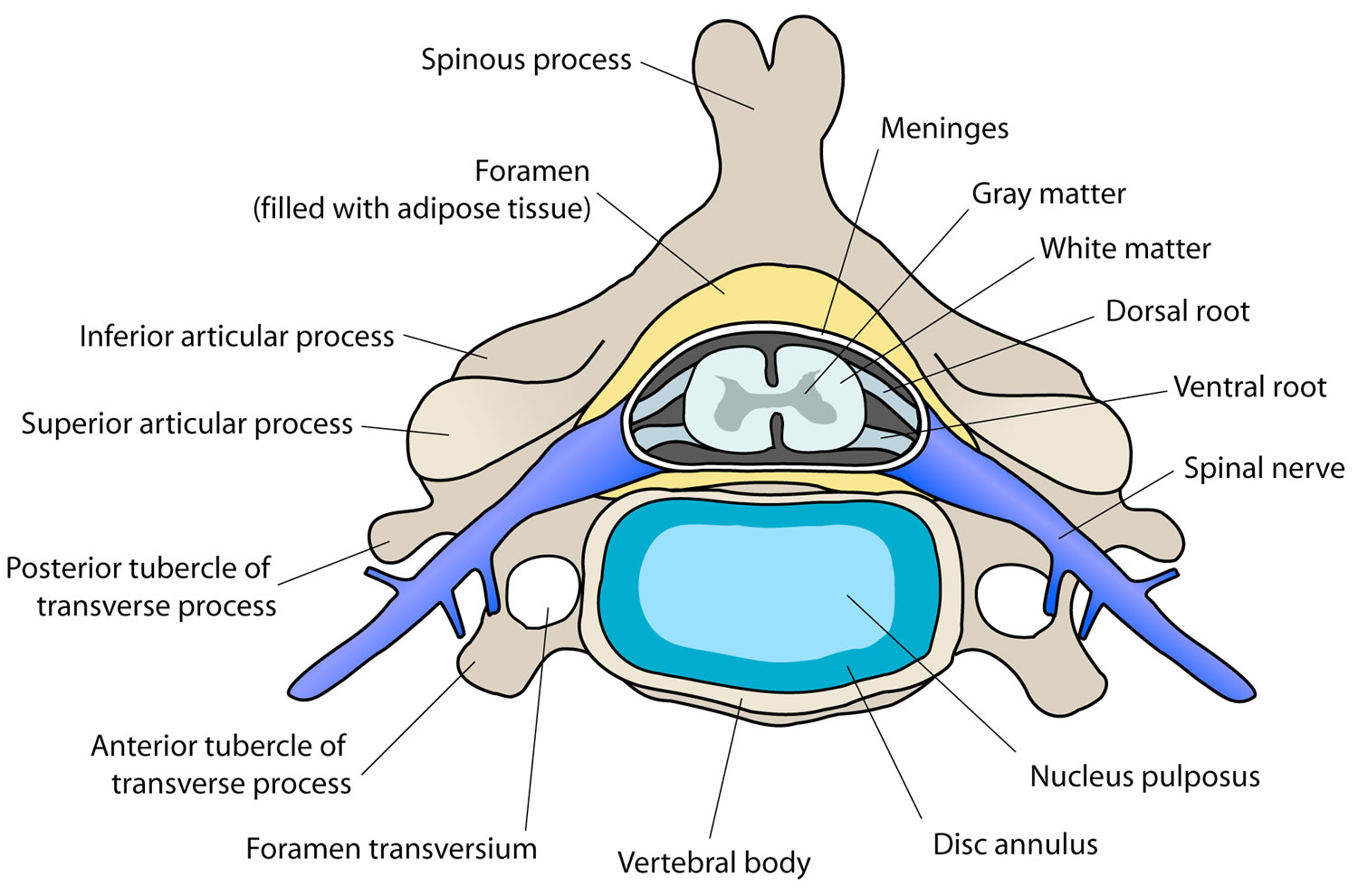
Intervertebral discs are located between each vertebral body caudad to the axis. The discs are composed of 4 parts, including the nucleus pulposus in the middle, the annulus fibrosis surrounding the nucleus, and 2 end plates that are attached to the adjacent vertebral bodies. The discs are involved in cervical spine motion, stability, and weight bearing. The annular fibers are composed of collagenous sheets called lamellae, which are oriented 65-70° from the vertical and alternate in direction with each successive sheet. Therefore, the annular fibers are prone to injury with rotation forces because only one half of the lamellae are oriented to withstand the force in this direction 12. The middle and outer one third of the annulus is innervated by nociceptors, and phospholipase A2 has been found in the disc and may be an inflammatory mediator 14.
Several ligaments of the cervical spine, which provide stability and proprioceptive feedback, are worth mentioning 15. The transverse ligament, the major portion of the cruciate ligament, arises from tubercles on the atlas and stretches across its anterior ring while holding the dens against the anterior arch. A synovial cavity is located between the dens and the transverse process. This ligament allows for rotation of the atlas on the dens and is responsible for stabilizing the cervical spine during flexion, extension, and lateral bending. The transverse ligament is the most important ligament in preventing abnormal anterior translation 16.
The alar ligaments run from the lateral aspects of the dens to the ipsilateral medial occipital condyles and to the ipsilateral atlas. The alar ligaments limit axial rotation and side bending. If the alar ligaments are damaged, as in a whiplash injury, the joint complex becomes hypermobile, which can lead to kinking of the vertebral arteries and stimulation of the nociceptors and mechanoreceptors. This may be associated with the typical complaints of patients with whiplash injuries such as headache, neck pain, and dizziness. The alar ligaments prevent excessive lateral and rotational motions, while allowing flexion and extension.
The anterior longitudinal ligament and the posterior longitudinal ligament are the major stabilizers of the intervertebral joints. Both ligaments are found throughout the entire length of the spine; however, the anterior longitudinal ligament is closely adhered to the discs in comparison to the posterior longitudinal ligament, and it is not well developed in the cervical spine. The anterior longitudinal ligament becomes the anterior atlantooccipital membrane at the level of the atlas, whereas the posterior longitudinal ligament merges with the tectorial membrane. Both ligaments continue onto the occiput. The posterior longitudinal ligament prevents excessive flexion and distraction 17.
The supraspinous ligament, interspinous ligament, and ligamentum flavum maintain stability between the vertebral arches. The supraspinous ligament runs along the tips of the spinous processes, the interspinous ligament runs between the spinous processes, and the ligamentum flavum runs from the anterior surface of the cephalad vertebra to the posterior surface of the caudad vertebra. The interspinous ligament and especially the ligamentum flavum control for excessive flexion and anterior translation 17. The ligamentum flavum also connects to and reinforces the facet joint capsules on the ventral aspect. The ligamentum nuchae is the cephalad continuation of the supraspinous ligament and has a prominent role in stabilizing the cervical spine.
Figure 1. Cervical spine
Figure 2. Cervical disc
Figure 3. Cervical facet joint
Neck cracking diagnosis
At your appointment a thorough consultation will work out why you are in pain or lacking mobility.
Medical History
Establish the characteristics of the pain, such as its site, onset, nature and radiation, and whether there was any preceding injury, trauma or neck surgery.
Older patients tend to have a narrower cervical canal and are more likely to have osteoporosis, which may result in fractures with only minor trauma. Younger patients may have congenital abnormalities of the spine.
Severe pain that is unremitting should ring alarm bells, particularly if worse at night. Night sweats, fevers and weight loss may indicate malignancy, or an infective process (for example, TB or osteomyelitis). A history of recent significant trauma, even to head, should make one consider fracture.
Neurological symptoms should prompt a neurological examination to exclude spinal cord compression or cervical myelopathy (such as clumsy hands, altered gait, or disturbances of sexual, bladder or sphincter function). A background of inflammatory arthritis or Down’s syndrome increases the chances of a more serious problem.
Drop attacks or dizziness, especially on upward gaze, may indicate vascular insufficiency, which is more common in older patients.
It is important to consider specific causes of neck pain such as neck pain with acute spasm but no underlying obvious cause (torticollis). There may be altered sensation or numbness associated with myeloradiculopathy but this can sometimes be present in patients with non-specific neck pain.
Physical Examination
Examine with adequate exposure of the neck and shoulders. Feel for severe tenderness over the vertebrae, which may indicate a fracture from trauma or malignancy. Also feel laterally in the supraclavicular region for cervical rib, and anteriorly for cervical lymph nodes, which may indicate infection or cancer. Specific exquisite tenderness over one vertebral body can sometimes be sign of infection, inflammation or malignancy.
Gently check neck movements. Lhermitte’s phenomenon (symptoms of an electric shock or burning radiating downwards) may occur with neck flexion and can suggest an underlying serious cause such as myelopathy or demyelination.
Neurological examination of the limbs is important. Disc prolapse commonly affects C5/6 and C6/7. Rarely, inverted reflexes may be found in cervical myeloradiculopathy, indicated by absent reflexes at the level of the lesion and enhanced below (for example, a C5/6 lesion would give absent biceps reflex but the triceps, C7, may be exaggerated).
Cord compression can present with upper motor neurone signs in the lower limbs (upper going plantars, hyper reflexia, spasticity and clonus) and lower motor neurone signs in the upper limbs (atrophy and hyporeflexia).
Rarely, a pulsatile mass may indicate carotid artery aneurysm, especially after neck manipulation or trauma. This should be referred urgently.
Neck cracking treatment
It is recommended that you seek a professional chiropractor, osteopathic health care provider, or physical therapist instead of asking your amateur buddy or trying to do it yourself. Second, if cracking your joints causes you pain, or if your limbs feel numb or lose strength, it’s best to consult with your health care provider. Third, if you do want to crack you joints yourself, consider doing so gently.
A history of substantial preceding trauma and cervical spine tenderness should prompt consideration for immediate immobilization, emergency room referral and imaging to exclude fracture or instability. Immediate referral may also be needed if spinal cord compression is suspected.
Consider urgent referral, imaging or specialist opinion if any of these red flags are present however in the absence of red flags, x-rays are often unhelpful and can often lead to false positive findings. For example, most patients over 30 have some degree of osteoarthritis radiologically and it is often difficult to correlate this clinically.
Neck manipulation
Recently, an international multidisciplinary task force endorsed manipulation as one of several firstline treatments for neck pain, whiplash, and related headaches based on a systematic review of randomised clinical trials of interventions and research on adverse events 18. They also published an original decision analysis model examining drugs, exercise, mobilization, and manipulation for neck pain, including summary estimates on benefits and harms, and incorporating patient preferences using the standard gamble method 19. Overall, there was no clear winner when the objective was to maximize quality adjusted life.
Another systematic review on conservative interventions for acute neck pain found that manipulation, multimodal physical therapy, neck exercises, and drugs (orphenadrine/paracetamol [acetaminophen] combined) all had significant short term effects on pain compared with placebo 20. In addition, acupuncture and manipulation had significant short term effects on disability compared with placebo. Thus the evidence clearly suggests that manipulation benefits patients with neck pain. Furthermore, a recent high quality trial found spinal manipulation more effective for acute and subacute neck pain, over both the short and long term, than management with non-steroidal anti-inflammatory drugs or acetaminophen (paracetamol) 21. The authors did not advocate abandoning these drugs, even though their harms are well documented 22.
Risks of neck manipulation
One concern about neck manipulation is the risk of stroke, and stroke has been reported in association with other activities that include rotation or extension of the neck such as yoga, looking up, and hair washing at a salon 6. There are multiple case reports of vertebrobasilar artery dissection and stroke after cervical manipulation, but case reports provide the lowest level of evidence. They raise hypotheses to be tested in analytical designs that include control groups but cannot be used to infer causation. In the case of rare events like vertebrobasilar stroke, the design of choice is the case-control study. Three such studies have been published, and their results are remarkably similar.
The first study was nested in the Ontario population and identified 582 patients admitted to hospital with vertebrobasilar stroke over five years 3. When compared with 2328 matched controls, there was a strong association between chiropractic care received within the previous week and stroke in people younger than 45 years (odds ratio 5.03). There was no association in older people. The authors calculated the risk attributable to chiropractic care was 1.3 cases per 100 000 people aged less than 45 years 3.
The second study by Smith et al 4 was nested in two California stroke registries. Cases included 26 strokes related to carotid dissection and 24 related to vertebral dissection compared with 100 non-dissection related strokes. They found a strong association between manipulative therapy received in the previous month and stroke related to vertebral dissection (odds ratio 6.6) but not carotid dissection.
The most recent study, by Cassidy et al 5, replicated the results of the two previous studies using the Ontario population over nine years—that is, over 100 million person years at risk. They confirmed a strong association between chiropractic care and subsequent vertebrobasilar stroke in people under 45 years old using both case-control and case-crossover designs (odds ratio 3.60) for those consulting a chiropractor in the previous month. However, they found a similar association between family physician care and vertebrobasilar strokes (odds ratio 2.99). Furthermore, the estimates for previous chiropractic or family physician care were similar when investigating different hazard periods up to 30 days before the stroke. Both associations increased when the analyses were limited to neck related diagnoses (such as cervical pain, strain, sprain, and headaches). This suggests that the association between neck manipulation and stroke is confounded by indication—that is, the disease (early dissection related neck pain or headache) is causing the exposures (visits to chiropractors and family doctors) 23. Neck pain and headache are the most common presenting complaints in people with cervical artery dissections 24 and are common reasons for seeking care. This evidence raises doubt about any causal relation between manipulation and stroke.
References- Boutin RD, Netto AP, Nakamura D, et al. Knuckle cracking: can blinded observers detect changes with physical examination and sonography? Clin Orthop Relat Res. 2017; 475(4):1265-71.
- Deweber K, Olszewski M, Ortolano R. Knuckle cracking and hand osteoarthritis. J Am Board Fam Med. 2011;24(2):169-74.
- Rothwell DM, Bondy SJ, Williams JI. Chiropractic manipulation and stroke: a population-based case-control study. Stroke2001;32:1054-60.
- Smith WS, Johnston SC, Skalabrin EJ, Weaver M, Azari P, Albers GW, et al. Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. Neurology2003;60:1424-8.
- Cassidy JD, Boyle E, Cote P, He Y, Hogg-Johnson S, Silver FL, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine 2008;33(suppl 4):S176-83.
- Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med2001;344:898-906.
- Cassidy JD, Boyle E, Cote P, et al. Risk of vertebrobasilar stroke and chiropractic care – results of a population-based case-control and case crossover study. Spine. 2008;33:S176-83.
- Symons B, Herzog W. Cervical artery dissection: a biomechanical perspective. J Can Chiropr Assoc. 2013 Dec;57(4):276–8.
- Johnson R. Anatomy of the cervical spine and its related structures. Torg JS, ed. Athletic Injuries to the Head, Neck, and Face. 2nd ed. St Louis, Mo: Mosby-Year Book; 1991. 371-83.
- Parke WW, Sherk HH. Normal adult anatomy. Sherk HH, Dunn EJ, Eismon FJ, et al, eds. The Cervical Spine. 2nd ed. Philadelphia, Pa: JB Lippincott Co; 1989. 11-32.
- McLain RF. Mechanoreceptor endings in human cervical facet joints. Spine. 1994 Mar 1. 19(5):495-501.
- Bogduk N, Twomey L. Clinical Anatomy of the Lumbar Spine. 2nd ed. New York, NY: Churchill Livingstone; 1991.
- Dreyfus P. The cervical spine: Non-surgical care Presented at: The Tom Landry Sports Medicine and Research Center; April 8, 1993; Dallas, Texas.
- Mendel T, Wink CS, Zimny ML. Neural elements in human cervical intervertebral discs. Spine. 1992 Feb. 17(2):132-5.
- Panjabi MM, Oxland TR, Parks EH. Quantitative anatomy of cervical spine ligaments. Part I. Upper cervical spine. J Spinal Disord. 1991 Sep. 4(3):270-6.
- Fielding JW, Cochran GB, Lawsing JF 3rd, Hohl M. Tears of the transverse ligament of the atlas. A clinical and biomechanical study. J Bone Joint Surg Am. 1974 Dec. 56(8):1683-91.
- Panjabi MM, Vasavada A, White A III. Cervical spine biomechanics. Semin Spine Surg. 1993. 5:10-6.
- Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on neck pain and its associated disorders. Spine2008;33(suppl 4):S123-52
- Van der Velde G, Hogg-Johnson S, Bayoumi AM, Cassidy JD, Cote P, Boyle E, et al. Identifying the best treatment among common nonsurgical neck pain treatments: a decision analysis. Spine2008;33(suppl 4):S184-91
- Leaver AM, Refshauge KM, Maher CG, McAuley JH. Conservative interventions provide short-term relief for non-specific neck pain: a systematic review. J Physiotherapy2010;56:73-85
- Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, Grimm RH. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Ann Intern Med2012;156:1-10
- Chang CH, Shau WY, Kuo CW, Chen ST, Lai MS. Increased risk of stroke associated with nonsteroidal anti-inflammatory drugs: a nationwide case-crossover study. Stroke2010;41:1884-90.
- Salas M, Hofman A, Stricker BH. Confounding by indication: an example of variation in the use of epidemiologic terminology. Am J Epidemiol1999;149:981-3.
- Lee VH, Brown RD Jr, Mandrekar JN, Mokri B. Incidence and outcome of cervical artery dissection: a population-based study. Neurology2006;67:1809-12.