What is necrotizing fasciitis
Necrotizing fasciitis represents a group of rare but highly lethal bacterial infections characterized by rapidly progressing inflammation and necrosis of skin and soft tissue 1. The bacteria most commonly get into the body through a break in the skin. Once in the body, the bacteria spread quickly and destroy the tissue they infect. The word “necrotizing” refers to something that causes body tissue to die. “Fasciitis” means inflammation of the fascia (the tissue under the skin that surrounds muscles, nerves, fat, and blood vessels). The spectrum of necrotizing fasciitis disease ranges from necrosis (death) of the skin to life-threatening infections involving the subcutaneous tissue, fascia, and muscle 2. The first clear description of necrotizing fasciitis was given by Joseph Jones 2, a surgeon in the Confederate Army of the United States in 1871. He described it as “hospital gangrene” in 2,642 soldiers with a mortality of 46 % during the Civil War. Necrotizing fasciitis itself was described in 1952 by Wilson when he observed edema and necrosis of subcutaneous fat and fascia with sparing of the underlying muscle in a series of 22 patients 3. Unfortunately, necrotizing fasciitis can result in a loss of limbs and even death. Accurate diagnosis, rapid antibiotic treatment, and prompt surgery are important to stopping this infection.
Necrotizing fasciitis has been classified according to the microbial infestation of the necrotic wound.
- Type I necrotizing fasciitis is caused by polymicrobials (i.e. more than one bacteria involved) including the anaerobes. Type I is the most common (70-80%) necrotizing fasciitis 4. Bacteria causing type 1 necrotizing fasciitis include Staphylococcus aureus, Haemophilus, Vibrio and several other aerobic and anaerobic strains (Escherichia coli, Bacteroides fragillis). It is usually seen in the elderly or in patients affected with diabetes or other conditions.
- Type II necrotizing fasciitis is caused by monomicrobials (only one bacteria involved) commonly by hemolytic group A streptococcus, staphylococci including methicillin resistant strains (MRSA) 4. Type II necrotizing fasciitis has been sensationalized in the media and is commonly referred to as flesh-eating disease. It affects all age groups. Healthy people are also prone to infection with this group.
- Type III necrotizing fasciitis is caused by Clostridia perfringens or less commonly Clostridia septicum. It usually follows significant injury or surgery and results in gas under the skin: this makes a crackling sound called crepitus. IV drug users injecting “black tar” heroin subcutaneously can also be infected with clostridia and develop necrotizing fasciitis. Necrotizing fasciitis due to marine organisms is usually due to contamination of wounds by sea water, cuts by fish fins or stingers, or consumption of raw seafood. It occurs more commonly in patients with liver disorders. These infections can be very serious and can be fatal if not attended within 48 hours.
- Type IV necrotizing fasciitis is a fungal infections caused by candida and zygomecetes, especially in cases of trauma and immunocompromised individuals.
- Necrotizing fasciitis affecting perineal, genital and perianal regions is known as Fournier’s gangrene. This has a particularly high death rate ranging from 15% to 50% 5.
Necrotising fasciitis can start from a relatively minor injury, such as a small cut, but gets worse very quickly and can be life threatening if it’s not recognized and treated early on. See a doctor right away if you have a fever, dizziness, or nausea soon after an injury or surgery. Necrotizing fasciitis usually involves the muscular fascia and subcutaneous tissue rapidly and extensively but can also affect the skin and muscle 6. These infections can have a fulminant presentation, and their clinical course is unpredictable 3. They may manifest as a low-grade cellulitis that quickly deteriorates to a limb or life-threatening infection 7. Necrotizing fasciitis is usually rapidly fatal unless there is a prompt recognition and aggressive surgical treatment 8. Necrotizing fasciitis must be treated as an emergency with repeated surgical interventions and high doses of broad-spectrum antibiotics through intravenous route 9.
Your chances of getting necrotizing fasciitis are extremely low if you have a strong immune system and practice good hygiene and proper wound care.
Most people who get necrotizing fasciitis have other health problems that may lower their body’s ability to fight infection. Some of these conditions include:
- Diabetes
- Kidney disease
- Cancer
Symptoms of necrotizing fasciitis can often be confusing and develop quickly. This fulminant tissue necrosis is usually accompanied by generalized toxicity, which may progress to shock and multiple organ failure. Without prompt recognition and immediate aggressive management, necrotizing fasciitis is often rapidly fatal. In the United States from 2003 to 2013, the overall mortality rate for necrotizing fasciitis-related death was 4.8 per 1,000,000 person-years 10.
Early symptoms of necrotizing fasciitis include:
- A red or swollen area of skin that spreads quickly
- Severe pain, including pain beyond the area of the skin that is red or swollen
- Fever
See a doctor right away if you have these symptoms after an injury, even if the injury doesn’t break the skin. Even though minor illnesses can cause symptoms like these, people should not delay getting medical care.
Later symptoms of necrotizing fasciitis can include:
- Ulcers, blisters, or black spots on the skin
- Changes in the color of the skin
- Pus or oozing from the infected area
- Dizziness
- Fatigue (tiredness)
- Diarrhea or nausea
Doctors often need to perform surgery in order to:
- Diagnose necrotizing fasciitis
- See how deep the infection has spread
- Quickly remove diseased tissue
Since necrotizing fasciitis can spread so rapidly, patients often must get surgery done very quickly. Doctors also give strong antibiotics through a needle into a vein (IV antibiotics) to try to stop the infection. Sometimes, however, antibiotics cannot reach all of the infected areas because the bacteria have killed too much tissue and reduced blood flow. When this happens, doctors have to surgically remove the dead tissue. Sometimes doctors have to remove the infected limb (e.g., leg, foot, arm) to stop the infection from spreading further. It is not unusual for someone with necrotizing fasciitis to end up needing multiple surgeries.
Necrotizing fasciitis is a medical emergency that requires immediate treatment.
Go to your nearest accident and emergency department as soon as possible if you think you have it. Call your local emergency services number for an ambulance if you’re too unwell to get yourself to emergency department.
Blood tests and scans may be carried out to find out what’s causing your symptoms, although a diagnosis of necrotizing fasciitis can usually only be confirmed by having an operation to examine the affected tissue.
Necrotizing fasciitis bacteria
Many types of bacteria can cause necrotizing fasciitis, including 11:
- Group A Streptococcus or group A strep (Streptococcus pyogenes)
- Bacterioides
- Klebsiella
- Clostridium
- Escherichia coli or E. coli
- Staphylococcus aureus
- Aeromonas hydrophila
- Pseudomonas
- Proteus
Media reports often call them “flesh eating bacteria” and necrotizing fasciitis is sometimes called the “flesh-eating disease”, although the bacteria that cause it don’t “eat” flesh – they release toxins that damage nearby tissue. Public health experts believe group A Streptococcus (group A strep) is the most common cause of necrotizing fasciitis 12. Group A strep (Streptococcus pyogenes) are the same bacteria that cause strep throat, scarlet fever, impetigo, toxic shock syndrome, cellulitis and necrotizing fasciitis. Group A strep bacteria live in the nose and throat. When someone who is infected coughs or sneezes, the bacteria travel in small droplets of water called respiratory droplets. One of the ways you can get sick is if you breathe in those droplets or if you touch something that has the droplets on it and then touch your mouth, nose, or eyes.
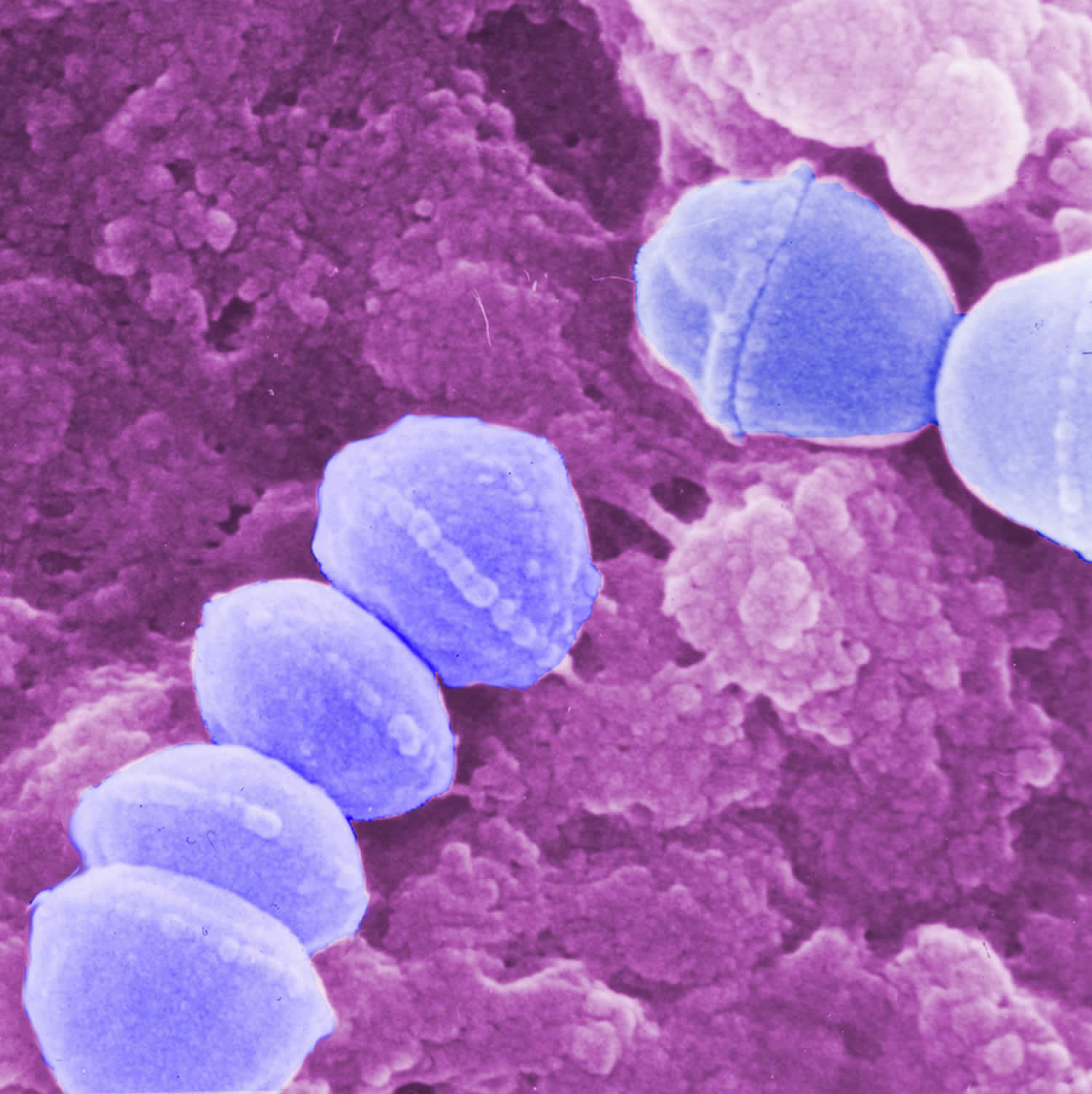
Figure 1. Group A Streptococcus (Streptococcus pyogenes) bacteria
Is necrotizing fasciitis contagious?
People rarely spread necrotizing fasciitis to other people. If you’re in close contact with someone who has necrotizing fasciitis, you may be given a course of antibiotics to reduce your risk of infection.
In general, someone with necrotizing fasciitis does not spread the infection to others. Most cases of necrotizing fasciitis occur randomly.
How do you get necrotizing fasciitis
Necrotizing fasciitis may occur in anyone, in fact, almost half of all known cases of streptococcal necrotizing fasciitis have occurred in young and previously healthy individuals.
The most common way of getting necrotizing fasciitis is when the bacteria enter the body through a break in the skin, including:
- Cuts and scrapes
- Burns
- Insect bites
- Puncture wounds (including those due to IV drug use)
- Surgical wounds
Necrotizing fasciitis infection may occur if the right set of conditions is present, these include:
- An opening in the skin that allows bacteria to enter the body. This may occur following minor injury (eg small cut, graze, pinprick, injection), or a large wound due to trauma or surgery (e.g., laparoscopy, sclerotherapy, endoscopic gastrostomy, thoracostomy, caesarean section, hysterectomy). Sometimes no point of entry can be found.
- Cervicofacial necrotizing fasciitis can follow mandibular fracture or dental infection.
- Direct contact with a person who is carrying the bacteria or the bacteria is already present elsewhere on the person.
- Particularly invasive strains of bacteria, eg streptococci that evade the immune system and produce a toxin called cysteine protease SpeB, which dissolves tissue.
- In children, type II necrotizing fasciitis may complicate chickenpox. Other causes of necrotizing fasciitis in chidren include omphalitis, necrotizing enterocolitis and urachal anomalies.
Risks for necrotizing fasciitis include:
- Aspirin and non-steroidal anti-inflammatory drugs
- Advanced age
- Diabetes
- Immune suppression
- Obesity
- Drug abuse
- Severe chronic illness
- Malignancy.
Figure 2. Necrotizing fasciitis
Figure 3. Necrotizing fasciitis upper limb
Figure 4. Necrotizing fasciitis face
Necrotizing fasciitis prognosis
Necrotizing fasciitis can progress very quickly and lead to serious problems such as blood poisoning (sepsis) and organ failure.
Necrotizing fasciitis carries a mortality rate between 8.7-76% 13. Mortality is high when this infection is associated with delayed treatment and immune compromised host 14. Early diagnosis and prompt treatment offers the only chance of cure. Even with treatment, it’s estimated that 1 or 2 in every 5 cases are fatal, due to complications such as renal failure and septicemia (blood poisoning) and multiorgan failure 15.
People who survive the infection are sometimes left with long-term disability as a result of amputation or the removal of a lot of infected tissue.
They may need further surgery to improve the appearance of the affected area and may need ongoing rehabilitation support to help them adapt to their disability. Thus necrotizing fasciitis is a condition that incurs significant morbidity and both early and late mortality.
Necrotizing fasciitis symptoms
The symptoms of necrotizing fasciitis develop quickly over hours or days. They may not be obvious at first and can be similar to less serious conditions such as flu, gastroenteritis or cellulitis.
Early symptoms can include:
- A small but painful cut or scratch on the skin. The most common site of infection is the lower leg. necrotizing fasciitis may also affect upper limb, perineum, buttocks, trunk, head and neck.
- Intense pain that’s out of proportion to any damage to the skin. Pain is often very severe at presentation and worsens over time.
- A high temperature (fever) and other flu-like symptoms, such as nausea, fever, diarrhea, dizziness and general malaise.
- Intense thirst develops as body becomes dehydrated.
- Symptoms appear usually within 24 hours of a minor injury.
After a few hours to 3 to 4 days, you may develop:
As necrotizing fasciitis takes hold:
- The affected area starts to swell and may show a purplish rash and redness in the painful area – the swelling will usually feel firm to the touch
- Diarrhea and vomiting
- Large dark blotches on the skin that turn into fluid-filled blisters with dark fluid
- Wound starts to die and area becomes blackened (necrosis)
- Edema is common
- A fine crackling sensation under the skin (crepitus) is due to gas in the tissues
- Severe pain continues until necrosis/gangrene destroys peripheral nerves when the pain subsides
- The infection may not improve when antibiotics are given.
- If left untreated, the infection can spread through the body quickly and cause symptoms such as dizziness, weakness and confusion.
By about days 4–5, the patient is very ill with dangerously low blood pressure and high temperature. The infection has spread into the bloodstream and the body goes into toxic shock. The patient may have altered levels of consciousness or become totally unconscious.
Metastatic abscesses can develop in liver, lung, spleen, brain, pericardium, and rarely, in the skin.
What causes necrotizing fasciitis
Necrotizing fasciitis can be caused by several different types of bacteria.
The bacteria that cause the infection live in the gut, in the throat, or on the skin of some people, where they don’t usually cause any serious problems.
But in rare cases, they can cause necrotizing fasciitis if they get into deep tissue – either through the bloodstream, or an injury or wound, such as:
- cuts and scratches
- insect bites
- puncture wounds caused by injecting drugs
- surgical wounds
Necrotizing fasciitis typically occurs when bacteria already on the skin or in the body get into deep tissue. The infection can also be spread from person to person, but this is very rare.
Anyone can get necrotizing fasciitis – including young and otherwise healthy people – but it tends to affect older people and those in poor general health.
Pathophysiology of necrotizing fasciitis
Infection starts in the superficial fascia. Enzymes and proteins released by the responsible organisms cause necrosis of fascial layers. Horizontal spread of infection may not be clinically apparent on the skin surface and hence diagnosis may be delayed. Infection then spreads vertically up into the skin and down into deeper structures. Thrombosis occludes the arteries and veins leading to ischemia and necrosis of the tissues.
Streptococci produce:
- M proteins, which initiate an inflammatory response with release of numerous cytokines (L-1, IL-6, TNFα)
- Exotoxins, which destroy neutrophils allowing bacterial growth and destroying tissues.
Aerobic and anaerobic bacteria produce hydrogen, nitrogen, hydrogen sulfide, and methane gases that destroy hyaluronic acid enabling spread of infection.
Risk factors for developing necrotizing fasciitis
- Chronic alcoholism
- Diabetes
- Vascular disease
- Peripheral vascular deficiency
- Acquired immune-deficiency syndrome
- Age >50 years
- Poor personal hygiene
- Malnutrition 16
- Kidney failure 16
- Obesity 17
Non-steroidal anti-inflammatory drugs (NSAIDs) have been suggested as possible risk factors for necrotizing fasciitis 18.
Necrotizing fasciitis prevention
There’s no vaccine for necrotizing fasciitis and it’s not always possible to prevent it. If you’re in close contact with someone who has necrotizing fasciitis, you may be given a course of antibiotics to reduce your risk of infection.
Common sense and good wound care are the best ways to prevent bacterial skin infections.
- Clean all minor cuts and injuries that break the skin (like blisters and scrapes) with soap and water.
- Clean and cover draining or open wounds with clean, dry bandages until they heal.
- Keep wounds clean and dry – after a wound has been cleaned, cover it with a sterile dressing (such as a plaster); change the dressing if it gets wet or dirty.
- See a doctor for puncture and other deep or serious wounds.
- Wash hands often with soap and water or use an alcohol-based hand rub if washing is not possible.
- Care for fungal infections like athlete’s foot.
If you have an open wound or skin infection, avoid spending time in:
- Hot tubs
- Swimming pools
- Natural bodies of water (e.g., lakes, rivers, oceans)
Necrotizing fasciitis treatment
Necrotizing fasciitis needs to be treated in hospital.
The main treatments are:
- surgery to remove infected tissue – this may be repeated several times to ensure all the infected tissue is removed, and occasionally it may be necessary to amputate affected limbs
- antibiotics – usually several different types are given directly into a vein
- supportive treatment – including treatment to control your blood pressure, fluid levels and organ functions
- hyperbaric oxygen and intravenous immunoglobulin may also be considered.
People with necrotizing fasciitis will often need to be looked after in an intensive care unit and may need to stay in hospital for several weeks.
While in hospital, they may be isolated from other patients to reduce the risk of spreading the infection.
References- Singh G, Bharpoda P, Reddy R. Necrotizing Fasciitis: A Study of 48 Cases. The Indian Journal of Surgery. 2015;77(Suppl 2):345-350. doi:10.1007/s12262-013-0835-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4692953/
- Bosshardt TL, Henderson VJ, Organ CH. Necrotizing soft tissue infections. Arch Surg. 1996;131:846–54. doi: 10.1001/archsurg.1996.01430200056011
- Wilson B. Necrotizing fasciitis. Am J Surg. 1952;18:416–31.
- Diagnosis and management of necrotising fasciitis: a multiparametric approach. Morgan MS. J Hosp Infect. 2010 Aug; 75(4):249-57. https://www.ncbi.nlm.nih.gov/pubmed/20542593/
- Kuzaka B, Wróblewska MM, Borkowski T, et al. Fournier’s Gangrene: Clinical Presentation of 13 Cases. Medical Science Monitor : International Medical Journal of Experimental and Clinical Research. 2018;24:548-555. doi:10.12659/MSM.905836. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5798415/
- Kotrappa KS, Bansal RS, Amin NM. Necrotizing fasciitis. Am Fam Physician. 1996;53(5):1691–7.
- Ardire L. Necrotizing fasciitis: case study of a nursing dilemma. Ostomy Wound Manage. 1997;43(5):30–4.
- Buchholz J, Jeske M, Kuhnen C, et al. (1997) Necrotizing fasciitis of extremities: clinical and histological examinations. Br J Surg 84–7
- Harmonson JK, Lobar MY, Harkless LB. Necrotizing fasciitis. Clin Podiatr Med Surg. 1996;13(4):635–46.
- Arif N, Yousfi S, Vinnard C. Deaths from Necrotizing Fasciitis in the United States, 2003–2013. Epidemiology and infection. 2016;144(6):1338-1344. doi:10.1017/S0950268815002745. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5725950/
- Acting Fast Is Key with Necrotizing Fasciitis. https://www.cdc.gov/Features/NecrotizingFasciitis/
- Lancerotto L, Tocco I, Salmaso R, Vindigni V, Bassetto F. Necrotizing fasciitis: classification, diagnosis, and management. Journal of Trauma and Acute Care Surgery 2012;72(3):560‐6.
- Current concepts in the management of necrotizing fasciitis. Misiakos EP, Bagias G, Patapis P, Sotiropoulos D, Kanavidis P, Machairas A. Front Surg. 2014; 1():36.
- Necrotizing fasciitis of the vulva. Stephenson H, Dotters DJ, Katz V, Droegemueller W. Am J Obstet Gynecol. 1992 May; 166(5):1324-7.
- Clark LA, Moon RE. Hyperbaric oxygen in the treatment of life‐threatening soft‐tissue infections. Respiratory Care Clinics of North America 1999;5(2):203‐19.
- Navinan MR, Yudhishdran J, Kandeepan T, Kulatunga A. Necrotizing fasciitis – a diagnostic dilemma: two case reports. Journal of Medical Case Reports. 2014;8:229. doi:10.1186/1752-1947-8-229. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4086700/
- [Necrotizing fasciitis. Clinical criteria and risk factors]. Roujeau JC. Ann Dermatol Venereol. 2001 Mar; 128(3 Pt 2):376-81.
- Necrotizing fasciitis. Puvanendran R, Huey JC, Pasupathy S. Can Fam Physician. 2009 Oct; 55(10):981-7.