Nevus depigmentosus
Nevus depigmentosus also called non-pigmented nevus, nevus achromicus or achromic nevus, is an uncommon birthmark (congenital nevus) characterized by a well-defined pale patch. The name is not quite right, as the hypomelanotic patches of a nevus depigmentosus are not completely white, unlike the areas of depigmentation in vitiligo, which are amelanotic, and completely lacking melanin 1. Nevus depigmentosus is usually several centimeters in diameter, with an irregular, serrated, feathered, or geographic margins but well-defined border. Shape and size varies. Nevus depigmentosus is generally classified as isolated, segmental, and whorled types. Often, smaller hypopigmented macules arise around the edges, resembling a splash of paint 2. Nevus depigmentosus most commonly arises on the trunk, but may also arise on the limbs and elsewhere 3. The face, when involved, is a cause of social embarrassment for the patient.
Nevus depigmentosus has to be differentiated from nevus anemicus, hypomelanosis of ito, vitiligo and albinism 4. Nevus anemicus is a congenital vascular anomaly that presents clinically as a hypopigmented macule or patch 5. Vitiligo is characterized by depigmented macules as a result of loss of functional cutaneous melanocytes. Lesions often show homogenous depigmentation and are well demarcated. Vitiligo lesions are well accentuated with obvious fluorescence upon Wood lamp examination. Nevus anemicus can be differentiated by diascopy where the lesion blends with the surrounding skin.
Nevus depigmentosus is usually solitary, in contrast to tuberous sclerosis, where multiple pale patches occur and are called ash-leaf macules. The ash-leaf macules seen in tuberous sclerosis are oval-shaped hypopigmented macules and look similar to nevus achromicus but usually present as multiple lesions.
Nevus depigmentosus is usually noted at birth or early childhood, although lesions may not be apparent until mid-childhood in those with light-colored skin. The hypopigmentation is permanent and enlarges in proportion with growth in the person 6. Lee et al. 7 found that the majority (92.5%) of nevus depigmentosus present before the age of three years and have serrated irregular borders (77.4%).
Occasionally, nevus depigmentosus is associated with other neurological, eye, hair, musculoskeletal, internal organ involvement and limb hypertrophy 8. Colocalized lentigines have been reported 1. They may represent a reverse mutation.
Treatment of nevus depigmentosus is often unnecessary. Cosmetic camouflage may be helpful. The treatment is difficult and options such as 308 nm excimer laser, epidermal grafts, and suction blister grafting has been tried.
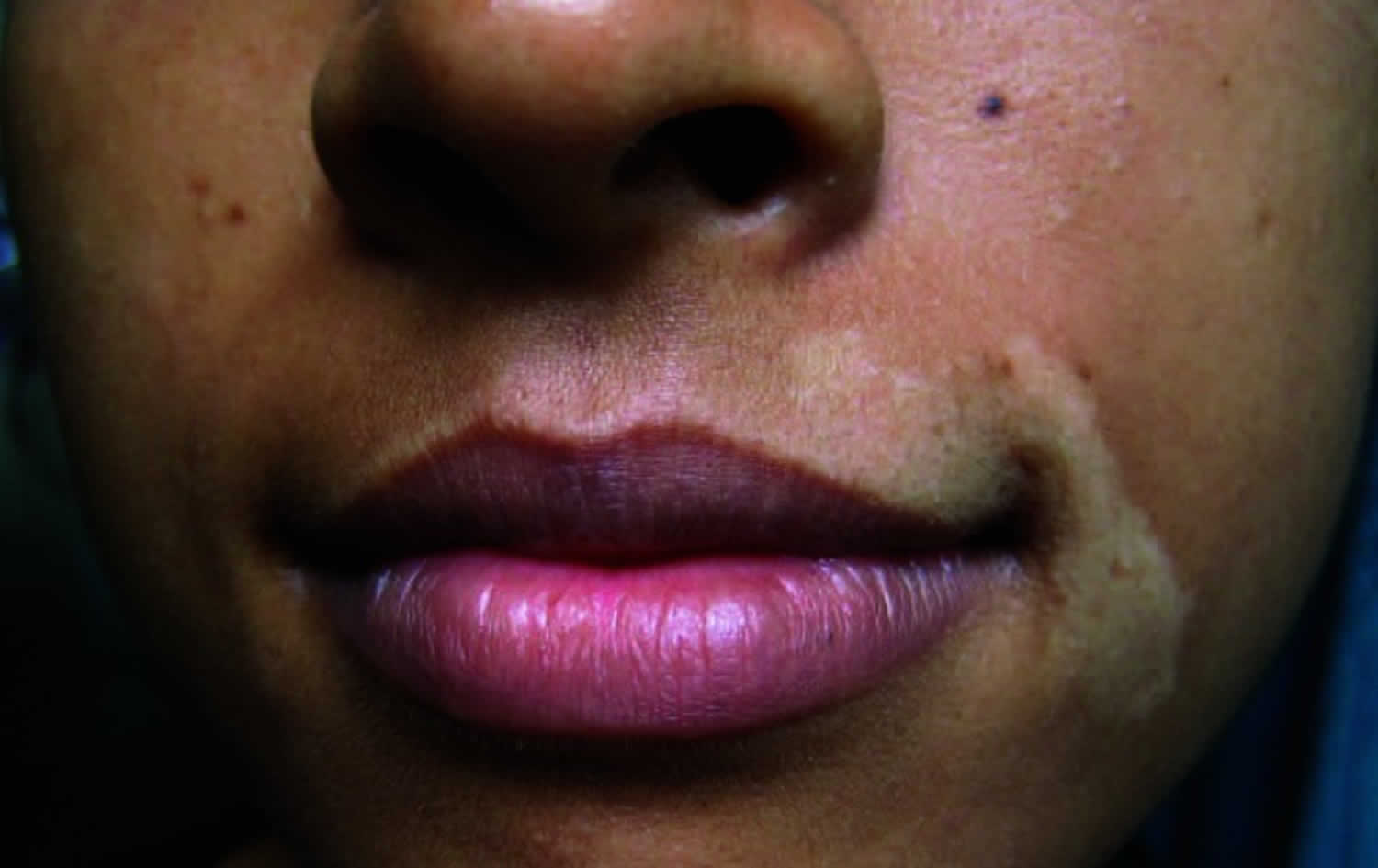
Figure 1. Nevus depigmentosus
Figure 2. Nevus depigmentosus
Nevus depigmentosus causes
The exact cause of nevus depigmentosus is still not clearly understood 9. A sporadic defect in the embryonic development has been suggested to be a causative factor 10. Most investigators agree that there is no change in the number of melanocytes (pigment cells) in the affected area 7 and report abnormal melanosomes (melanin-containing granules) transfer resulting in their decreased number in keratinocytes 11 or reduction in the number of melanosomes in melanocytes 7. However, Takaiwa and Mishima 12 reported decreased number of melanocytes without any disturbance in the melanocyte transfer to keratinocytes (skin cells). In a similar observation by Sung et al. 13, melanocyte counts were significantly decreased when stained with NKI/beteb and MART-1. It was mildly decreased when stained with the S-100 protein stain.
Nevus depigmentosus diagnosis
The commonly used clinical diagnostic criteria for nevus depigmentosus are as follows 3:
- The patch of pale skin (leukoderma) is present at birth or early in life
- It remains in the same site throughout lifetime
- There is no alteration in texture or change in sensation in the lesions
- There is no dark border around the affected skin.
On Wood’s lamp examination, nevus depigmentosus appears off-white, compared to the chalk-white accentuation seen in vitiligo 14.
Nevus depigmentosus treatment
Treatment of nevus depigmentosus is often unnecessary. Cosmetic camouflage may be helpful. Some of the options that have been used to attempt repigmentation include: excimer laser, phototherapy (PUVA and narrow-band UVB), and different skin grafting techniques 9. However, unlike vitiligo treatment, surgery has a limited role in nevus depigmentosus treatment because the extent of repigmentation from graft foci depends on the migration of melanocytes and this is difficult to predict in these cases 15. There has been only one report of repigmentation of a nevus depigmentosus lesion following treatment with 308-nm excimer laser irradation 16.
References- Achromic naevus. https://dermnetnz.org/topics/achromic-naevus
- Bolognia Dermatology 3rd Edition– Vitiligo and other disorders of hypopigmentation.
- Coup RL. Unilateral systemic achromic naevus. Dermatologica.1976;136:19-35.
- Jha AK, Sinha R, Prasad S. Nevus depigmentosus with unilateral bluish sclera, a rare entity. Indian Dermatol Online J. 2015;6(5):358-359. doi:10.4103/2229-5178.164491 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4594402
- Nevus Anemicus. https://emedicine.medscape.com/article/1084329-overview
- Kar BR. Nevus Depigmentosus Treated with Suction Blister Grafting: Follow-up After 10 Years. Indian J Dermatol. 2013;58(2):158. doi:10.4103/0019-5154.108074 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3657231
- Lee HS, Chun YS, Hann SK. Nevus depigmentosus: clinical features and histopathologic characteristics in 67 patients. J Am Acad Dermatol. 1999 Jan;40(1):21-6. doi: 10.1016/s0190-9622(99)70524-4
- Di Lernia V. Segmental nevus depigmentosus: analysis of 20 patients. Pediatr Dermatol. 1999 Sep-Oct;16(5):349-53. doi: 10.1046/j.1525-1470.1999.00091.x
- Mulekar SV, Al Issa A, Al Eisa A. Nevus depigmentosus treated by melanocyte-keratinocyte transplantation. J Cutan Aesthet Surg. 2011;4(1):29-32. doi:10.4103/0974-2077.79185 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3081481
- Pinto FJ, Bolognia JL. Disorders of hypopigmentation in children. Pediatr Clin North Am. 1991;38:991–1017.
- Jimbow K, Fitzpatrick TB, Szabo G, Hori Y. Congenital circumscribed hypomelanosis: a characterization based on electron microscopic study of tuberous sclerosis, nevus depigmentosus, and piebaldism. J Invest Dermatol. 1975 Jan;64(1):50-62. doi: 10.1111/1523-1747.ep12540914
- Takaiwa T, Mishima Y. Population density of intraepidermal dendritic cells in nevus depigmentosus. Jan J Clin Electron Microsc. 1970;3:651–2.
- Sung KK, Hee YK, Eun-so L, You CK. Clinical and histopathologic characteristics on nevus depigmentosus. J Am Acad Dermatol. 2006;55:423–8.
- Nevus depigmentosus: clinical features and histopathologic characteristics in 67 patients. J Am Acad Dermatol. 1999 Jan;40(1):21-6.
- Gupta S, Goel A. Letter to the editor: nevus depigmentosus needs transplant of epidermal sheets. Dermatol Surg. 2005 Dec;31(12):1746-7. doi: 10.2310/6350.2005.31327
- Kim DY, Lee KY, Park YK. Use of the 308-nm excimer laser for nevus depigmentosus: a promising treatment for either nevus depigmentosus or vitiligo. J Dermatol. 2007 Mar;34(3):217-8. doi: 10.1111/j.1346-8138.2007.00254.x