Oral herpes
Oral herpes is an infection of your lips, mouth, or gums caused by a contagious virus called herpes simplex virus (HSV) 1. Oral herpes causes small, painful blisters commonly called cold sores or fever blisters. Oral herpes is also called herpes labialis or orofacial herpes simplex. Oral herpes may also appear on other areas of your face, such as your chin or nose. These blisters are often grouped together in patches. After the blisters break, a crust forms over the resulting sore. Oral herpes usually heal in two to four weeks without leaving a scar. Some people have no symptoms from the infection. But others develop painful and unsightly cold sores. Oral herpes usually occur outside the mouth, on or around your lips. When they are inside the mouth, they are usually on the gums or the roof of the mouth. Oral herpes is not the same as canker sores (aphthous stomatitis), which is the most common cause of mouth ulcer, and presents as a painful punched-out sore on oral or genital mucous membranes 2, 3, 4. Canker sores are not contagious and cause of canker sores is unknown 2, 5.
There are two types of herpes simplex virus (HSV):
- Type 1 herpes simplex virus (HSV-1) usually causes oral herpes, fever blisters or cold sores. Type 1 herpes simplex virus (HSV-1) infects more than half of the U.S. population by the time they reach their 20s. HSV-1 is mainly transmitted via contact with the virus in sores, saliva or surfaces in or around the mouth. People may be exposed to HSV-1 as children due to close skin-to-skin contact with someone infected. Less commonly, HSV-1 can be transmitted to the genital area through oral-genital contact to cause genital herpes. Type 1 herpes simplex virus (HSV-1) can be transmitted from oral or skin surfaces that appear normal; however, the greatest risk of transmission is when there are active sores. People who already have HSV-1 are not at risk of reinfection, but they are still at risk of acquiring HSV-2.
- Type 2 herpes simplex virus (HSV-2) usually affects the genital area. Herpes simplex virus type 2 (HSV-2) usually causes sores on the genitals or sexual organs (genital herpes). Genital herpes is a sexually transmitted infection (STI). HSV-2 is mainly transmitted during sex through contact with genital or anal surfaces, skin, sores or fluids of someone infected with the virus. HSV-2 can be transmitted even if the skin looks normal and is often transmitted in the absence of symptoms.
- However, either HSV-1 or HSV-2 can affect almost any area of skin or mucous membrane. Once you’re infected, you have the virus for the rest of your life.
- Recurrent outbreaks of genital herpes caused by HSV-1 are often less frequent than outbreaks caused by HSV-2.
- In rare circumstances, herpes (HSV-1 and HSV-2) can be transmitted from mother to child during delivery, causing neonatal herpes.
A person with type 1 herpes simplex virus (HSV-1) in tissues of the mouth can pass the virus to the genitals of a sexual partner during oral sex. It can be spread at any time, even when the person who has herpes isn’t experiencing any symptoms. The newly caught infection is a genital herpes infection. If you touch sores on your lips, you can carry the virus on your fingers. Then you can pass it onto other parts of your body, including your eyes.
Neither HSV-1 nor HSV-2 survives well at room temperature. So the virus is not likely to spread through surfaces, such as a faucet handle or a towel. But kissing or sharing a drinking glass or silverware might spread the virus.
Even though oral herpes are called cold sores, they have nothing to do with having a cold. You catch oral herpes by coming into close contact with someone who has oral herpes, such as by kissing. Also, not everyone who comes into contact with the herpes virus will get oral herpes. For these people, the herpes simplex virus (HSV) just never becomes active. But the majority of people who are exposed to oral herpes will have some sort of reaction. It may be that they get one oral herpes and never have another. Or they may have oral herpes outbreaks several times a year.
After the primary episode of infection, the herpes simplex virus (HSV) resides in a latent state in spinal dorsal root nerves (in the trigeminal sensory ganglion) that supply sensation to your skin 6 and reactivation can be triggered by trauma, stress, immunosuppression, and sunlight exposure 7. During a recurrence, the herpes simplex virus follows the nerves onto your face, mouth, lips, oropharyngeal, and eye mucosa, where it multiplies, causing the clinical lesion. After each attack and lifelong, it enters the resting state.
During an attack, the herpes simplex virus (HSV) can be inoculated into new sites of your skin, which can then develop blisters as well as the original site of infection.
Because oral herpes are caused by a virus there is no cure for cold sores. They normally go away on their own in a few weeks. Antiviral medicines can help them heal faster. They can also help to prevent cold sores in people who often get them. Other medicines can help with the pain and discomfort of the sores. These include ointments that numb the blisters, soften the crusts of the sores, or dry them out. Protecting your lips from the sun with sunblock lip balm can also help.
Oral herpes key points:
- Fifty percent to 80 percent of U.S. adults have oral herpes.
- Oral herpes can be spread through intimate contact (e.g., kissing or oral sex) with someone who is infected.
- Oral herpes can be difficult to diagnose. Often confused with many other infections, it can only be confirmed with a virus culture called PCR (polymerase chain reaction), blood test or biopsy. PCR is the preferred test for diagnosing herpes infections.
- The best treatment for oral herpes is antiviral oral medication. Symptomatic treatment may include antiviral ointment, over-the-counter topical anesthetics or over-the-counter anti-inflammatory agents.
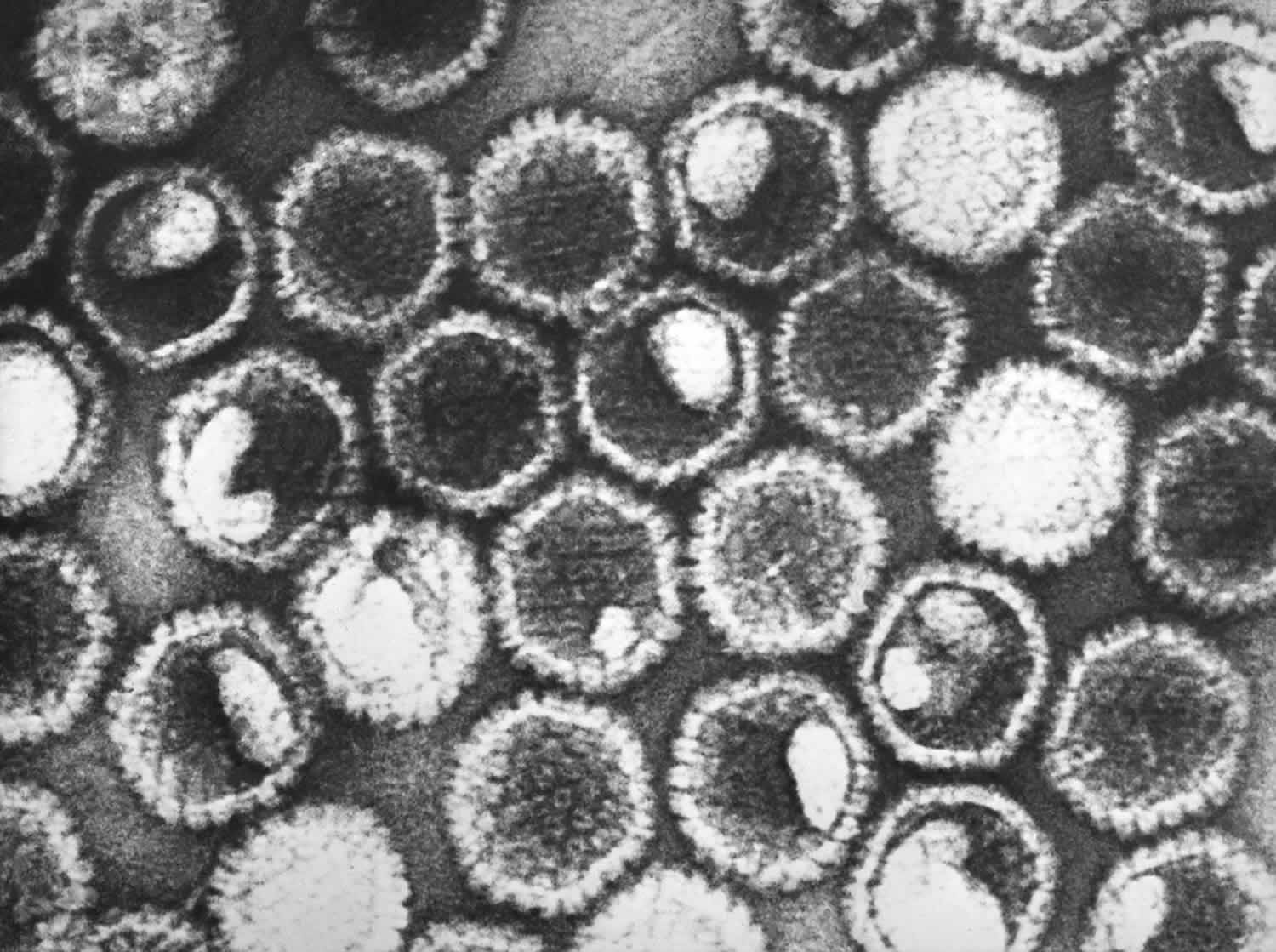
Figure 1. Herpes simplex virus (HSV)
Footnote: This negatively stained transmission electron microscopic image revealed the presence of numerous herpes simplex virions. At the core of its icosahedral proteinaceous capsid, the HSV contains a double-stranded DNA linear genome.
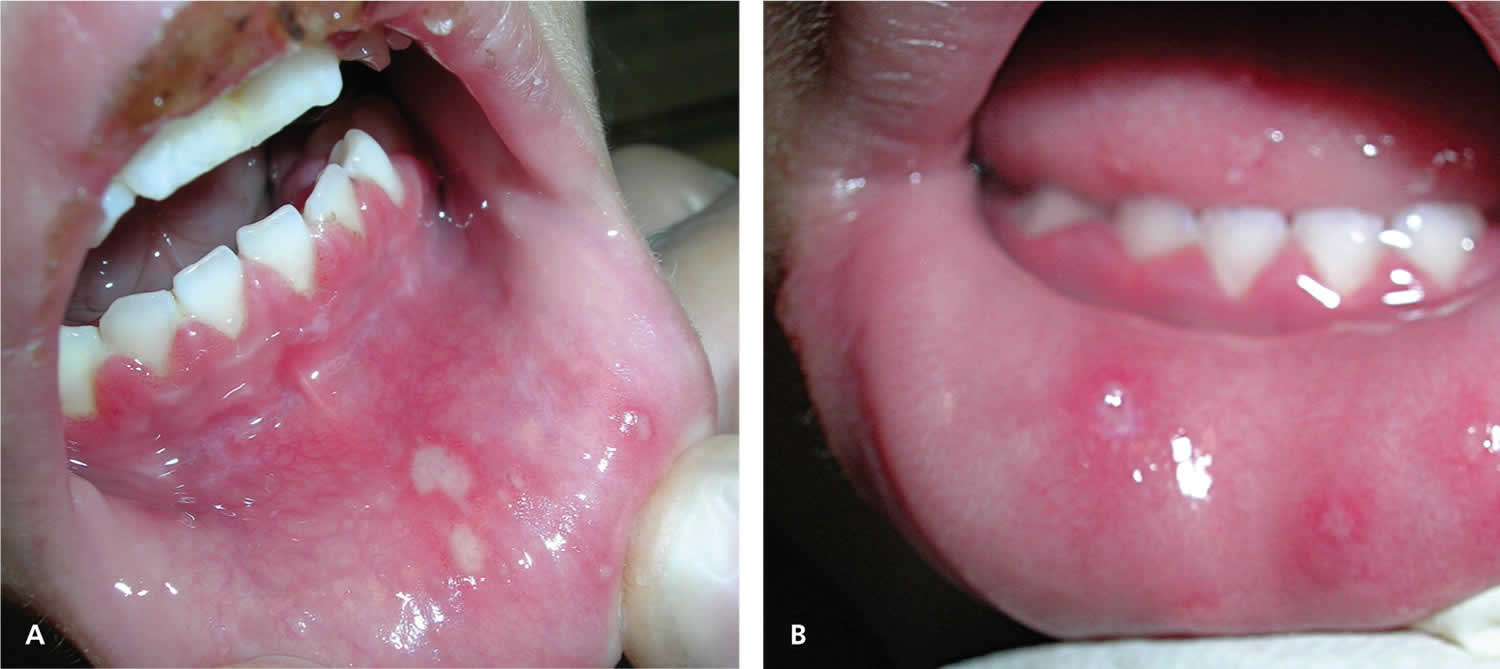
[Source 8 ]Figure 2. Primary oral herpes (primary herpetic gingivostomatitis) caused by herpes simplex virus type 1
Footnote: (A) a four-year-old girl with lower lip ulcers and crusting on the upper lip, and (B) a two-year-old girl with ulcers on the lower lip and tongue. Both patients show visible gingivitis with reddened, inflamed, and swollen gums.
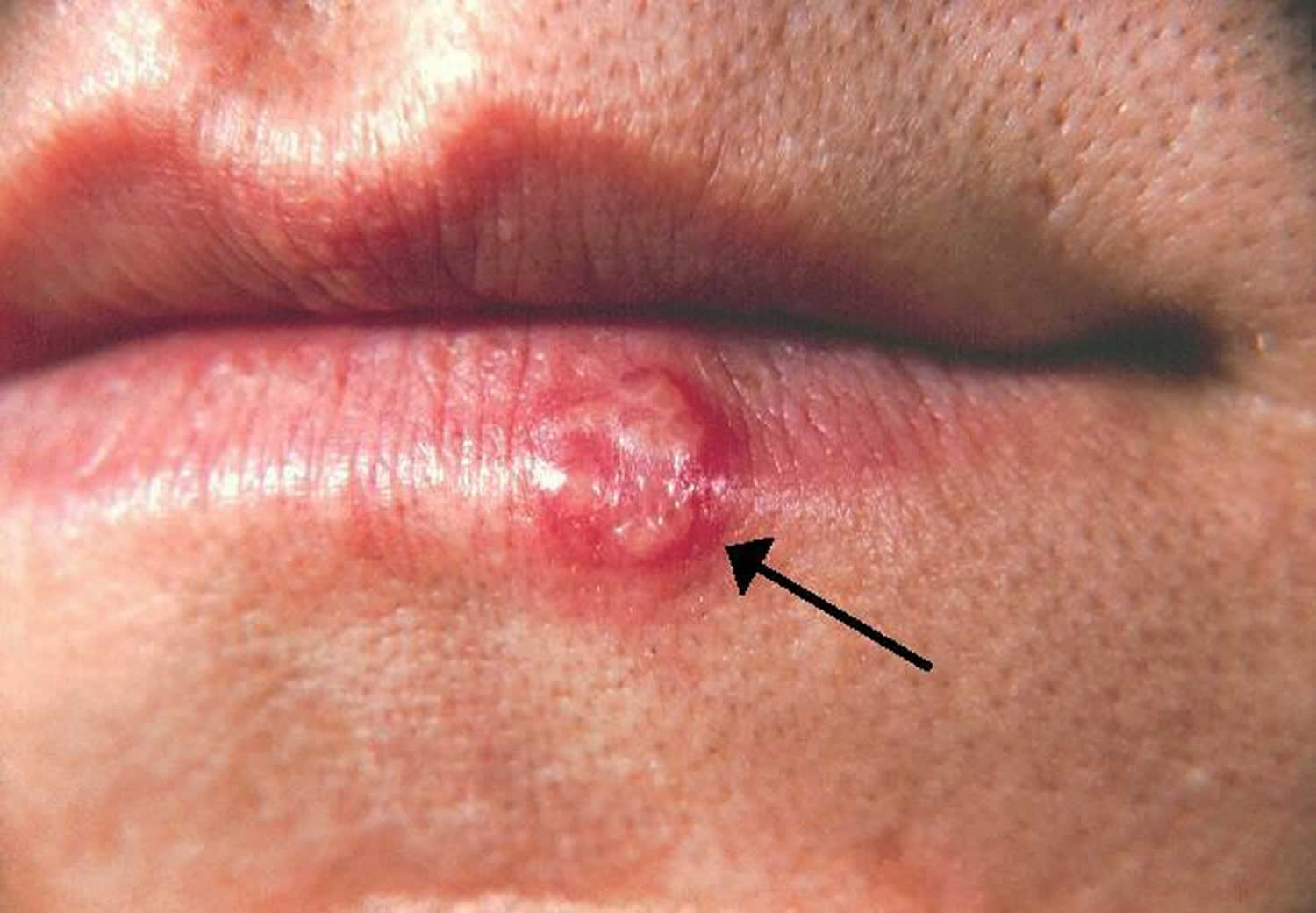
[Source 9 ]Figure 3. Cold sore on lip
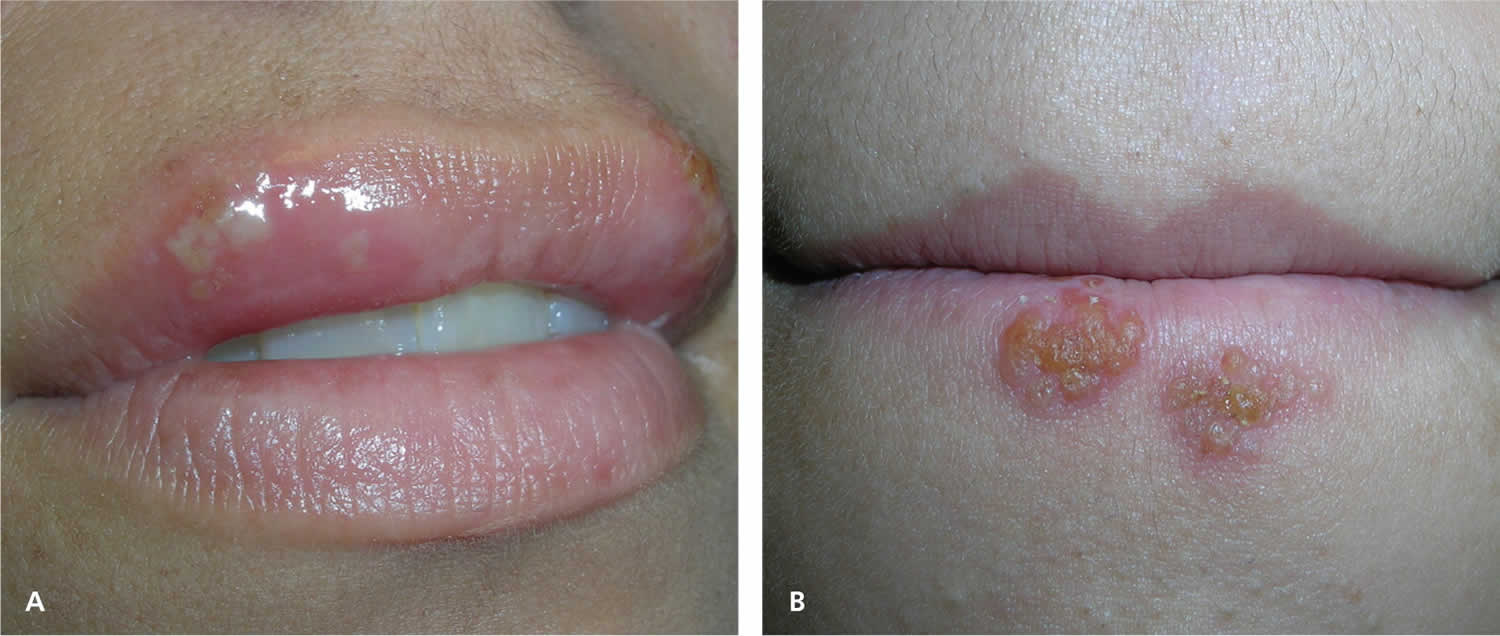
Figure 4. Recurrent herpes simplex virus
Footnote: Young girl with recurrent herpes simplex virus type 1 showing vesicles on a red base at the vermilion border.
[Source 9 ]Figure 5. Recurrent oral herpes
Footnote: (A) Ulcers that form after the vesicles break, as shown in an adult women with herpes labialis. (B) Recurrent herpes simplex virus type 1 in the crusting stage seen at the vermilion border.
[Source 9 ]Figure 6. Oral herpes tongue in a patient with weak immune system causing a severe and large ulcer on tongue
Figure 7. Facial herpes
Cold sores generally clear up without treatment. See your doctor if you have more severe symptoms or a weakened immune system (e.g., you have HIV, on immune suppressant medications or you are having cancer treatment):
- You have a weakened immune system
- The cold sores don’t heal within two weeks
- Symptoms are severe
- You have frequent recurrences of cold sores
- You experience irritation in your eyes
It’s also a good idea to see your doctor if:
- there are signs the cold sore is infected, such as redness around the sore, pus and a fever
- you aren’t sure you have a cold sore
- the cold sore isn’t healing, it’s spreading or you have more than one cold sore
- your cold sore has spread to near your eyes
- you get cold sores often
Antibiotics may be needed if the cold sore gets infected.
Does having oral herpes mean I have a sexually transmitted infection?
Having a cold sore does not mean that you have a sexually transmitted infection (STI). Most cold sores are caused by herpes simplex virus type 1 (HSV-1). Genital herpes (a type of STD) is typically caused by HSV-2. However, it is possible to transmit HSV-1 from a cold sore to the genital area during oral sex. In short, it is possible to get genital herpes from a cold sore from oral sex.
Is oral herpes contagious?
Yes. Cold sores are contagious even if you don’t see the sores. Cold sores are spread from person to person by close contact, such as kissing. Cold sores are caused by a herpes simplex virus (HSV-1) closely related to the one that causes genital herpes (HSV-2). Both of these viruses can affect your mouth or genitals and can be spread by oral sex.
Who’s at risk of oral herpes?
Herpes simplex virus (HSV) infections occur in people of all races or ethnicities, ages, and sexes. Up to 80% of Americans are infected with HSV-1 by the time they are 30.
Can you get genital herpes from oral herpes?
Yes, it is possible to get genital herpes from oral sex.
Genital herpes is caused by the herpes simplex virus (HSV). There are two types of herpes viruses — HSV-1 and HSV-2. Genital herpes is usually caused by HSV-2; oral herpes (cold sores) is usually caused by HSV-1.
However, genital herpes can also be caused by HSV-1. Someone with HSV-1 can transmit the virus through oral contact with another person’s genitals, anus, or mouth, even if they don’t have sores that are visible at the time.
Other than abstinence (not having sex) the best way to help prevent herpes is to use a condom during any type of sex (oral, vaginal, or anal). Girls should have their partners use a dental dam every time they receive oral sex to help protect against genital herpes. And if either partner has a sore, it’s best to not have sex until the sore has cleared up.
How long does oral herpes last?
Oral herpes usually heal in two to four weeks without leaving a scar.
There’s no cure for herpes simplex virus (HSV) infection, and the blisters may return. Antiviral medications can help cold sores heal more quickly and may reduce how often they return.
Is it safe for a mother to breastfeed if she has active herpetic lesions?
Maybe. Women with herpetic lesions may transmit HSV to their infants by direct or indirect contact with the lesions. Breastfeeding is acceptable if no lesions are present on the breasts and if active lesions elsewhere on the mother are carefully and fully covered. In cases where a mother has herpetic lesions on her breast, the mother should temporarily refrain from breastfeeding her infant from the affected breast or feeding her infant expressed breast milk from the affected breast. She should discard expressed breast milk from the affected side until the lesions have healed. A mother may breastfeed her infant or express milk from the unaffected breast but should ensure that the lesions on the affected breast are completely covered to avoid transmission. Mothers should also follow appropriate hand hygiene practices to avoid transmission of herpes to her infant.
Some mothers may need additional support to maintain their milk production and/or supplement with their expressed human milk (previously expressed milk or expressed milk from the unaffected breast) or formula while herpetic lesions on the breast are healing. Mothers should talk with their physicians to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
Oral herpes causes
Oral herpes are caused by certain strains of the herpes simplex virus (HSV). Type 1 herpes simplex virus (HSV-1) usually causes cold sores. Type 2 herpes simplex virus (HSV-2) is usually responsible for genital herpes. However, either type can cause sores in the facial area or on the genitals. Most people who are infected with the herpes simplex virus that causes cold sores never develop signs and symptoms.
HSV-1 is typically spread through direct contact with contaminated saliva or other infected bodily secretions, as opposed to HSV-2, which is spread primarily by sexual contact.
Oral herpes are most contagious when oozing blisters are present. But you can transmit the virus to others even if you don’t have blisters. Shared eating utensils, razors and towels, as well as kissing, may spread HSV-1. Oral sex can spread HSV-1 to the genitals and HSV-2 to the lips.
Primary infection appears two to 20 days after contact with an infected person. Transmission involves mucous membranes and open or abraded skin. During one study of herpes labialis, the median duration of HSV-1 shedding was 60 hours when measured by polymerase chain reaction (PCR) and 48 hours when measured by culture 10. Peak viral DNA load occurred at 48 hours, with no virus detected beyond 96 hours of onset of symptoms 10. Recurrent infections may be precipitated by various stimuli, such as stress, fever, sun exposure, extremes in temperature, ultraviolet radiation, immunosuppression, or trauma. The virus remains dormant for a variable amount of time.
Once you’ve had an episode of herpes infection, the virus lies dormant in nerve cells in your skin and may emerge as another cold sore at the same place as before. Recurrence may be triggered by:
- Viral infection or fever
- Hormonal changes, such as those related to menstruation or pregnancy.
- Stress
- Trauma, such as that caused by dental work or cuts from shaving.
- Fatigue
- Surgery.
- Exposure to sunlight and wind
- Changes in your immune system
Oral HSV-1 usually recurs one to six times per year 11. The duration of symptoms is shorter and the symptoms are less severe during a recurrence.
The likelihood of reactivation of HSV infection differs between HSV-1 and HSV-2, and between the sacral and trigeminal anatomic sites. In one study, the mean monthly frequencies of recurrence were 0.33 genital HSV-2 infections, 0.12 orolabial HSV-1 infections, 0.020 genital HSV-1 infections, and 0.001 oral HSV-2 infections 12. This shows that recurrences are more likely when HSV-1 is oral and HSV-2 is genital.
Risk factors for getting oral herpes
About 90 percent of adults worldwide — even those who’ve never had symptoms of an infection — test positive for evidence of the herpes simplex virus (HSV) that causes cold sores.
People who have weakened immune systems are at higher risk of complications from the herpes simplex virus (HSV). Medical conditions and treatments that increase your risk of complications include:
- HIV/AIDS
- Severe burns
- Eczema
- Cancer chemotherapy
- Anti-rejection drugs for organ transplants
Oral herpes prevention
Oral herpes cannot always be avoided, but you may be able to help prevent them by treating them at the very first sign of a cold sore (usually the tingling stage). You also can try to avoid known cold sore triggers (some of these are unavoidable).
- Sunlight
- Stress
- Hormones
- Fatigue
- Fever
- A weak immune system or changes in your immune system
Wearing sunscreen and proactively managing stress may help. Ways to reduce stress include exercising, meditating, and doing things you enjoy each day. You should also try to get 7 to 8 hours of sleep each night.
Because the herpes simplex virus (HSV) is very contagious, it is important to take the following steps to prevent spread (transmission) of the virus during the prodromal phase (burning, tingling, or itching) and active phase (presence of blisters or sores) of HSV infections:
- Avoid sharing cups and eating utensils.
- Avoid kissing and performing oral sex.
- Avoid sharing lip balm and lipstick.
- Avoid sharing razors, towels, and other personal care items.
- Wash your hands with soap and water if you touch an active lesion.
Unfortunately, the virus can still be transmitted even when someone does not have active lesions.
Oral herpes symptoms
Oral herpes signs and symptoms vary, depending on whether this is your first outbreak (primary infection) or a recurrence. Primary infection is defined as first outbreak of oral herpes in patients with no existing antibodies to HSV-1 or HSV-2. The most common location for primary oral herpes infection is inside the mouth. In primary HSV, there are painful sores anywhere inside your mouth (herpetic gingivostomatitis) . The lymph nodes in your neck may or may not be swollen. In severe cases of HSV infection, oral herpes may involve the entire lining of your mouth and both lips. These severe infections may be accompanied by fever, sore throat, foul breath, and difficulty eating.
The mouth lesions (herpetic gingivostomatitis) consist of painful vesicles on a red, swollen base that occur on the lips, gingiva, oral palate, or tongue. The lesions ulcerate (Figure 2) and the pain can be severe. Refusal to eat or drink may be a clue to the presence of oral HSV. The lesions usually heal within 10 to 14 days 11.
During first-time oral herpes infection (primary infection), some people experience:
- Fever
- Painful eroded gums
- Sore throat
- Headache
- Muscle aches
- Swollen lymph nodes
Children under 5 years old may have oral herpes inside their mouths and the lesions are commonly mistaken for canker sores. Canker sores involve only the mucous membrane and aren’t caused by the herpes simplex virus.
In recurrent herpes labialis, symptoms of tingling, pain, pins and needles sensation (paresthesias), itching, and burning of the area precede the lesions in 60 percent of persons 11. This may happen 24 to 48 hours before the cold sore actually appears. The lesions then appear as clusters of tiny blisters on the lip or vermilion border (Figures 3 and 4). The tiny blisters may have an erythematous base. The tiny blisters subsequently break open and form a crust (Figure 5). Healing begins within three to four days, and reepithelization may take seven to eight days 11. A typical oral herpes outbreak can last several days, and the blisters can take two to four weeks to heal completely without treatment. However, many people who are exposed to HSV-1 demonstrate asymptomatic seroconversion.
For recurrent oral herpes, locations include the:
- Lips.
- Nose.
- Chin.
- Cheeks.
Recurrences typically appear at the same spot each time and tend to be less severe than the first outbreak. There may also be sores inside your mouth, especially if your immune system has been affected, such as by cancer or HIV, or if you have undergone organ transplantation (Figure 6).
Additionally, some people never develop the symptoms of a primary HSV infection and may mistake a recurrent infection for a primary infection. A recurrent infection typically lasts 7-10 days. As it fades, it may leave a pink, purplish, or brownish color in lighter skin colors. In darker skin colors, HSV may fade to leave a darker brown color. People who are prone to recurrent outbreaks tend to get them 3-4 times per year.
Recurrent oral herpes usually passes through several stages:
- Tingling and itching. Many people feel an itching, burning or tingling sensation around their lips for a day or so before a small, hard, painful spot appears and blisters erupt.
- Blisters. Small fluid-filled blisters typically break out along the border where the outside edge of the lips meets the skin of the face. Cold sores can also occur around the nose or on the cheeks.
- Oozing and crusting. The small blisters may merge and then burst, leaving shallow open sores that will ooze fluid and then crust over.
Symptoms of recurrent oral herpes are typically milder than those of primary infection, with a 24-hour prodrome of tingling, burning, and itch 13. Recurrent orolabial HSV-1 infections classically affect the vermillion border of the lip (as opposed to the mouth and lips as seen in primary infection) 14.
Oral herpes complications
In immunocompromised people, including those with advanced HIV infection, herpes can have more severe symptoms and more frequent recurrences. Rare complications of HSV-2 include meningoencephalitis (brain infection) and disseminated infection. Rarely, HSV-1 infection can lead to more severe complications such as encephalitis (brain infection) or keratitis (eye infection). In some people, herpes simplex virus (HSV) that causes cold sores can cause problems in other areas of the body, including:
Eye infection
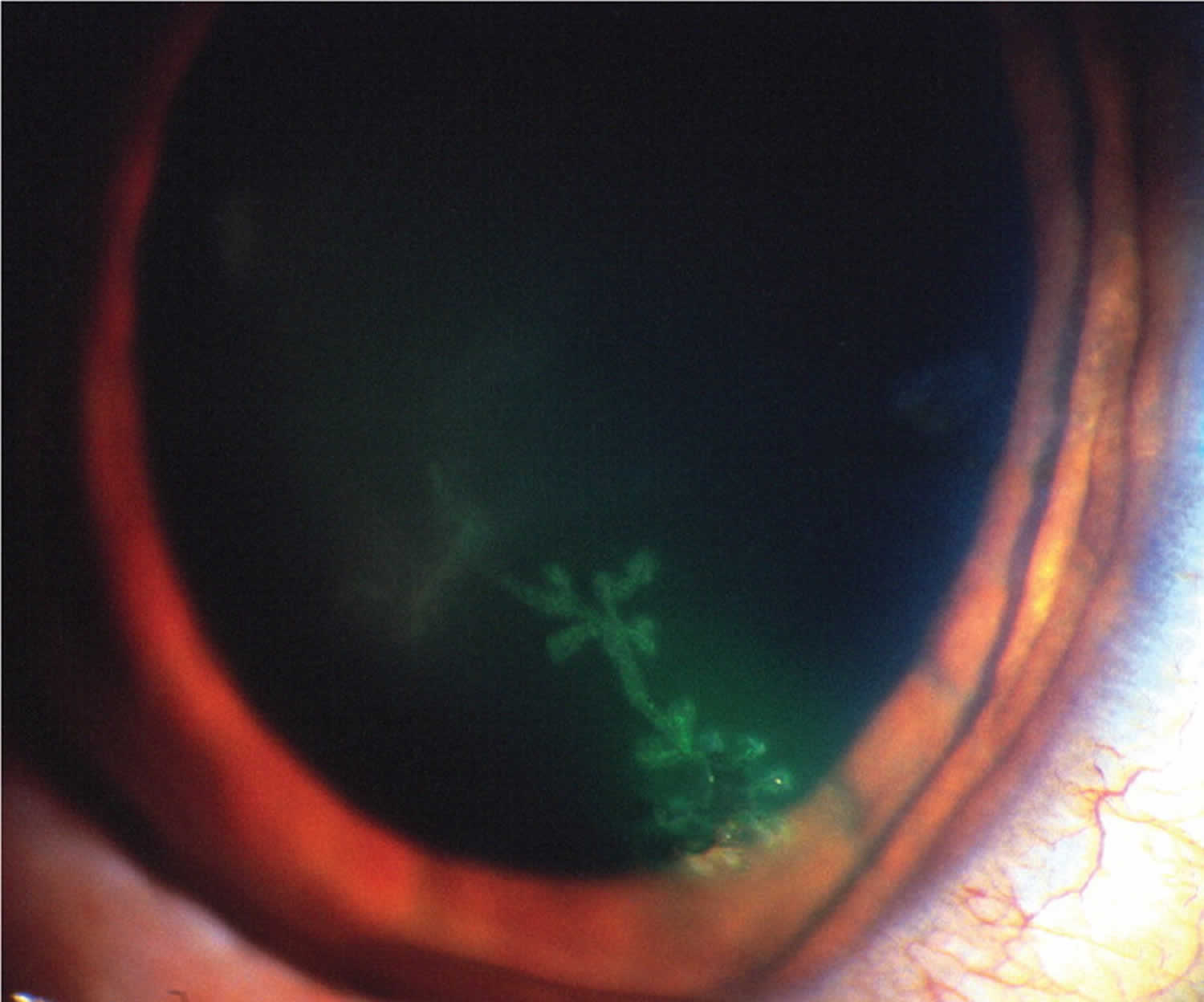
Herpes simplex may cause swollen eyelids and conjunctivitis with opacity and superficial ulceration of the cornea (dendritic ulcer, best seen after fluorescein staining of the cornea). HSV infection of the eye also known as herpetic keratitis is a common cause of blindness in the United States 15, 16, 17, 18. Common symptoms are eye pain, light sensitivity, and discharge with gritty sensation in the eye. Fluorescein stain with a ultraviolet light may show a classic dendritic ulcer on the cornea (Figure 8). Without prompt treatment, scarring of the cornea may occur (Figure 9).
Figure 8. HSV infection of the eye
Footnote: Slit-lamp view of a dendritic ulcer with fluorescein uptake from herpetic keratitis.
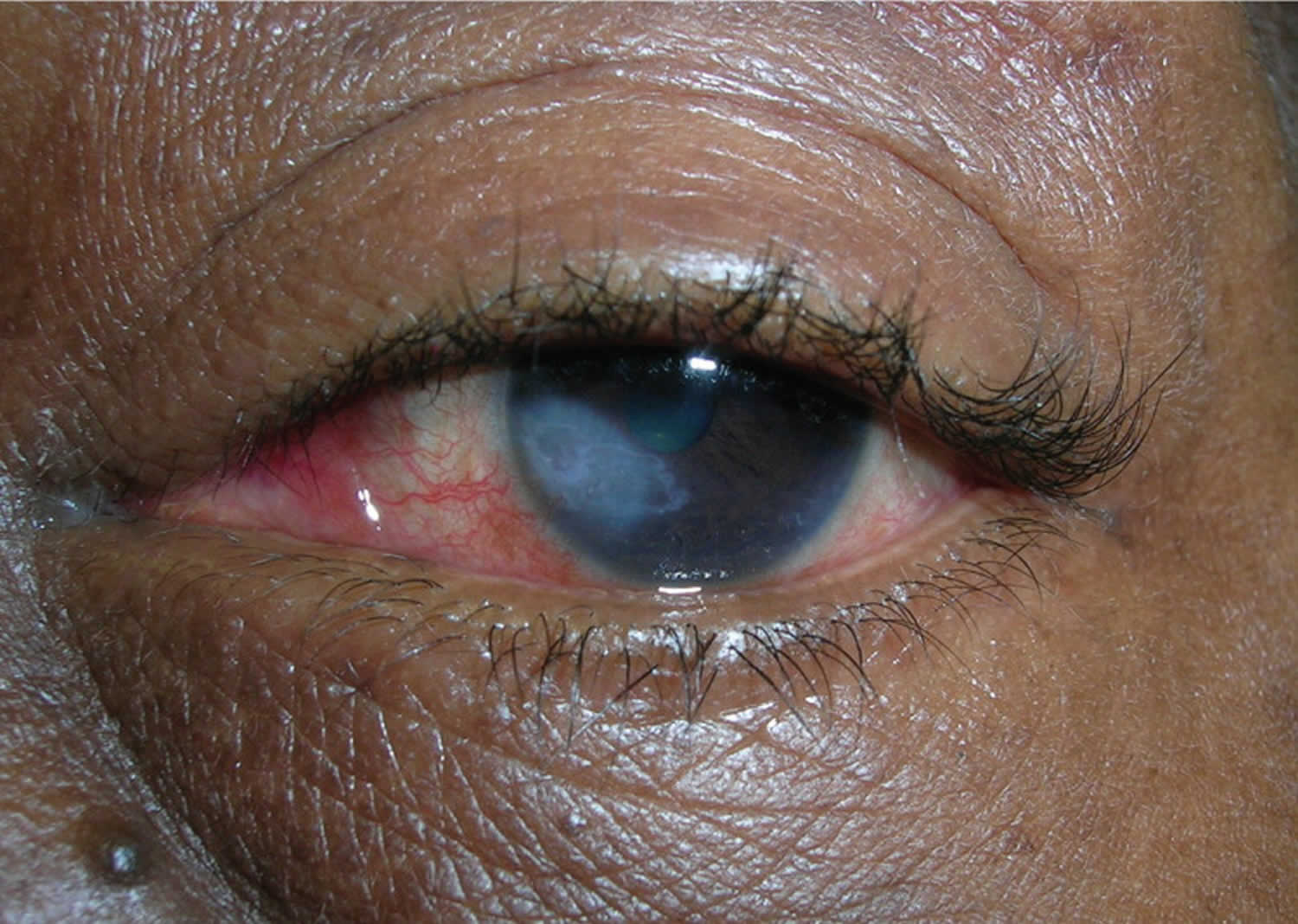
[Source 19 ]Figure 9. Herpetic keratitis with corneal scarring
Footnote: Herpetic keratitis with corneal scarring in a 56-year-old woman
[Source 9 ]Throat infection
Throat infections may be very painful and interfere with swallowing.
Eczema herpeticum
In patients with a history of atopic dermatitis, Darier disease, Hailey-Hailey disease, mycosis fungoides, and all types of ichthyosis, herpes simplex virus (HSV) may result in severe and widespread infection, known as eczema herpeticum. The skin disease can be active or historical. Numerous blisters erupt on the face or elsewhere, associated with swollen lymph glands and fever. The increased risk is also associated with mutations in the filaggrin gene, which is seen in atopic dermatitis and ichthyosis vulgaris. Pharmaceutical risk factors for eczema herpeticum include the use of topical calcineurin inhibitors such as pimecrolimus and tacrolimus.
Erythema multiforme
A single episode or recurrent erythema multiforme is an uncommon reaction to herpes simplex. The rash of erythema multiforme appears as symmetrical plaques on hands, forearms, feet and lower legs. It is characterized by target lesions, which sometimes have central blisters. Mucosal lesions may be observed.
Nervous system
Cranial or facial nerves may be infected by herpes simplex virus (HSV), producing temporary paralysis of the affected muscles. Rarely, neuralgic pain may precede each recurrence of herpes by 1 or 2 days (Maurice syndrome). Meningitis is rare. A major risk factor for herpes encephalitis is mutations in the toll-like receptor (TLR-3) or UNC-93B genes 13. It has been postulated that these mutations inhibit normal interferon-based responses.
Widespread infection
Disseminated infection and/or persistent ulceration due to herpes simplex virus (HSV) can be serious in debilitated or immune deficient patients, for example in people with human immunodeficiency virus (HIV) infection, transplant recipients (solid organ or hematopoietic stem cells) or leukemia/lymphoma patients 20, 21.
In the immunocompromised patient population, HSV infection can result in severe and chronic infection. The most common presentation of severe and chronic HSV infection is quickly enlarging ulcerations or verrucous/pustular lesions. It is not uncommon for patients to have respiratory or gastrointestinal tract involvement and present with shortness of breath (dyspnea) or difficulty or painful swallowing (dysphagia) 22, 23, 24, 25.
Neonatal herpes
Neonatal herpes can occur when an infant is exposed to HSV during vaginal delivery. Neonatal herpes simplex virus infection is rare, occurring in an estimated 1 in 1000 newborns in the United States. However, it is a serious condition that can lead to lasting neurologic disability or death. Women with recurrent genital herpes have a low risk of vertically transmitting HSV to their newborn baby. However, risk for neonatal herpes is greatest when a mother acquires HSV for the first time in late pregnancy.
Oral herpes diagnosis
Your doctor can usually diagnose oral herpes just by looking at them (grouped vesicles or ulcers on an erythematous base). To confirm the diagnosis, he or she may take a sample from the blister for testing in a laboratory by culture or polymerase chain reaction (PCR) of a viral swab taken from fresh vesicles. The most sensitive and specific mechanism is viral polymerase chain reaction (PCR). Herpes simplex virus (HSV) serology is not very informative, as it’s positive in most individuals and thus not specific for the lesion with which they present. Viral culture, direct fluorescent antibody (DFA) assay, and Tzanck smear are alternative methods of diagnosing. It is important to note that the Tzanck smear identifies multinucleated giant cells, so it cannot distinguish between HSV and varicella zoster virus (VZV) 13. The direct fluorescent antibody (DFA) assay, however, can distinguish between the 2 entities 26.
Oral herpes differential diagnosis
The differential diagnosis of nongenital herpes simplex virus (HSV) infection includes:
- Aphthous ulcers (canker sores),
- Acute paronychia,
- Varicellazoster virus infection,
- Herpangina,
- Herpes gestationis (pemphigoid gestationis),
- Pemphigus vulgaris, and
- Behçet syndrome.
Oral herpes treatment
Oral herpes generally clear up without treatment in two to four weeks. Oral herpes treatment includes managing outbreaks with over-the-counter (OTC) creams to prescription drugs to home remedies that include ice packs and aloe vera gels. Which you choose will depend on how many outbreaks you have and what works best for you.
For episodic treatment, oral antiviral agents, such as acyclovir (Zovirax), valacyclovir (Valtrex) and famciclovir (Famvir), are superior to topical antiviral therapy 27. Valacyclovir and famciclovir have greater oral bioavailability and are better absorbed than acyclovir, require less frequent dosing, but are more expensive and are not approved for children 27. Topical antiviral agents such as 5% acyclovir cream/ointment (Zovirax) ± hydrocortisone (Xerese), 1% penciclovir (Denavir) cream, and 50 mg Buccal Adhesive Tablet (ABT-50 mg) can also be used for episodic treatment of herpes labialis 27. These topical agents are not effective in the prevention of recurrent herpes labialis. For chronic daily suppressive therapy, oral antivirals are the treatment of choice 27.
Prescription medicines
If you have several outbreaks a year, you should see your family doctor. They will work with you on a treatment plan that may include prescription antiviral medicine. Oral antiviral medications include:
- Acyclovir (Zovirax) – 200 mg 5 times daily for five days
- OR
- Acyclovir (Zovirax) – 400 mg 3 times daily for five days
- OR
- Famciclovir (Famvir) – as a single dose of 3 x 500 mg
- OR
- Valacyclovir (Valtrex) – 1 g 3 times daily for seven days
- OR
- Valacyclovir (Valtrex) – 2 grams twice daily for one day
Some of these products are packaged as pills to be swallowed. Others are creams to be applied to the sores several times a day. In general, the pills work better than the creams. For very severe infections, some antiviral drugs can be given with an injection. These medicines not only help speed healing, they also may prevent future outbreaks.
Topical aciclovir or penciclovir may shorten attacks of recurrent herpes simplex, provided the cream is started early enough.
Higher doses of antiviral drugs are used for eczema herpeticum or for disseminated herpes simplex.
Your doctor may also prescribe you a numbing gel if your cold sore is painful.
OTC treatments
If your outbreaks aren’t as severe or frequent, an OTC medicine should help soothe and heal your cold sore. There are a variety of OTC creams, gels, patches, lip balms, and even lasers designed to minimize symptoms and shorten the cold sore cycle. A small sampling of popular products include:
- Creams, gels and ointments containing the drugs aciclovir (Zovirax cream 5%) or penciclovir (Denavir) are available in pharmacies without a prescription. For them to be able to work, they have to be applied to the affected area every 2 to 3 hours during the daytime. The treatment lasts five days, but should not exceed 10 days 28.
- Docosanol (Abreva) is an FDA approved cream safe for people 12 years of age and older. If you begin using it at first tingle, it can shorten healing time. It also helps minimize symptoms.
- Zilactin Cold Sore Gel relieves pain and promotes healing with an active ingredient of 10% benzyl alcohol. The gel creates a protective barrier over your cold sore.
- Orajel Cold Sore Patented Treatment is a liquid treatment with touch-free applicator. It cleans the affected area and provides pain relief.
- Mederma cold sore patch uses hydrocolloid gel to boost recovery and reduce scab formation.
- Compeed Cold Sore Patch conceals your cold sore while it heals it. The patch also helps prevent speading your cold sore to others.
- Laser treatment is the latest—and priciest—treatment to enter the market. The Virulite Invisible Light Electronic Cold Sore Treatment Device is FDA approved to treat your cold sore at home. Treatments may result in clearing cold sore in a matter of days.
- Acetaminophen (Tylenol) and ibuprofen (Advil) both help relieve cold sore pain.
There is also a combination drug (Zovirax Duo) that contains both aciclovir and a mild steroid 29, 30, 31. One study looked into whether this combination drug can lower the risk of cold sore blisters and scabs forming 31. The combination drug (Zovirax Duo) that contains both aciclovir and a mild steroid was either compared with aciclovir used alone or with a non-medicated cream (placebo). The people in the study had an average of 5 to 6 cold sores per year, and their cold sores often crusted over and formed scabs. They started using the treatment as soon as they noticed the first signs of a cold sore developing. The study suggests that the combination of aciclovir and a steroid is somewhat more effective than aciclovir alone 31. In other words, compared to aciclovir alone, the combination drug (Zovirax Duo that contain both aciclovir and a mild steroid) prevented the development of blisters and scabs in an extra 7 out of 100 people 31. Topical treatments for cold sores can sometimes irritate the skin a bit, but no serious side effects occurred in the studies.
To ease the discomfort of a cold sore:
- Try other cold sore remedies. Some over-the-counter preparations contain a drying agent, such as alcohol, that may speed healing.
- Use lip balms and cream. Protect your lips from the sun with a zinc oxide cream or lip balm with sunblock. If your lips become dry, apply a moisturizing cream.
- Apply a cool compress. A cool, damp cloth may reduce redness, help remove crusting and promote healing.
- Apply pain-relieving creams. Over-the-counter creams with lidocaine or benzocaine may offer some pain relief.
Home remedies for oral herpes
There are many home remedies for treating a cold sore. Some may be effective. However, there is no medical evidence that these methods can shorten healing time or provide pain relief.
- Aloe vera gel
- Vitamins C and vitamin E
- Tea tree oil
- Peppermint oil
- Lemon balm
- Vanilla extract
- Tea bag
- Ice
- Lysine. An amino acid, lysine is available as an oral supplement and as a cream.
- Propolis. Also known as synthetic beeswax, this is available as a 3 percent ointment. When applied early and often, it may shorten the duration of the breakout.
- Rhubarb and sage. A cream combining rhubarb and sage may be about as effective as acyclovir (Zovirax) cream.
- Stress reduction. If your cold sores are triggered by stress, you might want to try relaxation techniques, such as deep-breathing exercises and meditation.
Whichever treatment you choose for your cold sore, know that it has the best chance of working if you start it during the tingling stage.
Recurring oral herpes treatment
Oral acyclovir is effective in suppressing herpes labialis in immunocompetent adults with frequent recurrences. In one randomized control trial, treatment with oral acyclovir (400 mg twice per day) resulted in a 53 percent reduction in the number of clinical recurrences and a 71 percent reduction in virus culture-positive recurrences compared with placebo 32. The median time to first clinically documented recurrence was 46 days for placebo courses and 118 days for acyclovir courses 32. The mean number of recurrences per four-month treatment period was 1.80 episodes per patient during placebo treatment and 0.85 episodes per patient during acyclovir treatment 32.
Treatment with oral valacyclovir (500 mg per day) for 16 weeks was compared with placebo in the suppression of herpes labialis in patients with a history of four or more recurrent lesions in the previous year 33. Results showed 60 percent of persons in the valacyclovir group were recurrence-free throughout the study period compared with 38 percent in the placebo group. The mean time to first recurrence was longer with valacyclovir (13.1 weeks) compared with placebo (9.6 weeks) 33.
In a Cochrane review of herpes labialis prevention in patients receiving treatment for cancer, acyclovir was found to be effective in the prevention of HSV infections, as measured by oral lesions or viral isolates 34. There was no evidence that valacyclovir is more effective than acyclovir. In another study, daily valacyclovir (500 mg per day) and acyclovir (400 mg twice per day) were equally effective in the prevention of recurrent HSV eye disease 35.
Oral herpes prognosis
Overall, the vast majority of HSV-1 infections are asymptomatic, and if symptomatic present with mild recurrent cold sores. The prognosis of HSV-1 infection varies depending on your age, your overall health and avoiding of specific triggers (e.g., trauma, stress, immunosuppression, and sunlight exposure) that cause oral herpes to recur 7. The majority of the time, HSV-1 infection follows a chronic course of latency and reactivation. HSV encephalitis is associated with high mortality; approximately 70% of untreated cases are ultimately fatal. The prognosis of ocular HSV can also be grim if the patient develops eyeball rupture or corneal scarring, as these processes can ultimately lead to blindness 36.
References- Fatahzadeh M. Oral Manifestations of Viral Infections. Atlas Oral Maxillofac Surg Clin North Am. 2017 Sep;25(2):163-170. doi: 10.1016/j.cxom.2017.04.008
- Shah K, Guarderas J, Krishnaswamy G. Aphthous stomatitis. Ann Allergy Asthma Immunol. 2016 Oct;117(4):341-343. doi: 10.1016/j.anai.2016.07.005
- Messadi, D.V. and Younai, F. (2010), Aphthous ulcers. Dermatologic Therapy, 23: 281-290. https://doi.org/10.1111/j.1529-8019.2010.01324.x
- Staines K, Greenwood M. Aphthous ulcers (recurrent). BMJ Clin Evid. 2015 Feb 26;2015:1303. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4356175
- Brocklehurst P, Tickle M, Glenny AM, Lewis MA, Pemberton MN, Taylor J, Walsh T, Riley P, Yates JM. Systemic interventions for recurrent aphthous stomatitis (mouth ulcers). Cochrane Database Syst Rev. 2012 Sep 12;(9):CD005411. doi: 10.1002/14651858.CD005411.pub2
- McIntyre GT. Viral infections of the oral mucosa and perioral region. Dent Update. 2001 May;28(4):181-6, 188. doi: 10.12968/denu.2001.28.4.181
- Bandara, HMHN, Samaranayake, LP. Viral, bacterial, and fungal infections of the oral mucosa: Types, incidence, predisposing factors, diagnostic algorithms, and management. Periodontol 2000. 2019; 80: 148– 176. https://doi.org/10.1111/prd.12273
- Centers for Disease Control and Prevention Public Health Image Library. Dr. Fred Murphy & Sylvia Whitfield, 1975.
- Nongenital Herpes Simplex Virus. Am Fam Physician. 2010;82(9):1075-1082. https://www.aafp.org/pubs/afp/issues/2010/1101/p1075.html
- Boivin G, Goyette N, Sergerie Y, Keays S, Booth T. Longitudinal evaluation of herpes simplex virus DNA load during episodes of herpes labialis. J Clin Virol. 2006 Dec;37(4):248-51. doi: 10.1016/j.jcv.2006.09.006
- Cernik C, Gallina K, Brodell RT. The treatment of herpes simplex infections: an evidence-based review. Arch Intern Med. 2008 Jun 9;168(11):1137-44. doi: 10.1001/archinte.168.11.1137
- Lafferty WE, Coombs RW, Benedetti J, Critchlow C, Corey L. Recurrences after oral and genital herpes simplex virus infection. Influence of site of infection and viral type. N Engl J Med. 1987 Jun 4;316(23):1444-9. doi: 10.1056/NEJM198706043162304
- Saleh D, Yarrarapu SNS, Sharma S. Herpes Simplex Type 1. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482197
- Williams C, Wells J, Klein R, Sylvester T, Sunenshine R; Centers for Disease Control and Prevention (CDC). Notes from the field: outbreak of skin lesions among high school wrestlers–Arizona, 2014. MMWR Morb Mortal Wkly Rep. 2015 May 29;64(20):559-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4584520
- Chaabane S, Harfouche M, Chemaitelly H, Schwarzer G, Abu-Raddad LJ. Herpes simplex virus type 1 epidemiology in the Middle East and North Africa: systematic review, meta-analyses, and meta-regressions. Sci Rep. 2019 Feb 4;9(1):1136. doi: 10.1038/s41598-018-37833-8
- Fedoreyev SA, Krylova NV, Mishchenko NP, Vasileva EA, Pislyagin EA, Iunikhina OV, Lavrov VF, Svitich OA, Ebralidze LK, Leonova GN. Antiviral and Antioxidant Properties of Echinochrome A. Mar Drugs. 2018 Dec 15;16(12):509. doi: 10.3390/md16120509
- Marchi S, Trombetta CM, Gasparini R, Temperton N, Montomoli E. Epidemiology of herpes simplex virus type 1 and 2 in Italy: a seroprevalence study from 2000 to 2014. J Prev Med Hyg. 2017 Mar;58(1):E27-E33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5432775
- Finger-Jardim, F, Avila, EC, da Hora, VP, Gonçalves, CV, de Martinez, AMB, Soares, MA. Prevalence of herpes simplex virus types 1 and 2 at maternal and fetal sides of the placenta in asymptomatic pregnant women. Am J Reprod Immunol. 2017; 78:e12689. https://doi.org/10.1111/aji.12689
- Usatine RP, Smith MA, Chumley H, Mayeaux EJ Jr, Tysinger J, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:83.
- Pfaff F, Groth M, Sauerbrei A, Zell R. Genotyping of herpes simplex virus type 1 by whole-genome sequencing. J Gen Virol. 2016 Oct;97(10):2732-2741. doi: 10.1099/jgv.0.000589
- van Oeffelen L, Biekram M, Poeran J, Hukkelhoven C, Galjaard S, van der Meijden W, Op de Coul E. Update on Neonatal Herpes Simplex Epidemiology in the Netherlands: A Health Problem of Increasing Concern? Pediatr Infect Dis J. 2018 Aug;37(8):806-813. doi: 10.1097/INF.0000000000001905
- Kolawole OM, Amuda OO, Nzurumike C, Suleiman MM, Ikhevha Ogah J. Seroprevalence and Co-Infection of Human Immunodeficiency Virus (HIV) and Herpes Simplex Virus (HSV) Among Pregnant Women in Lokoja, North-Central Nigeria. Iran Red Crescent Med J. 2016 Aug 10;18(10):e25284. doi: 10.5812/ircmj.25284
- El Hayderi L, Rübben A, Nikkels AF. The alpha-herpesviridae in dermatology : Herpes simplex virus types I and II. Hautarzt. 2017 Dec;68(Suppl 1):1-5. English. doi: 10.1007/s00105-016-3919-7
- Li Z, Breitwieser FP, Lu J, Jun AS, Asnaghi L, Salzberg SL, Eberhart CG. Identifying Corneal Infections in Formalin-Fixed Specimens Using Next Generation Sequencing. Invest Ophthalmol Vis Sci. 2018 Jan 1;59(1):280-288. doi: 10.1167/iovs.17-21617
- El Hayderi L, Rübben A, Nikkels AF. Alpha-Herpesviridae in der Dermatologie : Herpes-simplex-Virus Typ I und II [The alpha-herpesviridae in dermatology : Herpes simplex virus types I and II. German version]. Hautarzt. 2017 Mar;68(3):181-186. German. doi: 10.1007/s00105-016-3929-5
- Giraldo D, Wilcox DR, Longnecker R. The Type I Interferon Response and Age-Dependent Susceptibility to Herpes Simplex Virus Infection. DNA Cell Biol. 2017 May;36(5):329-334. doi: 10.1089/dna.2017.3668
- Leung AKC, Barankin B. Herpes Labialis: An Update. Recent Pat Inflamm Allergy Drug Discov. 2017;11(2):107-113. doi: 10.2174/1872213X11666171003151717
- Glaxo Operations UK. ZOVIRAX Labialis, 50 mg/g, Crème Aciclovir (Package Insert) (2012).
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. How effective are creams and tablets for the treatment of cold sores? 2018 Jul 12. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525789
- Chen F, Xu H, Liu J, Cui Y, Luo X, Zhou Y, Chen Q, Jiang L. Efficacy and safety of nucleoside antiviral drugs for treatment of recurrent herpes labialis: a systematic review and meta-analysis. J Oral Pathol Med. 2017 Sep;46(8):561-568. https://doi.org/10.1111/jop.12534
- Arain N, Paravastu SC, Arain MA. Effectiveness of topical corticosteroids in addition to antiviral therapy in the management of recurrent herpes labialis: a systematic review and meta-analysis. BMC Infect Dis. 2015 Feb 21;15:82. doi: 10.1186/s12879-015-0824-0
- Rooney JF, Straus SE, Mannix ML, Wohlenberg CR, Alling DW, Dumois JA, Notkins AL. Oral acyclovir to suppress frequently recurrent herpes labialis. A double-blind, placebo-controlled trial. Ann Intern Med. 1993 Feb 15;118(4):268-72. doi: 10.7326/0003-4819-118-4-199302150-00004
- Baker D, Eisen D. Valacyclovir for prevention of recurrent herpes labialis: 2 double-blind, placebo-controlled studies. Cutis. 2003 Mar;71(3):239-42.
- Glenny AM, Fernandez Mauleffinch LM, Pavitt S, Walsh T. Interventions for the prevention and treatment of herpes simplex virus in patients being treated for cancer. Cochrane Database Syst Rev. 2009 Jan 21;(1):CD006706. doi: 10.1002/14651858.CD006706.pub2
- Miserocchi E, Modorati G, Galli L, Rama P. Efficacy of valacyclovir vs acyclovir for the prevention of recurrent herpes simplex virus eye disease: a pilot study. Am J Ophthalmol. 2007 Oct;144(4):547-51. doi: 10.1016/j.ajo.2007.06.001
- Gottlieb SL, Giersing BK, Hickling J, Jones R, Deal C, Kaslow DC; HSV Vaccine Expert Consultation Group. Meeting report: Initial World Health Organization consultation on herpes simplex virus (HSV) vaccine preferred product characteristics, March 2017. Vaccine. 2019 Nov 28;37(50):7408-7418. doi: 10.1016/j.vaccine.2017.10.084