What is Osgood Schlatter disease
Osgood-Schlatter disease (also called tibial tubercle apophysitis) is an inflammation of the bone, cartilage, and/or tendon at the top of the shinbone (tibia), where the tendon from the kneecap (patella) attaches caused by an overuse injury. Osgood Schlatter disease is really not a disease, but an overuse injury. Osgood-Schlatter disease causes pain at the tibial tubercle — the bony bump where the patellar tendon attaches to the tibia (shinbone). Osgood-Schlatter disease typically occurs in boys ages 12 to 14 and girls ages 10 to 13. The difference is because girls enter puberty earlier than do boys.
The pain from Osgood-Schlatter’s comes from a pulling of the patellar tendon on the tibial tubercle and the growth plate underneath. This condition most often occurs during growth spurts when bones, muscles, tendons, and other structures are growing. The muscle in the front of the thigh (quadriceps muscle) attaches to the kneecap (patella) and to the tibial tubercle through the patellar tendon. This tug-of-war concentrates at the tibial tubercle in growing children and teenagers. Children who participate in running and jumping sports are at an increased risk for this condition. However, less active adolescents may also experience this problem.
Children with Osgood Schlatter’s disease are at risk for other conditions such as osteochondritis dissecans because they are usually very active.
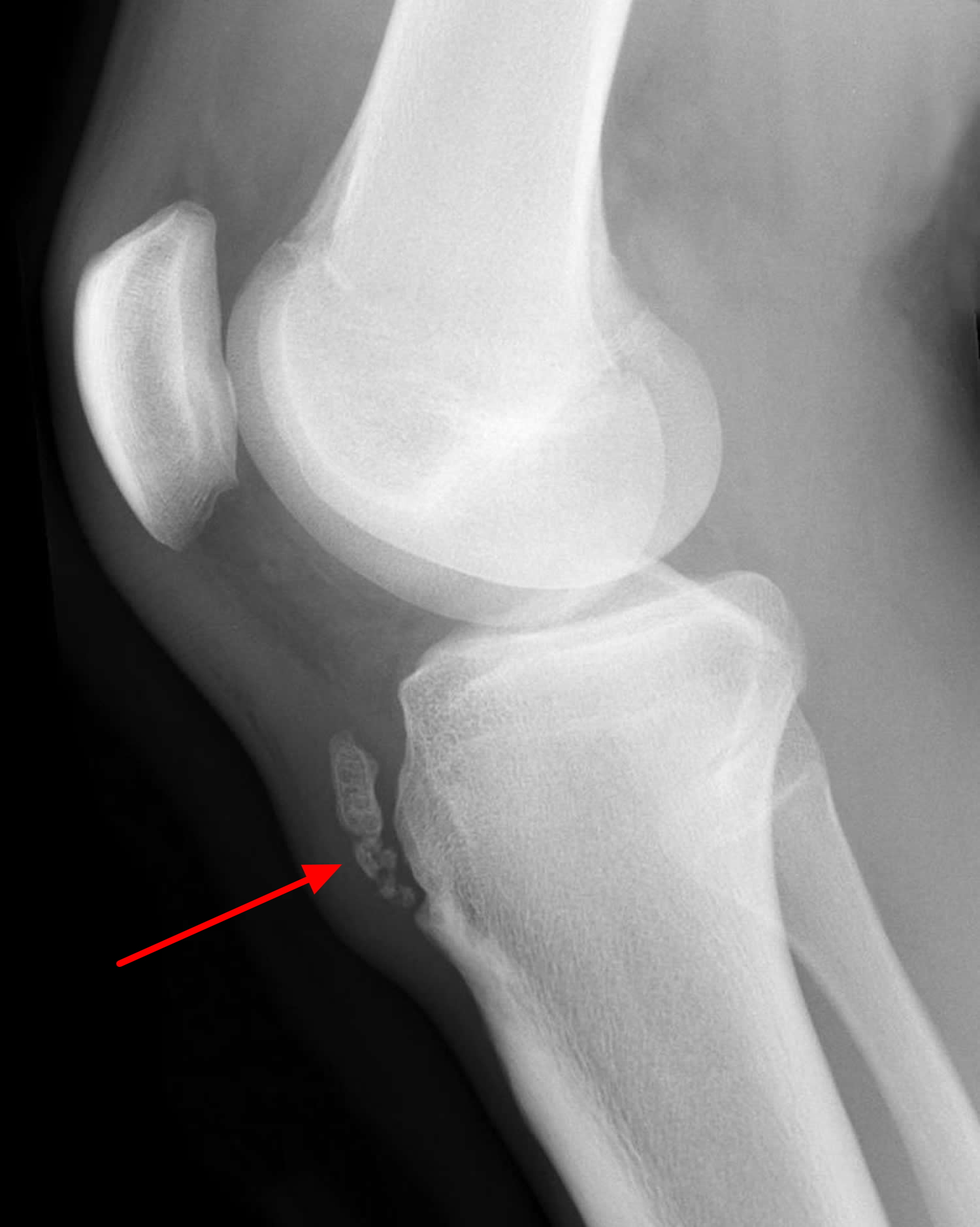
When a child straightens their knee, the quadriceps muscles pull on the patellar tendon, which pulls on the tibial tubercle. This repetitive traction on the tubercle can to inflammation of the growth plate. The patellar tendon remains strong, but the attachment at the growth plate can be weak and slowly separate. As the growth plate tries to heal, extra bone will form. This may be noticed as a bump at the front of the knee and may be seen on x-rays (see Figure 2).
Osgood Schlatter disease is one of the most common causes of knee pain in adolescents who participate in sports that involve running, jumping and swift changes of direction — such as soccer, basketball, figure skating and ballet. Osgood Schlatter disease can be quite painful and the discomfort can last from weeks to months, usually goes away within 12 to 24 months, but can recur until your child stops growing. Most often just one knee is affected.
Knee pain and swelling just below the kneecap are the main indicators of Osgood-Schlatter disease. Pain usually worsens during certain activities, such as running, kneeling and jumping, and eases with rest.
In most cases of Osgood-Schlatter disease, simple measures like rest, ice, over-the-counter medication, and stretching and strengthening exercises will relieve pain and allow a return to daily activities.
Figure 1. Knee anatomy
Osgood Schlatter disease prognosis
The knee pain almost always stops once your child is done growing, but the bump on the knee may be permanent. Removal of the bump of bone (ossicle) is rarely necessary. On rare occasions, the pain and inflammation worsen and the growth plate can give way with a jumping injury. A severe fracture can occur which may require surgery to repair.
Osgood-Schlatter disease complications
Complications of Osgood-Schlatter disease are uncommon. If they occur, they might include chronic pain or localized swelling.
Even after symptoms have resolved, a bony bump might remain on the shinbone just below the kneecap. This bump can persist to some degree throughout your child’s life, but it doesn’t usually interfere with knee function.
In rare cases, Osgood-Shlattter disease can cause the growth plate to be pulled away from the shinbone.
Osgood Schlatter disease causes
The bones of children and adolescents possess a special area where the bone is growing called the growth plate. Growth plates are areas of cartilage located near the ends of bones. When a child is fully grown, the growth plates harden into solid bone.
Some growth plates serve as attachment sites for tendons, the strong tissues that connect muscles to bones. A bony bump called the tibial tubercle covers the growth plate at the end of the tibia. The group of muscles in the front of the thigh (called the quadriceps) attaches to the tibial tubercle.
When a child is active doing activities that involve running, jumping and bending — such as soccer, basketball, volleyball and ballet, the quadriceps muscles pull on the patellar tendon which in turn, pulls on the tibial tubercle. In some children, this repetitive traction on the tubercle leads to inflammation of the growth plate resulting in the pain and swelling associated with Osgood-Schlatter disease. Some children’s bodies try to close that gap with new bone growth, which can result in a bony lump at that spot. The prominence, or bump, of the tibial tubercle may become very pronounced.
Osgood Schlatter disease pathophysiology
Strong repetitive quadriceps contractions are thought to cause a traction force on the tibial tuberosity, disrupting the immature bone. There is a higher incidence in active children during the adolescent growth spurt.
As a child grows, bones go through different stages of development:
- The tibial tuberosity is initially cartilaginous (cartilaginous stage).
- It then enters the apophyseal stage when the secondary ossification center (apophysis) appears.
- The unity of the proximal tibial epiphysis with the tibial apophysis marks the epiphyseal stage.
- Lastly, when the growth plates fuse, the bony stage has been reached.
Children are most susceptible to Osgood-Schlatter’s disease when their bones are in the (2nd) apophyseal stage.
During this phase, the apophysis is unable to withstand high tensile forces. When presented with strong, repetitive muscle contractions, micro-fractures occur in the immature area. The separation results in symptoms typical of Osgood Schlatter’s disease, as well as the irregular bone growth that explains an enlarged tibial tuberosity afterwards.
Another potential cause of Osgood Schlatter ‘s disease has been the lack of growth of the quadriceps in comparison to the femur. During a growth spurt in a child, the lengthening of the muscle is unable to keep up with the lengthening of the rapidly lengthening femur, resulting in an increased tensile force on the tibial tuberosity.
Risk factors for Osgood-Schlatter disease
The main risk factors for Osgood-Schlatter disease are:
- Age. Osgood-Schlatter disease occurs during puberty’s growth spurts. Age ranges differ by sex because girls enter puberty earlier than do boys. Osgood-Schlatter disease typically occurs in boys ages 12 to 14 and girls ages 10 to 13.
- Sex. Osgood-Schlatter disease is more common in boys, but the gender gap is narrowing as more girls become involved with sports.
- Sports. The condition happens most often with sports that involve running, jumping and swift changes in direction.
- Flexibility. Tightness in the quadriceps muscles can increase the pull of the kneecap’s tendon on the growth plate at the top of the shinbone.
Osgood Schlatter disease symptoms
Painful symptoms are often brought on by running, jumping, and other sports-related activities and decreased with rest. In some cases, both knees have symptoms, although one knee may be worse than the other.
- Knee pain and tenderness at the tibial tubercle
- Swelling at the tibial tubercle
- Tight muscles in the front or back of the thigh
The painful spot is over the bone at the top of the shinbone that is the attachment of the patellar tendon.
Osgood Schlatter disease diagnosis
During the appointment, your doctor will discuss your child’s symptoms and general health. He or she will conduct a thorough examination of the knee to determine the cause of the pain. This will include applying pressure to the tibial tubercle, which should be tender or painful for a child with Osgood-Schlatter disease. In addition, your doctor may also ask your child to walk, run, jump, or kneel to see if the movements bring on painful symptoms.
Your doctor may also order an x-ray image of your child’s knee to help confirm the diagnosis or rule out any other problems. An MRI scan is usually not necessary for the diagnosis of Osgood-Schlatter’s disease.
Osgood Schlatter disease treatment
Treatment for Osgood-Schlatter disease focuses on reducing pain and swelling. This typically requires limiting exercise activity until your child can enjoy activity without discomfort or significant pain afterwards. In some cases, rest from activity is required for several months, followed by a strength conditioning program. However, if your child does not have a large amount of pain or a limp, participation in sports may be safe to continue.
Your doctor may recommend additional treatment methods, including:
- Stretching exercises. Stretches for the front and back of the thigh (quadriceps and hamstring muscles) may help relieve pain and prevent the disease from returning.
- Non-steroidal anti-inflammatory medication. Drugs like ibuprofen and naproxen reduce pain and swelling.
Most symptoms will completely disappear when a child completes the adolescent growth spurt, around age 14 for girls and age 16 for boys. For this reason, surgery is rarely recommended. However, the prominence of the tibial tubercle will persist.
Physical therapy
A physical therapist can teach your child exercises to stretch the thigh’s quadriceps, which can help reduce the tension where the kneecap (patella) tendon attaches to the shinbone. A patellar tendon strap also can help relieve the tension. Strengthening exercises for the quadriceps and legs in general can help stabilize the knee joint.
Figure 3. Osgood Schlatter disease stretches (quadriceps stretch)
Home remedies
Your child should apply ice to the painful area. Ice can help prevent swelling and relieve pain. After applying ice, wrap your child’s knee with an elastic bandage and keep your child’s leg elevated.
A memory aid that may help remind you of these four basic treatment steps is the word “RICE”:
- R = Rest the knee from the painful activity. Limit time spent doing activities that aggravate the condition, such as kneeling, jumping and running.
- I = Ice the affected area for 20 minutes, 3 times a day. This can help with pain and swelling.
- C = Compress the painful area with an elastic bandage.
- E = Elevate the leg.
It might help your child to:
- Stretch leg muscles. Stretching the muscles on the front of the thigh (quadriceps), is especially important.
- Protect the knee. When your child is participating in sports, have him or her wear a pad over the affected knee where the knee can become irritated.
- Try a infrapatellar knee strap. A patellar tendon strap fits around the leg just below the kneecap. It can help to “tack down” the kneecap’s tendon during activities and distribute some of the force away from the shinbone.
- Cross-train. Suggest that your child switch to activities that don’t involve jumping or running, such as cycling or swimming, until symptoms subside.
Figure 5. Osgood Schlatter disease brace (infrapatellar knee strap)