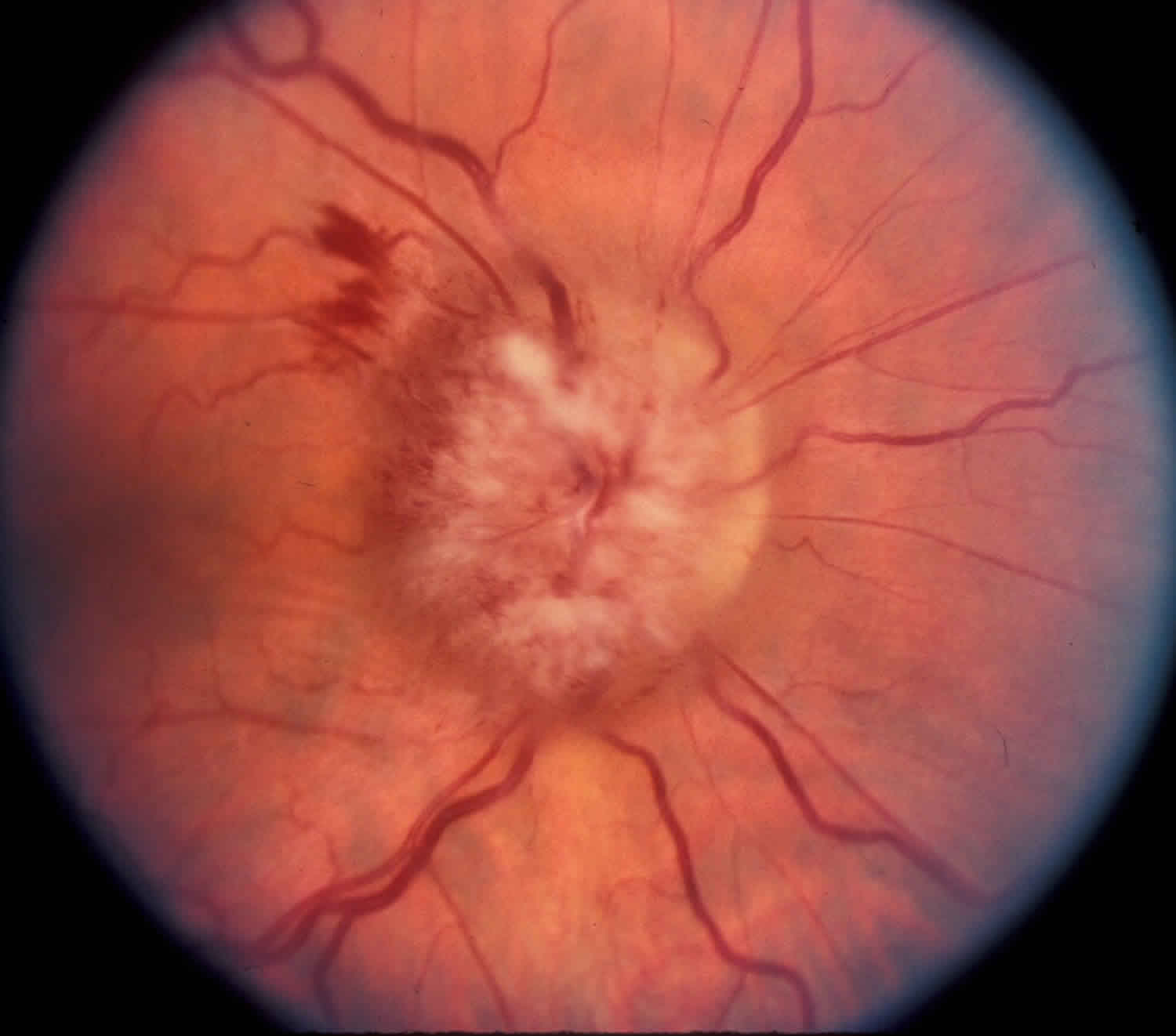
What is papilledema
Papilledema refers to swelling of the optic disc from increased intracranial pressure (ICP). Papilledema must be distinguished from optic disc swelling from other causes which is simply termed “optic disc edema”. Papilledema must also be distinguished from pseudo-papilledema such as optic disc drusen. Since the root cause of papilledema is increased intracranial pressure (ICP) this is an alarming sign which may be a early warning sign of such entities as brain tumor, CNS (central nervous system) inflammation, or idiopathic intracranial hypertension (pseudotumor cerebri) 1.
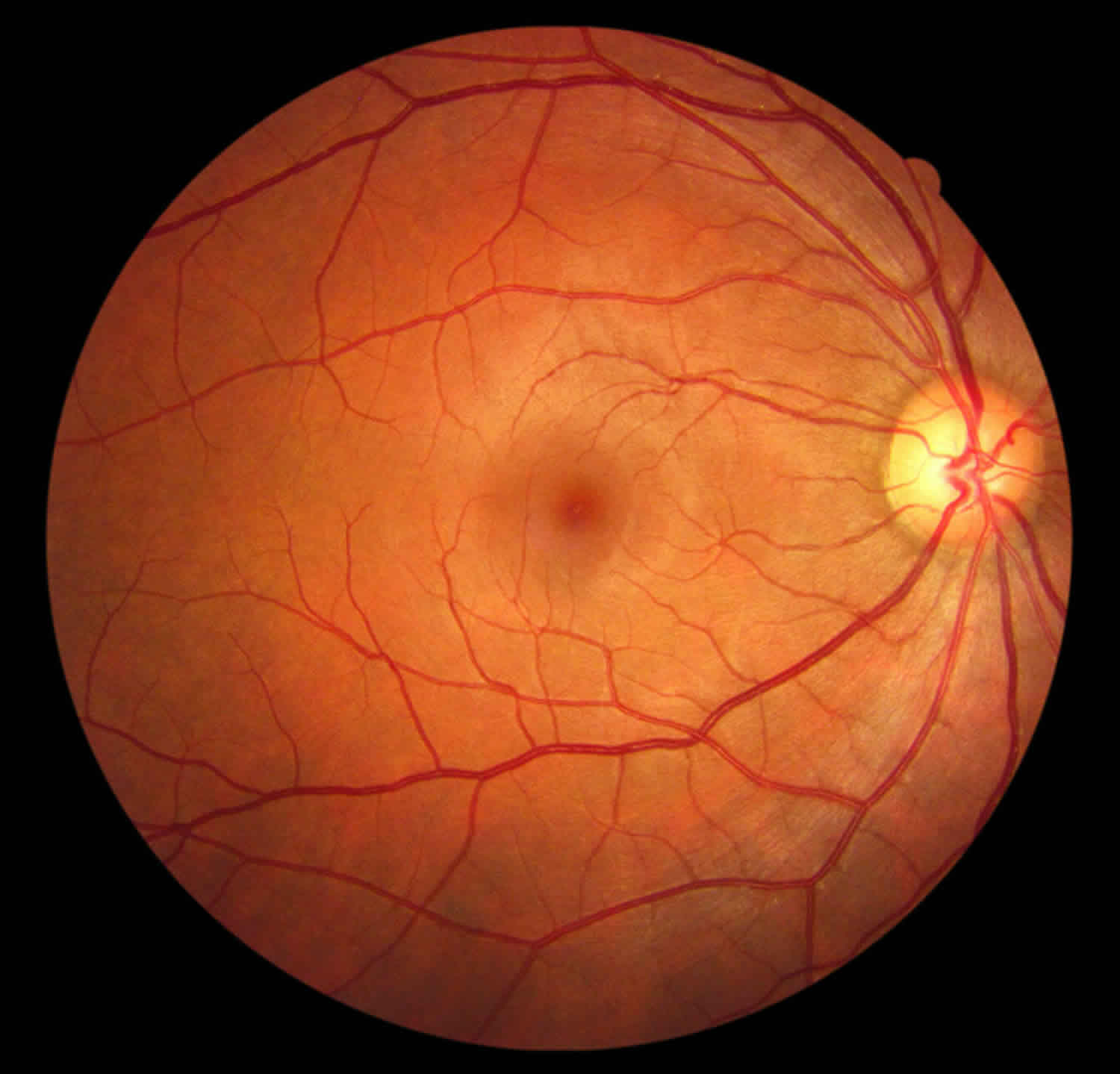
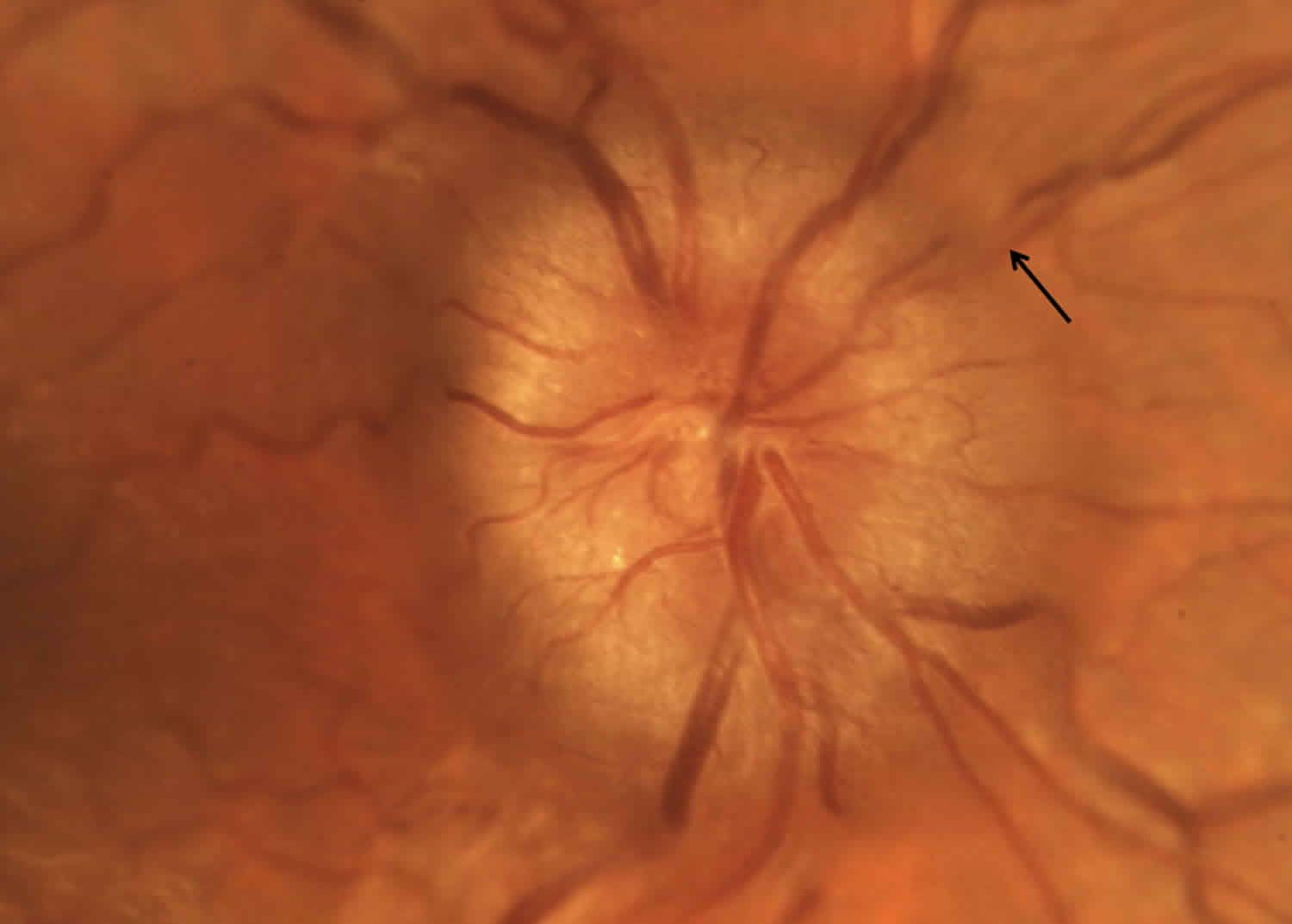
Figure 1. Normal retina (right eye)
Papilledema grading
Papilledema Grading System (Frisen Scale) 2
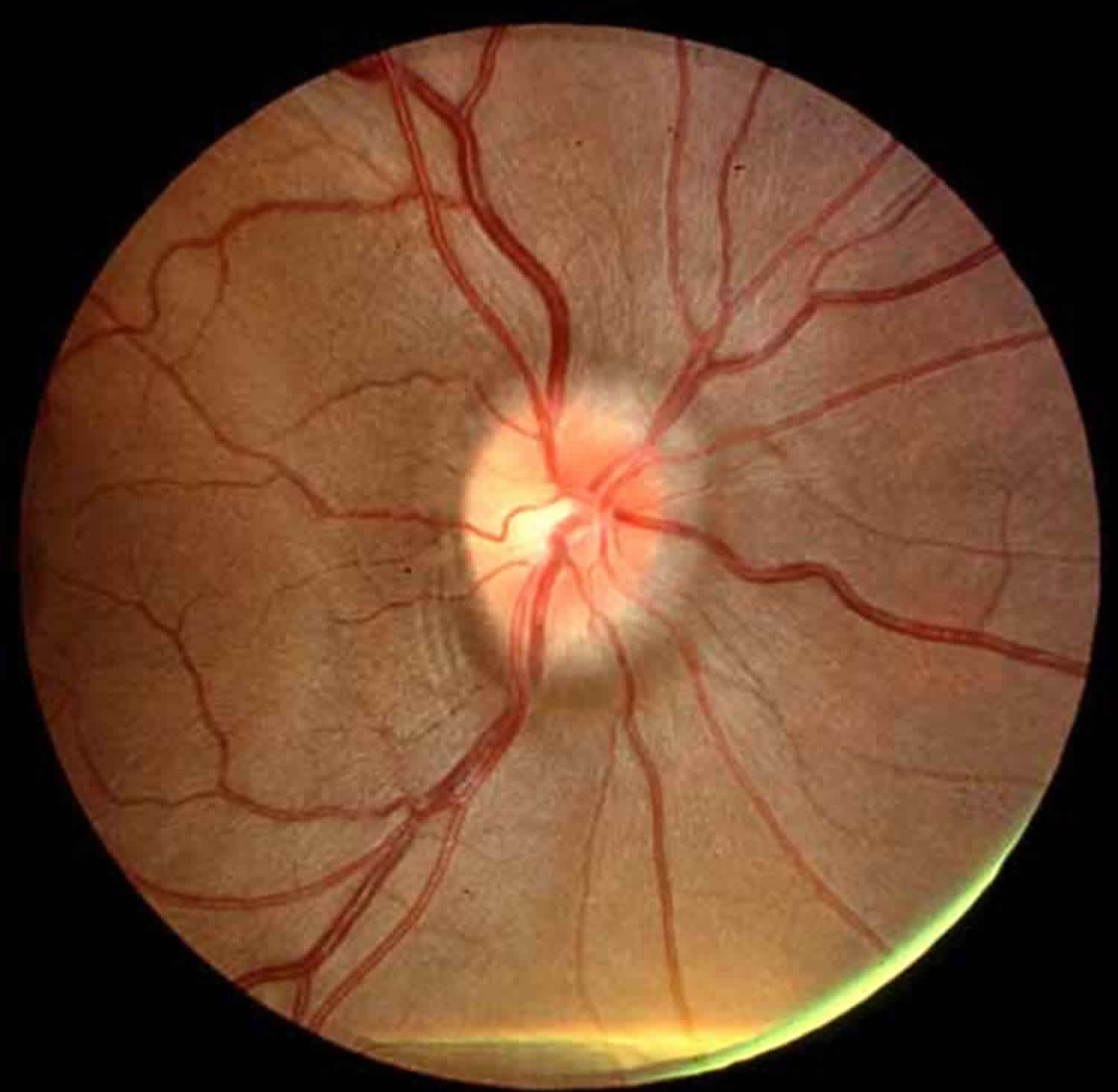
Papilledema Grade 1
Grade 1 papilledema is characterized by a C-shaped halo with a temporal gap.
Figure 2. Papilledema Grade 1
Papilledema Grade 2
Grade 2 papilledema, the halo becomes circumferential.
Figure 3. Papilledema Grade 2
Papilledema Grade 3
Grade 3 papilledema is characterized by loss of major vessels AS THEY LEAVE the disc (arrow).
Figure 4. Papilledema Grade 3
Papilledema Grade 4
Grade 4 papilledema is characterized by loss of major vessels on the optic disc.
Figure 5. Papilledema Grade 4
Papilledema Grade 5
Grade 5 papilledema has the criteria of grade 4 plus partial or total obscuration of all vessels of the optic disc.
Figure 6. Papilledema Grade 5
Papilledema stages
Papilledema Stage 0
Normal Optic Disc Blurring of nasal, superior and inferior poles in inverse proportion to disc diameter. Radial nerve fiber layer (NFL) without nerve fiber layer tortuosity.
Rare obscuration of a major blood vessel, usually on the upper pole.
Papilledema Stage 1
Very Early Papilledema Obscuration of the nasal border of the disc. No elevation of the disc borders. Disruption of the normal radial nerve fiber layer arrangement with grayish opacity accentuating nerve fiber layer bundles. Normal temporal disc margin. Subtle grayish halo with temporal gap (best seen with indirect ophthalmoscopy).
Concentric or radial retrochoroidal folds.
Papilledema Stage 2
Early Papilledema Obscuration of all borders. Elevation of the nasal border. Complete peripapillary halo.
Papilledema Stage 3
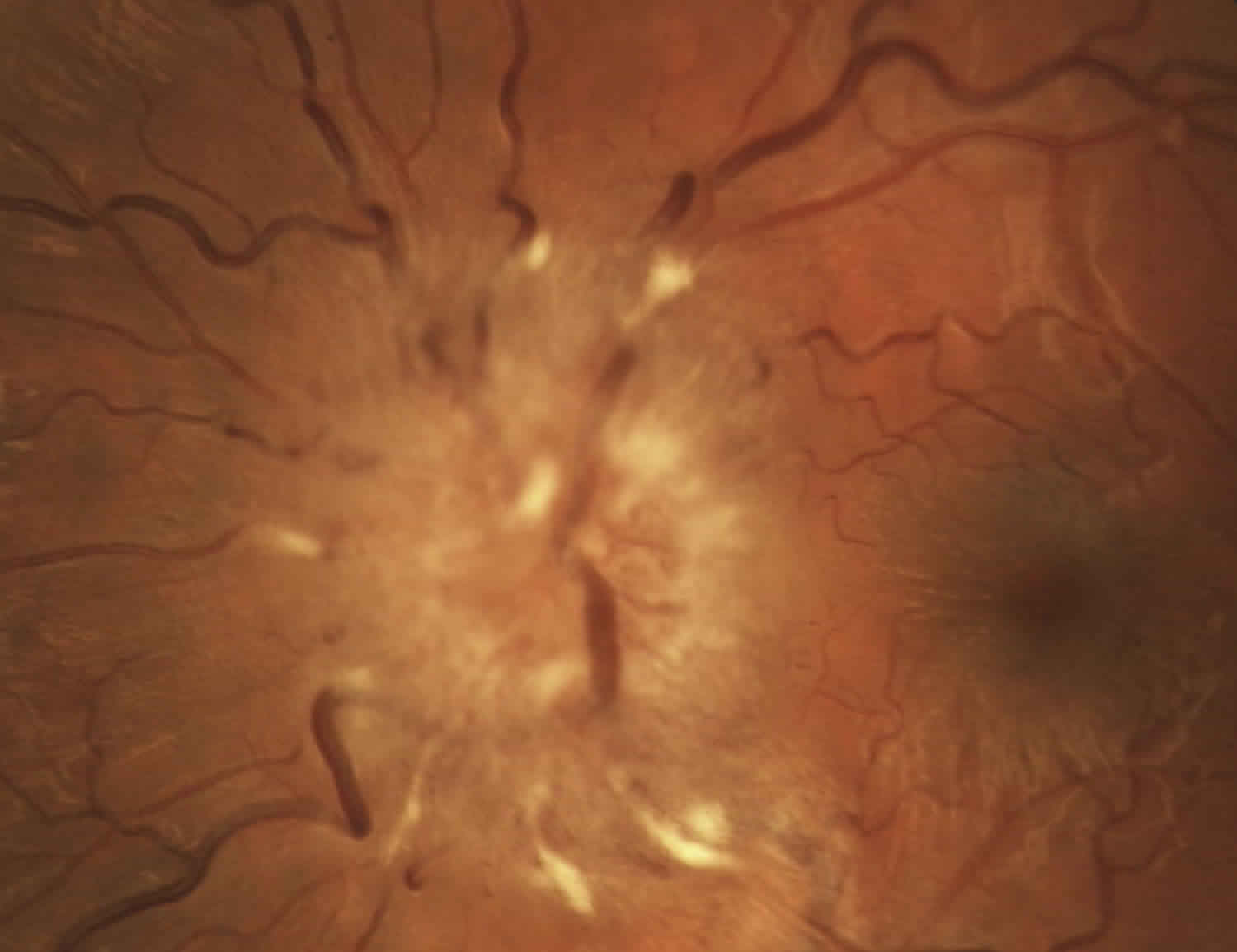
Moderate Papilledema Obscurations of all borders. Increased diameter of optic nerve head. Obscuration of one or more segments of major blood vessels leaving the disc. Peripapillary halo-irregular outer fringe with finger-like extensions.
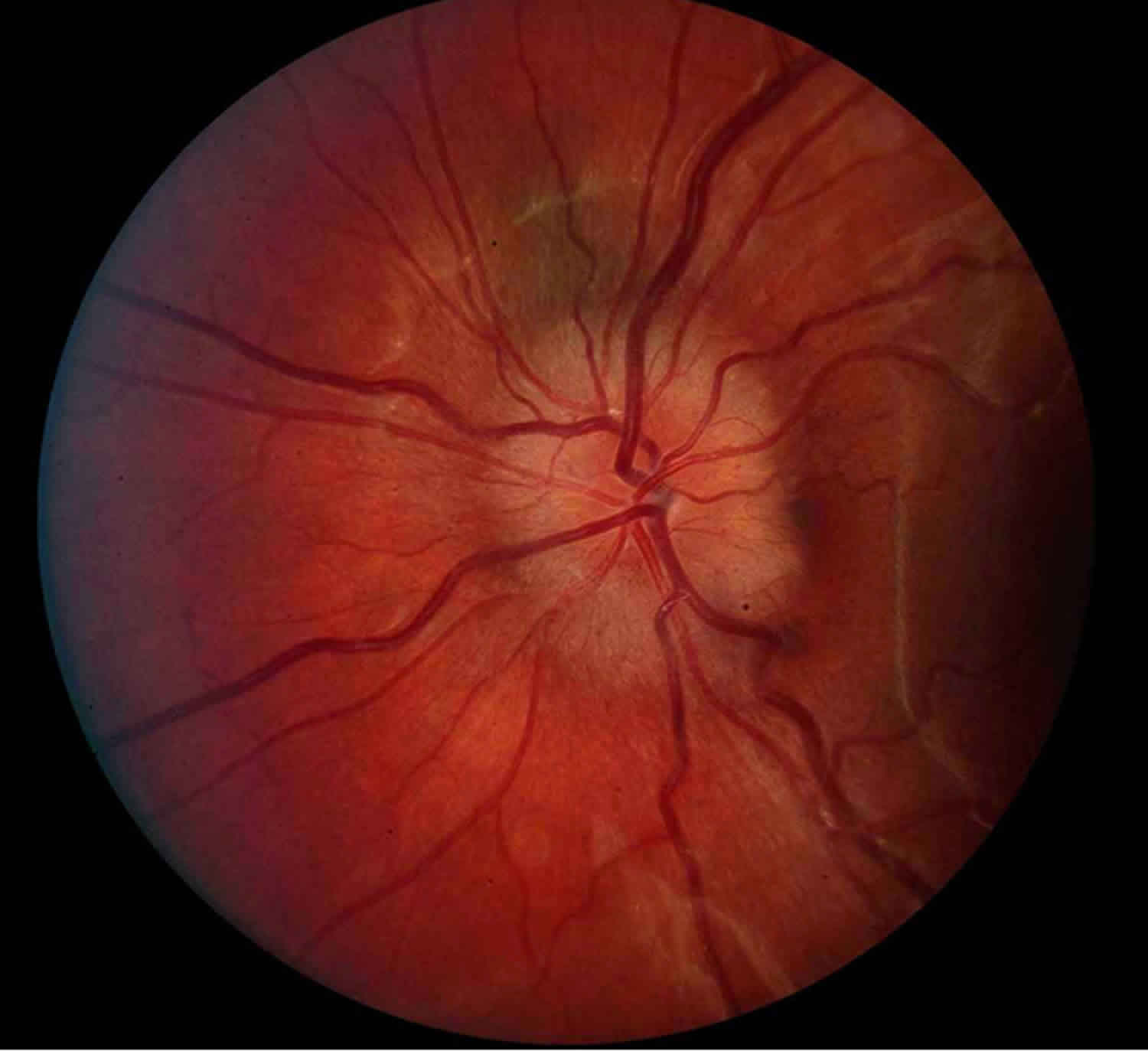
Papilledema Stage 4
Marked Papilledema Elevation of the entire nerve head. Obscuration of all borders. Peripapillary halo. Total obscuration on the disc of a segment of a major blood vessel.
Papilledema Stage 5
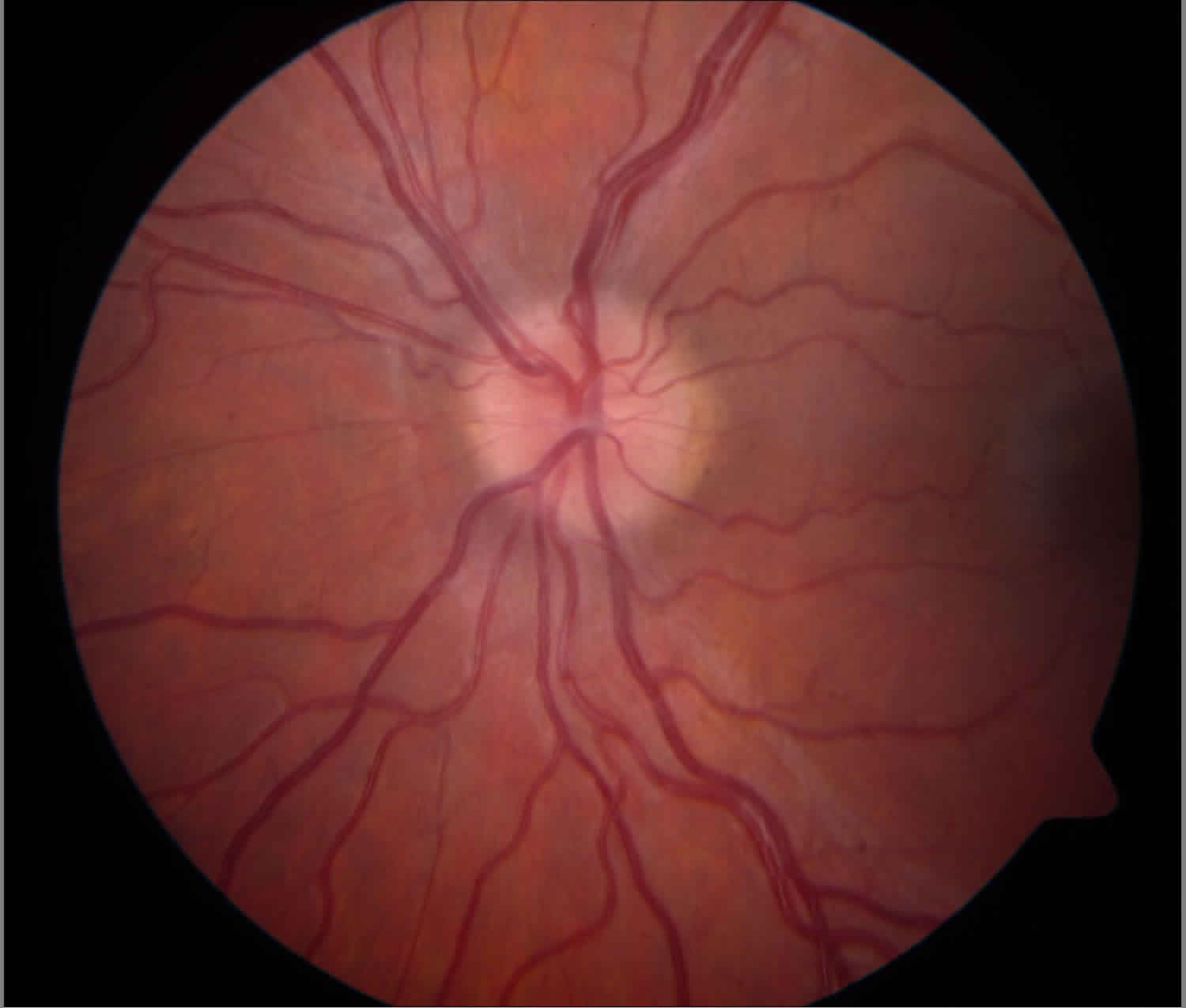
Severe Papilledema Dome-shaped protrusions representing anterior expansion of the optic nerve head. Peripapillary halo is narrow and smoothly demarcated.
Total obscuration of a segment of a major blood vessel may or may not be present. Obliteration of the optic cup.
Figure 7. Mild papilledema
Figure 8. Moderate papilledema
Figure 9. Severe papilledema
Figure 10. Severe papilledema resolved
Papilledema causes
Papilledema is due to increased intracranial pressure from any cause. Normal increased intracranial pressure is typically less than 250 mm water when measured with a manometer in the recumbent position. Papilledema results from orthograde axoplasmic flow stasis at the optic nerve head leading to edema of the nerve from the increased intracranial pressure pressing on the nerve behind the eye. Continued pressure can result in loss of axons and eventual optic atrophy. With optic atrophy there is little or no edema seen even with continuing increased intracranial pressure since there are no fibers to swell. Increased intracranial pressure can be caused by (1) a space occupying lesion such as a tumor or hemorrhage, by (2) decreased cerebrospinal fluid (CSF) drainage due to blockage (obstructive hydrocephalus) or decreased absorption (infection, hemmorhage, venous sinus thrombosis or venous outflow obstruction), by (3) Idiopathic Intracranial Hypertenion (also called pseudotumor cerebri), (4) rarely by increased CSF production such as from a choroid plexus tumor, and lastly by decreased skull volume (craniosynostosis). The time course for development of papilledema may be weeks if there is only a slow and mild rise in intracranial pressure, but severe and rapid changes in pressure can cause papilledema to present within a day.
Risk factors for papilledema
Risk factors for papilledema are those that raise intracranial pressure. This includes space occupying lesions such as tumor or subarrachnoid hemoorhage, decrease of absorption of cerebrospinal fluid, change in the dynamics of cerebrospinal flow through the ventricles (for example by obstruction of the 4th ventricle), or rarely by increase of flow of cerebrospinal fluid (CSF).
Papilledema symptoms
Early papilledema has few symptoms. Headache is common with increased intracranial pressure and often worse in the morning. Nausea and vomiting are noted with increased intracranial pressure, especially with an acute rise in pressure. This is made worse by straining, coughing or bending. Visual fields often demonstrate increased size of the blind spot. When papilledema is severe, the patient may note short periods lasting seconds of losing vision which are called transient visual obscurations. These are observed when raising to stand or changing position. Farsightedness (hypermetropia) may increase because of pressure from the dilated optic nerve sheath flattening the back of the eye. Increased intracranial pressure can lead to hearing vascular noises, whooshing sounds, or pulsatile tinnitus. Long standing papilledema may result in peripheral visual field loss as seen in idiopathic intracranial hypertension (pseudotumor cerebri). Increased intracranial pressure can also lead to cranial nerve palsies, usually an abducens palsy. It is thought that the long course of the 6th cranial nerve is compressed by the increased CSF pressure.
Papilledema diagnosis
Diagnostic procedures
- Fluorescein angiography can detect disc leakage. Autofluorescence can demonstrate drusen and B scan ultraound may also be helpful to find drusen.
- Stereo disc images obtained to document and follow disc status.
- Perimetry commonly shows enlarged blind spots. In severe chronic papilledema peripheral field loss may be seen.
- CNS imaging study (CT or MRI with contrast) to identify a central nervous system mass lesion.
- MR venography (MRV) should always be considered to look for venous sinus thrombosis.
- Lumbar puncture (after imaging demonstrates no risk for herniation) to document increased intracranial pressure and to look for neoplastic, infectious or inflammatory causes. At a minimum, opening pressure along with glucose, protein, cell count and differential, culture are obtained.
Fundoscopy noting disc swelling (usually bilateral unless one disc is atrophic) in the presence of increased intracranial pressure is the key to diagnosis. Other diagnostic tools include ultrasonography, fluroescein angiography, CT or MR imaging (MRI), When presented with the possibility of papilledema the first approach is imaging to rule out space occupying lesion. This is best done by MRI and an accompanying magnetic resonance venography (MRV) can help rule out a venous sinus thrombosis. Occasionally severe papilledema is noted on MRI as flattening of the sclera near the optic nerve and even a raised area at the disc head. A lumbar puncture with opening pressure and fluid sent for cytology and culture is done to confirm the diagnosis of increased intracranial pressure.
Disc appearance
If spontaneous venous pulsations are present this suggests that intracranial pressure is probably not high at this time, however the intracranial pressure may have been high before simply due to diurnal variations in intracranial pressure.
Early papilledema – disc hyperemia possibly with dilated disc capillaries. Nerve fiber layer opacification and swelling. Blurred disc margin(s). Venous pulsations are absent. More severe developed papilledema will have elevation of the disc and opacified nerve fiber layer obscuring disc vessels. There may be dilated veins, disc splinter hemorrhages, cotton wool spots, or hard exudates. With severe disc leakage a macular star may be seen, this is more prominent on the disc side of the macula. Later retinochroroidal folds called Paton’s lines may be present. With chronicity of papilledema funduscopy reveals all of the above plus the start of disc pallor along with decreasing disc swelling with the loss of axons. Sometimes optociliary shunts may be noted. In the wake of papilledema there may be retinal pigment epithelium (RPE) pigmentary changes around the disc, disc gliosis and residual chroidal folds.
Papilledema treatment
The primary cause of the increased intracranial pressure must be addressed. If a mass is present, primary therapy should be directed towards that. If medications (tetracyclines, vitamin A analogues, etc.) are felt to be causative they should be discontinued.
Medications are used to decrease intracranial pressure by helping increase CSF absorption or decreasing CSF production. Diuretics used include Acetalzolamide (diamox – a carbonic anhydrase inhibitor) and Lasix These are the mainstay of treatment in idiopathic intracranial hypertenion (pseudotumor cerebri) along with surgical interventions. Steroids can reduce inflammation if that is a component of the increased ICP and may help stabilize vision loss. Steroids (especially with change in dosage) have also been causative of increased ICP.
Weight reduction in idiopathic intracranial hypertenion (pseudotumor cerebri) weight loss (even 10-15% loss) in idiopathic intracranial hypertenion (pseudotumor cerebri) can lead to normalization of intracranial pressure.
Medical therapy
Carbonic anhydrase inhibitors (acetazolamide), lasix,
Surgery
If a mass is causative, it should be addressed.
Ventriculoperitoneal (VP) and lumboperitoneal (LP) shunts allow CSF fluid to drain and normalized ICP.
Optic nerve sheath fenestration- either unilateral or bilateral may be considered if vision is threatened. This will decompress the optic nerve but will usually not help with headache symptoms.
Surgical complications include shunt failure and closure or scarring of optic nerve fenestrations.
Papilledema prognosis
Chronic papilledema leads to axon loss with constriction of the visual field, loss of disc substance and in the end, loss of central acuity.Patients (especially those with idiopathic intracranial hypertenion) need to be followed to prevent vision loss.
References- Deshmukh S, Das D, Bhattacharjee H, Kuri GC, Magdalene D, Gupta K, Multani PK, Paulbuddhe V, Dhar S. Profile of brain tumors having ocular manifestations in a Tertiary Eye Care Institute: A retrospective study. TNOA J Ophthalmic Sci Res [serial online] 2018 [cited 2018 Sep 2];56:71-5. Available from: http://www.tnoajosr.com/text.asp?2018/56/2/71/238494
- Reference: Frisen L. Swelling of the optic nerve head: A staging scheme. J Neurol Neurosurg Psychiatry 1982; 45:13-18