What is paraphimosis
Paraphimosis occurs when the foreskin of an uncircumcised male can’t be returned to its normal position after being retracted. Paraphimosis can cause painful swelling of the penis and impaired blood flow. You should go to your local emergency room if this occurs. Paraphimosis requires emergency medical treatment to avoid serious complications, such as increased pain, swelling and restricted blood flow to the penis. A physical exam confirms the diagnosis. Typical paraphimosis symptoms include erythema, pain, and swelling of foreskin and glans due to the constricting ring of the phimotic foreskin. Your health care provider will usually find a “doughnut” around the shaft near the head of the penis (glans).
It is still possible to develop paraphimosis in a patient who has previously been circumcised. This can be due to the patient believing he was circumcised when he was not or excessive remaining foreskin despite the circumcision.
Paraphimosis treatment from home
Pressing on the head of the penis while pushing the foreskin forward may reduce the swelling. If this fails, prompt surgical circumcision or other surgery to relieve swelling will be needed.
It may be possible to reduce the pain and inflammation by applying a local anesthetic gel to the penis and pressing on the glans while pushing the foreskin forward.
In difficult cases, it may be necessary to make a small slit in the foreskin to help relieve the pressure.
In severe cases of paraphimosis, circumcision may be recommended. In very severe cases, a lack of blood flow to the penis can cause tissue death (gangrene) and surgical removal of the penis may be necessary.
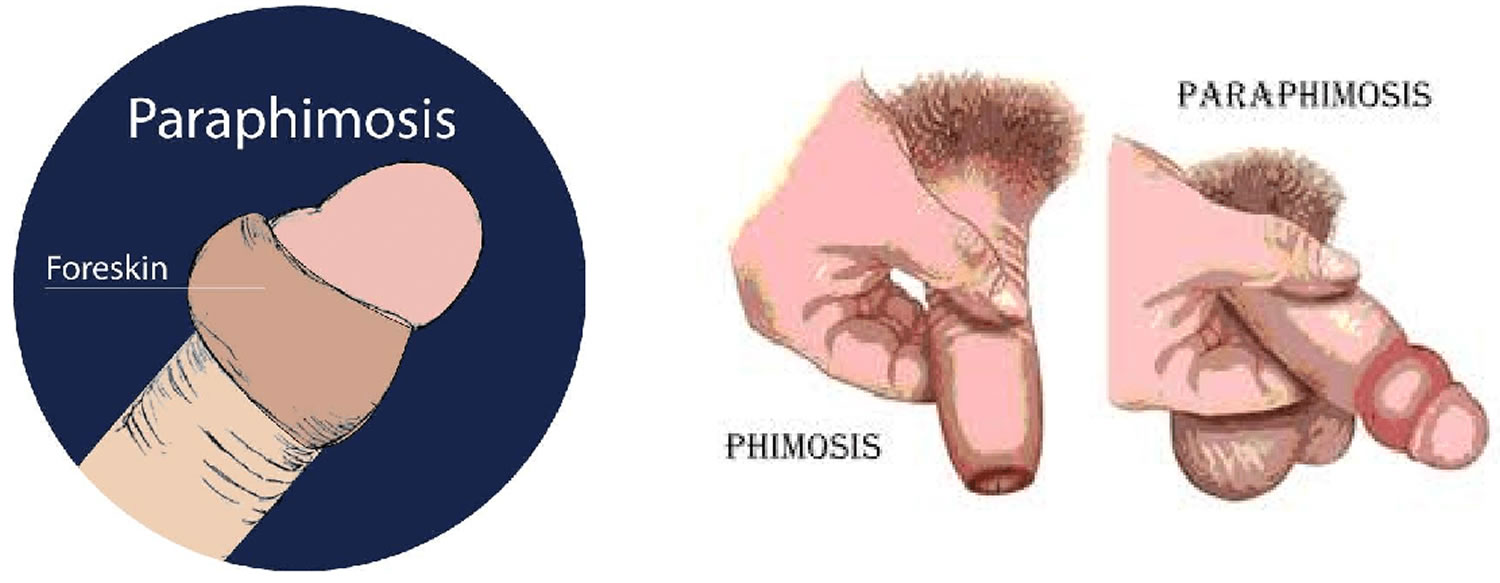
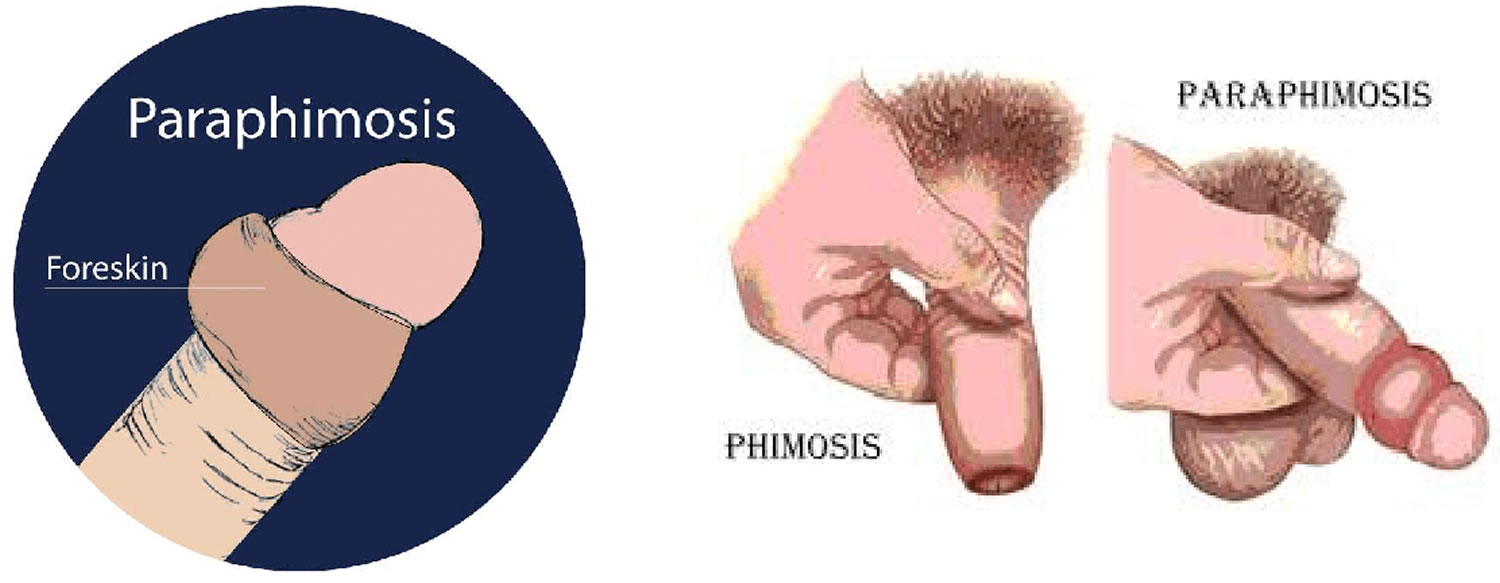
Figure 1. Paraphimosis
Normal foreskin development
Most uncircumcised baby boys have a foreskin that won’t pull back (retract) because it’s still attached to the glans.
This is perfectly normal for about the first 2 to 6 years. By around the age of 2, the foreskin should start to separate naturally from the glans.
The foreskin of some boys can take longer to separate, but this doesn’t mean there’s a problem – it’ll just detach at a later stage.
Never try to force your child’s foreskin back before it’s ready because it may be painful and damage the foreskin.
Penis hygiene
It’s important to clean your penis regularly to avoid problems developing.
You should:
- gently wash your penis with warm water each day while having a bath or shower
- gently pull back your foreskin (if you have one) and wash underneath; don’t pull back the foreskin of a baby or young boy because it could be painful and cause harm
- use a mild or non-perfumed soap (if you choose to use soap) to reduce the risk of skin irritation
- avoid using talc and deodorants on your penis as they may cause irritation
Circumcised men should also regularly clean their penis with warm water and a mild soap (if you choose to use soap).
Paraphimosis vs Phimosis
Phimosis is a condition where the foreskin is too tight to be pulled back over the head of the penis (glans). Phimosis is normal in babies and toddlers, but in older children it may be the result of a skin condition that has caused scarring. Phimosis isn’t usually a problem unless it causes symptoms.
Paraphimosis is where the foreskin can’t be returned to its original position after being retracted and the foreskin becomes trapped behind the corona of the glans penis which can lead to strangulation of the glans as well as painful vascular compromise, distal venous engorgement, edema, and even necrosis.
Immediate treatment is needed in cases where phimosis causes problems such as difficulty urinating.
Phimosis isn’t usually a problem unless it causes symptoms such as redness, soreness or swelling.
When phimosis is a problem
If your child’s glans is sore and inflamed, they may have balanitis (inflammation of the head of the penis).
There may also be a thick discharge underneath the foreskin. If both the glans and foreskin are inflamed, it’s known as balanoposthitis.
Take your child to see your doctor if they have these type of symptoms. Your doctor will be able to recommend appropriate treatment.
Most cases of balanitis can be easily managed using a combination of good hygiene, creams or ointments, and avoiding substances that irritate the penis.
Balanoposthitis can also sometimes be treated by following simple hygiene measures, such as keeping the penis clean by regularly washing it with water and a mild soap or moisturiser.
Urine can irritate the glans if it’s retained for long periods under the foreskin, so if possible you should withdraw the foreskin to wash the glans.
If balanoposthitis is caused by a fungal or bacterial infection, an antifungal cream or a course of antibiotics may be needed.
In adults, phimosis can occasionally be associated with sexually transmitted infections (STIs).
Phimosis can also be caused by a number of different skin conditions, including:
- Eczema – a long-term condition that causes the skin to become itchy, red, dry and cracked
- Psoriasis – a skin condition that causes red, flaky, crusty patches of skin covered with silvery scales
- Lichen planus – a non-infectious itchy rash that can affect many areas of the body
- Lichen sclerosus – a scarring condition of the foreskin (and sometimes glans) that’s probably caused by urinary irritation in susceptible men and boys
Topical steroids (a cream, gel or ointment that contains corticosteroids) are sometimes prescribed to treat a tight foreskin. They can help soften the skin of the foreskin, making it easier to retract.
Phimosis can cause pain, skin splitting, or a lack of sensation during sex. Using a condom and lubricants while having sex may make your penis more comfortable.
When surgery may be needed
Surgery may be needed if a child or adult has severe or persistent balanitis or balanoposthitis that causes their foreskin to be painfully tight.
Circumcision (surgically removing part or all of the foreskin) may be considered if other treatments have failed, but it carries risks such as bleeding and infection.
This means it’s usually only recommended as a last resort, although it can sometimes be the best and only treatment option.
Alternatively, surgery to release the adhesions (areas where the foreskin is stuck to the glans) may be possible. This will preserve the foreskin but may not always prevent the problem recurring.
Paraphimosis causes
Causes of paraphimosis include:
- Injury to the area.
- Failure to return the foreskin to its normal location after urination, washing, placement of a urinary catheter, a procedure such as a cystoscopy. This is more common in hospitals and nursing homes.
- Infection, which may be due to not washing the area well.
- Other, less common causes include penile coital trauma and self-inflicted injuries.
Men who have not been circumcised and those who may not have been correctly circumcised are at risk.
Paraphimosis occurs most often in boys and older men.
In uncircumcised children, four months to 12 years old, with foreskin problems, paraphimosis (0.2%) is less common than other penile disorders such as balanitis (5.9%), irritation (3.6%), penile adhesions (1.5%), or phimosis (2.6%) 1.
In adults, paraphimosis most commonly is found in adolescents. It will occur in about 1% of all adult males over 16 years of age.
Paraphimosis prevention
Returning the foreskin to its normal position after pulling it back may help prevent this condition.
Circumcision, when done correctly, prevents this condition.
Paraphimosis symptoms
The foreskin is pulled back (retracted) behind the rounded tip of the penis (glans) and stays there. The retracted foreskin and glans become swollen. This makes it difficult to return the foreskin to its extended position.
Paraphimosis symptoms include:
- Inability to pull the retracted foreskin over the head of the penis
- Painful swelling at the end of the penis
- Pain in the penis
Paraphimosis possible complications
If paraphimosis is left untreated, it can disrupt blood flow to the tip of the penis. In extreme (and rare) cases, this may lead to:
- Damage to the penis tip
- Gangrene
- Loss of the penis tip
Paraphimosis treatment
Mild, uncomplicated paraphimosis may be reduced manually, usually without the need for sedation or analgesia. More difficult or complicated cases may require local anesthesia with a dorsal penile block, systemic analgesia, or procedural sedation.
Several methods of reduction are available and can be classified into manual reduction or surgical repair.
Paraphimosis manual reduction
Manual, non-surgical, reduction of the paraphimosis can be done with or without compression methods, by osmotic agents, and using puncture-aspiration techniques.
Manual reduction of paraphimosis can often be facilitated by simple compression of the glans and the swollen, edematous foreskin for several minutes before attempting the reduction. This allows the edematous swelling of the retracted foreskin to diminish before attempting repositioning of the foreskin to its usual position. One simple method involves manually compressing the edematous foreskin while pulling slowly upward on the phallus.
Manual reduction can also be attempted by placing both thumbs over the glans with both index and long fingers surrounding the trapped foreskin. Then slow, steady pressure is applied to advance the phimotic portion of the foreskin outwards slowly, back over the glans. This can be facilitated with a little lubricant. Excessive lubricant should be avoided as it may make the skin too slippery for reliable grasping.
Another compression technique involves tightly wrapping the swollen portion of the penis from the glans towards the base with a 1-inch or 2-inch elastic bandage. A gauze pad should be applied first around the edematous foreskin. The compression bandage can remain for 10 to 20 minutes to minimize the edema. Then apply one of the manual reduction methods described above. This is often a preferred technique as the elastic wrap can be placed by nursing staff while you are traveling to the patient’s location.
Ice packs or surgical gloves filled with ice and applied to edematous areas have been described as possibly being useful in conjunction with other methods to aid in the reduction of the paraphimotic swelling. However, since the main issue in paraphimosis is distal penile vascular compromise from a constricting fibrous band of the phimotic foreskin, many experts recommend against using ice in these situations as it may further compromise arterial inflow to the possibly ischemic portion of the penis.
Another possible compressive treatment method involves cutting the thumb from a surgical glove to make a “sleeve” and emptying a tube of EMLA cream (2.5% lidocaine and 2.5% prilocaine) or similar into the sleeve. This is then placed over the penis and left for approximately 30 minutes. This allows for local anesthesia and softening of affected skin to aid in foreskin reduction. However, while it does provide some analgesic relief, it may make the skin a little more slippery and harder to manipulate.
Reducing the penile edema from paraphimosis can also be achieved by the injection of hyaluronidase directly into the edematous foreskin. This has been effective, particularly in children and infants, in resolving the edema which then allows for easier manual reduction of the paraphimosis. The hyaluronidase increases the diffusion of trapped fluid within the tissue planes of the malpositioned foreskin which reduces the swelling and edema.
Osmotic methods involve the application of substances with a high solute concentration on the external skin surfaces of the edematous tissue. This would tend to draw water along an osmotic gradient and thereby reduce the edema. For example, a generous topical application of granulated sugar to the affected glans and foreskin has been shown to be effective in aiding in the reduction of the edema from paraphimosis.
Gauze soaked in 20% mannitol solution has also been used as an osmotic agent to reduce the edema from paraphimosis. The gauze is left in place for 30 to 45 minutes and has been reported to completely eradicate the troublesome edema allowing for easy resolution of the paraphimosis with manual techniques as described above. This technique is relatively painless and is well suited for children.
In many cases, no additional local anesthetic or analgesia is needed, but if the paraphimosis is long-standing, extremely painful, or severe, then a formal penile anesthetic block can be used. A dorsal penile block is performed by using a 25-gauge or 27-gauge needle, infiltrating approximately 2.5 mL of 1% lidocaine without epinephrine into the base of the penis at the junction of the penis and suprapubic skin at the 10 o’clock position, off the midline to avoid the superficial dorsal vein. Another 2.5 mL is injected at the 2 o’clock position. Inject the lidocaine just deep to Buck’s fascia, approximately 3 mm to 5 mm beneath the skin, ensuring negative aspiration of blood before injecting. Ultrasound guidance has been shown to be effective in helping to identify landmarks for this procedure.
Puncture and aspiration methods
Puncture and aspiration methods (Dundee technique) are more invasive and should be reserved for cases refractory to other less-invasive techniques 2. The puncture technique involves puncturing the edematous foreskin several times with a hypodermic needle followed by manual expression of edematous fluid through the puncture holes. Experienced emergency practitioners can consider penile corporal aspiration of blood.
Surgical treatment
Surgical treatment of the paraphimosis will be required if the previously described manual reduction methods are unsuccessful. Prepare the penis and prepuce with a povidone-iodine or similar antiseptic solution. This can be achieved after the previously-described penile block. One method involves applying two straight hemostats to grab the dorsum of the constricting foreskin at the 12 o’clock position. This is followed by making a 1 cm to 2 cm longitudinal incision of the constricting band of edematous foreskin between the hemostats, which allows for passage over the glans. After reduction, the incised foreskin is not reapproximated, but the edges are oversown with a 3-0 or 4-0 absorbable suture. This will leave the phimotic portion of the foreskin widely separate and open to prevent recurrences.
Paraphimosis prognosis
After successful manual reduction, the foreskin should carefully be cleaned. Any superficial abrasions or tears to the foreskin should be treated with a topical antibiotic ointment such as bacitracin. Patients should be instructed to avoid retracting the foreskin for one week and avoid any offending activities that contributed to the paraphimosis.
Reducing the paraphimosis successfully is insufficient long-term therapy. All such patients should be evaluated for further treatment involving a dorsal slit or circumcision procedure to definitively deal with the tightened foreskin and permanently prevent any recurrences of the paraphimosis.
The outcome is likely to be excellent if the condition is diagnosed and treated quickly.
References- Bragg BN, Leslie SW. Paraphimosis. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459233
- Reynard JM, Barua JM. Reduction of paraphimosis the simple way – the Dundee technique. BJU Int 1999;83(7):859-860.