What is peritonitis
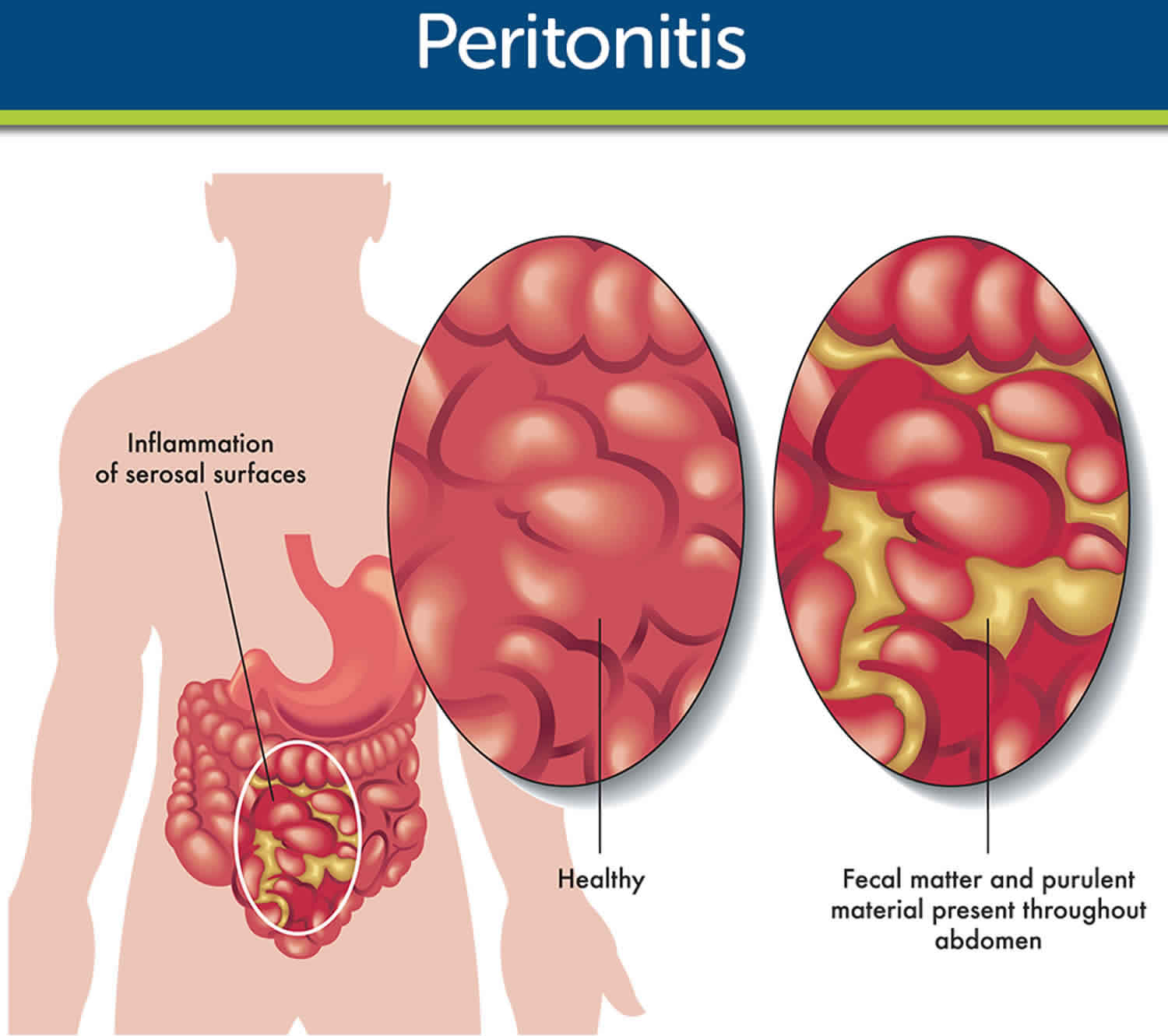
Peritonitis is an infection of the inner lining of the tummy (peritoneum), the serous membrane lining the abdominal cavity 1. Left untreated acute bacterial peritonitis can become life-threatening. The lining of the tummy (peritoneum) covers internal organs like the kidneys, liver and bowel. If the lining becomes infected the internal organs it covers can also be damaged. Peritonitis can result from any rupture (perforation) in your abdomen, or as a complication of other medical conditions. Peritonitis may result from a burst appendix or trauma-related abdominal injury.
Rarely if bacteria gets into peritoneal dialysis equipment used to treat people with kidney failure, this can cause peritonitis. If you’re receiving peritoneal dialysis therapy, you can help prevent peritonitis by following good hygiene before, during and after dialysis.
Peritonitis requires prompt medical attention to fight the infection and, if necessary, to treat any underlying medical conditions. Treatment of peritonitis usually involves antibiotics and, in some cases, surgery. Left untreated, peritonitis can lead to severe, potentially life-threatening infection throughout your body.
Peritonitis can be life-threatening if it’s not treated promptly. See your doctor immediately if you have severe pain or tenderness of your abdomen, abdominal bloating, or a feeling of fullness associated with:
- Fever
- Nausea and vomiting
- Low urine output
- Thirst
- Inability to pass stool or gas
If you’re receiving peritoneal dialysis, contact your health care provider immediately if your dialysis fluid is cloudy, if it contains white flecks, or strands or clumps (fibrin), or if it has an unusual odor, especially if the area around your tube (catheter) is red or painful.
Get an urgent doctor appointment or go to emergency room if you have:
- Sudden tummy pain that gets worse when touched or you move
- A very high temperature (you feel hot and shivery)
- Rapid heartbeat (your heart is beating more quickly than normal)
- Not been able to pee or are peeing much less than normal
You might also have:
- Lack of appetite and are feeling or being sick
- A swollen tummy
Serious complications like sepsis can happen if the infection spreads.
Spontaneous bacterial peritonitis
Spontaneous bacterial peritonitis is a term used to describe acute infection of ascites, an abnormal accumulation of fluid in the abdomen, without an obvious or identifiable source of infection 2.
Spontaneous bacterial peritonitis is most commonly (75%) caused by gram-negative aerobic organisms, with Klebsiella pneumonia accounting for 50% of these. Gram-positive aerobic organisms are responsible for the remainder of cases; the most common of these are Streptococcus pneumoniae or Viridans group streptococci 3.
The ascitic fluid typically has a high oxygen tension. Therefore anaerobic organisms are not commonly seen 2. In the majority of cases of spontaneous bacterial peritonitis, only one infecting organism is involved (92%), though a small number of cases have been reported as polymicrobial 2.
Typically, patients who experience spontaneous bacterial peritonitis have a chronic liver disease with a Child-Pugh classification, which assesses the prognosis of liver disease, of C. This ranking involves a high to a maximum score of 10 to 15 points (on the Child-Pugh scale), and measures 1-year patient survival at 45% and 2-year survival at 35%. Decompensated cirrhotic patients are those at highest risk of developing spontaneous bacterial peritonitis. Infecting organisms typically originate from the intestinal lumen, from where they pass via translocation to mesenteric lymph nodes.
Additional risk factors for spontaneous bacterial peritonitis include a previous history of spontaneous bacterial peritonitis, low complement levels, and reduced hepatic synthesis of proteins with (1) an associated prolonged prothrombin time (PT) time and reduced protein levels in ascitic fluid (less than 1 g/dL), and (2) long-term proton pump inhibitor therapy such as increased gastric pH with proton pump inhibitor use, which promotes gut bacterial growth and translocation.
Though in adults, spontaneous bacterial peritonitis is typically seen in patients with abdominal ascites, most children with spontaneous bacterial peritonitis do not have ascites. The reason for this has not yet been elucidated 4.
Spontaneous bacterial peritonitis can occur in adults and children. In children, it most commonly occurs in neonates and those around five years of age. It is most common in patients with cirrhosis, though it can occur as a complication of any disease that results in accumulation of ascitic fluid, such as liver disease, Budd-Chiari syndrome, congestive heart failure, systemic lupus erythematosus, renal failure, or cancers, and has a poor prognosis. Approximately 10% to 25% of patients with ascites will develop spontaneous bacterial peritonitis, and the condition is associated with a 20% in-hospital rate of mortality.
Patients with a prior incidence of spontaneous bacterial peritonitis are more likely to encounter a subsequent infection with a drug-resistant organism. Additionally, the risk of developing spontaneous bacterial peritonitis increases with age, use of proton-pump inhibitors (PPIs), and when undergoing spontaneous bacterial peritonitis prophylaxis such as selective intestinal decontamination 5.
Spontaneous bacterial peritonitis causes
The majority of the isolated organisms in spontaneous bacterial peritonitis (90%) are gram-negative enteric organisms (e.g., Escherichia coli or Klebsiella pneumoniae) which suggest that the main source of contamination is the gastrointestinal (GI) tract. Enterotoxin is also frequently isolated from ascitic fluid, further supporting the theory that bacteria involved in spontaneous bacterial peritonitis migrate transmurally from the intestinal lumen (i.e., bacterial translocation).
An alternatively proposed mechanism of contamination involves hematogenous spread, from a distant source, such as a urinary tract infection, in individuals predisposed to the disease by a weakened immune system (i.e., immunocompromised). Patients with cirrhosis typically have an elevated level of bacterial overgrowth in the gastrointestinal tract, largely due to a prolonged intestinal transit time. This, coupled with reduced protein production by a cirrhotic liver (e.g., low complement levels in both the serum and ascites) and poor phagocytic and reticuloendothelial system function, results in a decreased ability to clear microorganisms from the system, thereby further contributing to bacterial overgrowth, migration, and expansion within the ascites fluid 6.
Spontaneous bacterial peritonitis diagnosis
One should have a high index of suspicion for spontaneous bacterial peritonitis in all patients presenting with ascites, and this is especially true if the patient has an acute history of clinical deterioration. The majority of patients with spontaneous bacterial peritonitis will present with fever, chills, and abdominal pain, although some patients may be asymptomatic and spontaneous bacterial peritonitis is an incidental finding. Fever is the most common symptom encountered in patients with spontaneous bacterial peritonitis, which is a particularly useful clinical symptom as patients with cirrhosis are typically hypothermic. Additional signs and symptoms include diarrhea, paralytic ileus, new-onset or worsening encephalopathy (e.g., altered mental status) without any other identifiable cause, new-onset or worsening renal failure, or presence of ascites that does not improve with use of diuretic medications.
On physical examination, most patients will have a tender abdomen, although patient response can vary from mild discomfort to the presence of guarding and rebound tenderness.
There is a short window of opportunity for treating spontaneous bacterial peritonitis before it progresses to septic shock or multisystem organ failure; therefore, rapid assessment and diagnosis are critical (i.e., treatment is much more successful if antibiotics are started before the development of shock).[2][8][9]
Peritoneal fluid analysis (e.g., cell count, differential, culture, lactate level, pH) should be performed in all patients with suspected spontaneous bacterial peritonitis. This may be achieved either by diagnostic paracentesis or withdrawal of fluid through a peritoneal catheter, which is sometimes present in patients undergoing peritoneal dialysis. In patients with only a small amount of ascites, ultrasonography should be employed to help guide the paracentesis procedure.
Additionally, blood and urine cultures should be obtained before initiation of antibiotic therapy as the results of these may help point towards a source of infection and guide antibiotic therapy.
The most accurate predictor of spontaneous bacterial peritonitis is a polymorphonuclear leukocyte (granulocytes such as neutrophils, basophils, and eosinophils) count of greater than 500 cells/uL in a sample of ascitic fluid with a sensitivity and specificity of 86% and 98%, respectively. At a polymorphonuclear leukocyte count of greater than 250cells/uL, sensitivity increases to 93% while specificity declines to 94%. This is the widely accepted number of polymorphonuclear leukocytes needed to form a presumptive diagnosis of spontaneous bacterial peritonitis, before beginning empiric antibiotic therapy.
If the perforation is suspected within the abdomen, imaging is warranted, and computed tomography (CT) should be strongly considered, as it is more sensitive for detecting smaller perforations than a plain radiograph.
More recently proposed tests for spontaneous bacterial peritonitis include a rapid reagent strip that evaluates for the presence of leukocyte esterase in ascitic fluid, which is shown to have a sensitivity of 100% in the diagnosis of spontaneous bacterial peritonitis when compared to manual polymorphonuclear leukocyte counting. Though this may prove to be a much more efficient method of spontaneous bacterial peritonitis diagnosis than those previously used, the test still needs to undergo a large-scale comprehensive evaluation.
Spontaneous bacterial peritonitis treatment
Empiric antibiotic therapy, such as intravenous third-generation cephalosporin, should be started in all patients with suspected spontaneous bacterial peritonitis and a polymorphonuclear leukocyte count of greater than 250 cell/uL on ascitic fluid analysis. Exceptions to this rule include patients with recent beta-lactam antibiotic exposure or diagnosis of spontaneous bacterial peritonitis in a nosocomial setting. Antibiotics should be chosen based on results of susceptibility testing in these cases 7.
Patients with an ascitic fluid polymorphonuclear leukocyte count of greater than 500cells/uL should be admitted and treated with empiric antibiotic therapy as soon as possible and the antibiotics adjusted later based on the results of susceptibility testing. A follow-up analysis of ascitic fluid to assess polymorphonuclear leukocyte count should be performed to ensure the patient is receiving adequate and appropriate antibiotic therapy. This is important, as lack of improvement after 48 hours of therapy may indicate an underlying perforation or abscess formation, such as secondary bacterial peritonitis, that may require surgery. In general, ascitic fluid polymorphonuclear leukocyte count should be reduced by at least 25% after 48 hours of antibiotic therapy.
Some cirrhotic patients with spontaneous bacterial peritonitis and either a serum creatinine greater than 1mg/dL, a blood urea nitrogen (BUN) greater than 30mg/dL, or total bilirubin greater than 4mg/dL should be given adjunctive (i.e., in addition to antibiotics) albumin intravenously. This has been shown to reduce both in-hospital mortality and renal damage when compared to the use of antibiotic therapy alone.
Certain high-risk patients may benefit from outpatient antibiotic prophylactic therapy including norfloxacin, ciprofloxacin, or trimethoprim-sulfamethoxazole. These individuals have had a prior episode of spontaneous bacterial peritonitis, or ascitic fluid with either a low protein count (< 1g/dL) or is associated with a GI bleed.
Spontaneous bacterial peritonitis prognosis
Spontaneous bacterial peritonitis carries a mortality rate of 30-70% in patients with end-stage liver and kidney disease 2. The mortality rates are lower in children with nephrosis. Recently the mortality rates have shown a slight decrease because of earlier diagnosis and advances in treatment. For the patient who develops septic shock secondary to bacterial peritonitis, the mortality increases each hour until antibiotic therapy is started 8.
Peritonitis causes
Peritonitis is inflammation of the peritoneum — a silk-like membrane that lines your inner abdominal wall and covers the organs within your abdomen — that is usually due to a bacterial or fungal infection. Infection of the peritoneum can happen for a variety of reasons. In most cases, the cause is a rupture (perforation) within the abdominal wall. Though it’s rare, the condition can develop without an abdominal rupture. This type of peritonitis is called spontaneous peritonitis.
Peritonitis most often happens because of things like:
- a burst stomach ulcer
- a burst appendix
- digestive problems, such as Crohn’s disease or diverticulitis
- pancreatitis
- surgery
- injury to the stomach
- pelvic inflammatory disease
- cirrhosis
Common causes of ruptures that lead to peritonitis include:
- Medical procedures, such as peritoneal dialysis. Peritoneal dialysis uses tubes (catheters) to remove waste products from your blood when your kidneys can no longer adequately do so. An infection may occur during peritoneal dialysis due to unclean surroundings, poor hygiene or contaminated equipment. Peritonitis also may develop as a complication of gastrointestinal surgery, the use of feeding tubes or a procedure to withdraw fluid from your abdomen (paracentesis) and rarely as a complication of colonoscopy or endoscopy.
- A ruptured appendix, stomach ulcer or perforated colon. Any of these conditions can allow bacteria to get into the peritoneum through a hole in your gastrointestinal tract.
- Pancreatitis. Inflammation of your pancreas (pancreatitis) complicated by infection may lead to peritonitis if the bacteria spread outside the pancreas.
- Diverticulitis. Infection of small, bulging pouches in your digestive tract (diverticulitis) may cause peritonitis if one of the pouches ruptures, spilling intestinal waste into your abdominal cavity.
- Trauma. Injury or trauma may cause peritonitis by allowing bacteria or chemicals from other parts of your body to enter the peritoneum.
Peritonitis that develops without an abdominal rupture (spontaneous peritonitis) is usually a complication of liver disease, such as cirrhosis. Advanced cirrhosis causes a large amount of fluid buildup in your abdominal cavity (ascites). That fluid buildup is susceptible to bacterial infection.
Risk factors for peritonitis
Factors that increase your risk of peritonitis include:
- Peritoneal dialysis. Peritonitis is common among people undergoing peritoneal dialysis therapy.
- Other medical conditions. The following medical conditions increase your risk of developing peritonitis: cirrhosis, appendicitis, Crohn’s disease, stomach ulcers, diverticulitis and pancreatitis.
- History of peritonitis. Once you’ve had peritonitis, your risk of developing it again is higher than it is for someone who has never had peritonitis.
Peritonitis prevention
Often, peritonitis associated with peritoneal dialysis is caused by germs around the catheter. If you’re receiving peritoneal dialysis, take the following steps to prevent peritonitis:
- Wash your hands, including underneath your fingernails and between your fingers, before touching the catheter.
- Clean the skin around the catheter with an antiseptic every day.
- Store your supplies in a sanitary area.
- Wear a surgical mask during your dialysis fluid exchanges.
- If you have pets, don’t sleep with them.
- Talk with your dialysis care team about proper care for your peritoneal dialysis catheter.
If you’ve had spontaneous peritonitis before or if you have peritoneal fluid buildup due to a medical condition such as cirrhosis, your doctor may prescribe antibiotics to prevent peritonitis. If you’re taking a proton pump inhibitor, your doctor may ask you to stop taking it.
If you develop new abdominal pain or have a new injury
- Seek immediate medical attention if you develop abdominal pain so severe that you’re unable to sit still or find a comfortable position.
- Call your local emergency number for medical assistance if you have severe abdominal pain following an accident or injury.
Signs and symptoms of peritonitis
Signs and symptoms of peritonitis include:
- Abdominal pain or tenderness
- Bloating or a feeling of fullness (distention) in your abdomen
- Fever
- Nausea and vomiting
- Loss of appetite
- Diarrhea
- Low urine output
- Thirst
- Inability to pass stool or gas
- Fatigue
If you’re receiving peritoneal dialysis, peritonitis symptoms may also include:
- Cloudy dialysis fluid
- White flecks, strands or clumps (fibrin) in the dialysis fluid
Peritonitis complications
Left untreated, peritonitis can extend beyond your peritoneum, where it may cause:
- A bloodstream infection (bacteremia or sepsis).
- An infection throughout your body (sepsis). Sepsis is a rapidly progressing, life-threatening condition that can cause shock and organ failure.
Peritonitis diagnosis
To diagnose peritonitis, your doctor will talk with you about your medical history and perform a physical exam. When peritonitis is associated with peritoneal dialysis, your signs and symptoms, particularly cloudy dialysis fluid, may be enough for your doctor to diagnose the condition.
In cases of peritonitis in which the infection may be a result of other medical conditions (secondary peritonitis) or in which the infection arises from fluid buildup in your abdominal cavity (spontaneous peritonitis), your doctor may recommend the following tests to confirm a diagnosis:
- Blood tests. A sample of your blood may be drawn and sent to a lab to check for a high white blood cell count. A blood culture also may be performed to determine if there are bacteria in your blood.
- Imaging tests. Your doctor may want to use an X-ray to check for holes or other perforations in your gastrointestinal tract. Ultrasound may also be used. In some cases, your doctor may use a computerized tomography (CT) scan instead of an X-ray.
- Peritoneal fluid analysis. Using a thin needle, your doctor may take a sample of the fluid in your peritoneum (paracentesis), especially if you receive peritoneal dialysis or have fluid in your abdomen from liver disease. If you have peritonitis, examination of this fluid may show an increased white blood cell count, which typically indicates an infection or inflammation. A culture of the fluid may also reveal the presence of bacteria.
The above tests may also be necessary if you’re receiving peritoneal dialysis and a diagnosis of peritonitis is uncertain after a physical exam and an examination of the dialysis fluid.
Peritonitis treatment
If you’re diagnosed with peritonitis you’ll need treatment in hospital to get rid of the infection. This might take 10 to 14 days. Treatment usually involves being given antibiotics into a vein (intravenously).
Treatment may include:
- Antibiotics. You’ll likely be given a course of antibiotic medication to fight the infection and prevent it from spreading. The type and duration of your antibiotic therapy depend on the severity of your condition and the kind of peritonitis you have.
- Surgery. Surgical treatment is often necessary to remove infected tissue, treat the underlying cause of the infection, and prevent the infection from spreading, especially if peritonitis is due to a ruptured appendix, stomach or colon.
- Other treatments. Depending on your signs and symptoms, your treatment while in the hospital may include pain medications, intravenous (IV) fluids, supplemental oxygen and, in some cases, a blood transfusion.
If you’re undergoing peritoneal dialysis
If your peritonitis was caused by kidney dialysis treatment, antibiotics may be injected directly into the stomach lining.
If you have regular kidney dialysis your doctor might discuss a different way for dialysis for several days of doing it until the peritonitis has been treated. If peritonitis persists or recurs, you may need to stop having peritoneal dialysis entirely and switch to a different form of dialysis.
Help with eating during treatment
It can be hard to digest food if you have peritonitis. A feeding tube might be passed into your stomach through your nose or placed inside your stomach using keyhole surgery.
If a feeding tube can’t be used liquid nutrients can be given directly into one of your veins.
Surgery for peritonitis
If part of the stomach lining has been seriously damaged by infection you may need surgery to remove it.
Sometimes pus-filled swellings (abscesses) develop in the lining and need to be drained with a needle under local anesthetic.
You might also need an operation to deal with the cause of the peritonitis. For example, a burst appendix will need to be removed.
References- Brown D, Caballero Alvarado JA. Sepsis (Septic), Peritonitis. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526129
- Foris LA, Haseeb M. Spontaneous Bacterial Peritonitis. [Updated 2018 Dec 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448208
- Maraolo AE, Gentile I, Pinchera B, Nappa S, Borgia G. Current and emerging pharmacotherapy for the treatment of bacterial peritonitis. Expert Opin Pharmacother. 2018 Aug;19(12):1317-1325.
- Bolia R, Srivastava A, Marak R, Yachha SK, Poddar U. Prevalence and Impact of Bacterial Infections in Children With Liver Disease-A Prospective Study. J Clin Exp Hepatol. 2018 Mar;8(1):35-41.
- Oey RC, de Man RA, Erler NS, Verbon A, van Buuren HR. Microbiology and antibiotic susceptibility patterns in spontaneous bacterial peritonitis: A study of two Dutch cohorts at a 10-year interval. United European Gastroenterol J. 2018 May;6(4):614-621.
- MacIntosh T. Emergency Management of Spontaneous Bacterial Peritonitis – A Clinical Review. Cureus. 2018 Mar 01;10(3):e2253.
- Moreau R, Elkrief L, Bureau C, Perarnau JM, Thévenot T, Saliba F, Louvet A, Nahon P, Lannes A, Anty R, Hillaire S, Pasquet B, Ozenne V, Rudler M, Ollivier-Hourmand I, Robic MA, d’Alteroche L, Di Martino V, Ripault MP, Pauwels A, Grangé JD, Carbonell N, Bronowicki JP, Payancé A, Rautou PE, Valla D, Gault N, Lebrec D., NORFLOCIR Trial Investigators. Effects of Long-term Norfloxacin Therapy in Patients With Advanced Cirrhosis. Gastroenterology. 2018 Dec;155(6):1816-1827.e9.
- Haj M, Hart M, Rockey DC. Development of a novel clinical staging model for cirrhosis using the Nationwide Inpatient Sample. J. Investig. Med. 2018 Aug;66(6):992-997.