What is a pessary
The pessary is a medical device placed into your vagina for the management of pelvic organ prolapse and urinary stress incontinence 1. Pelvic organ prolapse refers to loss of support for the pelvic organs (bladder, uterus, bowel) and their descent into the vagina.
Types of pelvic organ prolapse:
- Uterine/ cervical prolapse: Observation of descent of the uterus or uterine cervix.
- Vaginal vault (cuff scar) prolapse: Observation of descent of the vaginal vault (cuff scar after hysterectomy).
- Anterior vaginal wall prolapse: Observation of descent of the anterior vaginal wall. Most commonly this would be due to bladder prolapse (cystocele, either central, paravaginal or a combination). Higher stage anterior vaginal wall prolapse will generally involve uterine or vaginal vault (if uterus is absent) descent. Occasionally, there might be anterior enterocele formation after prior reconstructive surgery.
- Posterior vaginal wall prolapse: Observation of descent of the posterior vaginal wall. Most commonly, this would be due to rectal protrusion into the vagina (rectocele). Higher stage posterior vaginal wall prolapse after prior hysterectomy will generally involve some vaginal vault (cuff scar) descent and possible enterocele formation. Enterocele formation can also occur in the presence of an intact uterus.
Pessaries have been used to treat women with pelvic organ prolapse since the beginning of recorded history 2. Hippocrates described reduction of vaginal prolapse by placing a halved pomegranate soaked in wine into the vagina 3. Pessaries are predominantly prescribed and fitted by gynecologists or general medical practitioners (family doctors) with a special interest in women’s health. There are some clinics where nurses are responsible for the review of women fitted with pessaries by gynecologists and urogynecologists. Pessaries are used in daily practice by more than 86% of gynecologists and 98% of urogynecologists 4.
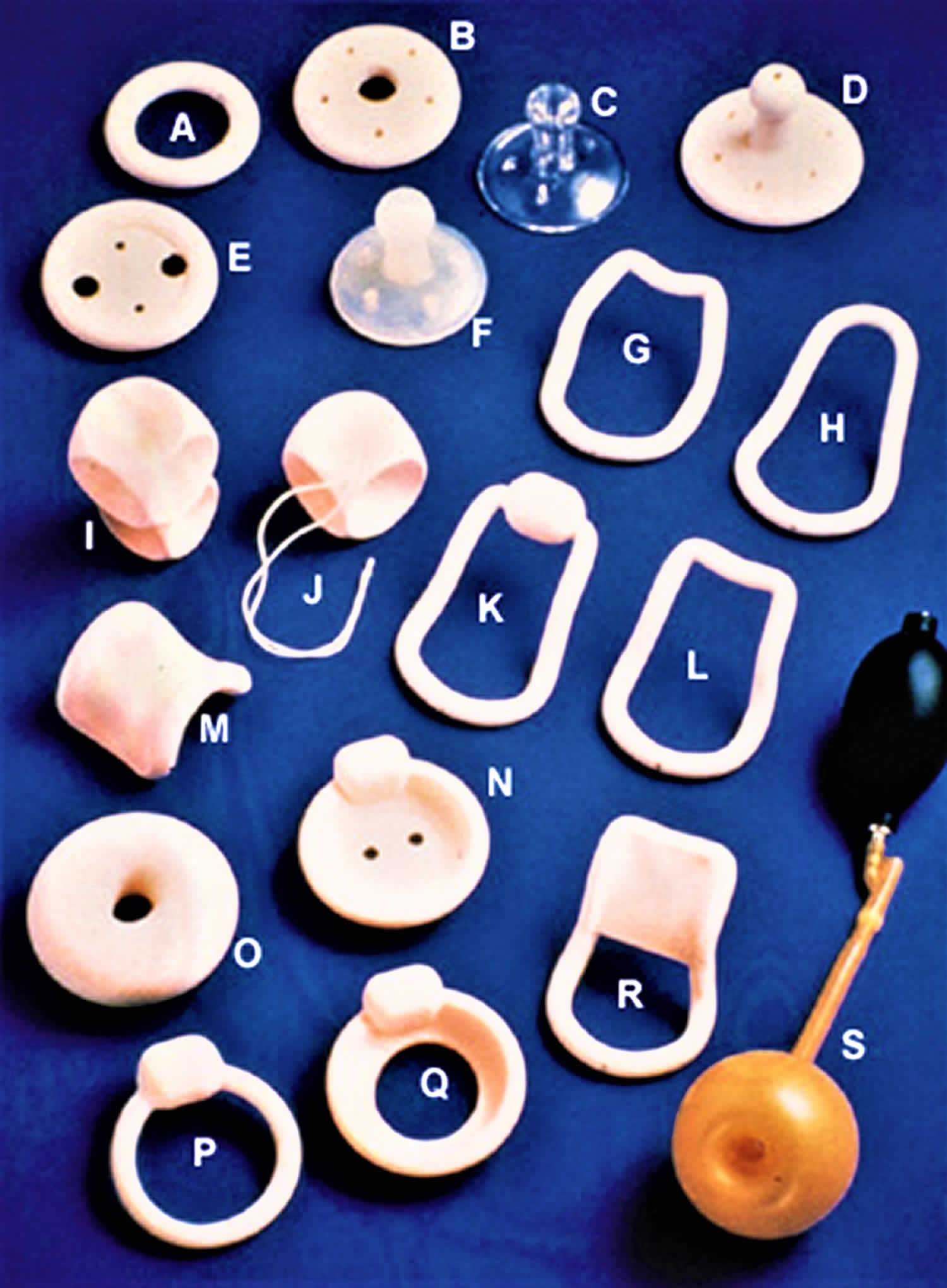
The type of pessary that is appropriate for each patient depends on the condition being treated (see Figure 1). The pessary is most commonly used in the management of pelvic support defects such as prolapsed bladder into the vagina (cystocele) and herniation or bulging of the front wall of the rectum into the back wall of the vagina (rectocele). Pessaries can also be used in the treatment of stress urinary incontinence. The wide variety of pessary styles may cause confusion during the initial selection of the pessary. However, an understanding of the different styles and their uses will enable you to make an appropriate choice. Complications can be minimized with simple vaginal hygiene and regular follow-up visits to your doctor.
Nowadays, most pessaries are made of silicone and are ring type pessaries with or without central support, Gellhorn pessaries and donut pessaries (Figure 2) 5. The ring with central support and the Gellhorn pessary are most frequently used and appear equally effective in relieving symptoms of genital prolapse and voiding dysfunction 6.
The goal of pessary use is to lessen the frequency and severity of prolapse and/or incontinence symptoms as well as to avoid or delay the need for surgery 7. In general, pessaries are a safe, inexpensive, and simple treatment option with high patient satisfaction rates 2. Other work has shown an improvement in co-morbid pelvic floor disorders, such as defecatory dysfunction, an increase in frequency and satisfaction of sexual activity and improvement in body image with pessary use 8.
Gynecologic conditions that can be managed with pessaries:
- Stress urinary incontinence
- Vaginal vault prolapse
- Cystocele (prolapsed bladder into the vagina)
- Enterocele (small bowel prolapse into the vagina)
- Rectocele (herniation or bulging of the front wall of the rectum into the back wall of the vagina)
- Uterine prolapse
- Preoperative preparation
Figure 1. Vaginal pessary
Footnote: Various types of pessaries: (A) Ring, (B) Shaatz, (C) Gellhorn, (D) Gellhorn, (E) Ring with support, (F) Gellhorn, (G) Risser, (H) Smith, (I) Tandem cube, (J) Cube, (K) Hodge with knob, (L) Hodge, (M) Gehrung, (N) Incontinence dish with support, (O) Donut, (P) Incontinence ring, (Q) Incontinence dish, (R) Hodge with support, (S) Inflatoball (latex).
[Source 9 ]Figure 2. Commonly used pessary device
Footnote: Pessary most prescribed. Doughnut pessary, Gellhorn pessary, ring pessary with and without support.
[Source 10 ]Ring pessary
- With and without central support diaphragm.
- Easiest to use for provider and user
- Can be used for any type of prolapse
- Intercourse is generally possible
- Sizing varies with the brand of pessary (Sizes 0-9: approx. 44mm-101mm).
Gellhorn pessary
- A space-filling pessary with a wide base and either a long or short stem
- The base creates suction onto the vaginal walls so that it stays in place without relying on the symphysis to keep it in place
- The cervix rests in the concave upper surface of the base, while the knob at the end of the stem rests on the posterior vaginal wall and perineal body
- Can be difficult for the inexperienced provider and user to insert and remove. Sponge or ring forceps can be used to facilitate removal
- Useful for all types of prolapse
- Must be removed for intercourse, which makes them less suitable for sexually active women
- Sizing varies with the brand of pessary (Sizes 0-8: approx. 38mm-89mm).
Cube pessary
- A space-filling pessary in the shape of a uniform square with six concave surfaces. It comes with perforations to allow passage of some vaginal secretions and with a loop, like a tampon string, to locate it and assist removal.
- The concave surfaces provide suction onto the vaginal walls to hold it in place
- Must be removed for intercourse
- Should be removed nightly
- It may be difficult to insert and remove
- Sizing varies with the brand of pessary (Sizes 0-10: approx. 25mm-75mm).
Figure 3. Types of pessary
Figure 4. Pelvic organ prolapse
Vaginal pessary uses
The pessary is most commonly used in the nonsurgical management of pelvic organ prolapse. Multiple vaginal deliveries can weaken the musculature of the pelvic floor. Hysterectomy or other pelvic surgery can predispose a woman to weakness of the pelvic floor, as can conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting 11.
Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a temporary management option. As the geriatric population continues to increase, more patients are presenting with pelvic floor defects. While many of these patients are poor candidates for surgery, most of them can safely use a pessary.
Pessaries are a first-line management option for women with pelvic organ prolapse. In particular, pessary prescription is appropriate for women:
- with symptomatic pelvic organ prolapse
- who decline surgery
- who are unfit for or awaiting surgery
- who have failed surgery
- who have not completed childbearing
- who are pregnant or postpartum
- who are of older age and with co-morbidities.
Table 1. Various Types of Pessaries and Their Uses
| Type | Uses | Most common sizes | Ease of insertion and removal |
|---|---|---|---|
Ring* | Mild uterine prolapse | 3 to 5 | Easy |
Incontinence ring* | Stress urinary incontinence | 2 to 7 | Easy |
Ring with support* | Mild uterine prolapse | 3 to 5 | Easy |
Mild cystocele | |||
Incontinence dish* | Stress urinary incontinence | 3 to 5 | Medium |
Mild uterine prolapse | |||
Dish with support* | Mild cystocele | 3 to 5 | Medium |
Stress urinary incontinence | |||
Mild uterine prolapse | |||
Donut* | Moderate uterine prolapse | 2 1/2 to 3 inches | Medium |
Mild cystocele | |||
Gellhorn* | Moderate uterine prolapse | 2 1/4 to 2 3/4 inches | Difficult |
Mild cystocele | |||
Inflatable* | Moderate uterine prolapse | Medium and large | Easy |
Cube* | Moderate to severe uterine prolapse | 2 to 4 | Medium |
Mild cystocele | |||
Mild rectocele | |||
Other vaginal vault prolapse | |||
Gehrung* | Moderate to severe cystocele | 3 to 5 | Difficult |
Mild rectocele | |||
Moderate to severe uterine prolapse | |||
Gehrung with knob* | Same uses as Gehrung | 3 to 5 | Difficult |
Stress urinary incontinence | |||
Hodge* | Mild cystocele | 2 to 4 | Medium |
Hodge with support* | Mild cystocele | 2 to 4 | Medium |
Stress urinary incontinence | |||
Smith, Risser* | Mild cystocele | 2 to 4 | Medium |
Stress urinary incontinence | |||
Introl† | Stress urinary incontinence | Call manufacturer | Easy |
Footnote:
* —Manufactured by Milex
† —Manufactured by Uromed
[Source 9 ]Classification of uterine prolapse
Uterine prolapse is classified by degree (Figure 5). In first-degree uterine prolapse, the cervix is visible when the perineum is depressed. In second-degree prolapse, the cervix is visible outside of the vaginal introitus, while the uterine fundus remains inside. In third-degree prolapse, or procidentia, the entire uterus is outside of the vaginal introitus. Uterine prolapse is associated with incontinence, vaginitis, cystitis and, possibly, uterine malignancy 12.
Pelvic organ prolapse quantification
- Grade 0: No prolapse is demonstrated.
- Grade 1: Most distal portion of the prolapse is more than 1cm above the level of the hymen.
- Grade 2: Most distal portion of the prolapse is 1 cm or less proximal to or distal to the plane of the hymen.
- Grade 3: The most distal portion of the prolapse is more than 1cm below the plane of the hymen.
- Grade 4: Essentially complete eversion of the total length of the lower genital tract is demonstrated.
Figure 5. Uterine prolapse grade [(1) First-degree, (II) second-degree, (III) third-degree and (IV) fourth-degree uterine prolapse]
Uterine prolapse treatment
First- and second-degree uterine prolapse are usually managed with a ring pessary. The donut and inflatable pessaries are also useful in the treatment of mild to moderate uterine prolapse. If the uterine prolapse is associated with a cystocele, a ring pessary with support is useful.
The cube pessary is designed to manage third-degree uterine prolapse. Because the cube is held in place by suction, removal can be somewhat difficult for some patients. This type of pessary can support the uterus even with a lack of vaginal tone. The cube pessary should be removed and cleaned daily, because it has no drainage capability 12.
A donut, inflatable or Gellhorn pessary can also be used in patients with third-degree uterine prolapse. The Gellhorn pessary is designed to manage severe uterine or vaginal prolapse. While the Gellhorn offers strong support, it can also be difficult for the patient to remove. If a cystocele or rectocele accompanies the third-degree uterine prolapse, a Gehrung pessary may be the most helpful. However, the Gehrung can be difficult to insert.
Types of vaginal prolapse
Variants of vaginal prolapse include rectocele, enterocele, cystocele and vault prolapse. A rectocele (Figure 6) occurs when the fascial layers between the rectum and the vagina become weak. This weakening allows the rectum to herniate, causing a bulging of the posterior vagina. The patient may report having to manually reduce the rectocele before defecation. An enterocele is the herniation of the sigmoid colon into the upper posterior vaginal wall (Figure 7). An enterocele differs from a rectocele in that it is a true hernia, lined by peritoneum and usually containing small bowel.
Figure 6. Rectocele (R = rectocele)
Figure 7. Enterocele
A cystocele (Figure 8) occurs when the tissues between the bladder and the vagina weaken, leading to a herniation of the bladder. This herniation causes a bulge in the anterior vaginal wall. Other portions of the vaginal vault may prolapse as well. Such vault prolapse may or may not cause symptoms.
Figure 8. Cystocele
Vaginal prolapse treatment
In patients with a mild cystocele, treatment using a ring with support, a dish with support, a Hodge with support or a donut pessary will suffice. To manage a large prolapse of the anterior vaginal wall, the Gellhorn pessary may be the best choice, although insertion and removal can be difficult. Inflatable and cube pessaries are also useful in patients with a larger cystocele. In patients with rectoceles and enteroceles, the use of a Gellhorn, donut, inflatable or cube pessary is usually required to provide the necessary support.
Stress urinary incontinence
Stress urinary incontinence, which is the involuntary loss of urine during exertion, is a common problem that affects many women. In one survey of women older than 18 years, 22 percent complained of symptoms associated with stress urinary incontinence 13.
Pessaries should be used by patients for whom conservative management is appropriate. Good candidates for a pessary trial might include a pregnant patient, an elderly woman in whom surgery would be risky and a woman whose previous operation for stress incontinence failed. A pessary can also be used by women who only have stress urinary incontinence with strenuous exercise. The prevalence of stress urinary incontinence with strenuous exercise may be as high as 27 percent 14.
Urinary stress incontinence pessary
The pessary compresses the urethra against the upper posterior portion of the symphysis pubis and elevates the bladder neck. This causes an increase in outflow resistance and corrects the angle between the bladder and the urethra so that Valsalva’s maneuvers alone are not strong enough to cause leakage of urine. Any style of pessary that can accomplish this will help with the management of stress urinary incontinence.
The incontinence ring and incontinence dish pessaries are most commonly used in patients with stress urinary incontinence. A Hodge pessary with or without support, depending on the presence of a cystocele, can also be used. Introl, a bladder neck support prosthesis that is marketed by Uromed, is also available. The prosthesis has two prongs that support the urethrovesical junction and bladder neck. This device was found to be effective in 83 percent of adult women with stress urinary incontinence 15.
For women who have urinary incontinence during strenuous activities such as jogging, aerobics or tennis, a cube pessary that is inserted before exercise may be all that is needed. A Hodge pessary with support is also effective in the prevention of exercise incontinence 16.
The pessary can be used to differentiate between patients with stress urinary incontinence that is secondary to a correctable anatomic defect and those with bladder instability. A properly fitted pessary can simulate the result of surgical correction of incontinence, thereby yielding diagnostic and prognostic information 17.
Pessary selection and fitting
Special nurses, doctors and physiotherapists can put a pessary in place. You won’t need an anesthetic because it’s usually not too uncomfortable. Pessaries come in different sizes and should be fitted carefully. Because pessaries come in a number of sizes and shapes, you may need to try a few before you find one that is comfortable and provides the right support.
Pessary selection
Selection of an appropriate pessary depends primarily on the condition for which you’re being treated. The ring pessary (with or without support) is often advocated for the initial fitting as it is considered to be easier for women to remove and reinsert themselves 18. One trial found that 70% of women could be fitted successfully with a size 64mm, 70mm, 76mm ring pessary (2-3 trials were often needed) 19. However, in a clinical controlled trial, the ring-with-support and Gellhorn were used with equal success for all types and stages of prolapse 20. A Gellhorn or cube is often advocated for stage 3 or 4 prolapse 21 with Gellhorn sizes 64mm, 70mm, 76mm most commonly used 22. However, cube pessaries have been used for any type or grade of prolapse with 44% of women continuing use at 12 months 23. Other types of pessary are used at the discretion of the health care provider.
Pessaries are available from Milex, the largest manufacturer, at a cost of $31.00 to $51.50 per pessary. Of the pessaries that are indicated for a particular condition (see Table 1 above), the style that works the best for you should be chosen. For example, a Gellhorn pessary can offer excellent support for uterine prolapse as long as the perineal body is intact. If the perineal body is weak, a cube or donut pessary will be more effective 24. An incontinence ring pessary usually helps with stress urinary incontinence, but if the patient has some degree of cystocele, a Hodge with support or a Gehrung pessary may be more effective.
Pessary fitting
Pessaries are fit by trial and error with a set of fitting rings. In patients who use a diaphragm, the size of the diaphragm does not correlate with the size of the pessary. Proper fitting of the pessary often requires the patient to try several sizes and/or styles. A variety of styles and sizes should be made available during the patient’s fitting session. The manufacturer of the pessary can provide pessaries in the most common sizes that will fit the majority of patients. The manufacturer can also provide detailed instructions on how to fit each particular style of pessary.
- To assist in selection of the pessary style and size, estimate the vaginal dimensions:
- a) Determine the vaginal width; spread the index and middle fingers horizontally high in the upper vagina.
- b) Determine vaginal length: palpate the posterior fornix (or vaginal vault in the absence of the cervix) with the index or middle finger and estimate the distance to the pubic symphysis.
- c) Then visually compare the mental image of the vaginal vault size and shape with the actual pessaries, trying the pessary that most closely represents the visual image.
- Wash the pessary in soap and water to remove any corn starch used for packaging.
- Apply water-based lubricant to the leading edge of the pessary, or to the introitus, to make insertion easier, but avoid lubricant on the gloved hand holding the pessary.
- Separate the labia and insert the pessary at the introitus and, with gentle pressure, slide it up the posterior vaginal wall. Ease the pessary right up into position in the upper part of the vagina and behind the pubic symphysis.
- If it is difficult to fit a pessary e.g. in the case of very advanced prolapse, two pessaries may be tried together e.g. two ring pessaries.
After a complete pelvic examination has been performed, your doctor should start with an average-sized pessary in the simplest style. When the pessary has been put into place, the fit and effectiveness should be checked. The largest pessary that you can wear comfortably is generally the most effective. Your finger should pass easily between the pessary and the vaginal wall. Your physician should check the pessary to be sure that the intended function is met. When the indication of the pessary is for stress urinary incontinence, you should cough to test for any leakage of urine.
To test for correct pessary fit
- Ask the woman to cough and valsalva in dorsal lithotomy or bent knee lying position. A correctly sized pessary may descend in the vagina, however it should recede on relaxation.
- Ask the woman to stand up and walk around. There should be no discomfort and it should not be expelled with coughing, Valsalva, bending or squatting.
- A larger size or different type should be tried if it is nearly or completely expelled.
- A smaller size or different type should be tried in the event of discomfort in the vagina or low abdominal pain.
- A vague sensation of discomfort or irritation may be due to irritation from the actual fitting procedure. Clinical judgment will determine whether removal and refit is necessary.
- Ask the woman to void. Ideally, the Post Void Residual (PVR) should be checked with ultrasound to ensure that there is no significant residual urine due to obstruction. If symptoms of voiding dysfunction are reported, the patient should be referred for an ultrasound scan. A Post Void Residual of <100 ml is recommended by the Expert Working Party.
Note:
- A correctly fitted pessary:
- Should not be tight against the vaginal walls
- Should have enough room to allow a fingertip between the edges and the vaginal wall or to be able to rock it
- Should be retained and not felt by the woman at rest or on standing, sitting, walking around, squatting or coughing
- Should not dislodge during voiding.
Figure 9. Pessary fitting
Successful fitting
There is no agreed definition of a successful fit. However, a pessary is deemed to fit when the following criteria are met.
A successful pessary fit is when the:
- biggest pessary is comfortably retained during upright, provocative activities such as walking, squatting, valsalva and coughing
- pessary is not felt by the woman and does not cause any pain or discomfort
- pessary does not obstruct bladder or bowel emptying
- pessary does not provoke occult urinary incontinence.
Reports of successful fitting at the first consultation vary from 74% – 94% 25. Cundiff et al 20 reported successfully fitting 92% of women at the first visit. However, several trials may be required to find the best fit. For those women who have not retained the pessary or when the pessary is uncomfortable or causes low abdominal pain, a further trial with a different size or type of pessary is recommended 19. Reports suggest that 76% of women can be successfully fitted at the follow-up visit (average 1.5 (range 1-4) pessaries). If occult urinary incontinence is provoked, an incontinence pessary may be tried, but these are outside the scope of this document. In this case, referral to a suitable medical practitioner is indicated to exclude other issues such as obstructed voiding.
The number of women continuing to use a pessary reduces with time 20. One study suggests that 66% of women using a pessary at 1 month continued for 1 year and 53% of these continued for 3 years 19. There are few studies reporting pessary use over longer periods, but one suggests a very low rate of continued use over 14 years 26.
Factors predicting success
Success or failure will depend on appropriate pessary selection, patient characteristics, provider training and experience, thorough counseling, as well as the achievement of an adequate fit and patient satisfaction 27.
Patient factors
There is little agreement in the literature regarding factors such as patient age, parity, obesity or hormone use predicting a successful pessary fitting 28.
The following factors have been reported in some studies as negatively impacting on the likelihood of successful fitting:
- short vaginal length (=/<6cm) 29
- wide vaginal introitus (>4 finger width) 29
- prior hysterectomy 30
- prior vaginal prolapse surgery 30
- severe posterior vaginal prolapse 30
- stress urinary incontinence 31.
Others have found that the stage of prolapse 28, predominant compartment 32 and genital hiatus size 32 did not predict successful fitting.
Discontinuation
The most common reasons for discontinuation of pessary use are:
- desire for surgery
- development or persistence of incontinence
- failure to retain the pessary
- inadequate support of prolapse
- dislike of the changing procedure
- discomfort
- pain
- vaginal discharge.
How to insert a pessary for prolapse
- Wash your hands.
- The notches inside the open ring and the openings in the ring-with-support are the flexible points. Grasp the device midway between these points and fold the pessary in half. The curved part should be facing the ceiling, like a taco. Put a small amount of water-soluble lubricant, such as KY Jelly, on the insertion edge.
- Hold the folded pessary in one hand and spread the lips of your vagina with the other hand. Gently push the pessary as far back into the vagina as it will go. You can do this squatting, standing with one foot propped on the tub or toilet, or sitting with your feet propped up.
Ring Pessary
- Two notches to allow it to be folded for insertion.
- For the ring with support, fold along the axis of the large holes.
To insert:
- Lubricate leading edge of pessary
- Fold the pessary over, concave side down, introduce it at the introitus, gently slide it up the posterior vaginal wall as far as possible before releasing. The index finger can help to push up the ring anteriorly behind the symphysis so that it sits parallel to the vaginal axis and behind the cervix in the posterior fornix. When correctly in situ, the cervix should sit in the ring or on the supportive diaphragm when the ring with support is used.
- Rotate the ring so the indentations are laterally to prevent expulsion (Bash 2000).
Gellhorn Pessary
To insert:
- Lubricate leading edge of pessary
- Holding the stem with the dominant hand, separate the labia with the non-dominant hand. With the convex base perpendicular to the introitus and slightly oblique to avoid the urethra, the leading edge enters the vagina with pressure directed along the posterior vaginal wall and easing the pessary in under the inferior pubic rami.
- To get the Gellhorn into position, use the index finger to push the knob up the axis of the vagina.
- When properly seated, the base of the Gellhorn pessary will be orientated at right angles to the vaginal canal and the stem and knob will lie along the vaginal canal and be visible at the introitus when the labia are separated.
- There is usually no descent of the Gellhorn with a valsalva because of the suction maintaining it in the upper vagina.
- If the Gellhorn provides good support but the stem is too long and projecting out of the vagina, the same sized model with a short stem can be substituted.
Cube Pessary
To insert:
- Lubricate the top edge of the cube or the vaginal introitus with a water-based gel.
- Compress the cube as much as possible with two gloved hands and insert at the introitus with downward pressure on the posterior vaginal wall, pushing it into the upper vagina with the index finger. Ensure that the loop is visible in the vaginal lumen and accessible for removal later.
Pessary care
Caring for a pessary is easy. Pessaries can be left in place for up to a week and removed for periodic easy cleaning. Some women choose to remove the pessary nightly before bed and replace it in the morning. It can be left in during intercourse if this is comfortable for you.
- Remove the pessary weekly/monthly for cleaning with soap and water
- Insert Trimosan or estrogen cream 2-3 x per week
- Vaginal examination by healthcare provider every 3-6 months to check for fit, erosions
Follow-up
After the initial fitting of the pessary, you should be followed-up within a few days so that your doctor can recheck the fit. The pessary should be removed so that the vagina can be examined for irritation, pressure sores or allergic reaction. Having to change the size of the pessary at least once after the initial fitting is not uncommon. You should then be instructed to follow-up within one to two weeks for another examination, after which time the examinations can be spaced to every two to three months. In the motivated patient who is able to demonstrate effective removal, insertion and care of the pessary, these examinations may be spaced further at the discretion of your doctor 33.
At each follow-up examination, the pessary should be removed and cleaned with soap and water while the vagina is inspected for erosions, pressure necrosis or allergic reaction. If inspection of the pessary reveals cracking or other defects, it should be replaced. The patient who is using a pessary should be considered to be under the care of the person who placed it for the duration of its use. Pessaries should never be placed in elderly, debilitated patients without excellent follow-up.
How to remove a pessary yourself
- Wash your hands.
- Find the rim of the pessary just under the pubic bone at the front of your vagina. Locate the notch or opening and hook your finger under or over the rim.
- Tilt the pessary slightly, to about a 30 degree angle, and gently pull down and out of the vagina. If you can fold the pessary somewhat, it will ease the removal.
Bearing down as if you are having a bowel movement can help push the rim of the pessary forward so you can grasp it more easily.
Ring Pessary
To remove:
- Rotate the ring with indentations to be anterior-posterior to allow folding and easier removal.
- Hook the index finger under the leading edge and draw it down while the woman gently valsalvas. Rotate the pessary obliquely to remove with gentle traction. A loop of dental floss can be attached to make removal easier.
Gellhorn Pessary
To remove:
- Grasp the knob with the dominant hand and pull it down towards the introitus while the index finger of the non-dominant hand sweeps behind the base to release the suction. Once the suction is released, reverse the steps used for insertion in order to remove it. It is not usually possible to pull it straight down, so the suction must be broken first. Sometimes sponge or ring-forceps may be needed to grasp the knob, break the suction and remove the pessary.
Cube Pessary
To remove:
- Locate the loop and sweep around the sides of the pessary with the non-dominant index finger to break the suction. Pull down gently on the loop, grasping the edge of the cube with fingers to remove it.
- Do not just pull on the string for removal but grip the actual pessary.
Pessary contraindications
There are few contraindications to the use of a pessary. Active infections of the pelvis or vagina, such as vaginitis or pelvic inflammatory disease, preclude the use of a pessary until the infection has been resolved. Patients who are noncompliant or unlikely to follow up should not be fitted for a pessary. Most pessaries are made of silicone; some are made of latex. An allergy to the product would also be a contraindication.
Contra-indications for pessary use are:
- active vaginal infection
- pelvic inflammatory disease
- undiagnosed vaginal bleeding
- when follow-up cannot be assured.
Pessary complications
Although the pessary is an extremely safe device, it is still a foreign body in the vagina. Because of this, the most common side effects of pessary use are increased vaginal discharge, foul smell, bleeding, pain and constipation 34. A recent study reported that 56% of women wearing a pessary reported one of these side effects 34. This side effect can be minimized with the use of an acidic vaginal gel such as Trimo-San, which also helps to relieve minor irritation and itching. Some physicians recommend that patients douche with dilute vinegar or hydrogen peroxide for relief 35. Changing a pessary at frequent intervals could also prevent this vaginal irritation. Therefore, it is helpful if the patient is willing and able to remove, clean and replace the pessary herself 36.
Rarely, pessaries cause major urinary, rectal and genital complications such as fistula, fecal impaction, hydronephrosis and urosepsis 3. These rare complications are almost exclusively related to a long period of use and negligence of care. With regular follow-up, the majority of pessary complications can be avoided and kept to a minimum 37.
Postmenopausal women with thin vaginal mucosa are more susceptible to vaginal ulceration with use of a pessary. Treatment with estrogen cream can make the vaginal mucosa more resistant to erosion and should be used before or concurrently with the fitting of the pessary in such patients 33.
A pessary that is neglected can become embedded in vaginal mucosa and may be difficult to remove. In some cases, the use of estrogen cream may enable easier removal of the pessary by decreasing inflammation and promoting epithelial maturation 38. In extreme and rare cases, the pessary must be removed surgically 24. Even with a neglected, embedded pessary, the development of a fistula is extremely rare 24.
In the patient with an improperly fitted ring pessary, the cervix and lower uterus can herniate through the open center of the ring and become incarcerated. If not recognized, this incarceration could lead to strangulation and necrosis of the cervix and uterus 24.
While vaginal cytology may reveal inflammatory changes, the presence of a pessary does not increase the patient’s risk of developing vaginal cancer 24.
References- Brown LK, Fenner DE, DeLancey JO, Schimpf MO. Defining Patient Knowledge and Perceptions of Vaginal Pessaries for Prolapse and Incontinence. Female Pelvic Med Reconstr Surg. 2016;22(2):93-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4983771/
- Pessary treatment for pelvic organ prolapse and health-related quality of life: a review. Lamers BH, Broekman BM, Milani AL. Int Urogynecol J. 2011 Jun; 22(6):637-44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3097351/
- Pelvic organ prolapse. Jelovsek JE, Maher C, Barber MD. Lancet. 2007 Mar 24; 369(9566):1027-38.
- Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Richter HE, Burgio KL, Brubaker L, Nygaard IE, Ye W, Weidner A, Bradley CS, Handa VL, Borello-France D, Goode PS, Zyczynski H, Lukacz ES, Schaffer J, Barber M, Meikle S, Spino C, Pelvic Floor Disorders Network. Obstet Gynecol. 2010 Mar; 115(3):609-17.
- A survey of pessary use by members of the American urogynecologic society. Cundiff GW, Weidner AC, Visco AG, Bump RC, Addison WA. Obstet Gynecol. 2000 Jun; 95(6 Pt 1):931-5.
- The PESSRI study: symptom relief outcomes of a randomized crossover trial of the ring and Gellhorn pessaries. Cundiff GW, Amundsen CL, Bent AE, Coates KW, Schaffer JI, Strohbehn K, Handa VL. Am J Obstet Gynecol. 2007 Apr; 196(4):405.e1-8.
- Mechanical devices for pelvic organ prolapse in women. Adams E, Thomson A, Maher C, Hagen S. Cochrane Database Syst Rev. 2004; (2):CD004010.
- Impact of pessary use on prolapse symptoms, quality of life, and body image. Patel M, Mellen C, O’Sullivan DM, LaSala CA. Am J Obstet Gynecol. 2010 May; 202(5):499.e1-4.
- Practical Use of the Pessary. Am Fam Physician. 2000 May 1;61(9):2719-2726. https://www.aafp.org/afp/2000/0501/p2719.html
- Lamers BH, Broekman BM, Milani AL. Pessary treatment for pelvic organ prolapse and health-related quality of life: a review. Int Urogynecol J. 2011;22(6):637-44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3097351/
- Davila GW. Vaginal prolapse: management with nonsurgical techniques. Postgrad Med. 1996;99:171–6181184–5.
- Zeitlin MP, Lebherz TB. Pessaries in the geriatric patient. J Am Geriatr Soc. 1992;40:635–9.
- Yarnell JW, Voyle GJ, Richards CJ, Stephenson TP. The prevalence and severity of urinary incontinence in women. J Epidemiol Community Health. 1981;35:71–4.
- Nygaard I, DeLancey JO, Arnsdorf L, Murphy E. Exercise and incontinence. Obstet Gynecol. 1990;75:848–51.
- Davila GW, Ostermann KV. The bladder neck support prosthesis: a nonsurgical approach to stress incontinence in adult women. Am J Obstet Gynecol. 1994;171:206–11
- Nygaard I. Prevention of exercise incontinence with mechanical devices. J Reprod Med. 1995;40:89–94.
- Bhatia NN, Bergman A. Pessary test in women with urinary incontinence. Obstet Gynecol. 1985;65:220–6.
- ACOG. ACOG Practice Bulletin: clinical management guidelines for obstetrician-gynecologists, Number 85, September 2007. Pelvic organ prolapse. American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Gynecology American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Gynecology. Obstetrics & Gynecology. 2007; 110(3): 717-29.
- Wu, Farrell SA, Baskett TF, Flowerdew G. Simplified Protocol for pessary use. Journal of Obstetrics and Gynaecology. 1997; 90: 990-4.
- Cundiff GW, Amundsen CL, Bent AE, Coates KW, Schaffer JI, Strohbehn K, Handa VL. The PESSRI study: symptom relief outcomes of a randomized crossover trial of the ring and Gellhorn pessaries. American Journal of Obstetrics and Gynecology. 2007; 196(4): 405.e1-405.e8.
- Roehl B, Buchanan EM. Urinary incontinence evaluation and the utility of pessaries in older women. Care Management Journals. 2006; 7(4): 213-7.
- Atnip SD. Pessary use and management for pelvic organ prolapse. Obstetrics & Gynecology Clinics of North America. 2009; 36(3): 541-63
- Kuhn A, Bapst D, Stadlmayr W, Vits K, Mueller MD. Sexual and organ function in patients with symptomatic prolapse: are pessaries helpful? Fertility and Sterility. 2009; 91(5): 1914-1918.
- Miller DS. Contemporary use of the pessary. In: Sciarra JJ, ed. Gynecology and obstetrics. Revised 1997 ed. Philadelphia: Lippencott-Raven, 1997:1–12.
- Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. American Journal of Obstetrics & Gynecology. 2004b; 190(4): 1025-9.
- Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: Discontinuation rates and adverse events. BJOG: An International Journal of Obstetrics and Gynaecology. 2009; 116(13): 1715-1721.
- Sitavarin S,Wattanayingcharoenchai R, Manonai J, Sarit-Apirak S, Chittacharoen A. The characteristics and satisfaction of the patients using vaginal pessaries. Journal of the Medical Association of Thailand. 2009; 92(6): 744-747.
- Friedman S, Sandhu, KS, Wang C, Mikhail MS, Banks E. Factors influencing long-term pessary use. International Urogynecology Journal and Pelvic Floor Dysfunction. 2010; 21(6): 673-678.
- Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Risk factors associated with an unsuccessful pessary fitting trial in women with pelvic organ prolapse. American Journal of Obstetrics & Gynecology. 2004c; 190(2): 345-50.
- Maito JM, Quam ZA, Craig E, Danner KA, Rogers RG. Predictors of successful pessary fitting and continued use in a nurse-midwifery pessary clinic. Journal of Midwifery & Women’s Health. 2006; 51(2): 78-84.
- Nguyen JN, Jones CR, Krissovich M. Pessary treatment of pelvic relaxation: factors affecting successful fitting and continued use. Journal of Wound, Ostomy & Continence Nursing. 2005; 32(4): 255-63.
- Mutone MF, Terry C, Hale DS, Benson JT. Factors which influence the short-term success of pessary management of pelvic organ prolapse. American Journal of Obstetrics & Gynecology. 2005; 193(1): 89-94.
- Brubacker L. The vaginal pessary. In: Friedman AJ, ed. American Urogynecologic Society Quarterly Report. 1991;9(3).
- Long-term vaginal ring pessary use: discontinuation rates and adverse events. Sarma S, Ying T, Moore KH. BJOG. 2009 Dec; 116(13):1715-21.
- Deger RB, Menzin AW, Mikuta JJ. The vaginal pessary: past and present. Postgrad Obstet Gynecol. 1993;13(18):1–8.
- Pelvic organ prolapse. Weber AM, Richter HE. Obstet Gynecol. 2005 Sep; 106(3):615-34.
- Arias BE, Ridgeway B, Barber MD. Complications of neglected vaginal pessaries: case presentation and literature review. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(8):1173–1178. doi: 10.1007/s00192-008-0574-2.
- Poma PA. Management of incarcerated vaginal pessaries. J Am Geriatr Soc. 1981;29:325–7.