What is Phosphorus
Phosphorus is an essential mineral contained in each cell in your body. Phosphorus is the second most abundant mineral in your body 1. The main function of phosphorus is in the formation of bones and teeth. Most phosphorus is in your bones and teeth, and some is in your genes (DNA and RNA) 2. In humans, phosphorus makes up about 1 to 1.4% of fat-free mass. Phosphorus makes up about 0.5 percent of the newborn infant body 3 and from 0.65 to 1.1 percent of the adult body total body weight 4, 5. About 85 % of the body’s phosphorus is in bones and teeth, and 14% is in soft tissues, including muscle, liver, heart and kidney and only 1% is present in extracellular fluids 2. Your body needs phosphorus to make energy and to carry out many important chemical processes. Phosphorus plays an important role in how your body uses carbohydrates and fats. Phosphorus is also needed for the body to make protein for the growth, regulation of the body’s acid-base balance, maintenance, and repair of cells and tissues. Phosphorus also helps the body make ATP (adenosine triphosphate), a molecule the body uses to store energy 6. In the form of phospholipids, phosphorus is also a component of cell membrane structure. In addition, phosphorus plays key roles in regulation of gene transcription, activation of enzymes, maintenance of normal pH in extracellular fluid, and intracellular energy storage 7.
Phosphorus works with the B vitamins. It also helps with the following:
- Kidney function
- Muscle contractions
- Normal heartbeat
- Nerve signaling
Phosphorus is also naturally present in many foods and available as a dietary supplement, mainly in the form of phosphates. Phosphorus is most commonly found in nature in its pentavalent form in combination with oxygen, as phosphate (PO43-) and phosphate esters 2. However, phosphorus in seeds and unleavened breads is in the form of phytic acid, the storage form of phosphorus 8. Because human intestines lack the phytase enzyme, much phosphorus in this form is unavailable for absorption 2. Phosphorus undergoes passive absorption in the small intestine, although some is absorbed by active transport 8.
Phosphorus homeostasis is intricately linked to that of calcium because of the actions of calcium-regulating hormones, such as parathyroid hormone (PTH) and 1,25-dihydroxy-vitamin D (1,25(OH)2D), at the level of the bone, the gut and the kidneys 9. In addition, phosphorus and calcium make up hydroxyapatite [Ca5(PO4)3(OH)], the main structural component in bones and tooth enamel 10. The combination of high phosphorus intakes with low calcium intakes increases serum PTH (parathyroid hormone) levels, but evidence is mixed on whether the increased parathyroid hormone (PTH) hormone levels decrease bone mineral density 11, 12.
The kidneys, bones, and intestines regulate phosphorus homeostasis, which requires maintenance of urinary losses at equivalent levels to net phosphorus absorption and ensuring that equal amounts of phosphorus are deposited and resorbed from bone 13. Several hormones, including estrogen and adrenaline, also affect phosphorus homeostasis. When kidney function declines, as in chronic kidney failure, the body cannot excrete phosphate efficiently, and serum levels rise 14.
Although phosphorus status is not typically assessed, phosphate can be measured in both serum and plasma 15. In adults, normal phosphate concentration in serum or plasma is 2.5 to 4.5 mg/dL (0.81 to 1.45 mmol/L) 15. Total phosphorus concentration in whole blood is 13 mmol/liter (40 mg/dl), most of which is in the phospholipids of red blood cells and plasma lipoproteins 1. Approximately 1 mmol/liter (3.1 mg/dl) is present as inorganic phosphate (Pi). This inorganic phosphate component, while a tiny fraction of body phosphorus (< 0.1 percent), is of critical importance. In adults this component makes up about 15 mmol (465 mg) and is located mainly in the blood and extracellular fluid. It is into this inorganic phosphate compartment that phosphate is inserted upon absorption from the diet and resorption from bone and from this compartment that most urinary phosphorus and hydroxyapatite mineral phosphorus are derived. This compartment is also the primary source from which the cells of all tissues derive both structural and high-energy phosphate 16.
Structurally, phosphorus occurs as phospholipids, which are a major component of most biological membranes, and as nucleotides and nucleic acids. The functional roles include: (1) the buffering of acid or alkali excesses, hence helping to maintain normal pH; (2) the temporary storage and transfer of the energy derived from metabolic fuels; and (3) by phosphorylation, the activation of many catalytic proteins. Since phosphate is not irreversibly consumed in these processes and can be recycled indefinitely, the actual function of dietary phosphorus is first to support tissue growth (either during individual development or through pregnancy and lactation) and, second, to replace excretory and dermal losses. In both processes it is necessary to maintain a normal level of Pi in the extracellular fluid (ECF), which would otherwise be depleted of its phosphorus by growth and excretion 17.
Hypophosphatemia is defined as serum phosphate concentrations lower than the low end of the normal range, whereas a concentration higher than the high end of the range indicates hyperphosphatemia. However, plasma and serum phosphate levels do not necessarily reflect whole-body phosphorus content 9. Furthermore, phosphorus is so readily available in the food supply so deficiency is rare. Hypophosphatemia, defined by a serum inorganic phosphorus concentration of < 0.80 mmol/L (2.48 mg/dL), only rarely occurs because of inadequate dietary phosphorus intake, and is generally due to metabolic disorders 9.
Excessively high levels of phosphorus in the blood (hyperphosphatemia), although rare, can combine with calcium to form deposits in soft tissues such as muscle. High levels of phosphorus in blood only occur in people with severe kidney disease or severe dysfunction of their calcium regulation.
Foods High in Phosphorus
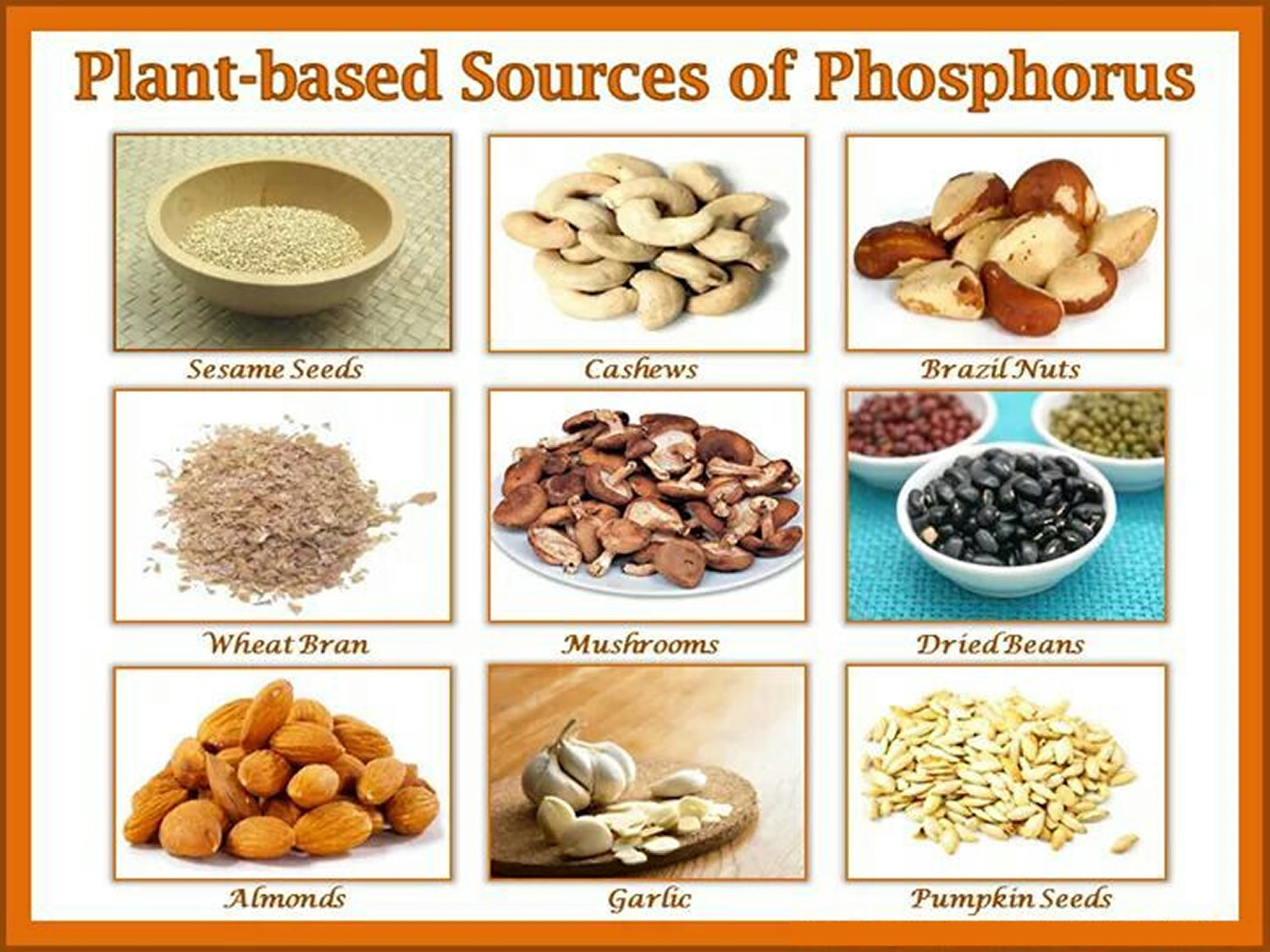
Many different types of foods contain phosphorus, including dairy products, meats and poultry, fish, eggs, nuts, legumes, vegetables, and grains 18. The major dietary contributors to phosphorus intake are foods high in protein content, i.e. milk and milk products followed by meat, poultry and fish, grain products and legumes. Several food sources of phosphorus are listed in Table 1. You can get recommended amounts of phosphorus by eating a variety of foods, including the following:
- Dairy products, such as yogurt, milk, and cheese
- Grain products, such as bread, tortillas, brown rice, and oatmeal
- Meats, poultry, fish, and eggs
- Nuts and seeds, such as cashews and sesame seeds
- Legumes, such as lentils, kidney beans, and peas
- Vegetables, such as potatoes and asparagus
Whole-grain breads and cereals contain more phosphorus than cereals and breads made from refined flour. However, the phosphorus is stored in a form that is not absorbed by humans.
Fruits and vegetables contain only small amounts of phosphorus.
Also, many processed foods have additives that contain phosphorus. These additives include phosphoric acid, sodium phosphate, and sodium polyphosphate. The U.S. Department of Agriculture’s (USDA’s) FoodData Central (https://fdc.nal.usda.gov/index.html) lists the nutrient content of many foods and provides a comprehensive list of foods containing phosphorus arranged by nutrient content (https://www.nal.usda.gov/sites/www.nal.usda.gov/files/phosphorus.pdf).
In the United States, dairy products contribute about 20% of total phosphorus intakes, and bakery products (e.g., breads, tortillas, and sweet bakery products) contribute 10% 18. Vegetables and chicken contribute 5% each. The absorption rate for the phosphorus naturally contained in food is 40%–70%; phosphorus from animal sources has a higher absorption rate than that from plants 19. Calcium from foods and supplements can bind to some of the phosphorus in foods and prevent its absorption 2. According to one analysis, a very high calcium intake of 2,500 mg/day binds 0.61–1.05 g phosphorus 20. In infants, phosphorus bioavailability ranges from 85%–90% for human milk to approximately 59% for soy-based formulas 8.
Phosphate additives (e.g., phosphoric acid, sodium phosphate, and sodium polyphosphate) are present in many foods, especially processed food products. Phosphates are a common additive in many dairy, cereals, packaged meals and other foods. Inorganic phosphates are used for such purposes as preserving moisture or color and enhancing and stabilizing frozen foods 21. Currently 4.3 percent of food additives contain phosphates, a number that has been on the rise. Inorganic phosphates are generally recognized as safe (GRAS) by the U.S. Food and Drug Administration. Foods containing these additives have an average of 67 mg more phosphorus per serving than similar foods not containing the additives, and these additives contribute to overall phosphorus intakes in the United States 22. The FDA does not require phosphorus to be reported on the Nutrient Facts Label, but it must be listed as an ingredient. Some are calling for this to change. Perhaps, this is one more reason to eat less processed foods.
Phosphate additives are estimated to contribute 300 to 1,000 mg to total daily phosphorus intakes 9 or about 10%–50% of phosphorus intakes in Western countries 23. The use of phosphate additives is rising, as are the amounts of these additives in foods 24. The absorption rate for the phosphorus in phosphate additives is approximately 70% 25.
There’s concern that inorganic phosphates have potential health implications. These additives may have a negative effect on heart and kidney function. It seems that added phosphates are absorbed and processed differently by your body than natural phosphorus found in meat, dairy and vegetables. Additionally, as phosphates are added to more foods and we continue to consume more packaged and processed foods, we may be consuming more than expected.
Table 1. Phosphorus content of selected foods
| Food | Milligrams (mg) per serving | Percent DV* |
| Yogurt, plain, low fat, 6-ounce container | 245 | 20 |
| Milk, 2% milkfat, 1 cup | 226 | 18 |
| Salmon, Atlantic, farmed, cooked, 3 ounces | 214 | 17 |
| Scallops, breaded and fried, 3 ounces | 201 | 16 |
| Cheese, mozzarella, part skim, 1.5 ounces | 197 | 16 |
| Chicken, breast meat, roasted, 3 ounces | 182 | 15 |
| Lentils, boiled, ½ cup | 178 | 14 |
| Beef patty, ground, 90% lean meat, broiled, 3 ounces | 172 | 14 |
| Cashew nuts, dry roasted, 1 ounce | 139 | 11 |
| Potatoes, Russet, flesh and skin, baked, 1 medium | 123 | 10 |
| Kidney beans, canned, ½ cup | 115 | 9 |
| Rice, brown, long-grain, cooked, ½ cup | 102 | 8 |
| Peas, green, boiled, ½ cup | 94 | 8 |
| Oatmeal, cooked with water, ½ cup | 90 | 7 |
| Egg, hard boiled, 1 large | 86 | 7 |
| Tortillas, corn, 1 medium | 82 | 7 |
| Bread, whole wheat, 1 slice | 60 | 5 |
| Sesame seeds, 1 tablespoon | 57 | 5 |
| Bread, pita, whole wheat, 4-inch pita | 50 | 4 |
| Asparagus, boiled, ½ cup | 49 | 4 |
| Tomatoes, ripe, chopped, ½ cup | 22 | 2 |
| Apple, 1 medium | 20 | 2 |
| Cauliflower, boiled, 1” pieces, ½ cup | 20 | 2 |
| Beverages, carbonated, cola, 1 cup | 18 | 1 |
| Clementine, 1 medium | 16 | 1 |
| Tea, green, brewed, 1 cup | 0 | 0 |
Footnotes: *DV = Daily Value. The U.S. Food and Drug Administration (FDA) developed DVs to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The DV for phosphorus is 1,250 mg for adults and children age 4 years and older. FDA does not require food labels to list phosphorus content unless phosphorus has been added to the food. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 26 ]
Phosphorus Absorption, Metabolism, and Excretion
Food phosphorus is a mixture of inorganic and organic forms. Intestinal phosphatases hydrolyze the organic forms contained in ingested protoplasm, and thus most phosphorus absorption occurs as inorganic phosphate. On a mixed diet, net absorption of total phosphorus in various reports ranges from 55 to 70 percent in adults 27, 28, 29 and from 65 to 90 percent in infants and children 30, 31. There is no evidence that this absorption efficiency varies with dietary intake. In the data from both Stanbury 29 and Lemann 27, this means that there is no apparent adaptive mechanism that improves phosphorus absorption at low intakes. This is in sharp contrast to calcium, for which absorption efficiency increases as dietary intake decreases 32 and for which adaptive mechanisms exist that improve absorption still further at habitual low intakes 33. The fact that fractional phosphorus absorption is virtually constant across a broad range of intakes suggests that the bulk of phosphorus absorption occurs by passive, concentration-dependent processes. Also, even in the face of dangerous hyperphosphatemia, phosphorus continues to be absorbed from the diet at an efficiency only slightly lower than normal 34.
Phosphorus absorption is reduced by ingestion of aluminum-containing antacids and by pharmacologic doses of calcium carbonate. There is, however, no significant interference with phosphorus absorption by calcium at intakes within the typical adult range.
In the healthy adult, urine phosphorus is essentially equal to absorbed diet phosphorus, less small amounts of phosphorus lost in shed cells of skin and intestinal mucosa 35, 27, 28.
This regulation of phosphorus excretion is apparent from early infancy. In infants, as in adults, the major site of regulation of phosphorus retention is at the kidney. In studies of infants receiving different calcium intakes 36, 37, 38, 31, phosphorus retention did not differ even with high amounts of dietary calcium (calcium:phosphorus [Ca:P] molar ratios of 0:6, 1:1, or 1.4:1). Any reduction in absorption of phosphorus due to high amounts of dietary calcium were compensated for by parallel reductions in renal phosphorus excretion 36, 39, 37. The least renal excretory work to maintain normal phosphorus homeostasis would be achieved with human milk as the major source of minerals during the first year of life.
Phosphorus interactions with medications
Phosphorus can interact with certain medications, and some medications can have an adverse effect on phosphate levels. Two examples are provided below. Individuals taking these and other medications on a regular basis should discuss their phosphorus status with their healthcare providers.
Antacids
Antacids that contain aluminum hydroxide, such as Maalox HRF and Rulox, bind phosphorus in the intestines, and their chronic use for 3 months or longer can therefore lead to hypophosphatemia 40. These drugs can also aggravate existing phosphate deficiency. Antacids containing calcium carbonate (Rolaids, Tums, Maalox) also decrease instestinal absorption of dietary phosphorus 41.
Laxatives
Some laxatives, such as Fleet Prep Kit #1, contain sodium phosphate, and ingesting these products can increase serum phosphate levels 42. After 13 reports of deaths associated with taking one dose that was higher than recommended on the label of a laxative containing sodium phosphate, the FDA issued a warning that these products are potentially dangerous if more than recommended doses are taken, especially in people with kidney disease, heart disease, or dehydration 43.
How much phosphorus do I need?
How much phosphorus you need depends on your age. Average daily recommended amounts are listed below in milligrams (mg).
According to Institute of Medicine recommendations, the recommended dietary intakes of phosphorus are as follows:
Table 2. Recommended Dietary Allowances (RDAs) for Phosphorus
| Age | Male | Female | Pregnancy | Lactation |
| Birth to 6 months* | 100 mg | 100 mg | ||
| 7–12 months* | 275 mg | 275 mg | ||
| 1–3 years | 460 mg | 460 mg | ||
| 4–8 years | 500 mg | 500 mg | ||
| 9–13 years | 1,250 mg | 1,250 mg | ||
| 14–18 years | 1,250 mg | 1,250 mg | 1,250 mg | 1,250 mg |
| 19+ years | 700 mg | 700 mg | 700 mg | 700 mg |
Footnotes:
- Recommended Dietary Allowance (RDA): Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- Adequate Intake (AI): Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an Recommended Dietary Allowance (RDA).
Phosphorus deficiency
Phosphorus deficiency (hypophosphatemia) is rare in the United States and is almost never the result of low dietary intakes 2. The effects of hypophosphatemia can include anorexia, anemia, proximal muscle weakness, skeletal effects (bone pain, rickets, and osteomalacia), increased infection risk, paresthesias (pins-and-needles sensation), ataxia (impaired balance or coordination) and confusion 2. In most cases, hypophosphatemia is caused by medical conditions, such as hyperparathyroidism, kidney tubule defects, and diabetic ketoacidosis 44.
Groups at risk of phosphorus inadequacy
The following groups are most likely to have inadequate phosphorus status.
Preterm newborns
Phosphorus deficiency in preterm infants is one of the main causes, along with calcium deficiency, of osteopenia of prematurity (impaired bone mineralization) 45. Because two-thirds of fetal bone mineral content is acquired during the third trimester of pregnancy, preterm infants are born with low stores of calcium and phosphorus in their bones 46. The benefits of providing extra phosphorus and calcium for bone health in preterm babies is not clear. However, milk fortified with higher amounts of these minerals and other nutritional components is typically recommended to support overall growth and development 47.
People with genetic phosphate regulation disorders
Rare genetic disorders of phosphorus metabolism include X-linked hypophosphatemic rickets 48. In addition to rickets, patients with this disease develop osteomalacia, pseudofractures (formation of new bone and thickened connective tissue over injured bone), enthesopathy (mineralization of ligaments and tendons), and dental damage. Other rare genetic disorders of phosphorus regulation associated with rickets include autosomal-dominant and autosomal-recessive hypophosphatemic rickets and hereditary hypophosphatemic rickets with hypercalciuria 49. Treatment typically consists of vitamin D and phosphorus supplementation from diagnosis until growth is complete 50.
Patients with severe malnutrition
People with severe protein or calorie malnutrition can develop refeeding syndrome, also known as refeeding hypophosphatemia, within 2 to 5 days of starting enteral or parenteral nutrition because of the shift in metabolism from a catabolic to an anabolic state 51. Causes of malnutrition that can lead to refeeding syndrome include chronic diseases (e.g., cancer, chronic obstructive pulmonary disease, or cirrhosis), very low birthweight, cachexia, low body weight, anorexia nervosa, excessive alcohol intake, and chewing or swallowing problems. The effects of refeeding syndrome can include impaired neuromuscular function, hypoventilation, respiratory failure, impaired blood clotting, confusion, coma, cardiac arrest, congestive heart failure, and death 51. Prophylactic administration of phosphorus and thiamin in patients at risk of refeeding syndrome can prevent this condition 51.
Excessive phosphorus health risks
High phosphorus intakes rarely produce adverse effects in healthy people 7. Although some studies have found associations between high phosphorus intakes (1,000 mg/day or higher) and cardiovascular, kidney, and bone adverse effects as well as an increased risk of death 52, 53, 54, others have found no link between high intakes and increased disease risk 55, 56. The Tolerable Upper Intake Levels (ULs) for phosphorus from food and supplements for healthy individuals are therefore based on intakes associated with normal serum phosphate concentrations 8 . The Tolerable Upper Intake Levels (ULs) do not apply to individuals who are receiving supplemental phosphorus under medical supervision.
According to one analysis of data on healthy U.S. adults using National Health and Nutrition Examination Survey (NHANES) III data collected in 1988–1994, high phosphorus intakes (1,000 mg/day or more) were associated with increased rates of all-cause and cardiovascular mortality in adults through 2006 52. These intakes are twice the RDA for adults—less than daily intakes in many men (especially those who are white or Hispanic) and well below the Tolerable Upper Intake Level. The implications of this analysis for the potential adverse effects of high phosphorus intakes are unclear. High phosphorus intakes might be signs of diets that are unhealthy in other ways, for example 52.
Very high phosphorus intakes over short periods (e.g., two 6,600 mg doses of sodium phosphate taken in one day) can cause hyperphosphatemia 57. The main effects of hyperphosphatemia include changes in the hormones that regulate calcium metabolism and calcification of nonskeletal tissues, especially in the kidney 8.
Table 3. Tolerable Upper Intake Levels (ULs) for Phosphorus
| Age | Male | Female | Pregnancy | Lactation |
| Birth to 6 months* | None established* | None established* | ||
| 7–12 months* | None established* | None established* | ||
| 1–3 years | 3,000 mg | 3,000 mg | ||
| 4–8 years | 3,000 mg | 3,000 mg | ||
| 9–13 years | 4,000 mg | 4,000 mg | ||
| 14–18 years | 4,000 mg | 4,000 mg | 3,500 mg | 4,000 mg |
| 19–50 years | 4,000 mg | 4,000 mg | 3,500 mg | 4,000 mg |
| 51–70 years | 4,000 mg | 4,000 mg | ||
| 71+ years | 3,000 mg | 3,000 mg |
Footnote: * Breast milk, formula, and food should be the only sources of phosphorus for infants.
[Source 8 ]Chronic kidney disease
Chronic kidney disease (CKD) means your kidneys are damaged and can’t filter blood the way they should. The disease is called “chronic” because the damage to your kidneys happens slowly over a long period of time. This damage can cause wastes to build up in your body. Chronic kidney disease (CKD), which affects 5%–10% of the population worldwide, can lead to cardiovascular disease and early death 58. As kidney function declines, phosphate excretion becomes less efficient and serum phosphate concentration rises. As a result, parathyroid hormone (PTH) and fibroblast growth factor 23 (FGF23) lose their ability to suppress phosphorus resorption by the kidneys 59.
Increased phosphorus retention often leads to chronic kidney disease (CKD) mineral and bone disorder. This systemic condition is characterized by abnormal metabolism of phosphorus, calcium, PTH, and/or vitamin D; abnormal bone turnover, mineralization, volume, growth, or strength; and vascular or other soft-tissue calcification 60.
An analysis of 2003–2006 National Health and Nutrition Examination Survey (NHANES) data illustrates the association between chronic kidney disease (CKD) and phosphate levels. In 7,895 adults (mean age 47 years, 52% Caucasian), participants with moderately reduced kidney function had significantly higher serum phosphate levels (4.12 ml/dL) than those with normal kidney function (3.74 mg/dL) 61.
Several studies have shown an increased risk of mortality or disease progression in patients who have chronic kidney disease (CKD) and high phosphate levels 62, 63. A meta-analysis of 9 cohort studies in 199,289 patients aged 50–73 years with end-stage renal disease (ESRD) showed, for example, that patients on dialysis with the highest phosphate levels (greater than 5.2–7.5 mg/dL, depending on the study) had a 39% greater risk of all-cause mortality during 12 to 97.6 months of follow-up than those with normal phosphate levels (defined in the analysis as 3.0–5.5 mg/dL, depending on the study) 64.
However, high phosphate levels do not seem to have the same associations in people with milder chronic kidney disease (CKD) 65, 66. For example, an analysis of NHANES III (1988-1994) data on 1,105 adults (mean age 67–71 years, depending on their phosphate intake tertile) with moderate chronic kidney disease (CKD) found that serum phosphate levels were very similar, regardless of phosphate intake—3.6 mg/dL in the lowest tertile of phosphorus intake (532 mg/day) and 3.5 mg/dL in the highest intake tertile (1,478 mg/day)—and that high phosphorus intakes were not associated with increased mortality rates over 6–12 years, possibly because these patients did not have severe chronic kidney disease (CKD) 66.
To prevent the complications of high phosphate levels in patients with chronic kidney disease (CKD), clinicians sometimes encourage patients to limit their phosphorus intakes (e.g., by replacing most animal proteins in their diets with plant-based protein sources, whose phosphorus is less bioavailable) and eat more calcium-rich foods 67. Some evidence shows that replacing foods containing phosphorus additives with foods that lack these additives can reduce serum phosphate levels 68. However, restricting phosphorus intakes can also reduce protein intakes because many foods (e.g., fish, meats, and legumes) containing large amounts of phosphorus also contain large amounts of protein 69. Furthermore, a Cochrane review of nine studies in 634 participants with chronic kidney disease (CKD) followed for 1–18 months found only limited, low-quality evidence indicating that dietary interventions might have a positive impact on chronic kidney disease (CKD) mineral and bone disorder 59.
In its clinical practice guideline for chronic kidney disease (CKD) mineral and bone disorder, the “Kidney Disease: Improving Global Outcomes” guidelines development group recommends that patients with stage 3–5 (more severe) chronic kidney disease (CKD) limit dietary phosphorus intake either alone or in combination with other treatments to reduce phosphate levels 70. However, the group notes that clinical trial data showing that treatments that lower serum phosphate levels improve patient-centered outcomes are lacking, and it acknowledges that this recommendation is weak.
Additional studies are needed on the link between phosphate concentrations and both chronic kidney disease (CKD) risk and morbidity in patients with chronic kidney disease (CKD) as well as the impact of dietary phosphorus restriction in patients with this disease.
Cardiovascular disease
Several observational studies support a link between high phosphate levels and cardiovascular disease risk in people with and without a history of cardiovascular disease 71, 72. For example, an analysis of 14,675 participants (55% women) without atrial fibrillation found, based on almost 20 years of follow-up, that each 1 mg/dL increase in serum phosphate was associated with a 13% higher risk of atrial fibrillation 73.
Several large epidemiologic studies have also found associations between higher serum phosphate concentrations and risk of cardiovascular mortality in healthy adults. A meta-analysis of data from four prospective cohort studies with 13,515 participants (with percentages of male participants ranging, depending on the study, from 44 to 100% and mean ages from 43 to 74 years) followed for 6–29 years showed a 36% higher risk of cardiovascular mortality in those with the highest phosphate concentration (2.79–4.0 mg/dL) compared with participants with a phosphate concentration of 0.61–3.28 mg/dL 74. A subsequent study not included in this meta-analysis in 13,165 nonpregnant adult participants (mean age 43–45 years, 52% female) in NHANES III (1988–1994) followed for a median of 14.3 years found that for every 1 mg/dL increase in phosphate above 3.5 mg/dL, the risk of death rose by 35% and the risk of cardiovascular death increased by 45% 75.
Not all observational data, however, support a link between serum phosphate concentrations and cardiovascular disease risk. A post hoc analysis of data from 7,269 postmenopausal women, mean age 66 years, with osteoporosis found no association between higher serum phosphate levels and risk of cardiovascular outcomes during 4 years of follow-up 76.
In spite of the evidence supporting a link between increased phosphate levels and cardiovascular disease risk, the literature offers no evidence on whether restricting phosphorus consumption can prevent cardiovascular disease in healthy adults 77. Additional research is needed to address this issue.
References- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington (DC): National Academies Press (US); 1997. 5, Phosphorus. Available from: https://www.ncbi.nlm.nih.gov/books/NBK109813
- Heaney RP. Phosphorus. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:447-58.
- Fomon SJ, Nelson SE. Calcium, phosphorus, magnesium, and sulfur. In: Fomon SJ, editor. Nutrition of Normal Infants. St. Louis: Mosby-Year Book, Inc.; 1993. pp. 192–216.
- Aloia JF, Vaswani AN, Yeh JK, Ellis K, Cohn SH. Total body phosphorus in postmenospausal women. Miner Electrolyte Metab. 1984;10:73–76. https://www.ncbi.nlm.nih.gov/pubmed/6700565
- Diem K. Documenta Geigy. Ardsley, NY: Geigy Pharmaceuticals; 1970.
- U.S. National Library of Medicine, MedlinePlus. Phosphorus in diet. https://medlineplus.gov/ency/article/002424.htm
- Phosphorus. https://ods.od.nih.gov/factsheets/Phosphorus-HealthProfessional
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academies Press; 1997.
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2015. Scientific Opinion on Dietary Reference Values for phosphorus. EFSA Journal 2015; 13( 7):4185, 54 pp. doi:10.2903/j.efsa.2015.4185
- Trautvetter U, Ditscheid B, Jahreis G, Glei M. Habitual Intakes, Food Sources and Excretions of Phosphorus and Calcium in Three German Study Collectives. Nutrients. 2018 Feb 2;10(2):171. doi: 10.3390/nu10020171
- Anderson, J., Adatorwovor, R., Roggenkamp, K., & Suchindran, C. M. (2017). Lack of Influence of Calcium/Phosphorus Ratio on Hip and Lumbar Bone Mineral Density in Older Americans: NHANES 2005-2006 Cross-Sectional Data. Journal of the Endocrine Society, 1(5), 407–414. https://doi.org/10.1210/js.2016-1077
- Trautvetter U, Jahreis G, Kiehntopf M, Glei M. Consequences of a high phosphorus intake on mineral metabolism and bone remodeling in dependence of calcium intake in healthy subjects – a randomized placebo-controlled human intervention study. Nutr J. 2016 Jan 19;15:7. doi: 10.1186/s12937-016-0125-5
- Calvo, M. S., & Lamberg-Allardt, C. J. (2015). Phosphorus. Advances in nutrition (Bethesda, Md.), 6(6), 860–862. https://doi.org/10.3945/an.115.008516
- Calvo MS, Sherman RA, Uribarri J. Dietary Phosphate and the Forgotten Kidney Patient: A Critical Need for FDA Regulatory Action. Am J Kidney Dis. 2019 Apr;73(4):542-551. doi: 10.1053/j.ajkd.2018.11.004
- Lindsay A. L. Bazydlo, PhD, Marisa Needham, PhD, Neil S. Harris, MD, Calcium, Magnesium, and Phosphate, Laboratory Medicine, Volume 45, Issue 1, February 2014, Pages e44–e50, https://doi.org/10.1309/LMGLMZ8CIYMFNOGX
- Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. https://www.ncbi.nlm.nih.gov/books/NBK109813
- Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. https://www.ncbi.nlm.nih.gov/books/NBK109813/
- Moshfegh AJ, Kovalchik AF, Clemens JC. Phosphorus Intake of Americans: What We Eat in American, NHANES 2011-2012. Food Surveys Research Group Dietary Data Brief No. 15. 2016. https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/DBrief/15_Phosphorus_intake_1112.pdf
- Calvo MS, Uribarri J. The Regulatory Aspects of Phosphorus Intake: Dietary Guidelines and Labeling. In: Uribarri J, Calvo MS, eds. Dietary Phosphorus: Health, Nutrition, and Regulatory Aspects. Boca Raton, Florida: CRC Press; 2018:249-66.
- Heaney RP, Nordin BE. Calcium effects on phosphorus absorption: implications for the prevention and co-therapy of osteoporosis. J Am Coll Nutr. 2002 Jun;21(3):239-44. doi: 10.1080/07315724.2002.10719216
- León JB, Sullivan CM, Sehgal AR. The prevalence of phosphorus-containing food additives in top-selling foods in grocery stores. J Ren Nutr. 2013 Jul;23(4):265-270.e2. doi: 10.1053/j.jrn.2012.12.003
- Calvo MS, Uribarri J. Contributions to total phosphorus intake: all sources considered. Semin Dial. 2013 Jan-Feb;26(1):54-61. doi: 10.1111/sdi.12042
- Itkonen ST, Karp HJ, Lamberg-Allardt CJ. Bioavailability of phosphorus. In: Uribarri J, Calvo MS, eds. Dietary Phosphorus: Health, Nutrition, and Regulatory Aspects. Boca Raton, Florida: CRC Press; 2018:221-33.
- Calvo MS, Uribarri J. Phosphorus in the modern food supply: Underestimation of exposure. In: Gutierrez OM, Kalantar-Zadeh K, Mehrotra R, eds. Clinical Aspects of Natural and Added Phosphorus in Foods. New York, New York: Springer-Verlag; 2017:47-76.
- Scanni R, vonRotz M, Jehle S, Hulter HN, Krapf R. The human response to acute enteral and parenteral phosphate loads. J Am Soc Nephrol. 2014 Dec;25(12):2730-9. doi: 10.1681/ASN.2013101076
- U.S. Department of Agriculture. https://fdc.nal.usda.gov
- Lemann J Jr. Calcium and phosphate metabolism: An overview in health and in calcium stone formers. In: Coe FL, Favus MJ, Pak CY, Parks JH, Preminger GM, editors. Kidney Stones: Medical and Surgical Management. Philadelphia, PA: Lippincott-Raven; 1996. pp. 259–288.
- Nordin BEC. Phosphorus. J Food Nutr. 1989;45:62–75.
- Stanbury SW. The phosphate ion in chronic renal failure. In: Hioco DJ, editor. Phosphate et Metabolisme Phosphocalcique. Paris: Sandoz Laboratories; 1971.
- Wilkinson R. Absorption of calcium, phosphorus, and magnesium. In: Nordin BEC, editor. Calcium, Phosphate and Magnesium Metabolism. Edinburgh: Churchill Livingstone; 1976. pp. 36–112.
- Ziegler EE, Fomon SJ. Lactose enhances mineral absorption in infancy. J Pediatr Gastroenterol Nutr. 1983;2:228–294.
- Heaney RP, Weaver CM, Fitzsimmons ML. Influence of calcium load on absorption fraction. J Bone Miner Res. 1990;5:1135–1138. https://www.ncbi.nlm.nih.gov/pubmed/2270776
- Heaney RP, Recker RR, Stegman MR, Moy AJ. Calcium absorption in women: Relationships to calcium intake, estrogen status, and age. J Bone Miner Res. 1989;4:469–475. https://www.ncbi.nlm.nih.gov/pubmed/2816496
- Brickman AS, Coburn JW, Massry SG. 1,25 dihydroxy-vitamin D3 in normal man and patients with renal failure. Ann Intern Med. 1974;80:161–168. https://www.ncbi.nlm.nih.gov/pubmed/4359739
- Bijvoet OLM. Relation of plasma phosphate concentration to renal tubular reabsorption of phosphate. Clin Sci. 1969;37:23–26.
- DeVizia B, Fomon SJ, Nelson SE, Edwards BE, Zeigler EE. Effect of dietary calcium on metabolic balance of normal infants. Pediatr Res. 1985;19:800–806. https://www.ncbi.nlm.nih.gov/pubmed/4034282
- Moya M, Cortes E, Ballester MI, Vento M, Juste M. Short-term polycose substitution for lactose reduces calcium absorption in healthy term babies. J Pediatr Gastroenterol Nutr. 1992;14:57–61. https://www.ncbi.nlm.nih.gov/pubmed/1573514
- Williams ML, Rose CS, Morrow G, Sloan SE, Barness LA. Calcium and fat absorption in neonatal period. Am J Clin Nutr. 1970;23:1322–1330. https://www.ncbi.nlm.nih.gov/pubmed/5536290
- Fomon SJ, Nelson SE. Calcium, phosphorus, magnesium, and sulfur. In: Fomon SJ, editor. Nutrition of Normal Infants. St. Louis: Mosby-Year Book, Inc.; 1993. pp. 192–216.
- Chines A, Pacifici R. Antacid and sucralfate-induced hypophosphatemic osteomalacia: a case report and review of the literature. Calcif Tissue Int. 1990 Nov;47(5):291-5. doi: 10.1007/BF02555911
- Ruospo M, Palmer SC, Natale P, Craig JC, Vecchio M, Elder GJ, Strippoli GF. Phosphate binders for preventing and treating chronic kidney disease-mineral and bone disorder (CKD-MBD). Cochrane Database Syst Rev. 2018 Aug 22;8(8):CD006023. doi: 10.1002/14651858.CD006023.pub3
- Casais MN, Rosa-Diez G, Pérez S, Mansilla EN, Bravo S, Bonofiglio FC. Hyperphosphatemia after sodium phosphate laxatives in low risk patients: prospective study. World J Gastroenterol. 2009 Dec 21;15(47):5960-5. doi: 10.3748/wjg.15.5960
- FDA Drug Safety Communication: FDA warns of possible harm from exceeding recommended dose of over-the-counter sodium phosphate products to treat constipation. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-possible-harm-exceeding-recommended-dose-over-counter-sodium
- Hruska K. Overview of phosphorus homeostasis. In: Gutierrez OM, Kalantar-Zadeh K, Mehrotra R, eds. Clinical Aspects of Natural and Added Phosphorus in Foods. New York, New York: Springer-Verlag; 2017:11-28.
- Karpen HE. Mineral Homeostasis and Effects on Bone Mineralization in the Preterm Neonate. Clin Perinatol. 2018 Mar;45(1):129-141. doi: 10.1016/j.clp.2017.11.005
- Harding JE, Wilson J, Brown J. Calcium and phosphorus supplementation of human milk for preterm infants. Cochrane Database Syst Rev. 2017 Feb 26;2(2):CD003310. doi: 10.1002/14651858.CD003310.pub2
- Abrams SA. In utero physiology: role in nutrient delivery and fetal development for calcium, phosphorus, and vitamin D. Am J Clin Nutr. 2007 Feb;85(2):604S-607S. doi: 10.1093/ajcn/85.2.604S
- de Menezes Filho H, de Castro LC, Damiani D. Hypophosphatemic rickets and osteomalacia. Arq Bras Endocrinol Metabol. 2006 Aug;50(4):802-13. doi: 10.1590/s0004-27302006000400025
- Gattineni J, Baum M. Genetic disorders of phosphate regulation. Pediatr Nephrol. 2012 Sep;27(9):1477-87. doi: 10.1007/s00467-012-2103-2
- Pavone V, Testa G, Gioitta Iachino S, Evola FR, Avondo S, Sessa G. Hypophosphatemic rickets: etiology, clinical features and treatment. Eur J Orthop Surg Traumatol. 2015 Feb;25(2):221-6. doi: 10.1007/s00590-014-1496-y
- Friedli N, Stanga Z, Culkin A, Crook M, Laviano A, Sobotka L, Kressig RW, Kondrup J, Mueller B, Schuetz P. Management and prevention of refeeding syndrome in medical inpatients: An evidence-based and consensus-supported algorithm. Nutrition. 2018 Mar;47:13-20. doi: 10.1016/j.nut.2017.09.007
- Chang, A. R., Lazo, M., Appel, L. J., Gutiérrez, O. M., & Grams, M. E. (2014). High dietary phosphorus intake is associated with all-cause mortality: results from NHANES III. The American journal of clinical nutrition, 99(2), 320–327. https://doi.org/10.3945/ajcn.113.073148
- Gutiérrez OM, Luzuriaga-McPherson A, Lin Y, Gilbert LC, Ha SW, Beck GR Jr. Impact of Phosphorus-Based Food Additives on Bone and Mineral Metabolism. J Clin Endocrinol Metab. 2015 Nov;100(11):4264-71. doi: 10.1210/jc.2015-2279
- Ito S, Ishida H, Uenishi K, Murakami K, Sasaki S. The relationship between habitual dietary phosphorus and calcium intake, and bone mineral density in young Japanese women: a cross-sectional study. Asia Pac J Clin Nutr. 2011;20(3):411-7.
- Chang, A. R., Miller, E. R., 3rd, Anderson, C. A., Juraschek, S. P., Moser, M., White, K., Henry, B., Krekel, C., Oh, S., Charleston, J., & Appel, L. J. (2017). Phosphorus Additives and Albuminuria in Early Stages of CKD: A Randomized Controlled Trial. American journal of kidney diseases : the official journal of the National Kidney Foundation, 69(2), 200–209. https://doi.org/10.1053/j.ajkd.2016.08.029
- Lee KJ, Kim KS, Kim HN, et al. Association between dietary calcium and phosphorus intakes, dietary calcium/phosphorus ratio and bone mass in the Korean population. Nutr J 2014;13:114.
- Malberti F. Hyperphosphataemia: treatment options. Drugs. 2013 May;73(7):673-88. doi: 10.1007/s40265-013-0054-y
- Moe SM, Drüeke T, Lameire N, Eknoyan G. Chronic kidney disease-mineral-bone disorder: a new paradigm. Adv Chronic Kidney Dis. 2007 Jan;14(1):3-12. doi: 10.1053/j.ackd.2006.10.005
- Liu Z, Su G, Guo X, Wu Y, Liu X, Zou C, Zhang L, Yang Q, Xu Y, Ma W. Dietary interventions for mineral and bone disorder in people with chronic kidney disease. Cochrane Database Syst Rev. 2015 Sep 16;(9):CD010350. doi: 10.1002/14651858.CD010350.pub2
- Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G; Kidney Disease: Improving Global Outcomes (KDIGO). Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2006 Jun;69(11):1945-53. doi: 10.1038/sj.ki.5000414
- Moore LW, Nolte JV, Gaber AO, Suki WN. Association of dietary phosphate and serum phosphorus concentration by levels of kidney function. Am J Clin Nutr. 2015 Aug;102(2):444-53. doi: 10.3945/ajcn.114.102715
- Da J, Xie X, Wolf M, Disthabanchong S, Wang J, Zha Y, Lv J, Zhang L, Wang H. Serum Phosphorus and Progression of CKD and Mortality: A Meta-analysis of Cohort Studies. Am J Kidney Dis. 2015 Aug;66(2):258-65. doi: 10.1053/j.ajkd.2015.01.009
- Cheungpasitporn W, Thongprayoon C, Mao MA, Kittanamongkolchai W, Sakhuja A, Erickson SB. Admission serum phosphate levels predict hospital mortality. Hosp Pract (1995). 2018 Aug;46(3):121-127. doi: 10.1080/21548331.2018.1483172
- Hou Y, Li X, Sun L, Qu Z, Jiang L, Du Y. Phosphorus and mortality risk in end-stage renal disease: A meta-analysis. Clin Chim Acta. 2017 Nov;474:108-113. doi: 10.1016/j.cca.2017.09.005
- Selamet U, Tighiouart H, Sarnak MJ, Beck G, Levey AS, Block G, Ix JH. Relationship of dietary phosphate intake with risk of end-stage renal disease and mortality in chronic kidney disease stages 3-5: The Modification of Diet in Renal Disease Study. Kidney Int. 2016 Jan;89(1):176-84. doi: 10.1038/ki.2015.284
- Murtaugh MA, Filipowicz R, Baird BC, Wei G, Greene T, Beddhu S. Dietary phosphorus intake and mortality in moderate chronic kidney disease: NHANES III. Nephrol Dial Transplant. 2012 Mar;27(3):990-6. doi: 10.1093/ndt/gfr367
- Moorthi RN, Moe SM. Special nutritional needs of chronic kidney disease and end-stage renal disease patients: rationale for the use of plant-based diets. In: Uribarri J, Calvo MS, eds. Dietary Phosphorus: Health, Nutrition, and Regulatory Aspects. Boca Raton, Florida: CRC Press; 2018:235-46.
- de Fornasari ML, Dos Santos Sens YA. Replacing Phosphorus-Containing Food Additives With Foods Without Additives Reduces Phosphatemia in End-Stage Renal Disease Patients: A Randomized Clinical Trial. J Ren Nutr. 2017 Mar;27(2):97-105. doi: 10.1053/j.jrn.2016.08.009
- Shinaberger CS, Greenland S, Kopple JD, Van Wyck D, Mehrotra R, Kovesdy CP, Kalantar-Zadeh K. Is controlling phosphorus by decreasing dietary protein intake beneficial or harmful in persons with chronic kidney disease? Am J Clin Nutr. 2008 Dec;88(6):1511-8. doi: 10.3945/ajcn.2008.26665
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group (2017). KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney international supplements, 7(1), 1–59. https://doi.org/10.1016/j.kisu.2017.04.001
- Dhingra R, Sullivan LM, Fox CS, Wang TJ, D’Agostino RB Sr, Gaziano JM, Vasan RS. Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med. 2007 May 14;167(9):879-85. doi: 10.1001/archinte.167.9.879
- Tonelli M, Sacks F, Pfeffer M, Gao Z, Curhan G; Cholesterol And Recurrent Events Trial Investigators. Relation between serum phosphate level and cardiovascular event rate in people with coronary disease. Circulation. 2005 Oct 25;112(17):2627-33. doi: 10.1161/CIRCULATIONAHA.105.553198. Erratum in: Circulation. 2007 Dec 4;116(23):e556.
- Lopez FL, Agarwal SK, Grams ME, Loehr LR, Soliman EZ, Lutsey PL, Chen LY, Huxley RR, Alonso A. Relation of serum phosphorus levels to the incidence of atrial fibrillation (from the Atherosclerosis Risk In Communities [ARIC] study). Am J Cardiol. 2013 Mar 15;111(6):857-62. doi: 10.1016/j.amjcard.2012.11.045
- Bai W, Li J, Liu J. Serum phosphorus, cardiovascular and all-cause mortality in the general population: A meta-analysis. Clin Chim Acta. 2016 Oct 1;461:76-82. doi: 10.1016/j.cca.2016.07.020
- Chang AR, Grams ME. Serum phosphorus and mortality in the Third National Health and Nutrition Examination Survey (NHANES III): effect modification by fasting. Am J Kidney Dis. 2014 Oct;64(4):567-73. doi: 10.1053/j.ajkd.2014.04.028
- Slinin Y, Blackwell T, Ishani A, Cummings SR, Ensrud KE; MORE Investigators. Serum calcium, phosphorus and cardiovascular events in post-menopausal women. Int J Cardiol. 2011 Jun 16;149(3):335-40. doi: 10.1016/j.ijcard.2010.02.013
- Menon MC, Ix JH. Dietary phosphorus, serum phosphorus, and cardiovascular disease. Ann N Y Acad Sci. 2013 Oct;1301:21-6. doi: 10.1111/nyas.12283