Pickwickian syndrome
Pickwickian syndrome also known as “obesity-hypoventilation syndrome”, is a disorder that can occur in people with a combination of obesity (body mass index [BMI] ≥ 30 kg/m²) , sleep-disordered breathing and awake daytime hypercapnia (elevated carbon dioxide levels in your bloodstream [arterial carbon dioxide partial pressure or PaCO2] of greater than 45 mmHg) in the absence of significant lung or respiratory muscle disease 1, 2, 3, 4, 5. Pickwickian syndrome or obesity-hypoventilation syndrome is defined as the presence of awake alveolar hypoventilation characterized by daytime hypercapnia (arterial carbon dioxide partial pressure [PaCO2] greater than 45 mmHg) and hypoxia (arterial oxygen partial pressure [PaO2] less than 60-70 mm Hg) that is thought to be a consequence of diminished ventilatory drive and capacity related to obesity (body mass index [BMI] over 30 kg/m²) in the absence of an alternate respiratory, neuromuscular, or metabolic explanation for hypoventilation 1, 3, 6, 7, 8.
People who have Pickwickian syndrome or obesity-hypoventilation syndrome, hypoventilate, or breathe in a way that is too slow or too shallow to meet the needs of their body, not only at night, but during the day. As a result, they experience elevated carbon dioxide levels in the bloodstream, called hypercapnia. Currently, Pickwickian syndrome is more commonly referred to as obesity-hypoventilation syndrome (OHS) and the American Academy of Sleep Medicine discourages the term Pickwickian syndrome, as it has also been used to describe people with only obesity or obstructive sleep apnea, not obesity hypoventilation syndrome 9. Pickwickian syndrome or obesity-hypoventilation syndrome is the most severe form of obesity-induced respiratory compromise and leads to serious complications, including increased rates of death and early death, chronic heart failure, pulmonary hypertension, hospitalization due to acute-on-chronic hypercapnic respiratory failure, poorer quality of life and higher health care expenses among others 10, 11, 12, 13.
In 1955, Auchincloss and colleagues 14, described in detail a patient with obesity-hypoventilation syndrome and the following year, Burwell and colleagues 15 compared patients with obesity-hypoventilation syndrome with an obese, somnolent Charles Dickens’ first novel character named Joe in “The Posthumous Papers of the Pickwick Club”, who was described as often falling asleep throughout the day and snoring as he sleeps 16.
Although Pickwickian syndrome or obesity hypoventilation syndrome can exist by itself, approximately 90% of patients with obesity hypoventilation syndrome (OHS) have coexistent obstructive sleep apnea (OSA). Obstructive sleep apnea (OSA) occurs when your breathing is interrupted during sleep due to partial airway obstruction, for longer than 10 seconds at least 5 times per hour (on average) throughout your sleep period. These periods are called hypopneas when your breathing is reduced by at least 50% that results in a decrease in your blood arterial oxygen saturation of 4% or more. They’re called apneas if your breathing completely stops or have almost no airflow. Your breathing typically stops because something is blocking your upper airway, such as the muscles, tongue, and other body tissues 17, 1. Obstructive sleep apnea (OSA) can range from moderate to severe, based on a measurement and rating system called the apnea-hypopnea index (AHI). The apnea-hypopnea index (AHI) measures an average number of apnea and hypopnea episodes that you experience per hour that you sleep. Obstructive sleep apnea is classified by severity:
- Severe obstructive sleep apnea means that your apnea-hypopnea index (AHI) is greater than 30 (more than 30 episodes per hour)
- Moderate obstructive sleep apnea means that your apnea-hypopnea index (AHI) is between 15 and 30 episodes per hour
- Mild obstructive sleep apnea means that your apnea-hypopnea index (AHI) is between 5 and 15 episodes per hour
Nearly 70% of Pickwickian syndrome or obesity hypoventilation syndrome (OHS) patients having severe obstructive sleep apnea (OSA) with apnea–hypopnea index (AHI) ≥ 30 events/hour 18. The remaining 10% of Pickwickian syndrome or obesity hypoventilation syndrome patients without obstructive sleep apnea (OSA) have an apnea–hypopnea index (AHI) less than 5 events/hour have nonobstructive, sleep-dependent hypoventilation 19, 7, 20, 21. The sleep-disordered breathing in this subset of patients has been labeled as nonobstructive sleep-dependent hypoventilation and is defined as an increase in PaCO2 during sleep by 10 mm Hg above wakefulness or significant oxygen desaturation that is not explained by obstructive apneas or hypopneas 1.
In a recent European Respiratory Society task force report, hypoventilation in obesity is now divided into five stages 2:
- Stage 0 encompasses the pure obstructive sleep apnea (OSA) population without evidence of nocturnal-only hypoventilation or daytime hypercapnia.
- In stages 1 and 2, only obesity-related sleep hypoventilation is present. Patients in stage 1 and 2 also have a bicarbonate level of less than 27 mmol/L or ≥ 27 mmol/L, respectively.
- Daytime hypercapnia is only present in the most advanced obesity hypoventilation syndrome stages of 3 and 4. Patients in stage 4 have concurrent comorbidities whereas those in stage 3 do not.
- Similar to patients with neuromuscular and chest wall restriction, it is believed that in patients with nocturnal hypoventilation without daytime hypercapnia, advanced obesity hypoventilation syndrome and diurnal hypercapnia may eventually develop 22, 23.
Obesity (body mass index (BMI) ≥30 kg/m²) and morbid obesity or “severe obesity” (class 3 obesity or body mass index (BMI) ≥ 40 kg/m²) is the hallmark of Pickwickian syndrome or obesity hypoventilation syndrome 24, 1, 25, 26, 27, 28. In recent decades, the prevalence of obesity and morbid obesity or “severe obesity” (class 3 obesity or body mass index (BMI) ≥ 40 kg/m²) has increased worldwide 29. The Centers for Disease Control and Prevention (CDC) estimated that 41.9% of the United States population suffers from obesity (BMI ≥30 kg/m²) and approximately 9.2% of the adult U.S. population has “severe obesity” with a BMI ≥40 kg/m² 30, 31. In addition, there is a growing global epidemic of obesity affecting all ages, including children, adolescents, and adults; hence the prevalence of obesity hypoventilation syndrome is also increasing in these age groups 3, 32, 33, 5.
The incidence rate of Pickwickian syndrome or obesity hypoventilation syndrome is seen at higher rates in men than in women, older individuals, and African Americans than in the White race population 20. However, among patients referred to the sleep disorders clinic, obesity hypoventilation syndrome was more prevalent in women than men 34. The delay in identifying obesity hypoventilation syndrome in women was linked to a worse and more advanced consequence of the disease 35. In addition, obesity hypoventilation syndrome is known to occur at a lower BMI range in the Asian community 36.
Because of the lack of studies on the prevalence of Pickwickian syndrome or obesity hypoventilation syndrome in the general population, Mokhlesi 37 infers that if approximately 3% of the general population in the USA are severely obese (BMI > 40 kg/m²), half of those individuals would have OSA. Considering, therefore, the estimate that 10-20% of severely obese patients with obstructive sleep apnea (OSA) would have obesity hypoventilation syndrome, a conservative estimate indicates a prevalence of obesity hypoventilation syndrome of 0.15-0.30% in the general population in the USA (ranging approximately from 1:300 to 1:600 adults) 37. Multiple studies have reported a prevalence of Pickwickian syndrome or obesity hypoventilation syndrome between 8% and 20% in obese patients referred to sleep centers for evaluation of sleep-disordered breathing 38, 39, 40, 41.
Signs of right heart failure can be present in Pickwickian syndrome or obesity hypoventilation syndrome and are secondary to chronic hypoxemia and pulmonary hypertension, both of which can accompany the clinical picture 3. In addition, arterial hypertension and insulin resistance are more prevalent in patients with obesity hypoventilation syndrome than in obese individuals without obesity hypoventilation syndrome 42, 25, 43.
Patients with obesity hypoventilation syndrome use more health care resources in the period prior to the diagnosis than do obese individuals without obesity hypoventilation syndrome or the general population 44. Obesity per se leads to a greater likelihood of diseases such as systemic arterial hypertension, diabetes, dyslipidemia, and hypothyroidism. Comorbidities such as heart failure, coronary artery disease, and right-sided heart failure (cor pulmonale) are more common in patients with obesity hypoventilation syndrome, and the likelihood that such patients will require invasive mechanical ventilation or ICU admission is also increased 28, 45. In addition, pulmonary hypertension is more common (50% vs. 15%) and more severe in patients with obesity hypoventilation syndrome than in patients with obstructive sleep apnea (OSA) 46, 47, 48.
Berg et al. 44 conducted a study involving 20 patients with obesity hypoventilation syndrome, who were matched to control subjects by age, gender, and zip code to try to equate socioeconomic factors. A comparison with controls revealed that the most common morbidities in patients with obesity hypoventilation syndrome were cardiovascular diseases: congestive heart failure; chest pain caused by reduced blood flow to the heart (angina pectoris) and right heart failure (cor pulmonale). In a retrospective study conducted by Basoglu & Tasbakan 25, having a BMI > 40 kg/m² and obesity-related complications showed a strong association with an increased risk of premature death in hospitalized patients. Nowbar et al. 28 reported that, at 18 months following hospital discharge, rate of death (mortality) was 23% in patients with obesity-related hypoventilation, which was almost twice as high as that among obese patients without hypoventilation.
Pickwickian syndrome is a diagnosis of exclusion after every other causes of alveolar hypoventilation such as severe obstructive or restrictive pulmonary disease, significant kyphoscoliosis, severe hypothyroidism, neuromuscular diseases, or other central hypoventilation syndromes is ruled out 1, 3. Patients can present both with an exacerbation of or a chronic state of progressive shortness of breath (dyspnea).
Unfortunately, the diagnosis of obesity hypoventilation syndrome is delayed in most cases, occurring during acute events of respiratory failure or cardiac decompensation 28, 49.
If you are diagnosed with obesity hypoventilation syndrome, your doctor may recommend healthy lifestyle changes, such as getting to and maintaining a healthy weight and being physically active. You may also need breathing assistance using special machines (mechanical ventilation) using continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) through a mask that fits tightly over the nose or nose and mouth (mainly for sleep) at night to help keep your airways open and increase blood oxygen levels. Other treatments may include weight-loss surgery or medicines.
If you have been prescribed a CPAP machine, use it as instructed and continue with your provider’s recommended healthy lifestyle changes to prevent complications. Tell your doctor about new symptoms, such as swelling around your ankles, chest pain, lightheadedness, or wheezing. Talk to your doctor if you will be flying or need surgery, because these situations can increase your risk for serious complications.
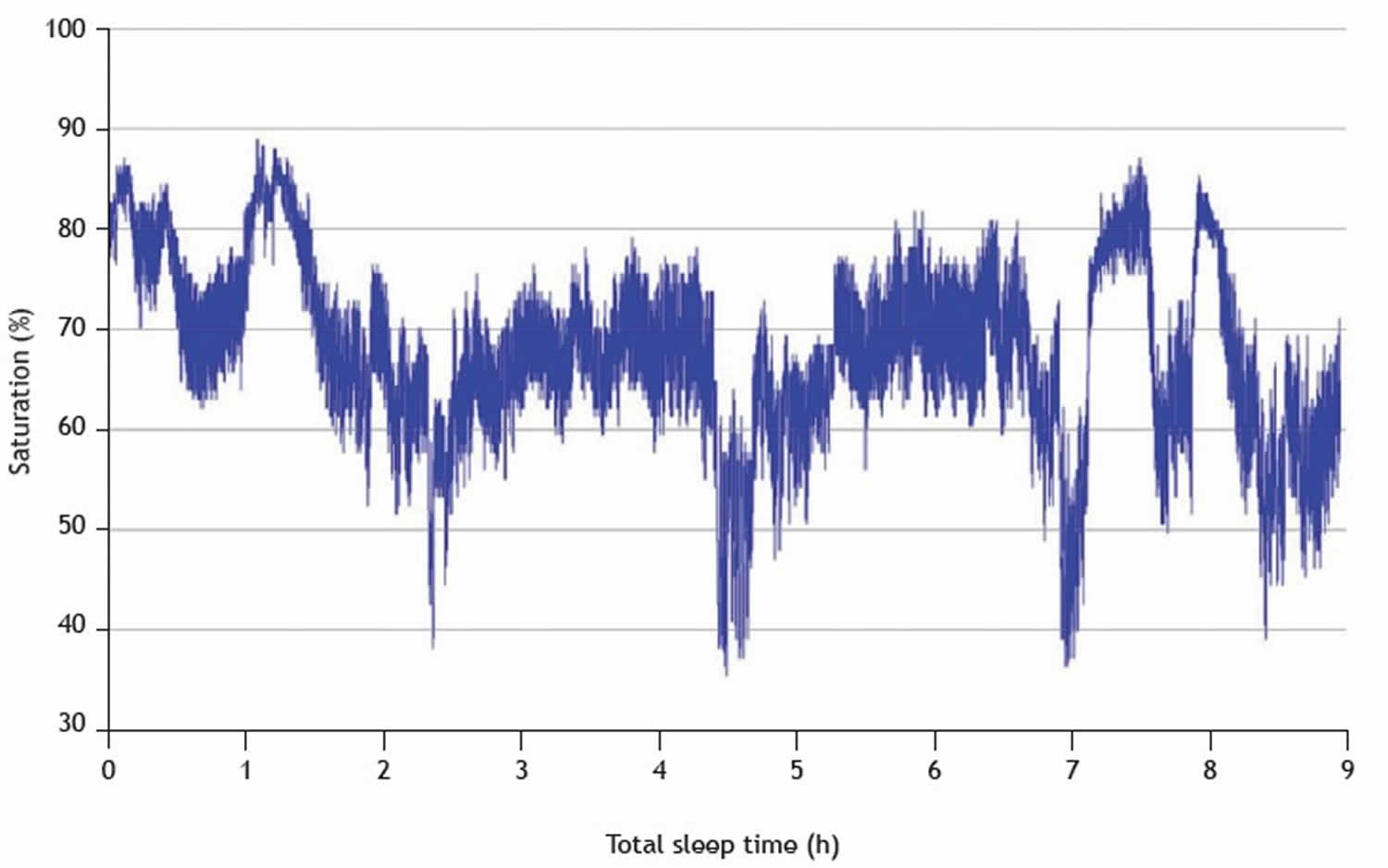
Figure 1. Pickwickian syndrome polysomnogram
Footnote: Female patient with a body mass index of 45 kg/m², PaCO2 = 55.6 mmHg, obstructive sleep apnea (OSA) and obesity hypoventilation syndrome presenting with persistent hypoxemia and frequent desaturations, which were more pronounced at three time points (at between 2 and 3 hours of sleep, at between 4 and 5 hours of sleep, and at 7 hours of sleep), suggestive of occurring during REM sleep.
[Source 3 ]Make an appointment with your doctor if you experience these symptoms:
- Extreme tiredness or sleepiness during the day. Having excessive daytime drowsiness, which may cause you to fall asleep while working, watching television or even driving a vehicle
- Loud snoring enough to disturb your sleep or that of others
- Gasping or choking during sleep
- Pauses in breathing during sleep
- Observed episodes of stopped breathing during sleep
- Suddenly waking from sleep with a snort
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Fatigue
- Mood changes, such as depression or irritability
- Morning headaches
- Slow thinking and difficulty concentrating
- Difficulty concentrating during the day
- High blood pressure
- Decreased libido
Loud snoring can indicate a potentially serious problem, but not everyone who has sleep apnea snores. Be sure to talk to your doctor if you snore loudly, especially if your snoring is interrupted by periods of silence. With obstructive sleep apnea, snoring usually is loudest when you sleep on your back, and it quiets when you turn on your side.
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness may be due to other disorders, such as narcolepsy.
Pickwickian syndrome causes
The exact cause of Pickwickian syndrome or obesity hypoventilation syndrome is not known. However, according to experts, Pickwickian syndrome or obesity hypoventilation syndrome stems from multiple complex processes in your body rather than a single, clear-cut cause. That said, obesity and and obstructive sleep apnea (OSA) often increase your risk of developing obesity hypoventilation syndrome, usually by making breathing more difficult. Most people who have obesity hypoventilation syndrome (OHS) also have obstructive sleep apnea (OSA). It is not clear why obesity hypoventilation syndrome affects some people who have obesity and not others. Extra fat around your neck, chest, or across your abdomen can make it difficult to breathe deeply and may produce hormone that affect your body’s breathing patterns. Being unable to fully breathe in deeply can lead to muscle weakness and reduced lung capacity over time. You may also have a problem with the way your brain controls your breathing. The excess body weight against yourchest wall also makes it harder for the muscles to draw in a deep breath and to breathe quickly enough. This worsens your brain’s breathing control. As a result, your blood contains too much carbon dioxide and not enough oxygen.
Other contributing factors involved in the cause of Pickwickian syndrome or obesity hypoventilation syndrome include ventilatory control defects leading to decreased responsiveness in the hypoxic and hypercapnic ventilatory drive 50. People with obesity hypoventilation syndrome do not experience the same respiratory drive in response to increased levels of carbon dioxide in the blood that most healthy people experience. Breathing in draws oxygen into your body and blood, and breathing out expels carbon dioxide. Because they have a decreased respiratory drive, people with obesity hypoventilation syndrome do not increase the amount they inhale and exhale enough to adequately decrease carbon dioxide levels in their blood. Researchers suspect this decreased respiratory drive could be due to the presence of certain genes, sleep-disordered breathing, or leptin resistance.
Leptin is a hormone created by fat tissue in the body, also called adipose tissue. In addition to helping people feel full and recognize when to stop eating, this hormone can stimulate breathing. When a person has leptin resistance, their leptin levels increase, but their body does not respond accordingly. That means people with obesity hypoventilation syndrome experience higher levels of leptin, but leptin resistance may keep their body from signaling when they feel full or need to breathe more.
Risk factors for Pickwickian syndrome
Other things that can raise your risk of Pickwickian syndrome or obesity hypoventilation syndrome include:
- Having a higher body mass index (BMI) increases a person’s risk of developing obesity hypoventilation syndrome. A person’s BMI is a number calculated using their height and weight (https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm). The National Heart, Lung, and Blood Institute defines obesity as having a BMI of 30 kg/m² or greater, with a BMI over 40 kg/m² considered severe obesity. Experts estimate that between 0.15% and 0.3% of adults with a BMI greater than 40 kg/m² have obesity hypoventilation syndrome.
- Obstructive sleep apnea (OSA) is another risk factor for obesity hypoventilation syndrome. Of people who have both OSA and obesity, 10% to 15% also have obesity hypoventilation syndrome.
- Obesity hypoventilation syndrome appears to be more common in certain groups of people, such as in men.
- Obesity hypoventilation syndrome also occurs more frequently among African Americans. In Asian communities, obesity hypoventilation syndrome appears to develop at a lower BMI than it does in other groups.
Pickwickian syndrome pathophysiology
Pickwickian syndrome or obesity hypoventilation syndrome occurs due to complex interactions between multiple pathological processes, including diminished respiratory drive, structural and functional respiratory impairment, and sleep-related breathing alterations 5. Chronic steady-state hypercapnia occurs due to the failure of compensatory ventilatory mechanisms 3, 51, 52, 53. Obesity-related increased CO2 production (VCO2) is an independent variable of arterial PaCO2 level, based on the alveolar ventilation (VA) equations: PaCO2=K VCO2/VA, (K is a constant ) and VA is minute ventilation (VE) minus dead space ventilation (VD) 5. In contrast, decreased alveolar ventilation due to any cause (obesity, atelectasis, or mechanical loading) leads to increased PaCO2.
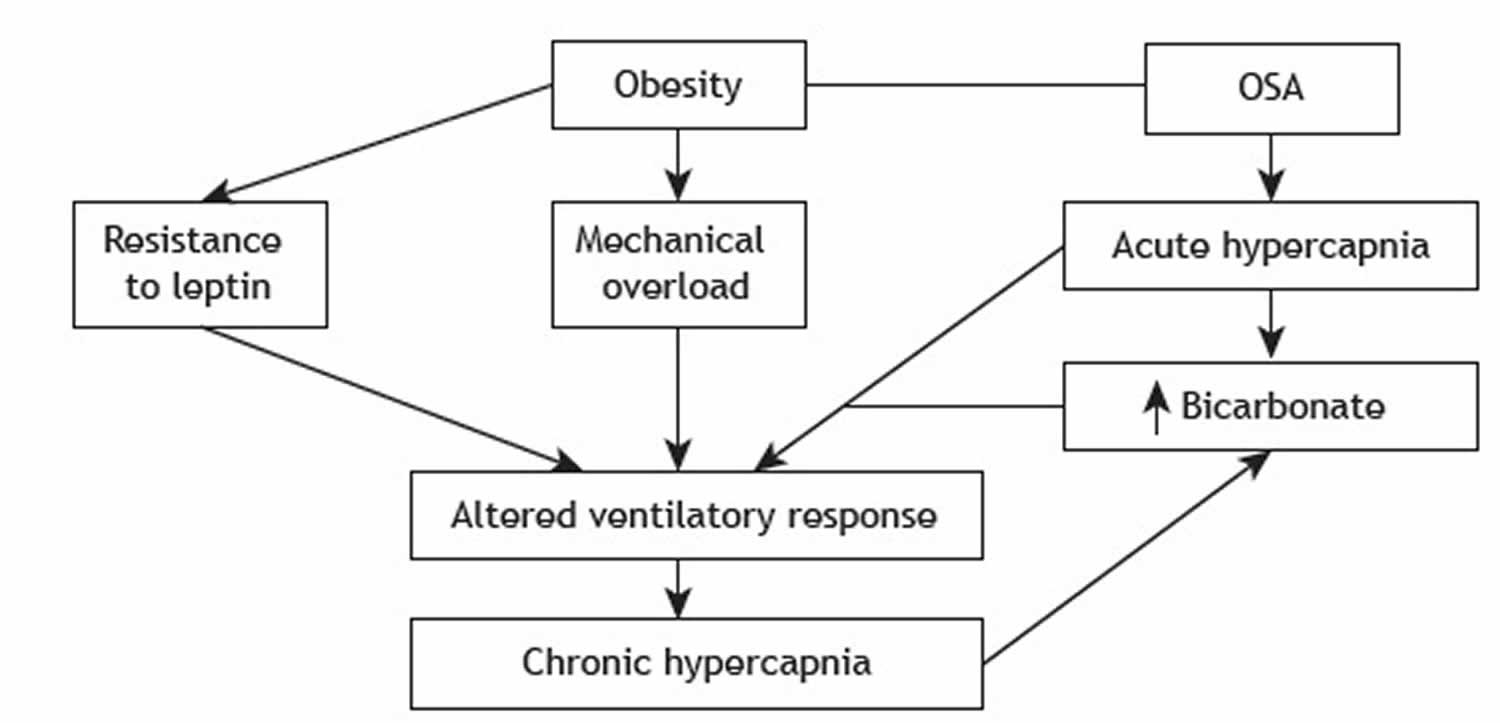
Figure 2. Pickwickian syndrome pathophysiology
Abbreviation: OSA = obstructive sleep apnea
[Source 3 ]Obesity
Respiratory system mechanics are affected significantly by obesity and fat distribution 54. The daily increase in PaCO2 in obese individuals was a strong respiratory determinant of hypercapnia in obesity hypoventilation syndrome 55. Furthermore, hypercapnic patients had significantly greater CO2 production as a cause for hypercapnia. However, when adjusting for body surface area, the CO2 production was similar between those with obstructive sleep apnea (OSA) and hypercapnia. They do not have hypercapnia (PaCO2 52 mmHg vs. 40 mmHg), matched for apnea-hypopnea index (AHI).
Impaired pulmonary mechanics
Respiratory muscles
The maximal inspiratory and expiratory pressures are reduced in patients with obesity hypoventilation syndrome while normal in morbidly obese patients with normal CO2 (eucapnic) or mild obesity hypoventilation syndrome 56, 57. In addition, patients with obesity hypoventilation syndrome who have hypercapnia could generate trans-diaphragmatic pressure similar to patients with obesity during hypercapnia-induced hyperventilation, suggesting that reduced ventilatory drive, not mechanical limitations, contribute to the pathogenesis of obesity hypoventilation syndrome 58.
Respiratory mechanics
Due to reduced pulmonary distensibility, obese patients suffer reduced ventilation in the lower pulmonary lobes 5. The alveoli close before the expiration, thus producing a characteristic breathing pattern of low tidal volume and an increased respiratory rate, causing an increase in the dead ventilation space. Decreased ventilation of the lower lobes causes alterations in the ventilation-perfusion (V/Q), thus triggering hypoxemia. Total lung capacity (TLC), expiratory reserve volume (ERV), and residual functional capacity (RFC) are reduced in patients with obesity hypoventilation syndrome as opposed to normal CO2 (eucapnic) obese patients 5.
Blunted respiratory drive
Patients with obesity hypoventilation syndrome have a blunted respiratory drive in response to a hypercapnic challenge 5. Multiple possible pathogenic mechanisms have been proposed to explain the blunted respiratory response, including possible leptin resistance, genetic predisposition, and sleep-disordered breathing.
Intrinsically diminished chemosensitivity to CO2 retention has been reported in obesity hypoventilation syndrome patients. It is possible that this diminished hypoxic and hypercapnic chemosensitivity could be the underlying reason for hypoventilation in patients with idiopathic obesity hypoventilation syndrome 5.
Leptin resistance
Leptin is a protein encoded by the ob (obese) gene discovered in 1994 59. Leptin is produced in the adipose tissue and regulates appetite, and stimulates ventilation 60. The excess fatty tissue associated with obesity leads to increasing levels of leptin which can prevent ventilatory depression 61. For leptin to increase ventilation, the level rises to compensate for increased respiratory demand 62. Therefore, patients with obesity hypoventilation syndrome and obstructive sleep apnea (OSA) have higher leptin levels and higher leptin resistance than matched control subjects without OSA 23. Likewise, compared with eupneic patients with obstructive sleep apnea (OSA), patients with obesity hypoventilation syndrome have higher serum levels of leptin 63. These elevated leptin levels drop after the treatment with positive airway pressure (PAP) 64.
Obstructive sleep apnea
An estimated 90% of patients with obesity hypoventilation syndrome have obstructive sleep apnea (OSA) (defined by an apnea-hypopnea index [AHI] ≥ 5 events/hour), and the majority (approximately 70%) are severe (AHI ≥ 30 events/hour) 18. However, 10% of obesity hypoventilation syndrome patients without obstructive sleep apnea (OSA) are due to sleep-related hypoventilation.
The PaCO2 increase is secondary to the cessation of ventilation during apneic events and the continued metabolic production of CO2. Normal CO2 (eucapnic) patients can normalize the PaCO2 levels via compensatory augmentation of alveolar ventilation, which increases CO2 clearance. However, in obesity hypoventilation syndrome patients, the compensatory mechanism is disrupted, causing the retention of CO2 4. In response to transitory hypercapnia, the renal system decreases bicarbonate clearance to compensate for the hypercapnic pH drop. This built-up in bicarbonate eventually blunts the ventilatory response to carbon dioxide, thus causing the development of nocturnal hypoventilation.
Sleep hypoventilation
Almost 5% to 10 % of patients with obesity hypoventilation syndrome have sleep hypoventilation and a PaCO2 elevation during sleep of 10 mm Hg or higher. These patients are clinically indistinguishable from those with concomitant OSA. Sustained hypoxia significantly delays the warning signals of decreased ventilation and could potentially contribute to hypoventilation.
Pickwickian syndrome prevention
To prevent obesity-hypoventilation syndrome, experts recommend making lifestyle changes in order to reduce body weight. Numerous studies have shown improvement in obesity hypoventilation syndrome symptoms with weight reduction 65. Weight loss significantly reduces CO2 production and improves sleep apnea severity and alveolar ventilation. It also improves pulmonary artery hypertension and left ventricular dysfunction, significantly reducing cardiovascular compromise in obesity hypoventilation syndrome patients 5.
Getting to and staying at a healthy weight involves finding a balance between food and activity. To lose weight, you need to take in fewer calories than you use up. Some ways to do this are:
- Eating more nutrient-rich foods, such as foods with lots of vitamins, minerals, and fiber.
- Eating and drinking less of the foods and beverages that have lots of calories, salt, sugar, and fat.
- Limiting alcohol.
- Finding healthier ways to cook, such as using healthier oils to cook with and baking or grilling instead of frying foods.
- Getting more physical activity. The general recommendation is for adults to get 150 minutes of physical activity each week, including:
- Aerobic activity, which is also called cardio. It uses your large muscle groups (chest, legs, and back) to speed up your heart rate and breathing.
- Muscle-strengthening activity, which is also called strength training. It works your muscles by making you push or pull against something.
You may decide to do these lifestyle changes on your own, or you may decide to try a weight-loss diet or program. Dietitians can help you with weight management Before you start, it’s important to check with your doctor first. Your doctor or dietitian can tell you what a healthy weight is for you, help you set goals, and give you tips on how to lose weight.
If making lifestyle changes or doing a weight-loss program are not enough to help you lose weight, your doctor may prescribe medicines. The prescription medicines to treat overweight and obesity work in different ways. Some may help you feel less hungry or full sooner. Others may make it harder for your body to absorb fat from the foods you eat.
Another treatment is weight loss surgery (bariatric surgery). Your doctor may recommend weight loss surgery (bariatric surgery) if you have severe obesity or serious obesity-related health problems and you have not been able to lose enough weight 24, 66.
If you’ve been diagnosed with sleep-disordered breathing, like obstructive sleep apnea (OSA), treating that disorder is also an important part of preventing complications.
Pickwickian syndrome symptoms
People with Pickwickian syndrome or obesity hypoventilation syndrome commonly experience multiple symptoms, including:
- Breathlessness or difficulty or labored breathing
- Choking or lapses in breathing during sleep
- Daytime sluggishness or excessive daytime sleepiness, especially if you also have sleep apnea
- Dizziness
- Fatigue, or extreme tiredness
- Morning headaches
- Enlarged neck
- Swelling in the feet, ankles, and legs
In addition to the above symptoms, you or a loved one may notice you often snore loudly, choke or gasp, or have trouble breathing at night. Your symptoms may get worse over time.
Since Pickwickian syndrome or obesity hypoventilation syndrome involves increased carbon dioxide levels in your bloodstream, also called hypercapnia or hypercarbia, people with Pickwickian syndrome may experience additional symptoms related to hypercapnia. Increased carbon dioxide in the bloodstream can cause:
- Fatigue
- Confusion
- Flushed skin
- Nausea
- Difficulty breathing during exercise
- Irritability
- Fever
- Wheezing
- Increased sweating
People with obesity hypoventilation syndrome have obesity (body mass index (BMI) of 30 kg/m² or greater). A physical exam may show:
- Bluish color in the lips, fingers, toes, or skin (cyanosis)
- Reddish skin
- Signs of right-sided heart failure (cor pulmonale), such as swollen legs or feet, shortness of breath, or feeling tired after little effort
- Signs of extreme sleepiness
The vast majority of patients with Pickwickian syndrome or obesity hypoventilation syndrome also have symptoms of obstructive sleep apnea (OSA), including snoring, nighttime choking, witnessed apneas, nonrestorative sleep, excessive daytime sleepiness, and fatigue. In contrast to patients with obstructive sleep apnea (OSA) alone, patients with obesity hypoventilation syndrome complain of shortness of breath (dyspnea), are often hypoxemic, and can have signs of pulmonary hypertension. Pulmonary hypertension is a type of high blood pressure that affects the arteries in your lungs and the right side of your heart. The signs and symptoms of pulmonary hypertension develop slowly. You may not notice them for months or even years. Pulmonary hypertension signs and symptoms include:
- Blue lips and skin (cyanosis)
- Chest pressure or pain
- Dizziness or fainting spells (syncope)
- Fast pulse or pounding heartbeat (palpitations)
- Fatigue
- Shortness of breath (dyspnea), initially while exercising and eventually while at rest
- Swelling (edema) in the ankles, legs and eventually the belly area (abdomen).
Pickwickian syndrome complications
In progressive or untreated Pickwickian syndrome or obesity hypoventilation syndrome, biventricular heart failure, pulmonary hypertension and volume overload are common 67. Patients with obesity hypoventilation syndrome have a lower quality of life with a higher overall symptom course, continued daytime sleepiness, and increased healthcare expenses. They are also at a higher risk of increased pulmonary and right-sided heart pressure overload complications, significantly increasing morbidity, and have overall early mortality than non-hypercapnic patients with sleep-disordered breathing alone 68. A post hoc analysis of the Pickwick trial found that 122 patients of the 246 participants who had obesity hypoventilation syndrome had elevated systolic pulmonary artery pressures (40 mmHg or more) 67. While obesity and early/late diastolic peak flow relationship were predictors of pulmonary hypertension in the non-severe obstructive sleep apnea (OSA) group, low wake PaO2 levels and BMI were risk factors for pulmonary hypertension in those with obesity hypoventilation syndrome and severe obstructive sleep apnea (OSA). Even when treated with positive airway pressure (PAP) therapy, the mortality in those with severe obesity hypoventilation syndrome remains substantially worse than in individuals with OSA alone 10. Higher hospitalization rates, intensive care unit admissions, and post-discharge long-term care are also higher in obesity hypoventilation syndrome patients than eucapnic obese individuals.
Pickwickian syndrome diagnosis
If your doctor suspects that you have Pickwickian syndrome or obesity hypoventilation syndrome, he/she will:
- Perform a physical exam
- Measure your weight and height
- Calculate your body mass index (BMI). You can calcultae your BMI here (https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm)
- Measure your waist and neck circumference
Plethoric (reddish) obese patients with hypoxemia, an increased neck circumference, a decreased airway area, a prominent P2 (a loud second heart sound) on cardiac auscultation, and leg edema, as determined by physical examination, are at risk of having obesity hypoventilation syndrome 42.
Additional tests might include lung tests to measure the amount of oxygen in your body or how well your lungs are working. You may also need a sleep study if your doctor thinks you may have sleep apnea.
The American Academy of Sleep Medicine defines Pickwickian syndrome or obesity hypoventilation syndrome as follows: the presence of awake daytime alveolar hypoventilation (PaCO2 > 45 mmHg as measured at sea level) in patients with a BMI ≥ 30 kg/m² in the absence of other causes of hypoventilation 9.
Pickwickian syndrome or obesity hypoventilation syndrome is considered a diagnosis of exclusion because so many other disorders manifest similarly and must be ruled out first. The following conditions can produce similar symptoms to those seen in obesity hypoventilation syndrome, and your doctor might perform tests related to them before giving an obesity hypoventilation syndrome diagnosis.
Other causes of hypoventilation should be ruled out first include:
- Chronic obstructive pulmonary disease (COPD) or other severe obstructive lung diseases. Patients with chronic obstructive pulmonary disease (COPD) who are hypercapnic and obese commonly have sleep-disordered breathing 69. Therefore, a complete pulmonary function test and arterial blood gas are critical in establishing the diagnosis. Patients who have evidence of obstructive ventilatory defect cannot be given a diagnosis of obesity hypoventilation syndrome.
- Severe interstitial lung diseas. Restrictive diseases from disorders affecting the pulmonary parenchyma may lead to hypoxemia without hypercapnia.
- Mechanical respiratory limitation such as in severe chest wall deformities, or chest wall changes such as kyphoscoliosis. Acute hypercapnic respiratory failure is more common in patients with extrapulmonary chest wall restriction (pectus deformity, scoliosis, kyphosis), which causes compromised respiratory mechanics. Ascites and severe bowel distention can compromise respiratory mechanics by exerting a significant cephalad force on the diaphragm. Extrapulmonary chest wall restriction commonly causes poor ventilatory reserve without overt respiratory failure.
- Neurological diseases and muscular conditions such as amyotrophic lateral sclerosis (ALS), spinal cord injuries, Duchenne muscular dystrophy, Guillain-Barre syndrome, myasthenia gravis, myositis, poliomyelitis (polio) and post-polio syndrome.
- Amyotrophic lateral sclerosis (ALS) often leads to hypercapnic respiratory failure 70. Patients usually have clues on neurologic examination suggestive of typical features of ALS, such as muscle weakness, fasciculation, and hyperactive deep tendon reflexes.
- Patients with spinal cord injuries can present with sleep-disordered breathing and chronic hypercapnia during sleep and wakefulness 71, 72. These patients are not usually obese and have a history of acute injury or trauma that led to neurological deficits. However, patients with spinal cord injury commonly have sleep-disordered breathing and restrictive ventilatory defects mimicking obesity hypoventilation syndrome 73, 74.
- Muscular dystrophies, such as Duchenne or Becker, can cause hypercapnic respiratory failure but have multiple other features like overall muscular weakness, growth delay, cardiomyopathies, and lab abnormalities like elevated creatinine kinase (CK), making the diagnosis apparent in a pediatric age group. Becker muscular dystrophy has a slightly more variable and benign course but remains with similar overall clinical features.
- Patients with Guillain-Barre syndrome generally present with rapid onset of ascending, symmetric paralysis, and areflexia occurring over 2 to 4 weeks. Dysautonomia is common and can cause hemodynamic instability or cardiac arrhythmias.
- In myasthenia gravis, the hallmark feature is muscle fatigability, diplopia, ptosis, dysarthria, limb weakness, and weak cough.
- Poliomyelitis and post-polio syndrome are associated with acute flaccid paralysis or new weakness and fatigability, but vaccination has largely eradicated these from the US.
- Diaphragmatic paralysis or phrenic nerve injury.
- Electrolyte disturbances such as hypophosphatemia, hypomagnesemia, hypermagnesemia, hypokalemia, and hypocalcemia;
- Central sleep apnea (CSA). In central sleep apnea, the problem is not a blocked airway. Instead, pauses in breathing occur because the brain and the muscles that control breathing do not function properly. Central sleep apnea occurs when your brain fails to transmit signals to your breathing muscles. As a result, a person with central sleep apnea repeatedly stops trying to breathe as they sleep. Patients with central sleep apnea are generally normocapnic or slightly hypocapnic on blood gas testing. Central sleep apnea can be caused by a number of conditions that affect the ability of your brainstem — which links your brain to your spinal cord and controls many functions such as heart rate and breathing — to control your breathing.
- Untreated hypothyroidism and myxedema. Extremely low levels of circulating free thyroid hormones can present with respiratory insufficiency and hypercapnic failure but will have coexistent features of hypothermia, including bradycardia, sluggish tendon reflexes they may be hemodynamically unstable along with neurological deficits up to coma in extreme cases.
- Bowel distention.
- Acute infection.
- Erythrocytosis, a red blood cell disorder.
- Congenital alveolar hypoventilation syndrome (Ondine’s syndrome).
- Use of sedatives, hypnotics, opiates, or alcohol.
Symptoms seen in obesity hypoventilation syndrome can also be caused by medications, such as sedatives or illicit drugs. For this reason, doctors might ask about medications or give a urine drug test as part of their assessment when they observe obesity hypoventilation syndrome-like symptoms.
Tests used to help diagnose obesity hypoventilation syndrome include:
- Pulse oximetry. Hypoxemia during wakefulness is not common in obstructive sleep apnea (OSA) alone and requires confirmation by an arterial blood gas (ABG) showing PaO2 <70 mmHg.Hypoxia can be measured noninvasively through pulse oximetry. Another tool used in evaluating obstructive sleep apnea (OSA) and obesity hypoventilation syndrome is the polysomnogram (sleep study).
- Complete blood count. Polycythemia due to chronic hypoventilation and hypoxia may be present. Blood tests can rule out secondary causes of erythrocytosis and other mimicking diagnoses like hypothyroidism.
- Arterial blood gas (ABG). A sensitive screening test for chronic hypercapnia is an elevated serum bicarbonate level (greater than 27 mEq/L), and almost all patients with obesity hypoventilation syndrome have elevated bicarbonate. However, this is not a specific test, and elevation can occur in several other diagnoses, including vomiting, dehydration, medications, etc. Arterial blood gas (ABG) is a more definitive test for alveolar hypoventilation and defines hypercapnia as the partial pressure of arterial CO2 (PaCO2) greater than 45 mmHg.
- Chest x-ray or CT scan to rule out other possible causes
- Lung function tests (pulmonary function tests). The pulmonary function test results in obesity hypoventilation syndrome can reveal a moderate restrictive defect without evidence of airway obstruction, but it may also be normal.
- Sleep study (polysomnography). Polysomnography (sleep study) with continuous nocturnal CO2 monitoring is the gold standard for evaluating obesity hypoventilation syndrome. In addition, the oxygen nadir and percent time spent below O2 saturation (SpO2) of 90% (T90) help suspect obesity hypoventilation syndrome.
- Electrocardiogram (EKG) and Echocardiogram (ultrasound of the heart) help assess right heart enlargement and failure secondary to pulmonary hypertension that develops late in obesity hypoventilation syndrome.
Your doctor can tell obesity hypoventilation syndrome (OHS) from obstructive sleep apnea (OSA) because a person with obesity hypoventilation syndrome (OHS) has a high carbon dioxide level in their blood when awake.
Patients suspected of having Pickwickian syndrome or obesity hypoventilation syndrome can initially be screened by pulse oximetry and by determination of serum levels of venous bicarbonate (HCO3–). A pulse oximeter reading only indicates what percentage of your blood is saturated with oxygen, known as the SpO2 level, as well as your heart rate. It’s a quick and harmless way to check if someone’s blood oxygen level is too low. Borderline pulse oximetry values are common findings. Consequently, SpO2 (blood oxygen saturation) values less than 93% on pulse oximetry would be suggestive of hypoventilation. However, higher values are not exclusionary, which explains why this is not a necessary criterion to establish the diagnosis of obesity hypoventilation syndrome, although it helps in screening 3. Nocturnal pulse oximetry showing sustained hypoxemia and no associated apneas strengthens the suspicion for hypoventilation 3.
Patients with obesity hypoventilation syndrome undergoing arterial blood gas (ABG) analysis rarely have PaO2 values > 70 mmHg 3. A serum bicarbonate (HCO3–) level ≥ 27 mEq/L had a sensitivity of 92% and a specificity of 50%, justifying its use in screening 75, 76, 77. After such screening, arterial blood gas analysis is mandatory 3.
For excluding other causes of hypoventilation, pulmonary function testing and assessment of respiratory muscle strength (MIP and MEP), chest X-ray, electrocardiography (ECG), and thyroid function testing should be performed 3. In addition, the use of drugs and medications, such as sedatives, hypnotics, opiates, and alcohol (alcohol abuse), should be investigated 3. Polysomnography (sleep study) is not necessary for the diagnosis of obesity hypoventilation syndrome 9. However, since it has been observed that individuals with obesity hypoventilation syndrome have obstructive events, as well as lower saturation in REM sleep (Figure 1), polysomnography (sleep study) is requested with a view to treating comorbid sleep apnea and to justifying possible treatments 78.
Pickwickian syndrome or obesity hypoventilation syndrome diagnostic criteria
The American Academy of Sleep Medicine set diagnostic criteria for Pickwickian syndrome or obesity hypoventilation syndrome in the International Classification of Sleep Disorders, Third Edition (ICSD-3) released in 2014 9, 1, 3, 6, 7, 8:
To be diagnosed with Pickwickian syndrome or obesity hypoventilation syndrome, a person must:
- Experience inadequate breathing, called hypoventilation, while they are awake, called daytime alveolar hypoventilation, resulting in increased carbon dioxide in the blood measuring above 45 mm Hg (PaCO2 > 45 mmHg as measured at sea level)
- Be categorized as obese, as defined by a body mass index (BMI) ≥ 30 kg/m²
- Not have any other disorders or medications causing their hypoventilation
Although not diagnostic criteria, people with obesity hypoventilation syndrome often find that their hypoventilation and blood carbon dioxide levels worsen during sleep, particularly in the rapid eye movement (REM) stage of sleep. People with obesity hypoventilation syndrome often have obstructive sleep apnea (OSA) and should receive a diagnosis of both obesity hypoventilation syndrome and OSA if both are present. Those with obesity hypoventilation syndrome also tend to experience lower blood oxygen levels, but that is not a diagnostic criteria.
Pickwickian syndrome differential diagnosis
Other causes of hypoventilation include:
- Chronic obstructive pulmonary disease (COPD) or other severe obstructive lung diseases. Patients with chronic obstructive pulmonary disease (COPD) who are hypercapnic and obese commonly have sleep-disordered breathing 69. Therefore, a complete pulmonary function test and arterial blood gas are critical in establishing the diagnosis. Patients who have evidence of obstructive ventilatory defect cannot be given a diagnosis of obesity hypoventilation syndrome.
- Severe interstitial lung diseas. Restrictive diseases from disorders affecting the pulmonary parenchyma may lead to hypoxemia without hypercapnia.
- Mechanical respiratory limitation such as in severe chest wall deformities, or chest wall changes such as kyphoscoliosis. Acute hypercapnic respiratory failure is more common in patients with extrapulmonary chest wall restriction (pectus deformity, scoliosis, kyphosis), which causes compromised respiratory mechanics. Ascites and severe bowel distention can compromise respiratory mechanics by exerting a significant cephalad force on the diaphragm. Extrapulmonary chest wall restriction commonly causes poor ventilatory reserve without overt respiratory failure.
- Neurological diseases and muscular conditions such as amyotrophic lateral sclerosis (ALS), spinal cord injuries, Duchenne muscular dystrophy, Guillain-Barre syndrome, myasthenia gravis, myositis, poliomyelitis (polio) and post-polio syndrome.
- Amyotrophic lateral sclerosis (ALS) often leads to hypercapnic respiratory failure 70. Patients usually have clues on neurologic examination suggestive of typical features of ALS, such as muscle weakness, fasciculation, and hyperactive deep tendon reflexes.
- Patients with spinal cord injuries can present with sleep-disordered breathing and chronic hypercapnia during sleep and wakefulness 71, 72. These patients are not usually obese and have a history of acute injury or trauma that led to neurological deficits. However, patients with spinal cord injury commonly have sleep-disordered breathing and restrictive ventilatory defects mimicking obesity hypoventilation syndrome 73, 74.
- Muscular dystrophies, such as Duchenne or Becker, can cause hypercapnic respiratory failure but have multiple other features like overall muscular weakness, growth delay, cardiomyopathies, and lab abnormalities like elevated creatinine kinase (CK), making the diagnosis apparent in a pediatric age group. Becker muscular dystrophy has a slightly more variable and benign course but remains with similar overall clinical features.
- Patients with Guillain-Barre syndrome generally present with rapid onset of ascending, symmetric paralysis, and areflexia occurring over 2 to 4 weeks. Dysautonomia is common and can cause hemodynamic instability or cardiac arrhythmias.
- In myasthenia gravis, the hallmark feature is muscle fatigability, diplopia, ptosis, dysarthria, limb weakness, and weak cough.
- Poliomyelitis and post-polio syndrome are associated with acute flaccid paralysis or new weakness and fatigability, but vaccination has largely eradicated these from the US.
- Diaphragmatic paralysis or phrenic nerve injury.
- Electrolyte disturbances such as hypophosphatemia, hypomagnesemia, hypermagnesemia, hypokalemia, and hypocalcemia;
- Central sleep apnea (CSA). In central sleep apnea, the problem is not a blocked airway. Instead, pauses in breathing occur because the brain and the muscles that control breathing do not function properly. Central sleep apnea occurs when your brain fails to transmit signals to your breathing muscles. As a result, a person with central sleep apnea repeatedly stops trying to breathe as they sleep. Patients with central sleep apnea are generally normocapnic or slightly hypocapnic on blood gas testing. Central sleep apnea can be caused by a number of conditions that affect the ability of your brainstem — which links your brain to your spinal cord and controls many functions such as heart rate and breathing — to control your breathing.
- Untreated hypothyroidism and myxedema. Extremely low levels of circulating free thyroid hormones can present with respiratory insufficiency and hypercapnic failure but will have coexistent features of hypothermia, including bradycardia, sluggish tendon reflexes they may be hemodynamically unstable along with neurological deficits up to coma in extreme cases.
- Bowel distention.
- Acute infection.
- Erythrocytosis, a red blood cell disorder.
- Congenital alveolar hypoventilation syndrome (Ondine’s syndrome).
- Use of sedatives, hypnotics, opiates, or alcohol.
Pickwickian syndrome treatment
Multiple treatments exist for obesity-hypoventilation syndrome or Pickwickian syndrome.
Weight loss through healthy lifestyle changes
Numerous studies have shown improvement in obesity hypoventilation syndrome symptoms with weight loss 65, 15. Weight loss significantly reduces CO2 production and improves sleep apnea severity and alveolar ventilation. Weight loss improves nocturnal oxyhemoglobin saturation, decreases the frequency of respiratory apneas hypopneas, and improves pulmonary function 79. Weight loss also improves pulmonary artery hypertension and left ventricular dysfunction, significantly reducing cardiovascular compromise in obesity hypoventilation syndrome patients 5. This weight loss should be controlled and supervised, preferably in a weight loss program. The weight-loss target recommended for obesity-hypoventilation syndrome is 25 to 30% of actual body weight to achieve hypoventilation effectively 24.
Healthy eating
Adopting a healthy eating style that promotes weight loss must include lowering your total calorie intake. One way you can lower your calorie intake is by eating more plant-based foods — fruits, vegetables and whole grains. Strive for variety to help you achieve your goals without giving up taste or nutrition.
Get your weight loss started with these tips:
- Eat at least four servings of vegetables and three servings of fruits daily.
- Replace refined grains with whole grains.
- Use modest amounts of healthy fats, such as olive oil, vegetable oils, avocados, nuts, nut butters and nut oils.
- Cut back on sugar as much as possible, except the natural sugar in fruit.
- Choose low-fat dairy products and lean meat and poultry in limited amounts.
These foods are the foundation of a heart-healthy eating plan.
- Vegetables such as leafy greens (spinach, collard greens, kale, cabbage), broccoli, and carrots
- Fruits such as apples, bananas, oranges, pears, grapes, and prunes
- Whole grains such as plain oatmeal, brown rice, and whole-grain bread or tortillas
- Fat-free or low-fat dairy foods such as milk, cheese, or yogurt
- Protein-rich foods:
- Fish high in omega-3 fatty acids (salmon, tuna, and trout)
- Lean meats such as 95% lean ground beef or pork tenderloin or skinless chicken or turkey
- Eggs
- Nuts, seeds, and soy products (tofu)
- Legumes such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
- Oils and foods high in monounsaturated and polyunsaturated fats:
- Canola, corn, olive, safflower, sesame, sunflower, and soybean oils (not coconut or palm oil)
- Nuts such as walnuts, almonds, and pine nuts
- Nut and seed butters
- Salmon and trout
- Seeds (sesame, sunflower, pumpkin, or flax)
- Avocados
- Tofu
A heart-healthy eating plan limits sodium (salt), saturated fat, added sugars, and alcohol.
Exercise
While you can lose weight without exercise, regular physical activity plus calorie restriction can help give you the weight-loss edge. Exercise can help burn off the excess calories you can’t cut through diet alone.
Regular physical activity can:
- Help you lose excess weight
- Improve physical fitness
- Lower many heart disease risk factors such as “bad” LDL cholesterol levels, increase “good” HDL cholesterol levels, and manage high blood pressure
- Lower stress and improve your mental health
- Lower your risk for other conditions such as type 2 diabetes, depression, and cancer
Exercise also offers numerous health benefits, including boosting your mood, strengthening your cardiovascular system and reducing your blood pressure. Exercise can also help in maintaining weight loss. Studies show that people who maintain their weight loss over the long term get regular physical activity.
How many calories you burn depends on the frequency, duration and intensity of your activities. The more active you are, the more you benefit. One of the best ways to lose body fat is through steady aerobic exercise — such as brisk walking — for at least 30 minutes most days of the week. Some people may require more physical activity than this to lose weight and maintain that weight loss.
Any extra movement helps burn calories. Think about ways you can increase your physical activity throughout the day if you can’t fit in formal exercise on a given day. For example, make several trips up and down stairs instead of using the elevator, or park at the far end of the lot when shopping.
The U.S. Department of Health and Human Services’ Physical Activity Guidelines for Americans recommends that each week, adults get at least:
- 150 minutes (2 hours and 30 minutes) to 300 minutes (5 hours) a week of moderate-intensity aerobic physical activity, or
- 75 minutes (1 hour and 15 minutes) to 150 minutes (2 hours and 30 minutes) a week of vigorous-intensity aerobic physical activity, or
- A combination of both moderate-intensity and vigorous-intensity activity.
Get enough good-quality sleep
Experts recommend 7 to 8 hours of sleep per night for adults.
Non-invasive positive airway pressure (PAP)
The first-line therapy involves positive airway pressure (PAP) breathing assistance using special machines (mechanical ventilation) 80, 81. Options include:
- Non-invasive airway pressure therapy, such as continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP), can help reduce carbon dioxide levels in the blood. Generally, people who have obesity hypoventilation syndrome and sleep-related breathing disorders start by using a CPAP machine during sleep. Positive airway pressure therapy is also sometimes recommended for those who experience higher carbon dioxide levels even without sleep-disordered breathing. Positive airway pressure (PAP) therapy should not be delayed while the patient tries to lose weight.
- Given that most patients with obesity hypoventilation syndrome (90%) have coexistent obstructive sleep apnea (OSA), CPAP is considered the initial modality of choice 82. In those with sleep-related hypoventilation and fewer obstructive events during sleep, BPAP is the first choice 83.
- Continuous positive airway pressure (CPAP) delivers constant pressure through the entire respiratory cycle, helping maintain the upper airway patency and reducing obstructive events. In the subset of patients with a lack of improvement in hypercapnia despite objective evidence of adequate adherence to CPAP, bi-level positive airway pressure (BiPAP) is chosen. Bi-level positive airway pressure (BiPAP) should also be the option if the patient is intolerant of CPAP or demonstrates a need for higher pressures in CPAP (over 15 cm H2O) 84. Although comparative trials are lacking, most would consider BPAP the mode of choice to augment ventilation when CPAP fails or becomes intolerant.
- For initiation of BPAP, an inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP) are independently titrated and set 85. The pressure difference between IPAP and EPAP is the driving pressure, the main contributor to ventilation and CO2 elimination.
- Supplemental oxygen therapy might be needed for some with obesity hypoventilation syndrome.
High levels of positive airway pressure (PAP) are often needed because of poor chest wall compliance from obesity, diminished lung compliance from atelectasis (complete or partial collapse of the entire lung or lobe of the lung), and cephalad displacement of the diaphragm from central adiposity during sleep. Using positive airway pressure (PAP), arterial blood gases should be monitored closely to ensure clinical improvement. For patients presenting to the hospital with acute worsening of chronic hypoxic hypercapnic respiratory failure, a decision about the ventilation mode must be made based on the severity of the respiratory failure. A trial of non-invasive positive pressure ventilation, as an initial choice, can be afforded to an arousable patient with an intact gag and cough reflex 4.
However, early intubation should be considered when patients cannot protect their airways, do not tolerate bi-level positive airway pressure (BiPAP), or do not improve quickly 4. Patients admitted to the hospital due to acute, chronic hypercapnia respiratory failure often do not have a formal diagnosis of OSA or known PAP pressures (based on official titration); therefore, empirical treatment is used. In these cases that require empirical therapy with non-invasive ventilation, the choice of pressures (IPAP and EPAP) depends on the severity of respiratory acidosis and body weight (to maintain upper airway patency while providing adequate pressure support for ventilation) 85.
Adherence to positive airway pressure (PAP) therapy, measured as the average hours of daily use in the past 30 days, is among the most challenging aspects of the management of obesity hypoventilation syndrome; this may be due to difficulty with the device and the masks, patient non-compliance, lack of education, or financial constraints. In a meta-analysis that included 25 studies, positive airway pressure (PAP) was associated with improving obesity hypoventilation syndrome symptoms and mortality 86. Furthermore, positive airway pressure (PAP) treatment improved gas exchange, daytime sleepiness, sleep quality, quality of life, and frequency of emergency department visits 86. Various types and sizes of masks can be used in patients diagnosed with obesity hypoventilation syndrome. Therefore patient education about the disease process, the availability of several kinds of masks, and the necessity for positive airway pressure (PAP) to prevent progression to complications and morbidity must be thoroughly addressed to maintain satisfactory adherence.
Supplemental oxygen therapy is necessary for patients with obesity hypoventilation syndrome and hypoxemia despite positive airway pressure (PAP) use. This situation occurs in up to 50% of patients in the literature 87. Over time, the correct use of positive airway pressure (PAP) may correct the hypoxemia to an acceptable level. This cohort of patients on positive airway pressure (PAP) with supplemental oxygen has to be regularly followed to avoid the long-term cost and toxicity of continued oxygen therapy. Oxygen therapy alone in the absence of positive airway pressure (PAP) is strongly discouraged as it will not augment ventilation and may have poor outcomes with worsening CO2 retention 88, 81. In a recent randomized crossover, a clinical study found that supplemental oxygen of 100% causes worsening hypercapnia (CO2 increased by 5.0 mmHg compared with room air) and decreased minute ventilation (by 1.4 L/min) in stable patients with obesity-associated hypoventilation 81, 89.
Weight loss surgery
Weight loss surgery (bariatric surgery) is often recommended to people with obesity hypoventilation syndrome who have trouble losing weight through lifestyle changes.
Types of weight-loss (bariatric) surgeries are listed below.
- Gastrectomy also called gastric sleeve surgery or vertical sleeve gastrectomy: In gastric sleeve surgery or vertical sleeve gastrectomy, a surgeon removes most of your stomach, leaving only a banana-shaped section that is closed with staples. The surgery reduces the amount of food that can fit in your stomach, making you feel full sooner. Taking out part of your stomach may also affect hormones or bacteria in the gastrointestinal system that affect appetite and metabolism. This type of surgery cannot be reversed because some of the stomach is permanently removed.
- Gastric bypass surgery also called Roux-en-Y gastric bypass: A small part of the stomach is connected to the middle part of the intestine, bypassing the first part of intestine. This reduces the amount of food that you can eat and the amount of fat your body can take in and store.
- Gastric banding: In adjustable gastric band surgery, the surgeon places a ring with an inner inflatable band around the top of your stomach to create a small pouch. Like gastric sleeve and gastric bypass surgery, the gastric band makes you feel full after eating a small amount of food. The inner band has a circular balloon inside that is filled with saline solution. The surgeon can adjust the inner band to resize the opening from the pouch to the rest of your stomach by injecting or removing the saline solution through a small device, called a port, that is placed under your skin. After surgery, you will need several follow-up visits to adjust the size of the band opening. If the band causes problems or is not helping you lose enough weight, the surgeon may remove it. Today, adjustable gastric band surgery is less commonly performed in the United States, compared with the gastric sleeve or gastric bypass, because it is associated with more complications, predominantly the need for band removal due to intolerance 90. Gastric band surgery also typically results in significantly less weight loss and is associated with more complications, predominately the need for band removal due to intolerance 90.
- Biliopancreatic diversion with duodenal switch (BPD-DS). A surgical procedure called biliopancreatic diversion with duodenal switch, or “mixed surgery,” involves two separate procedures. The first procedure is similar to gastric sleeve surgery. A second surgical procedure divides the small intestine into two tracts. Food moves through one tract, bypassing most of the small intestine. This reduces the number of calories and amount of nutrients absorbed. Digestive juices flow from the stomach through the other intestinal tract and mix with food as it enters the colon. This type of surgery allows you to lose more weight compared with the other three operations described above. However, it is also the most likely to cause surgery-related problems and a shortage of vitamins, minerals, and proteins in your body. For these reasons, surgeons do not perform this particular procedure often. However, some surgeons may recommend it for patients who have severe obesity and certain health conditions.
Talk to your doctor to learn more about the benefits and risks of each type of surgery. All surgeries carry some type of risk of possible complications, including bleeding, infection, or even death.
Although dedicated studies looking at weight loss surgery (bariatric surgery) for patients with obesity hypoventilation syndrome are lacking, various studies have shown these interventions having mixed efficacy for long-term improvement in obstructive sleep apnea (OSA) symptoms, apnea-hypopnea index (AHI), and weight loss maintenance. In a meta-analysis done in 2009, including 12 different studies, patients undergoing sleep studies before and after maximal weight loss from bariatric surgery reported a 71% reduction in apnea-hypopnea index (AHI) 91. Still, only 38% achieved a cure, defined as apnea-hypopnea index (AHI) less than 5/hour 91. Nearly two-thirds had residual disease, with most of them having persistent moderate obstructive sleep apnea (OSA), defined as apnea-hypopnea index (AHI) greater than or equal to 15/hour 91. With outcomes debatable, bariatric surgery still poses significant risks and complications. The perioperative mortality is high, and that for obstructive sleep apnea (OSA) and obesity hypoventilation syndrome may be higher 92. Therefore, it is usual to initiate PAP therapy immediately after extubation, especially since there is no compelling evidence of PAP therapy-induced anastomotic complications 93, 94.
Tracheostomy
In extreme cases, an opening in your neck (tracheostomy) surgery might be used to improve breathing by connecting a tube directly to the airway 23. Tracheostomy is aimed at sleep-disordered breathing and is generally only for those intolerant of or consistently non-adherent to positive airway pressure (PAP) therapy and those in whom disease progression to complications including cor pulmonale occurs 4. Most people with a tracheostomy for obesity hypoventilation syndrome still require positive airway pressure (PAP) therapy. It targets sleep-disordered breathing but does not alter the pulmonary mechanics, respiratory drive, or neurohumoral milieu 95. Moreover, some patients may not return to a normal CO2 (eucapnic) state post tracheostomy, as it does not affect CO2 production and impaired muscle strength. Also inherent to the tracheostomy procedure are surgical risks and procedural difficulties in the obese population.
Medication
The role of medications for obesity hypoventilation syndrome is limited. Respiratory stimulants, such as acetazolamide, medroxyprogesterone, and theophylline — can potentially lower carbon dioxide levels in blood by stimulating respiration. However, these are not usually prescribed for very long periods of time because of potential side effects and limited data supporting their use in a practical setting 96. These medications have sometimes been considered adjunctive (add-on) therapies of last resort for patients who chronically continue to have hypoventilation despite BPAP therapy and weight loss. By blocking carbon dioxide conversion to bicarbonate, acetazolamide can lower pH in the brain and theoretically increase central ventilatory drive and minute ventilation.
Medroxyprogesterone serves as a respiratory stimulant at the hypothalamic level, but results from studies have been insufficient and contradictory, along with increased risks of hypercoagulability and venous thromboembolism. Other side effects like decreased libido and erectile dysfunction in men and uterine bleeding in women should be considered 97.
Theophylline is a bronchodilator as well as a direct respiratory stimulant. Its use in obesity hypoventilation syndrome has never been studied and is currently not recommended.
Other pharmacological therapies that stimulate the respiratory system (such as buspirone and mirtazapine) and hypnotics (such as zolpidem) have been studied recently in patients with sleep-disordered breathing and high-risk patients such as spinal cord injury 98, 99, 99, 100.
The use of recombinant human leptin (metreleptin) as a subcutaneous injection in patients with congenital or acquired generalized lipodystrophy has been approved by the US Food and Drug Administration (FDA) to treat metabolic complications of leptin deficiency, however no studies to date in patients with obesity hypoventilation syndrome 101.
Pickwickian syndrome prognosis
Untreated, people with Pickwickian syndrome or obesity hypoventilation syndrome face a greater risk of being hospitalized, going into intensive care unit (ICU) and requiring more long-term care than people who have obesity but not obesity hypoventilation syndrome 102. Pickwickian syndrome or obesity hypoventilation syndrome can progress over time to serious heart and blood vessel problems, severe disability, or death 68. Studies show that people who have both obesity hypoventilation syndrome and another medical condition experience high mortality rates of 23% within 18 months and 46% within 50 months. Treating obesity hypoventilation syndrome early on with positive airway pressure (PAP) therapy can reduce mortality rates by 10%.
Pickwickian syndrome or obesity hypoventilation syndrome is linked with multiple complications.
Pickwickian syndrome or obesity hypoventilation syndrome complications related to a lack of sleep may include:
- Depression, agitation, irritability
- Increased risk for accidents or mistakes at work
- Problems with intimacy and sex
Obesity hypoventilation syndrome can also cause heart problems, such as:
- High blood pressure (hypertension)
- Right-sided heart failure (cor pulmonale)
- High blood pressure in the lungs (pulmonary hypertension)
People with obesity hypoventilation syndrome, especially when it is not properly treated, may experience heart failure or respiratory failure. The earlier obesity hypoventilation syndrome is found and treated, the less likely a person is to experience complications.
Obesity more generally is also linked with multiple complications. Since, by definition, people with obesity hypoventilation syndrome have obesity, they are at risk of these complications as well. Complications associated with obesity include high blood pressure, diabetes, hypothyroidism, high cholesterol, liver dysfunction, and osteoarthritis.
Pickwickian syndrome life expectancy
Untreated, people with Pickwickian syndrome or obesity hypoventilation syndrome face a greater risk of being hospitalized, going into intensive care unit (ICU) and requiring more long-term care than people who have obesity but not obesity hypoventilation syndrome 102.
Berg et al. 44 conducted a study involving 20 patients with obesity hypoventilation syndrome, who were matched to control subjects by age, gender, and zip code to try to equate socioeconomic factors. A comparison with controls revealed that the most common morbidities in patients with obesity hypoventilation syndrome were cardiovascular diseases: congestive heart failure; chest pain caused by reduced blood flow to the heart (angina pectoris) and right heart failure (cor pulmonale). In a retrospective study conducted by Basoglu & Tasbakan 25, having a BMI > 40 kg/m² and obesity-related complications showed a strong association with an increased risk of premature death in hospitalized patients. Nowbar et al. 28 reported that, at 18 months following hospital discharge, rate of death (mortality) was 23% in patients with obesity-related hypoventilation, which was almost twice as high as that among obese patients without hypoventilation.
Patients with obesity hypoventilation syndrome use more health care resources in the period prior to the diagnosis than do obese individuals without obesity hypoventilation syndrome or the general population 44. Obesity per se leads to a greater likelihood of diseases such as systemic arterial hypertension, diabetes, dyslipidemia, and hypothyroidism. Comorbidities such as heart failure, coronary artery disease, and right-sided heart failure (cor pulmonale) are more common in patients with obesity hypoventilation syndrome, and the likelihood that such patients will require invasive mechanical ventilation or ICU admission is also increased 28, 45. In addition, pulmonary hypertension is more common (50% vs. 15%) and more severe in patients with obesity hypoventilation syndrome than in patients with obstructive sleep apnea (OSA) 46, 47, 48.
References- Mokhlesi B, Kryger MH, Grunstein RR. Assessment and management of patients with obesity hypoventilation syndrome. Proc Am Thorac Soc. 2008 Feb 15;5(2):218-25. doi: 10.1513/pats.200708-122MG
- Randerath W, Verbraecken J, Andreas S, Arzt M, Bloch KE, Brack T, Buyse B, De Backer W, Eckert DJ, Grote L, Hagmeyer L, Hedner J, Jennum P, La Rovere MT, Miltz C, McNicholas WT, Montserrat J, Naughton M, Pepin JL, Pevernagie D, Sanner B, Testelmans D, Tonia T, Vrijsen B, Wijkstra P, Levy P. Definition, discrimination, diagnosis and treatment of central breathing disturbances during sleep. Eur Respir J. 2017 Jan 18;49(1):1600959. doi: 10.1183/13993003.00959-2016
- Athayde RAB, Oliveira Filho JRB, Lorenzi Filho G, Genta PR. Obesity hypoventilation syndrome: a current review. J Bras Pneumol. 2018 Nov-Dec;44(6):510-518. doi: 10.1590/S1806-37562017000000332
- Ghimire P, Sankari A, Kaul P. Pickwickian Syndrome. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542216
- Antoine MH, Sankari A, Bollu PC. Obesity-Hypoventilation Syndrome. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482300
- Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999 Aug 1;22(5):667-89.
- Mokhlesi B, Tulaimat A, Faibussowitsch I, Wang Y, Evans AT. Obesity hypoventilation syndrome: prevalence and predictors in patients with obstructive sleep apnea. Sleep Breath. 2007 Jun;11(2):117-24. doi: 10.1007/s11325-006-0092-8
- Mokhlesi B, Tulaimat A. Recent advances in obesity hypoventilation syndrome. Chest. 2007 Oct;132(4):1322-36. doi: 10.1378/chest.07-0027
- American Academy of Sleep Medicine. (2014). The International Classification of Sleep Disorders – Third Edition (ICSD-3). Darien, IL: American Academy of Sleep Medicine.
- Castro-Añón O, Pérez de Llano LA, De la Fuente Sánchez S, Golpe R, Méndez Marote L, Castro-Castro J, González Quintela A. Obesity-hypoventilation syndrome: increased risk of death over sleep apnea syndrome. PLoS One. 2015 Feb 11;10(2):e0117808. doi: 10.1371/journal.pone.0117808
- Masa JF, Corral J, Romero A, Caballero C, Terán-Santos J, Alonso-Álvarez ML, Gomez-Garcia T, González M, López-Martín S, De Lucas P, Marin JM, Marti S, Díaz-Cambriles T, Chiner E, Merchan M, Egea C, Obeso A, Mokhlesi B; Spanish Sleep Network(∗). Protective Cardiovascular Effect of Sleep Apnea Severity in Obesity Hypoventilation Syndrome. Chest. 2016 Jul;150(1):68-79. doi: 10.1016/j.chest.2016.02.647
- Berg G, Delaive K, Manfreda J, Walld R, Kryger MH. The use of health-care resources in obesity-hypoventilation syndrome. Chest. 2001;120(2):377–383. https://doi.org/10.1378/chest.120.2.377
- Budweiser S, Hitzl AP, Jörres RA, Schmidbauer K, Heinemann F, Pfeifer M. Health-related quality of life and long-term prognosis in chronic hypercapnic respiratory failure: a prospective survival analysis. Respir Res. 2007;8(1):92. https://doi.org/10.1186/1465-9921-8-92
- AUCHINCLOSS JH Jr, COOK E, RENZETTI AD. Clinical and physiological aspects of a case of obesity, polycythemia and alveolar hypoventilation. J Clin Invest. 1955 Oct;34(10):1537-45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC438731/pdf/jcinvest00628-0055.pdf
- BICKELMANN AG, BURWELL CS, ROBIN ED, WHALEY RD. Extreme obesity associated with alveolar hypoventilation; a Pickwickian syndrome. Am J Med. 1956 Nov;21(5):811-8. doi: 10.1016/0002-9343(56)90094-8
- Sankri-Tarbichi AG. Obstructive sleep apnea-hypopnea syndrome: Etiology and diagnosis. Avicenna J Med. 2012 Jan;2(1):3-8. doi: 10.4103/2231-0770.94803
- Mbata G, Chukwuka J. Obstructive sleep apnea hypopnea syndrome. Ann Med Health Sci Res. 2012 Jan;2(1):74-7. doi: 10.4103/2141-9248.96943
- Masa JF, Corral J, Alonso ML, Ordax E, Troncoso MF, Gonzalez M, Lopez-Martínez S, Marin JM, Marti S, Díaz-Cambriles T, Chiner E, Aizpuru F, Egea C; Spanish Sleep Network. Efficacy of Different Treatment Alternatives for Obesity Hypoventilation Syndrome. Pickwick Study. Am J Respir Crit Care Med. 2015 Jul 1;192(1):86-95. doi: 10.1164/rccm.201410-1900OC
- Mokhlesi B. Obesity hypoventilation syndrome: a state-of-the-art review. Respir Care. 2010 Oct;55(10):1347-62; discussion 1363-5
- Kessler R, Chaouat A, Schinkewitch P, Faller M, Casel S, Krieger J, Weitzenblum E. The obesity-hypoventilation syndrome revisited: a prospective study of 34 consecutive cases. Chest. 2001 Aug;120(2):369-76. doi: 10.1378/chest.120.2.369
- Pérez de Llano LA, Golpe R, Ortiz Piquer M, Veres Racamonde A, Vázquez Caruncho M, Caballero Muinelos O, Alvarez Carro C. Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome. Chest. 2005 Aug;128(2):587-94. doi: 10.1378/chest.128.2.587
- Piper AJ, Grunstein RR. Big breathing: the complex interaction of obesity, hypoventilation, weight loss, and respiratory function. J Appl Physiol (1985). 2010 Jan;108(1):199-205. doi: 10.1152/japplphysiol.00713.2009
- Piper AJ, Grunstein RR. Obesity hypoventilation syndrome: mechanisms and management. Am J Respir Crit Care Med. 2011 Feb 1;183(3):292-8. doi: 10.1164/rccm.201008-1280CI
- Mokhlesi B, Masa JF, Brozek JL, Gurubhagavatula I, Murphy PB, Piper AJ, Tulaimat A, Afshar M, Balachandran JS, Dweik RA, Grunstein RR, Hart N, Kaw R, Lorenzi-Filho G, Pamidi S, Patel BK, Patil SP, Pépin JL, Soghier I, Tamae Kakazu M, Teodorescu M. Evaluation and Management of Obesity Hypoventilation Syndrome. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2019 Aug 1;200(3):e6-e24. doi: 10.1164/rccm.201905-1071ST. Erratum in: Am J Respir Crit Care Med. 2019 Nov 15;200(10):1326.
- Basoglu OK, Tasbakan MS. Comparison of clinical characteristics in patients with obesity hypoventilation syndrome and obese obstructive sleep apnea syndrome a case-control study. Clin Respir J. 2014;8(2):167–174. doi: 10.1111/crj.12054
- BICKELMANN AG, BURWELL CS, ROBIN ED, WHALEY RD. Extreme obesity associated with alveolar hypoventilation; a Pickwickian syndrome. Am J Med. 1956;21(5):811–818. doi:10.1016/0002-9343(56)90094-8
- Olson AL, Zwillich C. The obesity hypoventilation syndrome. Am J Med. 2005;118(9):948–956. doi: 10.1016/j.amjmed.2005.03.042
- Nowbar S, Burkart KM, Gonzales R, Fedorowicz A, Gozansky WS, Gaudio JC. Obesity-associated hypoventilation in hospitalized patients prevalence, effects, and outcome. Am J Med. 2004;116(1):1–7. doi: 10.1016/j.amjmed.2003.08.022
- Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014 Aug 30;384(9945):766-81. doi: 10.1016/S0140-6736(14)60460-8. Epub 2014 May 29. Erratum in: Lancet. 2014 Aug 30;384(9945):746.
- National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. http://dx.doi.org/10.15620/cdc:106273
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, Ogden CL. Differences in Obesity Prevalence by Demographic Characteristics and Urbanization Level Among Adults in the United States, 2013-2016. JAMA. 2018 Jun 19;319(23):2419-2429. doi: 10.1001/jama.2018.7270
- Nicolini A, Ferrando M, Solidoro P, Di Marco F, Facchini F, Braido F. Non-invasive ventilation in acute respiratory failure of patients with obesity hypoventilation syndrome. Minerva Med. 2018 Dec;109(6 Suppl 1):1-5. doi: 10.23736/S0026-4806.18.05921-9
- Markussen H, Lehmann S, Nilsen RM, Natvig GK. Health-related quality of life as predictor for mortality in patients treated with long-term mechanical ventilation. BMC Pulm Med. 2019 Jan 11;19(1):13. doi: 10.1186/s12890-018-0768-4
- BaHammam, A.S., Pandi-Perumal, S.R., Piper, A., Bahammam, S.A., Almeneessier, A.S., Olaish, A.H. and Javaheri, S. (2016), Gender differences in patients with obesity hypoventilation syndrome. J Sleep Res, 25: 445-453. https://doi.org/10.1111/jsr.12400
- Palm A, Midgren B, Janson C, Lindberg E. Gender differences in patients starting long-term home mechanical ventilation due to obesity hypoventilation syndrome. Respir Med. 2016 Jan;110:73-8. doi: 10.1016/j.rmed.2015.11.010
- Iftikhar IH, Roland J. Obesity Hypoventilation Syndrome. Clin Chest Med. 2018 Jun;39(2):427-436. doi: 10.1016/j.ccm.2018.01.006
- Mokhlesi B. Obesity hypoventilation syndrome: a state-of-the-art review. Respir Care. 2010 Oct;55(10):1347-62; discussion 1363-5.
- BaHammam AS. Prevalence, clinical characteristics, and predictors of obesity hypoventilation syndrome in a large sample of Saudi patients with obstructive sleep apnea. Saudi Med J. 2015 Feb;36(2):181-9. doi: 10.15537/smj.2015.2.9991
- Kaw R, Hernandez AV, Walker E, Aboussouan L, Mokhlesi B. Determinants of hypercapnia in obese patients with obstructive sleep apnea: a systematic review and metaanalysis of cohort studies. Chest. 2009 Sep;136(3):787-796. doi: 10.1378/chest.09-0615
- Balachandran JS, Masa JF, Mokhlesi B. Obesity Hypoventilation Syndrome Epidemiology and Diagnosis. Sleep Med Clin. 2014 Sep;9(3):341-347. doi: 10.1016/j.jsmc.2014.05.007
- Harada, Y., Chihara, Y., Azuma, M., Murase, K., Toyama, Y., Yoshimura, C., Oga, T., Nakamura, H., Mishima, M., Chin, K. and (2014), Obesity hypoventilation and PaCO2. Respirology, 19: 1233-1240. https://doi.org/10.1111/resp.12367
- Mokhlesi B, Kryger MH, Grunstein RR. Assessment and management of patients with obesity hypoventilation syndrome. Proc Am Thorac Soc. 2008;5(2):218–225. doi: 10.1513/pats.200708-122MG
- BICKELMANN AG, BURWELL CS, ROBIN ED, WHALEY RD. Extreme obesity associated with alveolar hypoventilation; a Pickwickian syndrome. Am J Med. 1956;21(5):811–818. doi: 10.1016/0002-9343(56)90094-8
- Berg G, Delaive K, Manfreda J, Walld R, Kryger MH. The use of health-care resources in obesity-hypoventilation syndrome. Chest. 2001;120(2):377–383. doi: 10.1378/chest.120.2.377
- Bender R, Trautner C, Spraul M, Berger M. Assessment of excess mortality in obesity. Am J Epidemiol. 1998;147(1):42–48. doi: 10.1093/oxfordjournals.aje.a009365
- Kessler R, Chaouat A, Weitzenblum E, Oswald M, Ehrhart M, Apprill M. Pulmonary hypertension in the obstructive sleep apnoea syndrome prevalence, causes and therapeutic consequences. Eur Respir J. 1996;9(4):787–794. doi: 10.1183/09031936.96.09040787
- Atwood CW, Jr, McCrory D, Garcia JG, Abman SH, Ahearn GS. American College of Chest Physicians Pulmonary artery hypertension and sleep-disordered breathing ACCP evidence-based clinical practice guidelines. Chest. 2004;126(1 Suppl):72S–77S. doi: 10.1378/chest.126.1_suppl.72S
- Sugerman HJ, Baron PL, Fairman RP, Evans CR, Vetrovec GW. Hemodynamic dysfunction in obesity hypoventilation syndrome and the effects of treatment with surgically induced weight loss. Ann Surg. 1988;207(5):604–613. doi: 10.1097/00000658-198805000-00015
- Owens RL. A big problem in the ICU. Initiation of CPAP/bilevel PAP therapy. J Clin Sleep Med. 2014 Oct 15;10(10):1161-2. doi: 10.5664/jcsm.4128
- Zwillich CW, Sutton FD, Pierson DJ, Greagh EM, Weil JV. Decreased hypoxic ventilatory drive in the obesity-hypoventilation syndrome. Am J Med. 1975 Sep;59(3):343-8. doi: 10.1016/0002-9343(75)90392-7
- Ballard, HA, Leavitt, OS, Chin, AC, et al. Perioperative anesthetic management of children with congenital central hypoventilation syndrome and rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation undergoing thoracoscopic phrenic nerve-diaphragm pacemaker implantation. Pediatr Anesth. 2018; 28: 963- 973. https://doi.org/10.1111/pan.13475
- Piper AJ, BaHammam AS, Javaheri S. Obesity Hypoventilation Syndrome: Choosing the Appropriate Treatment of a Heterogeneous Disorder. Sleep Med Clin. 2017 Dec;12(4):587-596. doi: 10.1016/j.jsmc.2017.07.008
- Lemyze, M., Guiot, A., Mallat, J., and Thevenin, D. (2018) The obesity supine death syndrome (OSDS). Obesity Reviews, 19: 550– 556. doi: 10.1111/obr.12655
- Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018 Sep;12(9):755-767. doi: 10.1080/17476348.2018.1506331
- Javaheri S, Simbartl LA. Respiratory determinants of diurnal hypercapnia in obesity hypoventilation syndrome. What does weight have to do with it? Ann Am Thorac Soc. 2014 Jul;11(6):945-50. doi: 10.1513/AnnalsATS.201403-099OC
- Han F, Chen E, Wei H, He Q, Ding D, Strohl KP. Treatment effects on carbon dioxide retention in patients with obstructive sleep apnea-hypopnea syndrome. Chest. 2001 Jun;119(6):1814-9. doi: 10.1378/chest.119.6.1814
- Kelly TM, Jensen RL, Elliott CG, Crapo RO. Maximum respiratory pressures in morbidly obese subjects. Respiration. 1988;54(2):73-7. doi: 10.1159/000195504
- Sampson MG, Grassino K. Neuromechanical properties in obese patients during carbon dioxide rebreathing. Am J Med. 1983 Jul;75(1):81-90. doi: 10.1016/0002-9343(83)91171-3
- Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994 Dec 1;372(6505):425-32. doi: 10.1038/372425a0. Erratum in: Nature 1995 Mar 30;374(6521):479.
- Mateus R Amorim, O Aung, Babak Mokhlesi, Vsevolod Y Polotsky, Leptin-mediated neural targets in obesity hypoventilation syndrome, Sleep, Volume 45, Issue 9, September 2022, zsac153, https://doi.org/10.1093/sleep/zsac153
- O’donnell CP, Schaub CD, Haines AS, Berkowitz DE, Tankersley CG, Schwartz AR, Smith PL. Leptin prevents respiratory depression in obesity. Am J Respir Crit Care Med. 1999 May;159(5 Pt 1):1477-84. doi: 10.1164/ajrccm.159.5.9809025
- Makinodan K, Yoshikawa M, Fukuoka A, Tamaki S, Koyama N, Yamauchi M, Tomoda K, Hamada K, Kimura H. Effect of serum leptin levels on hypercapnic ventilatory response in obstructive sleep apnea. Respiration. 2008;75(3):257-64. doi: 10.1159/000112471
- Phipps PR, Starritt E, Caterson I, Grunstein RR. Association of serum leptin with hypoventilation in human obesity. Thorax. 2002 Jan;57(1):75-6. doi: 10.1136/thorax.57.1.75
- Phipps PR, Starritt E, Caterson I, Grunstein RR. Association of serum leptin with hypoventilation in human obesity. Thorax. 2002 Jan;57(1):75-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1746178/pdf/v057p00075.pdf
- Gudzune KA, Doshi RS, Mehta AK, Chaudhry ZW, Jacobs DK, Vakil RM, Lee CJ, Bleich SN, Clark JM. Efficacy of commercial weight-loss programs: an updated systematic review. Ann Intern Med. 2015 Apr 7;162(7):501-12. doi: 10.7326/M14-2238. Erratum in: Ann Intern Med. 2015 May 19;162(10):739-40
- Kakazu MT, Soghier I, Afshar M, Brozek JL, Wilson KC, Masa JF, Mokhlesi B. Weight Loss Interventions as Treatment of Obesity Hypoventilation Syndrome. A Systematic Review. Ann Am Thorac Soc. 2020 Apr;17(4):492-502. doi: 10.1513/AnnalsATS.201907-554OC
- Masa JF, Benítez ID, Javaheri S, Mogollon MV, Sánchez-Quiroga MÁ, de Terreros FJG, Corral J, Gallego R, Romero A, Caballero-Eraso C, Ordax-Carbajo E, Troncoso MF, González M, López-Martín S, Marin JM, Martí S, Díaz-Cambriles T, Chiner E, Egea C, Barca J, Barbé F, Mokhlesi B; Spanish Sleep Network. Risk factors associated with pulmonary hypertension in obesity hypoventilation syndrome. J Clin Sleep Med. 2022 Apr 1;18(4):983-992. doi: 10.5664/jcsm.9760
- Borel JC, Burel B, Tamisier R, Dias-Domingos S, Baguet JP, Levy P, Pepin JL. Comorbidities and mortality in hypercapnic obese under domiciliary noninvasive ventilation. PLoS One. 2013;8(1):e52006. doi: 10.1371/journal.pone.0052006
- Brennan M, McDonnell MJ, Walsh SM, Gargoum F, Rutherford R. Review of the prevalence, pathogenesis and management of OSA-COPD overlap. Sleep Breath. 2022 Dec;26(4):1551-1560. doi: 10.1007/s11325-021-02540-8
- Dorst, J, Behrendt, G, Ludolph, AC. Non-invasive ventilation and hypercapnia-associated symptoms in amyotrophic lateral sclerosis. Acta Neurol Scand. 2019; 139: 128– 134. https://doi.org/10.1111/ane.13043
- Bauman KA, Kurili A, Schotland HM, Rodriguez GM, Chiodo AE, Sitrin RG. Simplified Approach to Diagnosing Sleep-Disordered Breathing and Nocturnal Hypercapnia in Individuals With Spinal Cord Injury. Arch Phys Med Rehabil. 2016 Mar;97(3):363-71. doi: 10.1016/j.apmr.2015.07.026
- Sankari A, Badr MS. Diagnosis of Sleep Disordered Breathing in Patients With Chronic Spinal Cord Injury. Arch Phys Med Rehabil. 2016 Jan;97(1):176-7. doi: 10.1016/j.apmr.2015.10.085
- Sankari A, Vaughan S, Bascom A, Martin JL, Badr MS. Sleep-Disordered Breathing and Spinal Cord Injury: A State-of-the-Art Review. Chest. 2019 Feb;155(2):438-445. doi: 10.1016/j.chest.2018.10.002
- Sankari A, Bascom A, Oomman S, Badr MS. Sleep disordered breathing in chronic spinal cord injury. J Clin Sleep Med. 2014 Jan 15;10(1):65-72. doi: 10.5664/jcsm.3362
- Mokhlesi B, Tulaimat A, Faibussowitsch I, Wang Y, Evans AT. Obesity hypoventilation syndrome prevalence and predictors in patients with obstructive sleep apnea. Sleep Breath. 2007;11(2):117–124. doi: 10.1007/s11325-006-0092-8
- Harada Y, Chihara Y, Azuma M, Murase K, Toyama Y, Yoshimura C. Obesity hypoventilation syndrome in Japan and independent determinants of arterial carbon dioxide levels. Respirology. 2014;19(8):1233–1240. doi: 10.1111/resp.12367
- Piper AJ, Grunstein RR. Obesity hypoventilation syndrome mechanisms and management. Am J Respir Crit Care Med. 2011;183(3):292–298. doi: 10.1164/rccm.201008-1280CI
- Castro-Añón O, Pérez de Llano LA, De la Fuente Sánchez S, Golpe R, Méndez Marote L, Castro-Castro J, et al. Obesity-hypoventilation syndrome increased risk of death over sleep apnea syndrome. PLoS One. 2015;10(2):e0117808. doi: 10.1371/journal.pone.0117808
- Thomas PS, Cowen ER, Hulands G, Milledge JS. Respiratory function in the morbidly obese before and after weight loss. Thorax. 1989 May;44(5):382-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC461837/pdf/thorax00281-0016.pdf
- Soghier I, Brożek JL, Afshar M, Tamae Kakazu M, Wilson KC, Masa JF, Mokhlesi B. Noninvasive Ventilation versus CPAP as Initial Treatment of Obesity Hypoventilation Syndrome. Ann Am Thorac Soc. 2019 Oct;16(10):1295-1303. doi: 10.1513/AnnalsATS.201905-380OC
- Xu J, Wei Z, Li W, Wang W. Effect of different modes of positive airway pressure treatment on obesity hypoventilation syndrome: a systematic review and network meta-analysis. Sleep Med. 2022 Mar;91:51-58. doi: 10.1016/j.sleep.2022.01.008
- Piper AJ, Wang D, Yee BJ, Barnes DJ, Grunstein RR. Randomised trial of CPAP vs bilevel support in the treatment of obesity hypoventilation syndrome without severe nocturnal desaturation. Thorax. 2008 May;63(5):395-401. doi: 10.1136/thx.2007.081315
- Masa JF, Benítez I, Sánchez-Quiroga MÁ, Gomez de Terreros FJ, Corral J, Romero A, Caballero-Eraso C, Alonso-Álvarez ML, Ordax-Carbajo E, Gomez-Garcia T, González M, López-Martín S, Marin JM, Martí S, Díaz-Cambriles T, Chiner E, Egea C, Barca J, Vázquez-Polo FJ, Negrín MA, Martel-Escobar M, Barbé F, Mokhlesi B; Spanish Sleep Network. Long-term Noninvasive Ventilation in Obesity Hypoventilation Syndrome Without Severe OSA: The Pickwick Randomized Controlled Trial. Chest. 2020 Sep;158(3):1176-1186. doi: 10.1016/j.chest.2020.03.068
- Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA; Positive Airway Pressure Titration Task Force; American Academy of Sleep Medicine. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008 Apr 15;4(2):157-71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2335396
- Gong Y, Sankari A. Noninvasive Ventilation. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK578188
- Wearn J, Akpa B, Mokhlesi B. Adherence to Positive Airway Pressure Therapy in Obesity Hypoventilation Syndrome. Sleep Med Clin. 2021 Mar;16(1):43-59. doi: 10.1016/j.jsmc.2020.10.009
- Banerjee D, Yee BJ, Piper AJ, Zwillich CW, Grunstein RR. Obesity hypoventilation syndrome: hypoxemia during continuous positive airway pressure. Chest. 2007 Jun;131(6):1678-84. doi: 10.1378/chest.06-2447
- Kaw R, Doufas AG. Is regular oxygen supplementation safe for obese postoperative patients? Cleve Clin J Med. 2020 Nov 23;87(12):723-727. doi: 10.3949/ccjm.87a.19051
- Wijesinghe M, Williams M, Perrin K, Weatherall M, Beasley R. The effect of supplemental oxygen on hypercapnia in subjects with obesity-associated hypoventilation: a randomized, crossover, clinical study. Chest. 2011 May;139(5):1018-1024. doi: 10.1378/chest.10-1280
- Angrisani L, Santonicola A, Iovino P, et al. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obesity Surgery. 2018;28(12):3783–3794. doi: 10.1007/s11695-018-3450-2
- Greenburg DL, Lettieri CJ, Eliasson AH. Effects of surgical weight loss on measures of obstructive sleep apnea: a meta-analysis. Am J Med. 2009 Jun;122(6):535-42. doi: 10.1016/j.amjmed.2008.10.037
- Fernandez AZ Jr, Demaria EJ, Tichansky DS, Kellum JM, Wolfe LG, Meador J, Sugerman HJ. Multivariate analysis of risk factors for death following gastric bypass for treatment of morbid obesity. Ann Surg. 2004 May;239(5):698-702; discussion 702-3. doi: 10.1097/01.sla.0000124295.41578.ab
- Ebeo CT, Benotti PN, Byrd RP Jr, Elmaghraby Z, Lui J. The effect of bi-level positive airway pressure on postoperative pulmonary function following gastric surgery for obesity. Respir Med. 2002 Sep;96(9):672-6. doi: 10.1053/rmed.2002.1357
- Huerta S, DeShields S, Shpiner R, Li Z, Liu C, Sawicki M, Arteaga J, Livingston EH. Safety and efficacy of postoperative continuous positive airway pressure to prevent pulmonary complications after Roux-en-Y gastric bypass. J Gastrointest Surg. 2002 May-Jun;6(3):354-8. doi: 10.1016/s1091-255x(01)00048-8
- Camacho, M., Teixeira, J., Abdullatif, J., Acevedo, J.L., Certal, V., Capasso, R. and Powell, N.B. (2015), Maxillomandibular Advancement and Tracheostomy for Morbidly Obese Obstructive Sleep Apnea. Otolaryngology–Head and Neck Surgery, 152: 619-630. https://doi.org/10.1177/0194599814568284
- Ginter G, Sankari A, Eshraghi M, Obiakor H, Yarandi H, Chowdhuri S, Salloum A, Badr MS. Effect of acetazolamide on susceptibility to central sleep apnea in chronic spinal cord injury. J Appl Physiol (1985). 2020 Apr 1;128(4):960-966. doi: 10.1152/japplphysiol.00532.2019
- Poulter NR, Chang CL, Farley TM, Meirik O. Risk of cardiovascular diseases associated with oral progestagen preparations with therapeutic indications. Lancet. 1999 Nov 6;354(9190):1610. doi: 10.1016/s0140-6736(99)03132-3
- Maresh S, Prowting J, Vaughan S, Kruppe E, Alsabri B, Yarandi H, Badr MS, Sankari A. Buspirone decreases susceptibility to hypocapnic central sleep apnea in chronic SCI patients. J Appl Physiol (1985). 2020 Oct 1;129(4):675-682. doi: 10.1152/japplphysiol.00435.2020
- Prowting J, Maresh S, Vaughan S, Kruppe E, Alsabri B, Badr MS, Sankari A. Mirtazapine reduces susceptibility to hypocapnic central sleep apnea in males with sleep-disordered breathing: a pilot study. J Appl Physiol (1985). 2021 Jul 1;131(1):414-423. doi: 10.1152/japplphysiol.00838.2020
- Ahmad B, Sankari A, Eshraghi M, Aldwaikat A, Yarandi H, Zeineddine S, Salloum A, Badr MS. Effect of Zolpidem on nocturnal arousals and susceptibility to central sleep apnea. Sleep Breath. 2023 Mar;27(1):173-180. doi: 10.1007/s11325-022-02593-3
- Mosbah H, Vantyghem MC, Nobécourt E, et al. Therapeutic indications and metabolic effects of metreleptin in patients with lipodystrophy syndromes: Real-life experience from a national reference network. Diabetes Obes Metab. 2022 Aug;24(8):1565-1577. doi: 10.1111/dom.14726
- Marik PE, Chen C. The clinical characteristics and hospital and post-hospital survival of patients with the obesity hypoventilation syndrome: analysis of a large cohort. Obes Sci Pract. 2016 Mar;2(1):40-47. doi: 10.1002/osp4.27