What is pink eye
Pink eye is also called conjunctivitis or red eye. Pink eye involves inflammation or infection of the outer layer of the eye, the transparent membrane (conjunctiva) that lines inside your eyelid and covers the white part of your eyeball. When small blood vessels in the conjunctiva become inflamed, they’re more visible. This is what causes the whites of your eyes to appear reddish or pink. Pink eye (conjunctivitis) can cause swelling, itching, burning, discharge, and redness. Pink eye is an eye condition that is caused by infection or allergies. Pink eye (conjunctivitis) usually gets better in a couple of weeks without treatment.
Pink eye is commonly caused by a bacterial or viral infection, an allergic reaction, or — in babies — an incompletely opened tear duct.
Though pink eye can be irritating, it rarely affects your vision. Treatments can help ease the discomfort of pink eye. Because pink eye can be contagious, early diagnosis and treatment can help limit its spread.
Check if you have conjunctivitis
Pink eye (conjunctivitis) usually affects both eyes and makes them:
- bloodshot
- burn or feel gritty
- produce pus that sticks to lashes
- itch
- water
What causes pink eye:
- Bacterial infection. Bacterial conjunctivitis is the second most common cause and is responsible for the majority (50%-75%) of cases in children; it is observed more frequently from December through April.
- Viral infection. Viral conjunctivitis is the most common cause of infectious conjunctivitis both overall and in the adult population and is more prevalent in summer.
- Allergies. Allergic conjunctivitis is the most frequent cause, affecting 15% to 40% of the population and is observed more frequently in spring and summer.
- Substances that cause irritation
- Contact lens products, eye drops, or eye ointments
- A chemical splash in the eye
- A foreign object in the eye
- In newborns, a blocked tear duct
Pink eye usually does not affect vision. Infectious pink eye can easily spread from one person to another. The infection will clear in most cases without medical care, but bacterial pinkeye needs treatment with antibiotic eye drops or ointment.
There are serious eye conditions that can cause eye redness. These conditions may cause eye pain, a feeling that something is stuck in your eye (foreign body sensation), blurred vision and light sensitivity. If you experience these symptoms, seek urgent care.
Make an appointment with your doctor if you notice any signs or symptoms you think might be pink eye. Pink eye can be highly contagious for as long as two weeks after signs and symptoms begin. Early diagnosis and treatment can protect people around you from getting pink eye too.
People who wear contact lenses need to stop wearing their contacts as soon as pink eye symptoms begin. If your symptoms don’t start to get better within 12 to 24 hours, make an appointment with your eye doctor to make sure you don’t have a more serious eye infection related to contact lens use.
See your doctor for advice if you have a pink eye that doesn’t start to improve after a few days.
Contact your doctor immediately or go to your nearest accident and emergency department if:
- you have a painful pink eye or red eye
- you have other symptoms, including any changes in your vision like wavy lines or flashing, sensitivity to light (photophobia), a severe headache and feeling sick
- you’ve recently injured your eye, particularly if something has pierced it
- your baby has red eyes – get an urgent medical care if your baby is less than 28 days old
- you wear contact lenses and have conjunctivitis symptoms as well as spots on your eyelids – you might be allergic to the lenses
- your symptoms haven’t cleared up after 2 weeks
- sensitivity to light
- intense redness in one eye or both eyes
Home remedies for pink eye
Pink eye treatment is usually focused on symptom relief. Your doctor may recommend using artificial tears, cleaning your eyelids with a wet cloth, and applying cold or warm compresses several times daily.
Use clean cotton wool (one piece for each eye). Boil water and then let it cool down before you:
- gently rub your eye lashes to clean off crusts
- hold a cold flannel on your eyes for a few minutes to cool them down
If you wear contact lenses, you’ll be advised to stop wearing them until treatment is complete. Your doctor will likely recommend that you throw out contacts you’ve worn if your lenses are disposable.
Disinfect hard lenses overnight before you reuse them. Ask your doctor if you should discard and replace your contact lens accessories, such as the lens case used before or during the illness. Also replace any eye makeup used before your illness.
In most cases, you won’t need antibiotic eyedrops. Since conjunctivitis is usually viral, antibiotics won’t help, and may even cause harm by reducing their effectiveness in the future or causing a medication reaction. Instead, the virus needs time to run its course — up to two or three weeks.
Stop infectious conjunctivitis from spreading
DO
- wash hands regularly with warm soapy water
- wash pillows and face cloths in hot water and detergent
DON’T
- wear contact lenses until your eyes are better
- share towels and pillows
- rub your eyes
Staying away from work or school
You don’t need to avoid work or school unless you or your child are feeling very unwell.
Pink eye complications
In both children and adults, pink eye can cause inflammation in the cornea that can affect vision. Prompt evaluation and treatment by your doctor can reduce the risk of complications.
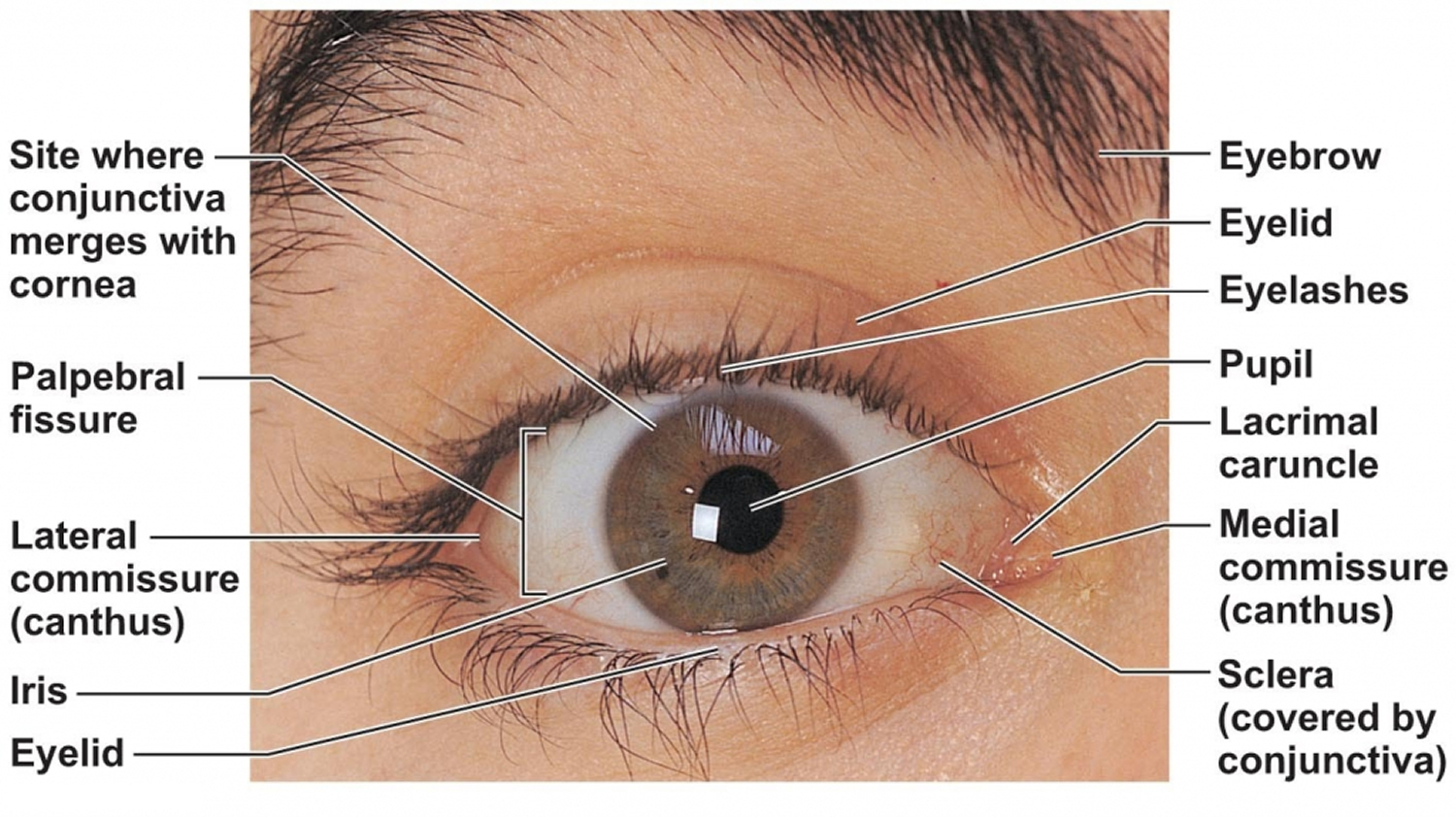
Figure 1. Human eye
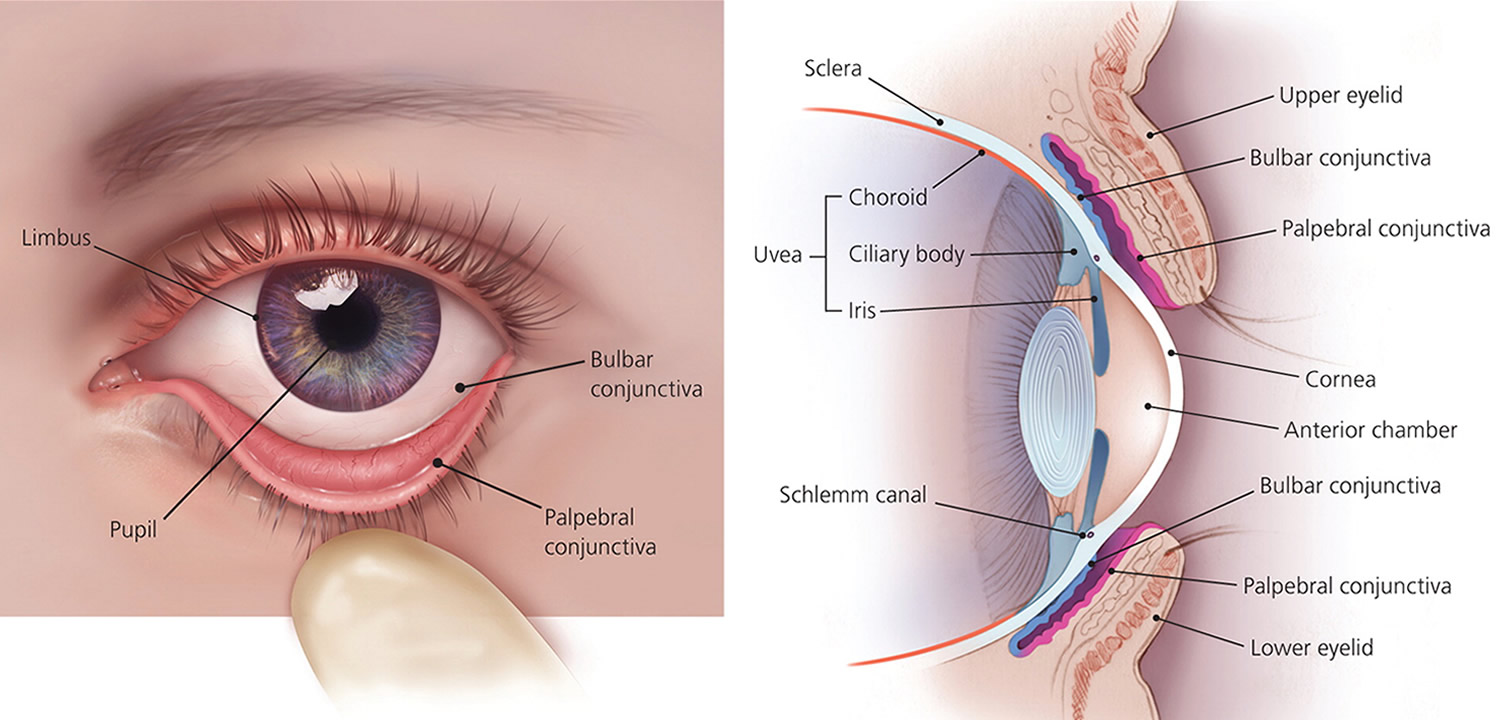
Figure 2. Eye anatomy
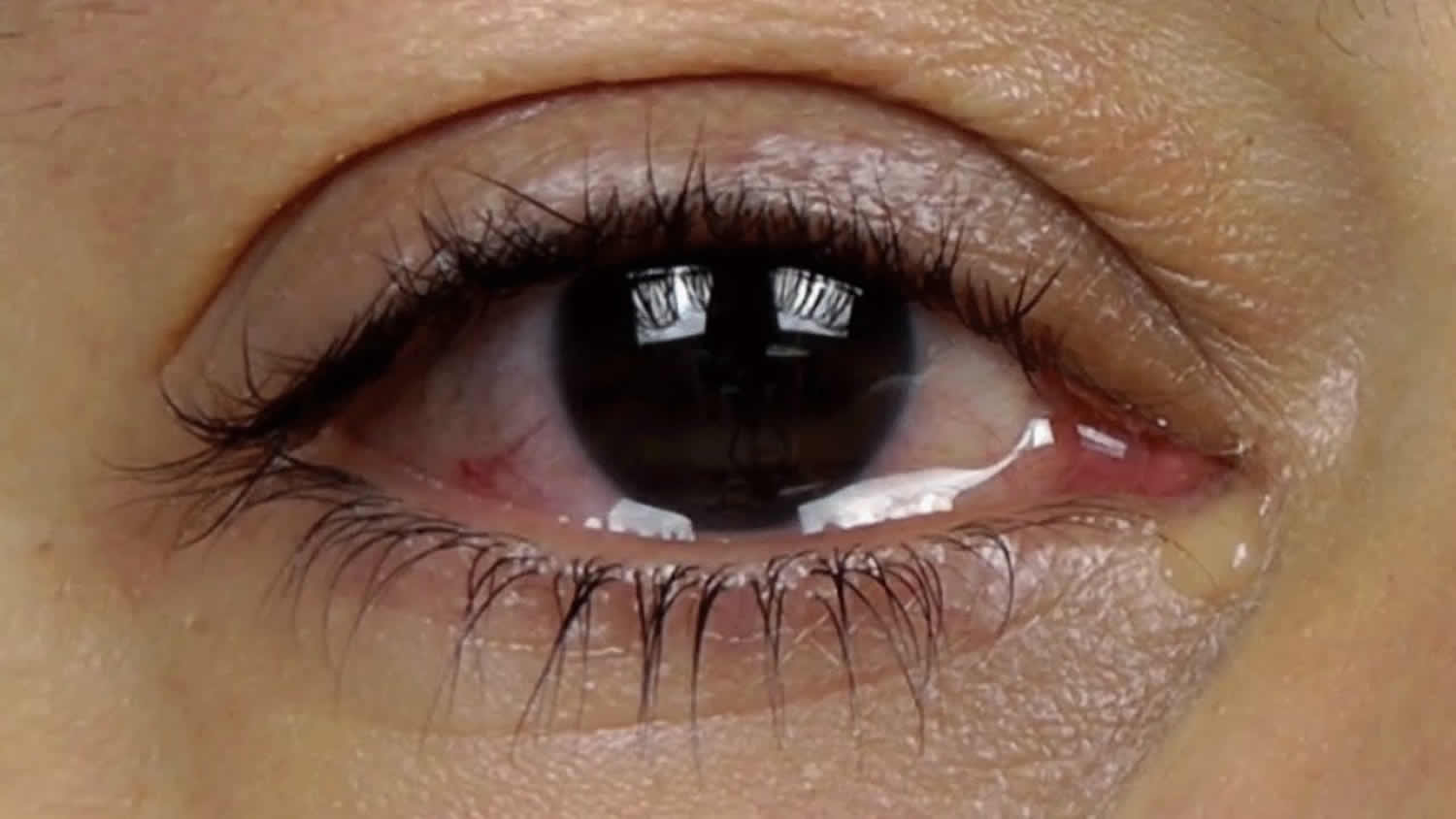
Figure 4. If your eyes are red and feel gritty, the pink eye is also usually contagious
Figure 5. Pink eye caused by allergies like hay fever makes eyes red and watery but isn’t contagious
What causes pink eye
Conjunctivitis can be divided into infectious and noninfectious causes. Most cases of pink eye are caused by a virus, however, viruses and bacteria are the most common infectious causes 1. Both viral and bacterial conjunctivitis can occur along with common cold or symptoms of a respiratory infection, such as a sore throat. Wearing contact lenses that aren’t cleaned properly or aren’t your own can cause bacterial conjunctivitis. Both viral and bacterial conjunctivitis are very contagious. They are spread through direct or indirect contact with the liquid that drains from the eye of someone who’s infected. One or both eyes may be affected.
- Bacterial conjunctivitis causes:
- Acute and subacute bacterial causes includes:
- Neisseria gonorrhoeae
- Neisseria meningitidis
- Streptococcus pneumonia
- Haemophilus influenzae
- Chronic conjunctivitis:
- Staphylococus aureus
- Moraxella lacunata
- Less common causes includes:
- Streptococcus
- Moraxella catarrhalis
- Corynebacterium diphtheriae
- Mycobacterium tuberculosis
- Chlamydia trachomatis
- Acute and subacute bacterial causes includes:
- Viral conjunctivitis:
- Acute viral follicular conjunctivitis
- Chronic viral follicular conjunctivitis
- Viral blepharoconjunctivitis
- Rickettsia
- Fungus
- Parasitic conjunctivitis
- Allergic conjunctivitis causes
- Toxic
- Idoxuridine
- Brimonidine
- Apraclonidine
- Dipivefrin
- Contact lens solution
- Secondary to systemic causes
- Immune-mediated diseases and neoplastic processes.
Allergic conjunctivitis
Allergic conjunctivitis affects both eyes and is a response to an allergy-causing substance such as pollen in seasonal allergic conjunctivitis or a persistent allergen (e.g. house dust mite) in perennial allergic conjunctivitis. In response to allergens, your body produces an antibody called immunoglobulin E (IgE). This antibody triggers special cells called mast cells in the mucous lining of your eyes and airways to release inflammatory substances, including histamines. Your body’s release of histamine can produce a number of allergy signs and symptoms, including red or pink eyes.
All clinical forms of allergic conjunctivitis present with symptoms like redness, watering, discharge, and discomfort or sometimes pain of the eyes and, most importantly, with ocular itching, which is unusual in non-allergic eye conditions. Visual disturbance is usually minimal except in the more severe disorders and patients may also complain of swelling of the lids.
Many patients with allergic conjunctivitis will have a history of current or previous non-ocular allergic or atopic conditions (ezcema, asthma, urticaria, rhinitis).
If you have allergic conjunctivitis, you may experience intense itching, tearing and inflammation of the eyes — as well as sneezing and watery nasal discharge. Most allergic conjunctivitis can be controlled with allergy eyedrops.
Seasonal allergic conjunctivitis is a type 1 hypersensitivity response with conjunctival activated mast cells as a direct result of allergen cross-linking of surface IgE receptors resulting in degranulation and release of histamine, leukotrienes, proteases, prostaglandins, cytokines, and chemokines. All these substances induce vascular leakage, resulting in further cellular infiltration of eosinophils and neutrophils and edema but little or no T-cell infiltration is observed.
In perennial allergic conjunctivitis, the conjunctival tissue is infiltrated by eosinophils, neutrophils, and a small number of T cells, probably recruited as a result of the release of chemokines that attract these cells to the site of inflammation during the persistent, allergen-driven inflammatory response.
Bacterial conjunctivitis
Sometimes, bacterial conjunctivitis can be contracted directly of infected individuals, or by an abnormal proliferation of the native conjunctival flora, or can result from the spread of infection from the organisms colonizing the patient’s own nasal and sinus mucosa. Bacteria infiltrate the conjunctival epithelial layer and sometimes the substantia propia as well.
Direct infection and inflammation of the conjunctival surface, bystander effects on adjacent tissues such as the cornea, and the host’s acute inflammatory response and long-term reparative response all contribute to the pathology
The most common pathogens for bacterial conjunctivitis in adults are staphylococcal species, followed by Streptococcus pneumoniae and Haemophilus influenzae.
In children, the disease is often caused by H influenzae , S pneumoniae , and Moraxella catarrhalis.
The course of bacterial conjunctivitis usually lasts 7 to 10 day.
- Hyperacute bacterial is often caused by Neisseria gonorrhoeae. When Conjunctivitis not responding to standard antibiotic therapy in sexually active patients a chlamydial infection should be suspected. Hyperacute bacterial conjunctivitis has a period of incubation and communicability estimated to be 1 to 7 days.
- Chronic bacterial conjunctivitis is used to describe any conjunctivitis lasting more than 4 weeks. It has an incubation period from 2 to 7 days. Chronic bacterial is commonly caused Staphylococcus aureus, Moraxellalacunata, and enteric bacteria.
Viral conjunctivitis
Adenoviral conjunctivitis
Viral conjunctivitis secondary to adenoviruses is highly contagious, and the risk of transmission has been estimated to be 10% to 50%. Patients commonly refer contact with an individual with red eye or they may have a history of recent symptoms of an upper respiratory tract infection.
Incubation is estimated to be 5 to 12 days and communicability is about 10 to 14 days.
Between 65% and 90% of cases of viral conjunctivitis are caused by adenoviruses, and they produce 2 of the common clinical entities associated with viral conjunctivitis, pharyngoconjunctival fever, and epidemic keratoconjunctivitis.
- Pharyngoconjunctival fever is characterized by abrupt onset of high fever, pharyngitis, and bilateral conjunctivitis, and by periauricular lymph node enlargement.
- Epidemic keratoconjunctivitis is more severe and presents with watery discharge, hyperemia, chemosis, and ipsilateral lymphadenopathy. Lymphadenopathy is observed in up to 50% of viral conjunctivitis cases and is more prevalent in viral conjunctivitis compared with bacterial conjunctivitis
Herpes virus conjunctivitis
Herpes simplex virus comprises 1.3% to 4.8% of all cases of acute conjunctivitis and conjunctivitis caused by the virus is usually unilateral.
Primary HSV- l infection in humans occurs as a nonspecific upper respiratory tract infection. Herpes simplex virus spreads from infected skin and mucosal epithelium via sensory nerve axons to establish latent infection in associated sensory cranial nerve 5 (Trigeminal nerve) and it´s ganglia. Latent infection of the trigeminal ganglion occurs in the absence of recognized primary infection, and reactivation of the virus may follow any of the 3 branches.
When primary ocular herpes simplex virus infection occurs, the patient typically manifests unilateral discharge, thin and watery, and sometimes accompanying vesicular eyelid lesions.
In a small percentage, there is history of external ocular herpes simplex virus infection that may lead to the diagnosis.
Conjunctivitis resulting from irritation
Irritation from a chemical splash or foreign object in your eye is also associated with conjunctivitis. Sometimes flushing and cleaning the eye to rid it of the chemical or object causes redness and irritation. Signs and symptoms, which may include watery eyes and a mucous discharge, usually clear up on their own within about a day.
Risk Factors for developing conjunctivitis
Bacterial conjunctivitis
- Contact with contaminated fingers, fomites or oculo-genital contact with someone infected
- Young, sexually active adults below age 25 years, have a high risk, especially if they do not use condom on sexual encounters.
- Newborns the eyes can be infected after vaginal delivery by infected mothers
- Compromised tear production
- Disruption of the natural epithelial barrier
- Abnormality of adnexal structures
- Trauma
- Immunosuppressed status
Viral conjunctivitis
Direct contact with:
- Contaminated fingers
- Medical instruments
- Swimming pool water
- Personal items from an infected person
Allergic conjunctivitis
- History of current or previous non-ocular allergic or atopic conditions (ezcema, asthma, urticaria, rhinitis).
If you’re not sure it’s conjunctivitis
The following information aims to give you a better idea about what might be causing your red eye. But it shouldn’t be used to self-diagnose your condition.
- Always see a doctor for a proper diagnosis and treatment!
Common causes of a painless pink eye (red eye)
The most likely causes of a painless pink eye are minor problems such as conjunctivitis or a burst blood vessel. These conditions don’t tend to affect your vision and usually get better within a week or two.
Conjunctivitis
- Conjunctivitis causes the blood vessels on the eye to swell, making one or both eyes look bloodshot and feel gritty.
- Other symptoms can include itchiness and watering of the eyes, and a sticky coating on the eyelashes.
- Conjunctivitis can be caused by an infection, an allergy (for example, to pollen), or an irritant like chlorine or dust.
- Treatment will depend on what’s causing the condition. Sometimes treatment isn’t needed because it may get better on its own.
Burst blood vessel in the eye
Straining, coughing or injuring your eye can sometimes cause a blood vessel to burst on the surface of the eye, resulting in a bright red blotch.
It can look alarming, particularly if you’re taking medication like aspirin or warfarin as these reduce the blood’s ability to clot, which can exaggerate the redness, but it’s not usually serious and should clear up on its own within a few weeks.
Figure 6. Pink eye caused by subconjunctival hemorrhage
Common causes of a painful pink eye (red eye)
If your pink eye is painful or you have other symptoms, such as changes in your vision, it should be assessed by a doctor as soon as possible.
Uveitis
- Uveitis is inflammation of the iris, the colored part of the eye. It’s also known as iritis.
- As well as a red eye, your eye may be sensitive to light, your vision may be blurred, and you may have a headache.
- Uveitis usually responds quickly to treatment with steroid medication to reduce the inflammation. It rarely leads to severe problems.
Glaucoma
Glaucoma is an eye condition where the optic nerve, which connects your eye to your brain, becomes damaged.
Your eye will probably be very red and painful, and you may feel sick and see halos around lights. Your vision may be blurred or cloudy.
If your doctor thinks you may have glaucoma, they’ll refer you to an eye specialist called an ophthalmologist immediately. This is because it could lead to a permanent loss of vision if not treated quickly.
Corneal ulcer (ulcer on the cornea)
An ulcer on the cornea, the clear outer layer at the front of the eyeball, can make the eye red and sensitive to light. It can also feel like there’s something in your eye.
People who wear contact lenses have an increased risk of getting bacterial corneal ulcers. Viral corneal ulcers are more likely to affect people who often get cold sores.
If your doctor thinks you have a corneal ulcer, they’ll refer you to an eye specialist for treatment.
A scratch to the cornea or particle in the eye
A red and painful eye can sometimes be caused by a particle, such as a piece of grit, getting in your eye.
If there’s something in your eye, your doctor or a hospital doctor at an A&E department will try to remove it. They’ll first put anaesthetic eye drops into your eye to numb it and reduce further discomfort.
If the particle has scratched your eye, it may feel a bit uncomfortable when the anaesthetic wears off. You may be given antibiotic eye drops or ointment to use for a few days to reduce the risk of infection while it heals.
Pink eye prevention
Preventing the spread of pink eye
Practice good hygiene to control the spread of pink eye. For instance:
- Don’t touch your eyes with your hands.
- Wash your hands often.
- Use a clean towel and washcloth daily.
- Don’t share towels or washcloths.
- Change your pillowcases often.
- Throw away your eye cosmetics, such as mascara.
- Don’t share eye cosmetics or personal eye care items.
The safest way to prevent spreading pink eye is to stay home — or keep your child at home — until eye discharge has stopped. Most schools and child care facilities require that your child wait at least 24 hours after starting treatment before returning to school or child care. Check with your doctor if you have any questions about when your child can return to school or child care.
Keep in mind that pink eye is no more contagious than the common cold. It’s okay to return to work, school or child care if you’re not able to take time off — just stay consistent in practicing good hygiene.
Preventing pink eye in newborns
Newborns’ eyes are susceptible to bacteria normally present in the mother’s birth canal. These bacteria cause no symptoms in the mother. In rare cases, these bacteria can cause infants to develop a serious form of conjunctivitis known as ophthalmia neonatorum, which needs treatment without delay to preserve sight. That’s why shortly after birth, an antibiotic ointment is applied to every newborn’s eyes. The ointment helps prevent eye infection.
Pink eye signs and symptoms
The most common pink eye symptoms include:
- Redness in one or both eyes
- Itchiness in one or both eyes
- A gritty feeling in one or both eyes
- A discharge in one or both eyes that forms a crust during the night that may prevent your eye or eyes from opening in the morning
- Tearing
Bacterial conjunctivitis
Signs and symptoms include red eye, purulent or mucopurulent discharge, and chemosis and presents with a severe copious purulent discharge and decreased vision. There is often accompanying eyelid swelling, eye pain on palpation, and preauricular adenopathy. When conjunctivitis is caused by Neisseria gonorrhoeae carries a high risk for corneal involvement and subsequent corneal perforation.
Bilateral mattering of the eyelids and adherence of the eyelids, lack of itching, and no history of conjunctivitis are strong positive predictors of bacterial conjunctivitis
Severe purulent discharge should always be cultured.
The possibility of bacterial keratitis is high in contact lens wearers, who should be treated with topical antibiotics and referred to an ophthalmologist. A patient wearing contact lenses should be asked to immediately remove them
Viral conjunctivitis
Conjunctivitis caused by adenoviruses:
- Pharyngoconjunctival fever presents by abrupt onset of high fever, pharyngitis, and bilateral conjunctivitis, and by periauricular lymph node enlargement.
- Epidemic keratoconjunctivitis is more severe and presents with watery discharge, conjunctival membranes or pseudo membranes, hyperemia, chemosis, and ipsilateral lymphadenopathy. Lymphadenopathy is observed in up to 50% of viral conjunctivitis cases and is more prevalent in viral conjunctivitis compared with bacterial conjunctivitis
Herpes Virus conjunctivitis
- The eyelids often are edematous and ecchymotic.
- Cutaneous or eyelid margin vesicles, or ulcers on the bulbar conjunctiva
- The cornea often demonstrates a punctate epitheliopathy.. In severe cases, there can be a corneal epithelial defect (Dendritic epithelial keratitis). It typically begins in one eye and progresses to the fellow eye over a few days.
- It is important to note that conjunctivitis caused by Herpes virus do not form conjunctival membranes or pseudo membranes.
- Herpes zoster virus can involve ocular tissue, especially if the first and second branches of the trigeminal nerve are involved. Eyelids (45.8%) are the most common site of ocular involvement, followed by the conjunctiva. Corneal complication and uveitis may be present in 38.2% and 19.1% of cases, respectively. Severe forms include those presenting with Hutchinson sign (vesicles at the tip of the nose, which has high correlations with corneal involvement)
Allergic conjunctivitis
Classic ocular signs of allergic inflammation are lid swelling, diffuse conjunctival redness, and mild swelling, which often combine to give a pink rather than red color, and a velvety thickening and redness of the tarsal conjunctiva with the presence of fine excrescences called papillae, which may vary from tiny pinprick size to giant papillae which are >1 mm in diameter and give a cobblestone appearance under the lid. Macroscopic noticeable swelling of the conjunctiva, called ‘chemosis’, is sometimes seen. Other signs, such as dermatitis of the lid skin, inflammation of the lid margin (blepharitis), conjunctival scarring, and involvement of the cornea occur only in certain of the most severe disorders. When the limbus becomes inflamed might presents a pale-pink coloration in an annular pattern or with characteristic white dots called Trantas Dot’s
Clinical presentation of disease subtypes:
- Seasonal and perennial allergic conjunctivitis
- Atopic keratoconjunctivitis
- Vernal keratoconjunctivitis
- Giant papillary conjunctivitis
Pink eye diagnosis
In most cases, your doctor can diagnose pink eye by asking questions about your symptoms and recent health history and performing a physical examination of your eyes.
Rarely, your doctor may also take a sample of the liquid that drains from your eye for laboratory analysis (culture). A culture may be needed if your symptoms are severe or if your doctor suspects a high-risk cause, such as a foreign body in your eye, a serious bacterial infection or a sexually transmitted infection.
Pink eye treatment
Treatment will depend on the cause of your pink eye. If it’s a bacterial infection you might be prescribed antibiotics. But these won’t work if it’s caused by a virus (viral conjunctivitis) or an allergy.
Some sexually transmitted infections (STIs) can cause pink eye. This type takes longer to clear up.
Viral conjunctivitis often begins in one eye and then infects the other eye within a few days. Your signs and symptoms should gradually clear on their own. Antiviral medications may be an option if your doctor determines that your viral conjunctivitis is caused by the herpes simplex virus.
Pink eye remedies
To help you cope with the signs and symptoms of pink eye until it goes away, try to:
- Apply a compress to your eyes. To make a compress, soak a clean, lint-free cloth in water and wring it out before applying it gently to your closed eyelids. Generally, a cool water compress will feel the most soothing, but you can also use a warm compress if that feels better to you. If pink eye affects only one eye, don’t touch both eyes with the same cloth. This reduces the risk of spreading pink eye from one eye to the other.
- Try eyedrops. Over-the-counter eyedrops called artificial tears may relieve symptoms. Some eyedrops contain antihistamines or other medications that can be helpful for people with allergic conjunctivitis.
- Stop wearing contact lenses. If you wear contact lenses, you may need to stop wearing them until your eyes feel better. How long you’ll need to go without contact lenses depends on what’s causing your conjunctivitis. Ask your doctor whether you should throw away your disposable contacts, as well as your cleaning solution and lens case. If your lenses aren’t disposable, clean them thoroughly before reusing them.
Treatment for allergic conjunctivitis
If the irritation is allergic conjunctivitis, your doctor may prescribe one of many different types of eyedrops for people with allergies. These may include medications that help control allergic reactions, such as antihistamines and mast cell stabilizers, or drugs that help control inflammation, such as decongestants, steroids and anti-inflammatory drops.
Over-the-counter eyedrops that contain antihistamines and anti-inflammatory medications also may be effective. Ask your doctor if you’re not sure which product to use.
- Topical antihistamines: (Levocabastine, azelastine, and emedastine) these are commonly prescribed in combination with a sympathomimetic vasoconstrictor (e.g. antazoline– naphazoline).
- Oral antihistamines
- Topical mast cell inhibitors: (Cromolyn sodium/chlorphenamine, Nedocromil sodium, Lodoxamide tromethamine, Olopatadine and ketotifen). They offer a preventive action and are most effective if used before the onset of symptoms where possible (e.g. at the beginning of the pollen season as their onset of action is relatively slow (5–7 days) and stinging upon instillation can occur particularly in the presence of active inflammation, patients should be warned that their eyes may initially feel worse.
- Surface-acting steroids (fluorometholone, rimexolone)
- Ciclosporin
You may also reduce the severity of your allergic conjunctivitis symptoms by avoiding whatever causes your allergies when possible.
Treatment for Bacterial conjunctivitis
- Most cases are self-limiting within 1 to 2 weeks of presentation, but in cases caused by highly virulent bacteria, such as Streptococcus pneumonia, Neisseria gonorrhoeae and Haemophilus influenzae might be beneficial reducing the duration of conjunctivitis.
- There are no significant differences among all broad-spectrum antibiotic eyedrops in achieving clinical cure. Factors that influence antibiotic choice are local availability, patient allergies, resistance patterns, and cost.
- Initial medical therapy dosing schedule for acute non-severe bacterial conjunctivitis is 4 times daily for approximately 5- 7 days of any of the following:
- Polymixin combination drops
- Aminoglycosides or fluoroquinolone (ciprofloxacin, ofloxacin, levofloxacin, moxifloxacin, or gatifloxacin) drops
- Bacitracin or ciprofloxacin ointment.
- Topical steroids should be avoided because of the risk of potentially prolonging the course of the disease and potentiating the infection.
- Treatment for hyperacute conjunctivitis secondary to Neisseria gonorrhoeae consists of 1 gram intramuscular Ceftriaxone, only dose and patient should be instructed on how to lavage the infected eye.
- Concurrent chlamydial infection should be managed with either of the following:
- Azithromycin 1000 mg single dose
- Doxycycline 100 mg twice daily for 7 days
- Tetracycline 250 mg four times daily for 7 days
- Erythromycin 500 mg four times daily for 7 days
Treatment for Viral conjunctivitis
Adenoviral conjunctivitis:
- Although no effective treatment exists, artificial tears, topical antihistamines, or cold compresses may be useful in alleviating some of the symptoms
- Topical antibiotics should not be indicated in due they do not protect against secondary infections, and their use may complicate the clinical presentation by causing allergy and toxicity, leading to delay in diagnosis of other possible ocular diseases and they can even increase the risk of spreading the infection to the other eye from a contaminated dropper.
- Complications should be investigated if symptoms do not resolve after 7 to 10 days because of the risk of complications.
Herpes virus conjunctivitis:
Topical and oral antivirals are recommended to shorten the course of the disease.
Acyclovir:
- 3% ophthalmic ointment 200, 400, 800 mg 5x/day for 10 days.
- 200 mg/5 mL suspension, 400 mg 5x/day for 10 days
- 5% dermatologic ointment, 6x/day for 7 days.
Ganciclovir: 0.15% topical ophthalmic gel, 5x/day until epithelium heals; then 3x/day for 7 days
Topical corticosteroids should be avoided because they potentiate the virus and may cause harm.
Herpes Zoster conjunctivitis
Treatment usually consists of a combination of oral antivirals and topical steroids.
References