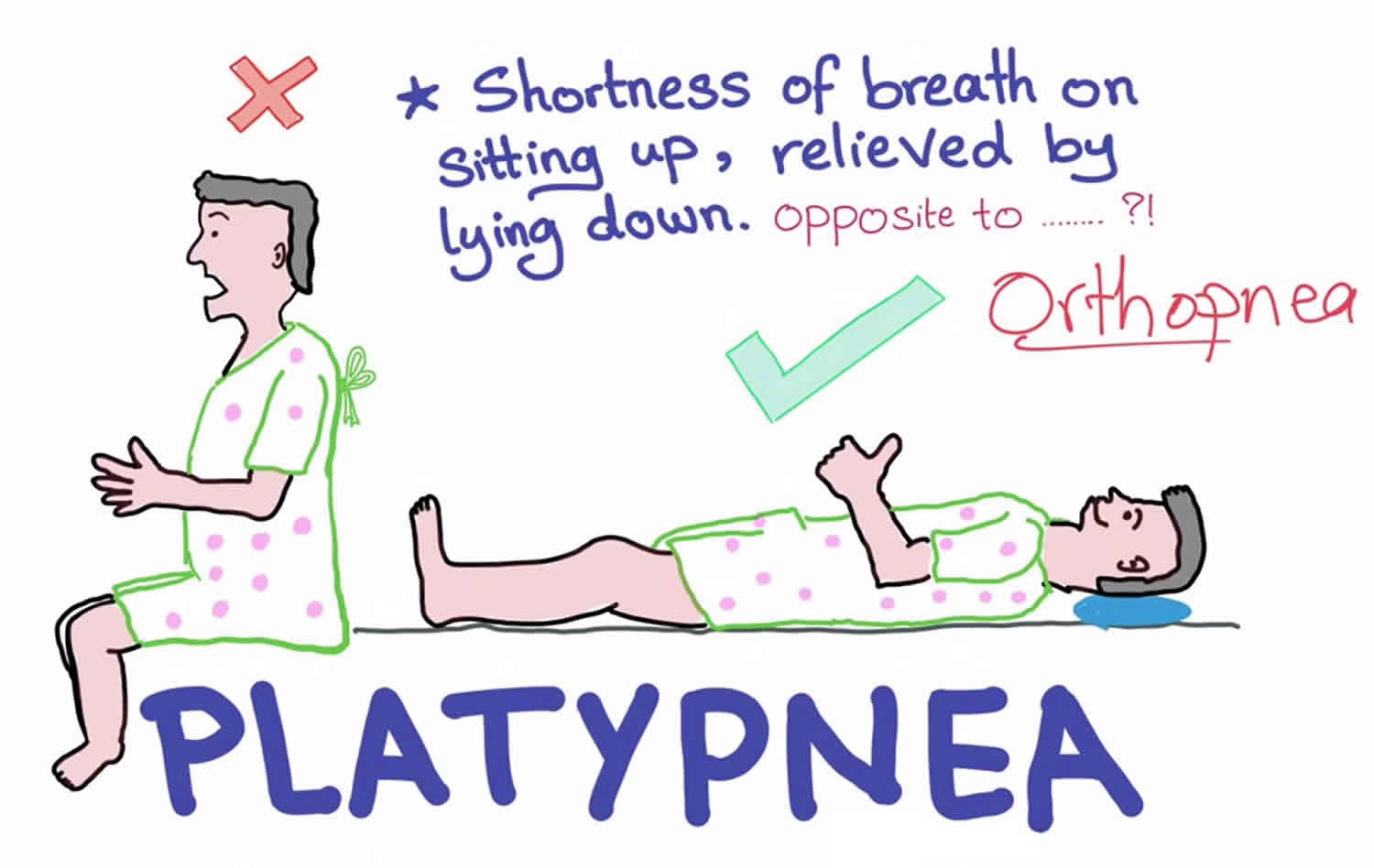
Platypnea
Platypnea, derived from Greek platus meaning flat and pnoia meaning breath, is a descriptive term which means shortness of breath that is worsened by being upright (standing or sitting) and improves when lying supine (flat) 1. In contrast, shortness of breath when lying supine is called orthopnea 2.
Platypnea may co-exist with or be caused by orthodeoxia which is defined as oxygen desaturation in the upright position. Both constitute a syndrome named platypnea-orthodeoxia syndrome 3. Platypnea-Orthodeoxia syndrome is a rare clinical entity that is characterized by positional dyspnea (platypnea) and arterial desaturation (orthodeoxia) while in the upright position 4. The hypoxia in platypnea-orthodeoxia syndrome has been attributed to the mixing of the deoxygenated venous blood with the oxygenated arterial blood via a shunt. The primary mechanisms of platypnea-orthodeoxia syndrome in these patients can be broadly classified based on intracardiac abnormalities, extracardiac abnormalities and miscellaneous etiologies. A patent foramen ovale (PFO) was the most common reported site of an intracardiac shunt. In addition to PFO (patent foramen ovale), intracardiac shunt leading to platypnea-orthodeoxia syndrome has been reported from either an atrial septal defect (ASD) or an atrial septal aneurysm. Most patients with an intracardiac shunt also demonstrated a secondary anatomic or a functional defect. Extracardiac causes of platypnea-orthodeoxia syndrome included intra-pulmonary arteriovenous malformations and lung parenchymal diseases.
No data currently exists to estimate the incidence of platypnea and most cases go undetected unless clinicians specifically ask about the symptoms. Additionally, measuring the degree of dyspnea or the oxygen saturation in the upright and sitting position is not usually part of the routine vital signs measurement or physical examination; hence, positional alterations in oxygenation can be easily overlooked 5.
The diagnosis of platypnea is usually complex and requires a thorough clinical and radiological assessment of the patient.Coordination of care and early involvement of an interprofessional team that includes a pulmonologist, cardiologist, radiologist, and a respiratory therapist is essential for early diagnosis and targeted treatment 6. Ideally, the underlying disorder will be treated, thus eliminating the respiratory symptoms. If this is not possible due to the nature of the underlying disorder, clinical management of platypnea must target patient education and symptom management.
Platypnea key points
- Platypnea is commonly associated with orthodeoxia and both result from diseases that cause intracardiac or extracardiac right-to-left shunting significant enough to cause hypoxia.
- Measuring oxygen saturation in different positions should be performed any time platypnea is reported.
- Treatment of platypnea is directed to the underlying cause.
Platypnea causes
Review articles have classified the cause of platypnea broadly into 2:
Intracardiac Shunts
Patent foramen ovale (PFO), atrial septal defect (ASD) and atrial septal aneurysm (ASA) were listed as the most frequent causes 7.
Extra-Cardiac Causes
Extra-cardiac causes mainly include intra-pulmonary shunts and extra-pulmonary shunts. Pulmonary arteriovenous malformation (AVM), lung parenchymal diseases, and hepato-pulmonary syndrome are examples of pulmonary causes. A few articles described other causes of this condition such as fat embolism, Parkinson disease, among others, but the precise mechanism of those etiologies leading to platypnea remained controversial and elusive 8.
Platypnea pathophysiology
The pathophysiology of platypnea is not completely understood, but it appears that the condition occurs in patients with disorders that increase the positional right-to-left shunting through intrapulmonary or intracardiac shunts. This right-to-left shunt could be transient and related to conditions that may worsen right-to-left shunting (like pulmonary hypertension or various other disorders). For example, platypnea may occur in patients with intracardiac right-to-left shunts such as atrial septal defect (ASD) or patent foramen ovale (PFO) after developing a disorder that increases the shunting such as pulmonary hypertension, pulmonary embolism, following a pneumonectomy, or having a large pericardial effusion. Intrapulmonary right-to-left shunts occur mainly in the base of lungs in patients with hepatopulmonary syndrome. Being in the upright position causes more blood to flow to the lung base, thus aggravating shunting 7.
Platypnea may also result from worsening ventilation-perfusion mismatch in patients with underlying lung disease especially if the disease is worse at the base of the lung. Many case reports cite such a presentation. For example, patients with idiopathic pulmonary fibrosis may have platypnea-orthodeoxia in the upright position because the fibrosis primarily occurs at the base of the lungs compared to apices 9.
In the upright position, the blood (perfusion) is directed mainly towards diseased areas resulting in worsening ventilation-perfusion ratio that will improve when lying flat. The same alteration may occur with other lung diseases, such as basilar pneumonia because the disease primarily affects the base of the lung.
Shunt fraction of total cardiac output (Qs/Qt) can be calculated by supplying the patient with 100% oxygen for 20 to 30 minutes then using this equation 10:
- Qs/Qt (Shunt Fraction): (CcO2 – CaO2) / (CcO2 – CvO2)
Where CcO2 is the end capillary O2 content; CaO2 is the oxygen content of the arterial blood, and CvO2 is the oxygen content of the mixed venous blood. In normal people, the shunt fraction is about 5%.
Platypnea symptoms
Platypnea is a descriptive term which means shortness of breath that is worsened by being upright (standing or sitting) and improves when lying supine (flat) 1. Platypnea is a symptom and not a disease, so once found, a careful history and physical examination should focus on finding the underlying disease that may predispose to it 6. Some of the findings that one should look for include:
- Vital signs in orthodeoxia: Not responding to oxygen administration may be related to the presence of a right-to-left shunt.
- Assessment for spider nevi, palmar erythema, ascites, edema, etc. may be signs of chronic liver disease.
- Heart exam for any murmurs that may suggest a shunt.
- Lung exam for underlying lung disease (exam will vary based on disease, for example, velcro crackles in patients with idiopathic pulmonary fibrosis).
Platypnea diagnosis
Laboratory tests should be directed to the possible underlying etiology. For example, laboratory studies to evaluate for suspected liver disease 5.
Echocardiogram with agitated saline bubble study is a very useful initial test to evaluate the presence of intracardiac or extra-cardiac shunts. The appearance of microbubbles in the left atrium during the first 3 beats after opacification of the right chambers suggests an intracardiac shunt whereas the appearance of microbubbles in the left side after more than 3 to 6 beats suggests an extracardiac shunt, for example, an intrapulmonary shunt like in hepatopulmonary syndrome). A Valsalva maneuver may help increase the right-to-left shunting. Other tests to evaluate shunts include a contrast-enhanced echocardiogram, macroaggregated albumin scintigraphy scan, and an invasive angiogram 11.
Chest plain radiograph may show some underlying lung disease that can explain the platypnea, but this test may not be sensitive 12.
CT scan in case of suspected lung abnormality may give further details. For example, CT with contrast may show arteriovenous malformations that are causing the right-to-left shunt.
Platypnea treatment
Platypnea is a symptom; therefore, management should be directed toward the underlying disorder. The following general managements apply:
- Supplemental oxygen should be provided to all hypoxic patients.
Examples of managing causative disorders include:
- Hepatopulmonary syndrome: The only definitive treatment for cirrhotic patients with hepatopulmonary syndrome is liver transplantation. Supportive management should be provided waiting for transplantation 13.
- Lung disease: Management depends on the underlying disease, but examples include antibiotics for pneumonia, embolotherapy for large pulmonary arteriovenous malformations and disease-specific treatment for patients with interstitial lung disease 14.
- Intracardiac shunts: PFO usually does not require any treatment as it may present in up to 25% of people. If the patient is symptomatic with platypnea-orthodeoxia or to prevent paradoxical embolic stroke, then device closure may be an option. Consultation with a cardiologist and cardiovascular surgeon is often required for the management of other intracardiac shunts 6.
Platypnea prognosis
The clinical outcomes of platypnea depend on identifying the underlying etiology.
References- Khauli S, Mahmoud N. Platypnea. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534834
- Agrawal A, Palkar A, Talwar A. The multiple dimensions of Platypnea-Orthodeoxia syndrome: A review. Respir Med. 2017 Aug;129:31-38. https://doi.org/10.1016/j.rmed.2017.05.016
- Altman M, Robin ED. Platypnea (diffuse zone I phenomenon?). N. Engl. J. Med. 1969 Dec 11;281(24):1347-8.
- The multiple dimensions of Platypnea-Orthodeoxia syndrome: A review. Respiratory Medicine Volume 129, August 2017, Pages 31-38 https://doi.org/10.1016/j.rmed.2017.05.016
- Rodrigues P, Palma P, Sousa-Pereira L. Platypnea-orthodeoxia syndrome in review: defining a new disease?. Cardiology. 2012;123(1):15-23.
- Cheng TO. Platypnea-orthodeoxia syndrome: etiology, differential diagnosis, and management. Catheter Cardiovasc Interv. 1999 May;47(1):64-6.
- Cheng TO. Mechanisms of platypnea-orthodeoxia: what causes water to flow uphill? Circulation. 2002 Feb 12;105(6):e47
- Lee CH, Cheng ST. Shortness of breath while sitting up: hepatopulmonary syndrome. CMAJ. 2011 Jan 11;183(1):80
- Rodríguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome–a liver-induced lung vascular disorder. N. Engl. J. Med. 2008 May 29;358(22):2378-87.
- Glenny RW. Teaching ventilation/perfusion relationships in the lung. Adv Physiol Educ. 2008 Sep;32(3):192-5.
- Soliman OI, Geleijnse ML, Meijboom FJ, Nemes A, Kamp O, Nihoyannopoulos P, Masani N, Feinstein SB, Ten Cate FJ. The use of contrast echocardiography for the detection of cardiac shunts. Eur J Echocardiogr. 2007 Jun;8(3):S2-12.
- White RI, Mitchell SE, Barth KH, Kaufman SL, Kadir S, Chang R, Terry PB. Angioarchitecture of pulmonary arteriovenous malformations: an important consideration before embolotherapy. AJR Am J Roentgenol. 1983 Apr;140(4):681-6.
- Akin E, Krüger U, Braun P, Stroh E, Janicke I, Rezwanian R, Akin I, Schöls WH. The platypnea-orthodeoxia syndrome. Eur Rev Med Pharmacol Sci. 2014;18(18):2599-604.
- Reynaud-Gaubert M, Thomas P, Gaubert JY, Pietri P, Garbe L, Giudicelli R, Orehek J, Fuentes P. Pulmonary arteriovenous malformations: lung transplantation as a therapeutic option. Eur. Respir. J. 1999 Dec;14(6):1425-8.