Porencephaly
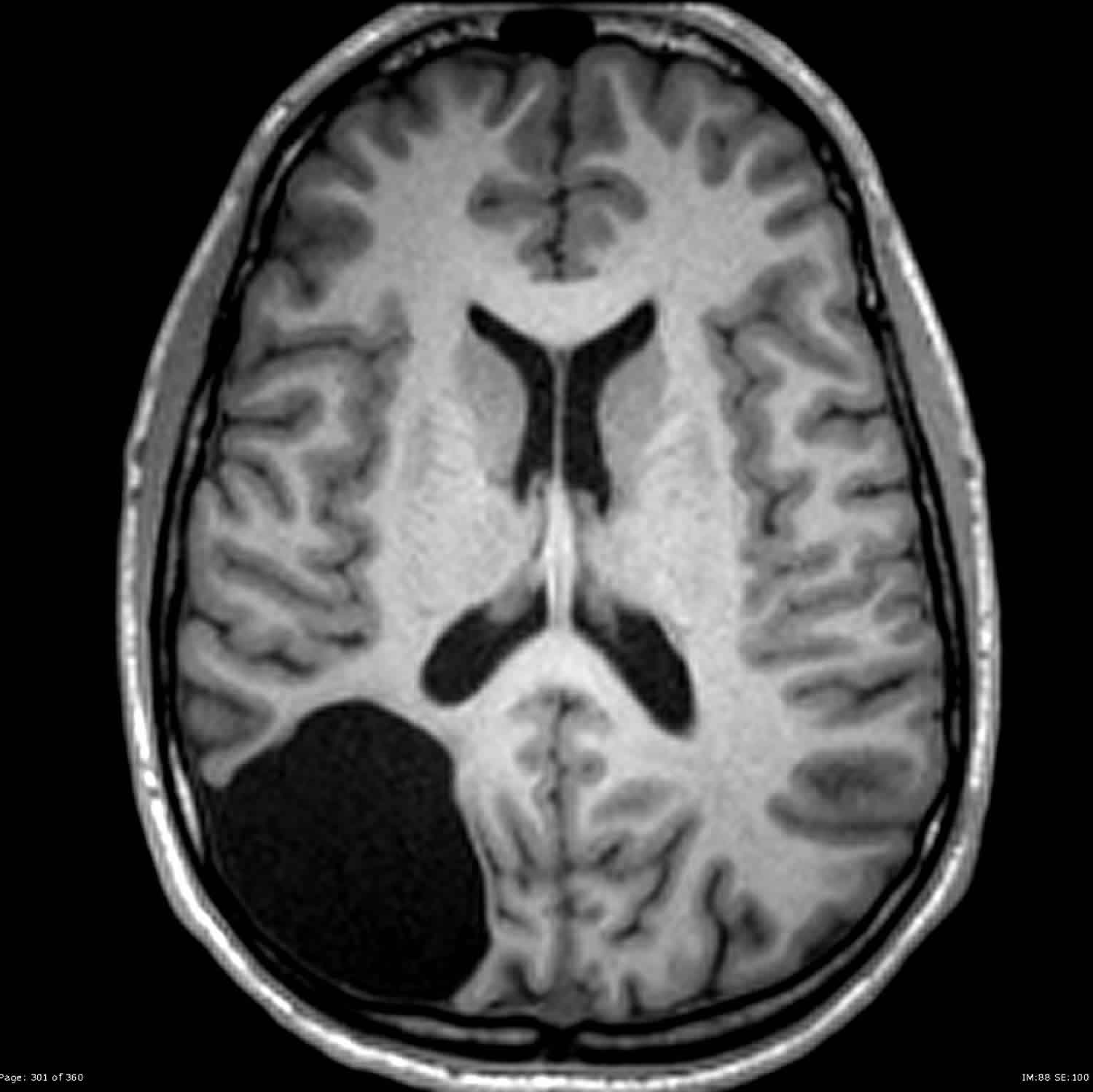
Porencephaly is an extremely rare disorder of the central nervous system in which a cyst or cavity filled with cerebrospinal fluid (CSF) develops in the brain. The terminology regarding porencephaly used in the medical literature has caused confusion. Some researchers break down porencephaly into porencephaly type 1 also known as encephaloclastic porencephaly and porencephaly type 2 also known as schizencephaly 1. The term is used variably among radiologists with its broadest definition being a cleft or cystic cavity within the brain 2 and its more narrow definition being a focal cystic area of encephalomalacia that communicates with the ventricular system and/or the subarachnoid space.
The necessity of a cyst communicating with the ventricular system and/or subarachnoid space to earn the designation porencephaly is a point of contention amongst neuroradiologists. Some authors use the porencephaly term for cysts in the brain whether or not communication exists. Others reserve the term for cysts that communicate with at least one space, in which case they divide porencephalic cysts into internal (communicating with the ventricle) or external (communicating with the subarachnoid space). Still, others require communication with both.
Porencephaly may be classified as sporadic porencephaly or familial porencephaly. Sporadic porencephaly, the more common type, is usually the result of damage from stroke, infection just before or just after birth (perinatal infection), trauma, maternal disease or sickness, maternal diabetes, or maternal use of alcohol or drugs such as cocaine during pregnancy 1. Familial porencephaly (infantile hemiplegia with porencephaly), less common type, which is inherited is caused by abnormal development before birth and occurs due to mutations of the COL4A1 gene 1.
The severity and associated symptoms of porencephaly vary dramatically from one person to another based upon the size and exact locations of the fluid-filled cavities or cysts in the brain. Some infants develop serious complications shortly after birth; others individuals may have mild symptoms that may go undetected. Symptoms of porencephaly include delayed growth and development, spastic hemiplegia (slight or incomplete paralysis), hypotonia (low muscle tone), seizures (often infantile spasms), and macrocephaly (large head) or microcephaly (small head). Children with porencephaly may have poor or absent speech development, epilepsy, hydrocephalus (accumulation of fluid in the brain), spastic contractures (shrinkage or shortening of the muscles), and cognitive impairment.
Porencephaly diagnosis is usually made before an infant reaches his or her first birthday. Neurologic examination is usually abnormal, with manifestations including either low or increased muscle tone, developmental delays, hemiparesis, or impairment of visual attention. However, a few children develop only minor neurologic signs and have normal intelligence. Diagnosis of porencephaly is confirmed by cranial computed tomography (CT), magnetic resonance imaging (MRI), or ultrasonography.
Treatment of porencephaly is supportive which may include physical therapy, medication for seizures, and the placement of a shunt in the brain to remove excess fluid in the brain.
Porencephaly prognosis is variable depending on the location and extent of the cysts or cavities. Some children with porencephaly develop only minor neurological problems and have normal intelligence, while others may be severely disabled and die before their second decade of life 3.
What is hydranencephaly?
Hydranencephaly is an extreme form of porencephaly in which the cerebral hemispheres are almost totally absent. Usually, the cerebellum and brain stem are formed normally, and the basal ganglia are intact. The meninges, bones, and skin over the cranial vault are normal.
Neurologic examination is usually abnormal, and the infant does not develop normally; children often have seizures and intellectual disability. Externally, the head may appear normal, but when transilluminated, light shines completely through.
Often hydranencephaly is diagnosed by prenatal ultrasonography. Computed tomography (CT) or ultrasonography confirms the diagnosis.
Treatment of hydranencephaly is supportive, with shunting if head growth is excessive.
What is schizencephaly?
Schizencephaly, which some experts classify as a form of porencephaly, involves the presence of abnormal slits, or clefts, in the cerebral hemispheres. These clefts extend from the cortical surface to the ventricles and, unlike in other porencephalies, are lined with heterotopic gray matter. This gray matter is usually consistent with polymicrogyria, ie, there are miniature folds and abnormal lamination, resembling abnormally formed gyri. If the walls of the cleft are tightly opposed, so that MRI does not show a clear channel of cerebrospinal fluid (CSF) from the ventricle to the subarachnoid space, the defect is called closed-lip schizencephaly. If a CSF channel is visible, the defect is called open-lip schizencephaly. Open-lip schizencephaly may lead to hydrocephalus.
Unlike other porencephalies, many of which are thought to result from brain injury, schizencephaly represents a defect in neuronal migration and is thus more often a genetically determined malformation. Affected infants often have developmental delay and, depending on the location of the defect, may have focal neurologic findings such as hemiparetic weakness or spasticity. Seizures are common in both types of schizencephaly.
Treatment of schizencephaly is supportive.
Porencephaly causes
Causes of porencephaly include:
- Genetic anomalies (familial porencephaly)
- Inflammatory diseases
- Disorders that interrupt regional cerebral blood flow (eg, intraventricular hemorrhage with parenchymal extension)
Sporadic porencephaly
Sporadic porencephaly is caused by damage to the cerebral hemispheres of the brain, which results in the formation of fluid-filled cavities or cysts on the surface of the brain. Researchers believe that the damage or loss of brain tissue that characterizes porencephaly results from infection, interrupted or obstructed blood flow (ischemia) to the brain, or bleeding (hemorrhaging) in the brain.
A variety of different conditions can potentially cause the localized brain tissue degeneration that ultimately leads to sporadic porencephaly. Such conditions include infection just before or shortly after birth (perinatal infection), too little oxygen in the body just before or shortly after birth (perinatal asphyxia), birth trauma, drug or alcohol use by the mother during pregnancy, maternal sickness or infection, maternal diabetes, or injury or trauma (particularly to the abdominal area) to the mother during pregnancy.
Rarely, porencephaly has associated with performance of diagnostic techniques known as amniocentesis and chorionic villus sampling. Amniocentesis and chorionic villus sampling may be performed during pregnancy to detect certain problems in a fetus such as chromosomal abnormalities or certain genetic disorders. During an amniocentesis procedure, a small amount of amniotic fluid is removed from the sac that surrounds the fetus and studied. During chorionic villus sampling, tissue is removed from the placenta and certain cells called chorionic villi are studied.
Disorders that increase the bleeding tendency in newborns have also been linked to porencephaly. These disorders include neonatal alloimmune thrombocytopenia, von Willebrand’s disease, and maternal use of the drug warfarin (a blood thinner). Neonatal alloimmune thrombocytopenia is a disorder in which antibodies from the mother attack a newborn’s platelets (cells that assist in forming blood clots). Von Willebrand’s disease is an inherited bleeding disorder that results in prolonged bleeding.
Porencephaly is usually sporadic and the risk of recurrence in subsequent pregnancies is unlikely. However, in some patients, genetic factors may play a role in the development of porencephaly. For example, porencephaly is believed to occur with greater frequency than in the general population in individuals with disorders that promote excess blood clotting (thrombophilias). Such disorders include factor V Leiden or protein C deficiency.
Familial porencephaly
Familial porencephaly also called porencephaly type 1 or autosomal dominant porencephaly type 1, is part of a group of conditions called the COL4A1-related disorders. The conditions in this group have a range of signs and symptoms that involve fragile blood vessels. In familial porencephaly, fluid-filled cysts develop in the brain (porencephaly) during fetal development or soon after birth. These cysts typically occur in only one side of the brain and vary in size. The cysts are thought to be the result of bleeding within the brain (hemorrhagic stroke). People with this condition also have leukoencephalopathy, which is a change in a type of brain tissue called white matter that can be seen with magnetic resonance imaging (MRI).
Mutations in the COL4A1 gene cause familial porencephaly. The COL4A1 gene provides instructions for making one component of a protein called type IV collagen. Type IV collagen molecules attach to each other to form complex protein networks. These protein networks are the main components of basement membranes, which are thin sheet-like structures that separate and support cells in many tissues. Type IV collagen networks play an important role in the basement membranes in virtually all tissues throughout the body, particularly the basement membranes surrounding the body’s blood vessels (vasculature).
The COL4A1 gene mutations that cause familial porencephaly result in the production of a protein that disrupts the structure of type IV collagen. As a result, type IV collagen molecules cannot attach to each other to form the protein networks in basement membranes. Basement membranes without normal type IV collagen are unstable, leading to weakening of the tissues that they surround. In people with familial porencephaly, the vasculature in the brain weakens, which can lead to blood vessel breakage and hemorrhagic stroke. Bleeding within the brain is followed by the formation of fluid-filled cysts characteristic of this condition. It is thought that the pressure and stress on the head during birth contributes to vessel breakage in people with this condition; however in some individuals, bleeding in the brain can occur before birth.
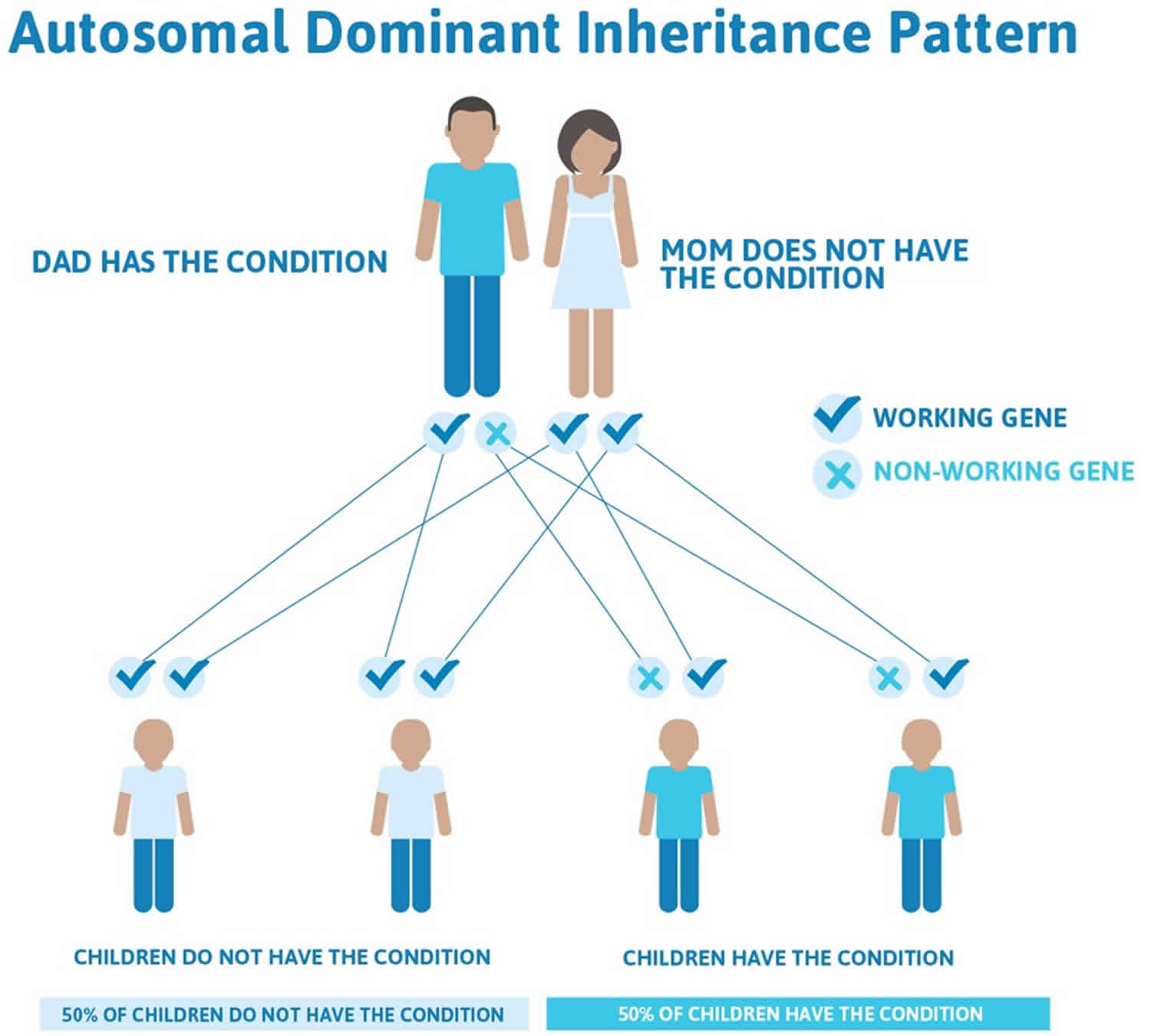
Familial porencephaly is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. In many cases, an affected person has one parent with the condition. The risk of passing the non-working gene from an affected parent to an offspring is 50% for each pregnancy. The risk is the same for males and females.
Figure 1. Familial porencephaly autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Porencephaly symptoms
As can be expected from the knowledge that porencephalic cysts vary widely in size and location, clinical manifestations are also variable. Patients with porencephalic cysts range from asymptomatic, to profoundly impaired.
Often signs and symptoms become evident in the first year of life, with spasticity and seizures being common early manifestations. Language impairment, intellectual disability, diminished muscle tone (hypotonia), delays in growth and development and motor deficits are also frequently encountered 4.
Additional findings that have been reported with porencephaly include poor speech development or absent speech, paralysis of one side of the body (hemiplegia), abnormal tightening or shortening of certain muscles, resulting in restricted or stiff movements (contractures). Some individuals develop hydrocephalus, a condition in which accumulation of excessive cerebrospinal fluid in the skull causes pressure on the tissues of the brain, resulting in a variety of symptoms.
Head circumference is variable with either normal, microcephaly (head circumference is smaller) or macrocephaly (head circumference is larger). Synechiae (term for adhesions, which in radiological contexts usually relates to bands of scar tissue between structures) can create a one-way valve effect with progressive enlargement of the cyst and skull expansion or hydrocephalus, resulting in an enlarged head (macrocephaly).
Familial porencephaly symptoms
Familial porencephaly symptoms are similar to those associated with sporadic porencephaly. During infancy, children with familial porencephaly typically have paralysis affecting one side of the body (infantile hemiplegia). Affected individuals may also have recurrent seizures (epilepsy), migraine headaches, speech problems, intellectual disability, and uncontrolled muscle tensing (dystonia). Some people are severely affected, and others may have no symptoms related to the brain cysts.
Some individuals with familial porencephaly (autosomal dominant porencephaly type 1) have additional symptoms related to two other disorders, brain small vessel disease and hereditary angiopathy with neuropathy, aneurysms, and muscle cramps, which are also caused by mutations of the COL4A1 gene.
Porencephaly diagnosis
A diagnosis of sporadic porencephaly can be made before or after birth through a variety of specialized imaging tests such as an ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI). Ultrasonography may detect porencephaly prenatally after the 30th week of gestation. During an ultrasound, reflected sound waves are used to make an image of the developing fetus. During CT scanning, a computer and x-rays are used to create a film showing cross-sectional images of certain tissue structures. An MRI uses a magnetic field and radio waves to produce cross-sectional images of particular organs and bodily tissues.
Porencephaly treatment
The treatment of sporadic porencephaly is geared toward the specific symptoms that are present in each individual. Treatment may include physical therapy, speech therapy, anti-convulsant medications for seizures, and a shunt to treat hydrocephalus by draining excess fluid from the skull.
Early intervention is important in ensuring that children with sporadic porencephaly reach their highest potential. Services that may be beneficial for some affected individuals include medical, social, and/or vocational services such as special remedial education.
Porencephaly prognosis
The prognosis for children with porencephaly varies according to the location and extent of the cysts or cavities. Some children with porencephaly develop only minor neurological problems and have normal intelligence, while others may be severely disabled and die before their second decade of life 3.
References- Sporadic Porencephaly. https://rarediseases.org/rare-diseases/sporadic-porencephaly
- Bianchi DW, Crombleholme TM, D’Alton ME. Fetology, diagnosis & management of the fetal patient. McGraw-Hill Professional. (2000) ISBN:0838525709
- Porencephaly Information Page. https://www.ninds.nih.gov/disorders/all-disorders/porencephaly-information-page
- Kaufman HH. Cerebrospinal Fluid Collections. Thieme/AANS. (1997) ISBN:1879284480