What are best superfoods for pregnancy
A healthy diet is an important part of a healthy lifestyle at any time, but is especially vital if you’re pregnant or planning a pregnancy. Eating healthily during pregnancy will help your baby to develop and grow. Scientists know that your diet can affect your baby’s health — even before you become pregnant. For example, recent research shows that folic acid helps prevent neural tube defects (including spina bifida) from occurring during the earliest stages of fetal development — so it’s important to consume plenty of it before you become pregnant and during the early weeks of your pregnancy.
Even though many foods, particularly breakfast cereals, are fortified with folic acid, doctors now encourage women to take folic acid supplements before and throughout pregnancy (especially for the first 28 days). Be sure to ask your doctor about folic acid if you’re considering becoming pregnant.
Calcium is another important nutrient. Because your growing baby’s calcium demands are high, you should increase your calcium consumption to prevent a loss of calcium from your own bones. Your doctor will also likely prescribe prenatal vitamins for you, which contain some extra calcium.
Your best food sources of calcium are milk and other dairy products. However, if you have lactose intolerance or dislike milk and milk products, ask your doctor about a calcium supplement. (Signs of lactose intolerance include diarrhea, bloating, or gas after eating milk or milk products. Taking a lactase capsule or pill or using lactose-free milk products may help.) Other calcium-rich foods include sardines or salmon with bones, tofu, broccoli, spinach, and calcium-fortified juices and foods.
Doctors don’t usually recommend starting a strict vegan diet when you become pregnant. However, if you already follow a vegan or vegetarian diet, you can continue to do so during your pregnancy — but do it carefully. Be sure your doctor knows about your diet. It’s challenging to get the nutrition you need if you don’t eat fish and chicken, or milk, cheese, or eggs. You’ll likely need supplemental protein and may also need to take vitamin B12 and D supplements.
To ensure that you and your baby receive adequate nutrition, consult a registered dietitian for help with planning meals.
You’ve heard the statistics: in 2007-2008, about one-third of adults in the United States were obese. We know the consequences: increased risks for coronary heart disease, high blood pressure, diabetes, cancer, and other conditions. Most of us would like to lose a few pounds to improve our health. Now women of childbearing age have another motivation for watching their weight: studies show that prepregnancy weight and pregnancy weight gain can impact not only pregnancy outcomes for mother and baby, but also their long-term health.
- Don’t rely on supplements to make up for an unhealthy diet. Vitamin and mineral supplements cannot replace a healthy diet.
Most doctors recommend that pregnant women take a vitamin and mineral supplement every day, in addition to eating a healthy diet. Doctors often recommend this for those trying to get pregnant as well. Supplements designed for pregnant women are called “prenatal supplements.”
What foods should you avoid ?
There are some foods you should avoid eating during pregnancy because they could cause food poisoning, and the possible presence of bacteria, chemicals or parasites in these foods could harm your unborn baby.
Here is a list of items you should avoid:
- Alcohol. No level of alcohol consumption is considered safe during pregnancy. You should avoid drinking alcohol if you’re pregnant or trying to get pregnant. Do not drink alcohol like wine or beer. Too much exposure to alcohol can seriously affect your baby’s development. Enjoy decaf coffee or tea, non-sugar-sweetened drinks, or water with a dash of juice.
- Caffeine. Avoid diet drinks and drinks with caffeine. You should limit caffeine during pregnancy – avoid having more than 200 milligrams (mg) of caffeine a day. High levels of caffeine can cause babies to have a low birthweight. Too much caffeine can also cause a miscarriage. Caffeine is found naturally in some foods and is added to some soft drinks.
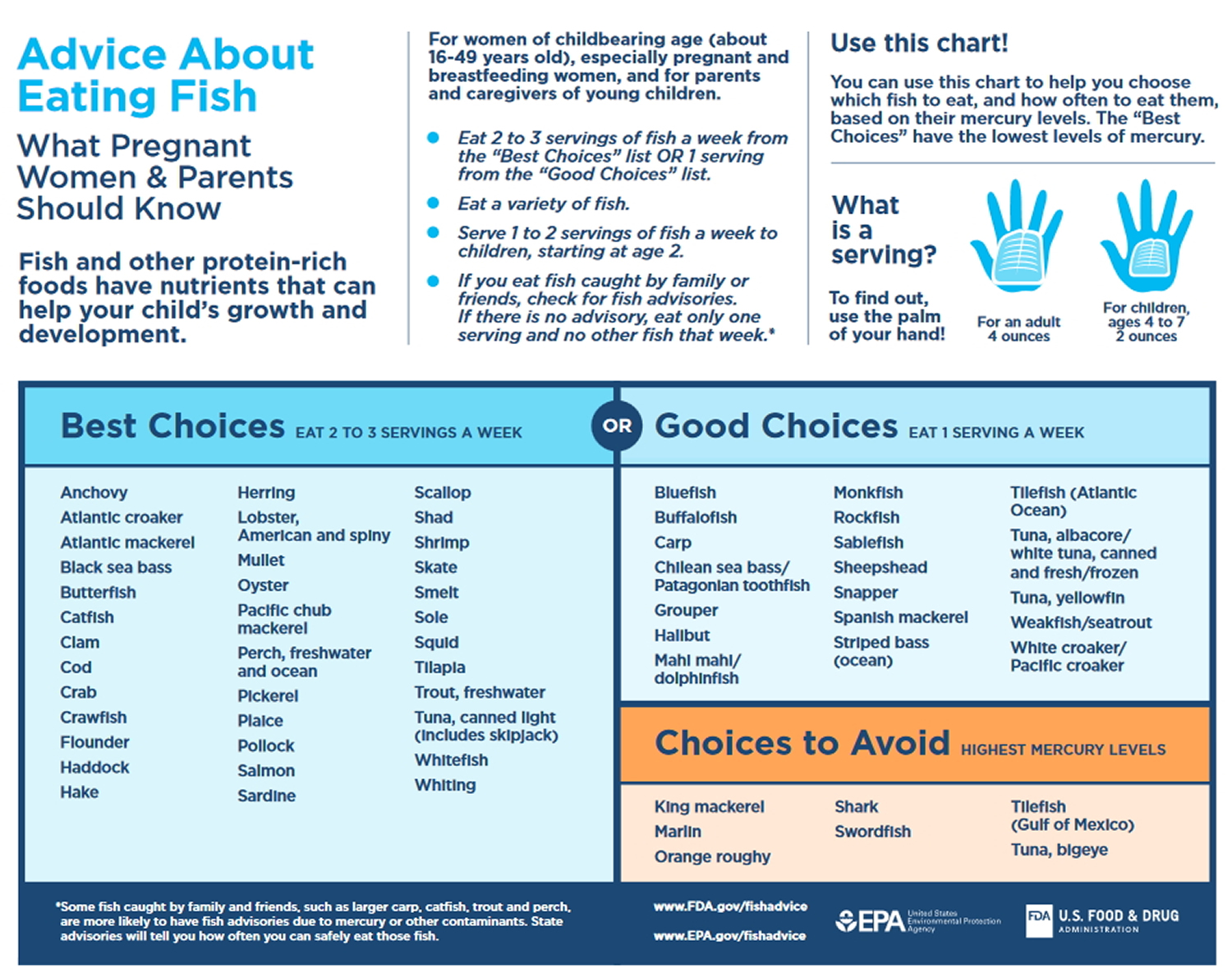
- Fish that may have high levels of mercury (a substance that can build up in fish and harm an unborn baby). You should eat 8 to 12 ounces of seafood per week, but limit white (albacore) tuna to 6 ounces per week. Do not eat tilefish, shark, swordfish, and king mackerel.
- Anything that is not food. Some pregnant women may crave something that is not food, such as laundry starch or clay. This may mean that you are not getting the right amount of a nutrient. Talk to your doctor if you crave something that is not food. He or she can help you get the right amount of nutrients.
Other foods to avoid during pregnancy:
Cheese
Avoid:
- mould-ripened soft cheeses – such as brie, camembert and others with a similar rind, including goats’ cheese
- soft blue-veined cheeses – such as danish blue, gorgonzola and roquefort
Cheeses like this are made with mould and can contain listeria bacteria that cause listeriosis. Although an infection with listeria is rare, even a mild form of this infection in a pregnant woman can lead to miscarriage, stillbirth or severe illness in a newborn baby.
Raw eggs
Eggs produced under the British Lion Code of Practice are safe for pregnant women to eat raw or partially cooked. These eggs have a red lion logo stamped on their shell.
You should avoid any raw or undercooked eggs not produced under the lion code, and any foods that contain them such as homemade mayonnaise.
Make sure eggs without the lion code are thoroughly cooked until the whites and yolks are solid. This prevents the risk of salmonella food poisoning.
Duck eggs, quail eggs and goose eggs should be cooked until the whites and yolks are solid.
Unpasteurised milk
Do not drink raw (unpasteurised) milk, including unpasteurised goats’ or sheep’s milk, or any food that is made of them, such as soft goats’ cheese.
If only raw or green-top milk is available, boil it first.
Pâté
Avoid all types of pâté, including vegetable pâtés, as they can contain listeria.
Raw meat
Do not eat raw or undercooked meat.
Cook all meat and poultry thoroughly so there’s no trace of pink or blood. Be particularly careful with sausages and minced meat.
The latest advice from the Food Standards Agency is that pregnant women should take care when eating cold cured meats such as salami, chorizo, pepperoni and prosciutto, because these meats are not cooked but cured and fermented, so they may contain toxoplasmosis-causing parasites.
It’s best to check the instructions on the pack to see whether the product is ready-to-eat or needs cooking first.
For ready-to-eat meats, you can reduce any risk from parasites by freezing cured/fermented meats for four days at home before you eat them. Freezing kills most parasites, making the meat safer to eat.
Liver
Avoid liver or liver products, such as liver pâté or liver sausage, as they may contain a lot of vitamin A. Too much vitamin A can harm your baby.
Vitamin A
Don’t take:
- high-dose multivitamin supplements
- fish liver oil supplements
- any supplements containing vitamin A
Reducing the risk of toxoplasmosis
Wash fruit, vegetables and salads to remove all traces of soil, which may contain toxoplasma, a parasite that can cause toxoplasmosis.
Pregnancy superfoods list
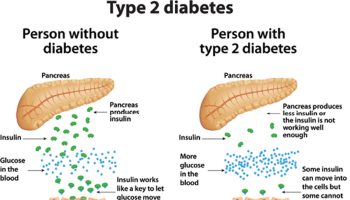
Maternal nutrition prepregnancy and during pregnancy is important for the health, growth, and development of the fetus and the newborn infant. New research shows that maintaining a healthy weight before and during pregnancy can reduce the likelihood of negative effects for mothers and babies. This theory hypothesizes that term infants who are small for gestational age have an increased risk of cardiovascular disease and type II diabetes in adulthood and that this is due to undernutrition of the fetus 1.
A healthy diet includes proteins, carbohydrates, fats, vitamins, minerals, and plenty of water. The U.S. government publishes dietary guidelines that can help you determine how many servings of each kind of food to eat every day. Eating a variety of foods in the proportions indicated is a good step toward staying healthy.
Food labels can tell you what kinds of nutrients are in the foods you eat. The letters RDA, which you find on food labeling, stand for recommended daily allowance, or the amount of a nutrient recommended for your daily diet. When you’re pregnant, the RDAs for most nutrients are higher.
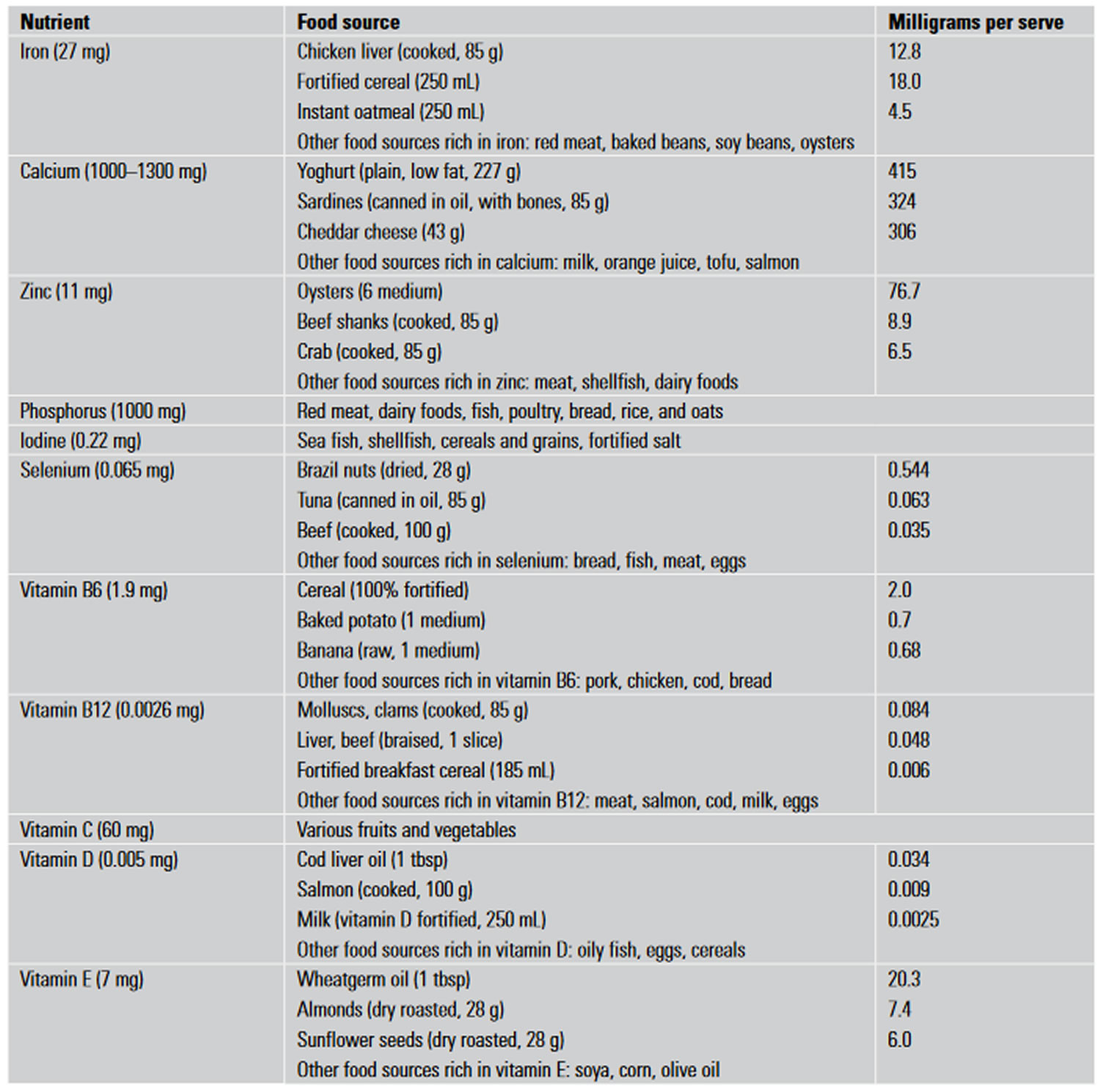
Here are some of the most common nutrients you need and the foods that contain them:
Table 1. Pregnancy superfoods list
| Nutrient | Needed for | Best sources |
|---|---|---|
| Protein | cell growth and blood production | lean meat, fish, poultry, egg whites, beans, peanut butter, tofu |
| Carbohydrates | daily energy production | breads, cereals, rice, potatoes, pasta, fruits, vegetables |
| Calcium | strong bones and teeth, muscle contraction, nerve function | milk, cheese, yogurt, sardines or salmon with bones, spinach |
| Iron | red blood cell production (to prevent anemia) | lean red meat, spinach, iron-fortified whole-grain breads and cereals |
| Vitamin A | healthy skin, good eyesight, growing bones | carrots, dark leafy greens, sweet potatoes |
| Vitamin C | healthy gums, teeth, and bones; assistance with iron absorption | citrus fruit, broccoli, tomatoes, fortified fruit juices |
| Vitamin B6 | red blood cell formation; effective use of protein, fat, and carbohydrates | pork, ham, whole-grain cereals, bananas |
| Vitamin B12 | formation of red blood cells, maintaining nervous system health | meat, fish, poultry, milk (Note: vegetarians who don’t eat dairy products need supplemental B12.) |
| Vitamin D | healthy bones and teeth; aids absorption of calcium | fortified milk, dairy products, cereals, and breads |
| Folic acid | blood and protein production, effective enzyme function | green leafy vegetables, dark yellow fruits and vegetables, beans, peas, nuts |
| Fat | body energy stores | meat, whole-milk dairy products, nuts, peanut butter, margarine, vegetable oils (Note: limit fat intake to 30% or less of your total daily calorie intake.) |
Folic Acid
Folate is also known vitamin B9 (Folacin, Folic Acid, Pteroylglutamic acid) that is naturally present in many foods. Folic Acid is a form of folate that is manufactured and used in dietary supplements and fortified foods. Our bodies need folate to make DNA and other genetic material. Folate is also needed for the body’s cells to divide.
All women need 400 micrograms of folic acid every day. Women who can get pregnant should get 400 to 800 micrograms of folic acid from a vitamin or from food that has added folic acid, such as breakfast cereal 2. This is in addition to the folate you get naturally from food.
If you do not get enough folic acid before and during pregnancy, your baby is at higher risk for neural tube defects.
Neural tube defects are serious birth defects that affect the spine, spinal cord, or brain and may cause death. These include:
- Spina bifida 3. This condition happens when an unborn baby’s spinal column does not fully close during development in the womb, leaving the spinal cord exposed. As a result, the nerves that control the legs and other organs do not work. Children with spina bifida often have lifelong disabilities. They may also need many surgeries.
- Anencephaly 4. This means that most or all of the brain and skull does not develop in the womb. Almost all babies with this condition die before or soon after birth.
Table 2. Selected Food Sources of Folate and Folic Acid
| Food | mcg DFE per serving | Percent DV* |
|---|---|---|
| Beef liver, braised, 3 ounces | 215 | 54 |
| Spinach, boiled, ½ cup | 131 | 33 |
| Black-eyed peas (cowpeas), boiled, ½ cup | 105 | 26 |
| Breakfast cereals, fortified with 25% of the DV† | 100 | 25 |
| Rice, white, medium-grain, cooked, ½ cup† | 90 | 23 |
| Asparagus, boiled, 4 spears | 89 | 22 |
| Spaghetti, cooked, enriched, ½ cup† | 83 | 21 |
| Brussels sprouts, frozen, boiled, ½ cup | 78 | 20 |
| Lettuce, romaine, shredded, 1 cup | 64 | 16 |
| Avocado, raw, sliced, ½ cup | 59 | 15 |
| Spinach, raw, 1 cup | 58 | 15 |
| Broccoli, chopped, frozen, cooked, ½ cup | 52 | 13 |
| Mustard greens, chopped, frozen, boiled, ½ cup | 52 | 13 |
| Green peas, frozen, boiled, ½ cup | 47 | 12 |
| Kidney beans, canned, ½ cup | 46 | 12 |
| Bread, white, 1 slice† | 43 | 11 |
| Peanuts, dry roasted, 1 ounce | 41 | 10 |
| Wheat germ, 2 tablespoons | 40 | 10 |
| Tomato juice, canned, ¾ cup | 36 | 9 |
| Crab, Dungeness, 3 ounces | 36 | 9 |
| Orange juice, ¾ cup | 35 | 9 |
| Turnip greens, frozen, boiled, ½ cup | 32 | 8 |
| Orange, fresh, 1 small | 29 | 7 |
| Papaya, raw, cubed, ½ cup | 27 | 7 |
| Banana, 1 medium | 24 | 6 |
| Yeast, baker’s, ¼ teaspoon | 23 | 6 |
| Egg, whole, hard-boiled, 1 large | 22 | 6 |
| Vegetarian baked beans, canned, ½ cup | 15 | 4 |
| Cantaloupe, raw, 1 wedge | 14 | 4 |
| Fish, halibut, cooked, 3 ounces | 12 | 3 |
| Milk, 1% fat, 1 cup | 12 | 3 |
| Ground beef, 85% lean, cooked, 3 ounces | 7 | 2 |
| Chicken breast, roasted, ½ breast | 3 | 1 |
* DV = Daily Value. The FDA developed DVs to help consumers compare the nutrient contents of products within the context of a total diet. The DV for folate is 400 mcg for adults and children aged 4 and older. However, the FDA does not require food labels to list folate content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient.
† Fortified with folic acid as part of the folate fortification program.
[Source 5]Iron
Iron is one of the major trace elements required during pregnancy 6. It is suggested that a lack of iron in pregnancy can result in preterm delivery and maternal anemia. Adequate iron is required from conception, throughout the pregnancy and during lactation. Iron deficiency during lactation may be associated with mental retardation 7. The recommended daily iron intake for pregnant women is 27 mg/day 8.
Good dietary sources of iron (ie. more than 2 mg/serve) include liver, beef, fortified cereals, cashew nuts and baked beans. Although it is believed that iron excess can hinder the absorption of other vitamins, this hypothesis has yet to be fully substantiated 9.
Calcium
Calcium is required for the maintenance of skeletal, neuromuscular, and cardiac function 10. Studies have shown the maternal skeleton is not the source for fetal calcium needs, thus adequate calcium supplementation during pregnancy and lactation (~1000 mg/day) is essential for fetal bone mineralisation.
In pregnant women who are vegetarians, calcium absorption can be poor from foods rich in oxalic acid (beans and spinach) or phytic acid (nuts and grains). In comparison to dairy milk, calcium absorption from soy milk may be as efficient, while calcium absorption from dried beans is about 50% and from spinach only about 10% 10.
Zinc
Zinc is an important constituent of various enzymes that help maintain structural integrity of proteins and regulate gene expression 11.
It is recommended that pregnant women take 11 mg/day and 12 mg/day during lactation 12. Nevertheless, it is important to be aware that dietary intake of iron at levels found in some supplements may impair zinc absorption.
Vitamin A
Deficiency in vitamin A has been associated with intrauterine growth retardation, preterm birth, low birth weight, placental abruption and increased mortality of the mother 13. Research has also ascertained that vitamin A supplementation can increase haemoglobin concentrations by about 4 g/L in marginally deficient maternal populations 14. Daily intake of 800 μg is recommended in pregnant women 15. Breast milk is a good source of vitamin A 16. However, adequate maternal dietary vitamin A is essential to maintain adequate levels in breast milk
Vitamin B group
The group of B vitamins, which consists of thiamine (B1), riboflavin (B2), niacin or nicotinic acid (B3), B6, folate (B9) and B12, is essential for enhancing the immune system as well as reducing the plasma concentration of homocysteine 17. Elevated maternal plasma homocysteine levels as a result of vitamin B deficiency may lead to pre-eclampsia, premature birth and low birth weight 18. Most cases of B12 deficiency in infants are related to maternal veganism or
malabsorption, such as pernicious anemia 19. Vitamin B12 is found exclusively in animal products including meat, eggs, fish and milk. Excessive vitamin B consumption may result in weight gain, which can potentially complicate labour 20.
Vitamin D
Vitamin D is a group of fat soluble prohormones that help to absorb calcium and phosphorous from dietary intakes, which are required for stimulating skeleton formation of the fetus 16. Deficiency of vitamin D during pregnancy may result in an infant with rickets or type 1 diabetes mellitus 21. The recommended daily intake of vitamin D during pregnancy and lactation is 5 μg/day 22. However, excessive supplementation may be detrimental as it is associated with maternal fatigue and loss of appetite 23.
Vitamin C
Vitamin C stimulates better absorption of iron 21 and therefore helps to reduce the risk of maternal anemia. As an oxidant, it also guards the body against injurious free radicals. Combined with other factors, deficiency of vitamin C is thought to result in difficult labour, but this is yet to be established 21. The recommended daily intake of vitamin C in
pregnancy is 60 mg/day 24.
Vitamin E
Vitamin E acts as an antioxidant in the lipid phase of cell membrane by protecting polyunsaturated fatty acid from free radical damage 25. Higher intake of vitamin E has been found to be associated with a decrease in cardiovascular risk, diabetic complications, and certain cancers and cataracts. Vitamin E deficiency may lead to peripheral neuropathy, spinocerebellar ataxia, skeletal myopathy and pigmented retinopathy; however this has only been reported in association with other genetic or malabsorption syndormes, not simply with a diet low in vitamin E 25. The recommended daily intake for pregnant women is equivalent to the normal requirement in women (7 mg/day), but higher during lactation (11 mg/day) 25.
Iodine
Iodine is essential for fetal and neonatal growth and development. Severe iodine deficiency may result in abortion or stillbirth, congenital anomalies, neurological cretinism, or mental deficiency with deafness, spastic diplegia, squint and myxoedematous cretinism 26. It is recommended that pregnant women consume no less than 220 μg/day.
Selenium
Selenium is thought to have an antioxidant property as well as a role in cellular function, muscle maintenance, fertility and cancer prevention 27. Deficiency in selenium can result in osteoarticular disorder, cardiac enlargement, heart failure, arrhythmia and premature death 27. In conjunction with iodine deficiency, selenium deficiency has also been reported to increase the risk of cretinism 27. It is recommended that pregnant women increase their daily intake of selenium to 65 μg/day and to 70 μg/day during lactation 27.
Phosphorus
Phosphorus, in the form of phosphate, is thought to regulate acid base balance in the bloodstream and activate catalytic proteins 28. Deficiency in this mineral, although rare, may result in symptoms such as anaemia, muscle weakness, bone pain, rickets, parenthesis, anorexia, ataxia, confusion, and possibly death 28. Phosphorus is available in a wide range of foods and the recommended intake in pregnancy is similar to that of nonpregnant women.
Figure 1. Foods (sources of micronutrient) for pregnant women aged 19–50 years
 Food Cravings During Pregnancy
Food Cravings During Pregnancy
You’ve probably known women who craved specific foods during pregnancy, or perhaps you’ve had such cravings yourself. Some old theories held that a hunger for a particular type of food indicated that a woman’s body lacked the nutrients that food contains. Although this turned out not to be so, it’s still unclear why these urges occur.
Some pregnant women crave chocolate, spicy foods, fruits, and comfort foods, such as mashed potatoes, cereals, and toasted white bread. Other women crave non-food items, such as clay and cornstarch. The craving and eating of non-food items is known as pica. Consuming things that aren’t food can be dangerous to both you and your baby. If you have urges to eat non-food items, notify your doctor.
But following your cravings is fine as long as you crave foods that contribute to a healthy diet. Often, these cravings let up about 3 months into the pregnancy.
Prenatal supplements
During pregnancy, your needs increase for several vitamins and minerals, like folate, iron, and calcium. You need enough for your growing baby’s needs as well as your own needs. This makes it difficult to get all that you need from food. This is especially true for folic acid and iron: During pregnancy, mothers need to consume enough nutrients to meet their increased needs as well as those of their growing baby 29.
Most health care providers tell women who are pregnant to take a prenatal vitamin every day and eat a healthy diet. Ask your doctor about what you should take.
Take a prenatal supplement instead of individual vitamins or minerals. This ensures that you and your baby get balanced amounts of the vitamins and minerals you need. A high dose of some nutrients in a supplement, in particular vitamin A, can be harmful to your baby. Too much vitamin A from supplements can cause birth defects.
Don’t take dietary supplements or herbal products on your own. Scientists have not determined the possible risks for your baby of taking most herbal or botanical supplements. For this reason, avoid them when you are pregnant or breastfeeding. Not all “natural” products are safe, and they are not tested or regulated like other drugs and medicines.
Taking too much of a dietary supplement can have harmful effects. Take the supplement your doctor recommends. Follow his or her advice about taking any other supplements or herbal products.
Tell your doctor about any supplements you are already taking, including herbal or botanicals, to protect yourself against taking too much. Also, tell your doctor about any other medicines you are taking, to see if there could be interactions of your supplement with these medicines.
Folic Acid
Folic acid, also called folate, is a B vitamin that helps prevent serious birth defects of a baby’s brain or spine. These are called neural tube defects. Getting enough folic acid can also help prevent birth defects like cleft lip and congenital heart disease. These birth defects often happen before most women know they are pregnant. This is why folic acid is important for any woman who could become pregnant as well as those who are pregnant.
- Most prenatal supplements contain 600 micrograms per day of folic acid. This is the amount recommended for pregnant women from food and supplements combined.
For women who are capable of becoming pregnant, 400 micrograms of folic acid from fortified foods or supplements, in addition to the folate from a healthy diet, is recommended. Foods high in folate include orange juice, strawberries, spinach, broccoli, beans, and fortified breads and breakfast cereals.
Iron
Pregnant women need extra iron for the increasing amount of blood in their bodies. Iron helps keep your blood healthy and able to carry oxygen to your cells. Plus, your baby needs to store iron in his body to last through the first few months of life.
Too little iron can cause a condition called anemia. If you have anemia, you might look pale or notice paleness under your nails, and feel very tired. Your doctor checks for anemia with blood tests during your pregnancy.
Most prenatal supplements contain 27 milligrams of iron. This is the amount recommended for pregnant women per day.
What about fortified foods ?
Some foods are fortified with vitamins and minerals that may help you meet your nutrient needs while you are pregnant or breastfeeding. Examples of vitamins and minerals in fortified foods are:
- Vitamin D – Fluid milk, including fat-free and low-fat milk, is typically fortified with vitamin D. Yogurt may also be fortified with vitamin D. Some calcium-fortified fruit juices and soymilk (soy beverage) also have vitamin D added. Check the label and choose products with vitamin D.
- Iodine – Some salt is fortified with iodine, an essential mineral. Choose salt that is labeled “iodized salt.” But remember to keep the amount of salt and sodium you eat low.
- Folic acid – Enriched bread, flour, pasta, rice, and other grain products are fortified with folic acid. Many ready-to-eat cereals are also fortified with folic acid. Check the label and choose products with folic acid.
- Iron – Some ready-to-eat and cooked cereals are fortified with iron. When you are pregnant, choose these cereals to help meet your increased need for iron. Choose cereals that say “iron fortified.”
Medical conditions and allergies
Some women have specific health needs while they are pregnant or breastfeeding, because of a medical condition. These conditions include diabetes, celiac disease, renal disease, and phenylketonuria (PKU). If you have a medical condition, ask your doctor or health care provider for advice about food choices while you are pregnant or breastfeeding.
Other women may have specific needs because of a food allergy, such as egg, nut, or wheat allergy. If you have a food allergy, ask your doctor for advice about food choices while you are pregnant or breastfeeding.
In addition, if you have any allergies, or your family has a history of allergies, ask your doctor about avoiding common food allergens, such as peanuts, while you are pregnant or breastfeeding.
If you are breastfeeding and your baby has a medical condition or a food allergy, visit your doctor and follow his or her advice about your food choices.
Lactose intolerance
If you avoid milk because you are lactose intolerant, the most reliable way to get the health benefits of milk is to select lactose-free milk and milk products or calcium-fortified soymilk (soy beverage).
You can also take a lactase pill or drops that help you digest lactose before eating or drinking milk products. Also, check with your doctor for his or her advice if you have trouble digesting milk products.
In addition, many people who have a problem digesting lactose can usually eat or drink:
- Smaller portions (up to ½ cup) of milk with a meal
- Yogurt or hard cheeses
- Milk on hot or cold cereal
Remember to choose low-fat or fat-free milk, yogurt, and cheeses.
If you do not drink or eat any foods in the Dairy Group, be sure to get the calcium you need from other foods. These include:
- Calcium-fortified juices and other beverages, cereals, or breads
- Tofu (prepared with calcium sulfate)
- Canned fish with bones you eat (such as sardines or salmon canned with bones)
- Soybeans, black eyed peas (cow peas), and white beans
- Some leafy greens (collard and turnip greens, kale, bok choy)
The amount of calcium that can be absorbed from these foods varies. Check with your doctor to be sure you are getting enough calcium from your foods and beverages.
Pregnancy Healthy Weight
Gaining the right amount of weight during pregnancy helps your baby grow to a healthy size. But gaining too much or too little weight may lead to serious health problems for you and your baby.
Too much weight gain raises your chances for diabetes and high blood pressure during pregnancy and after. If you are overweight when you get pregnant, your chances for health problems may be even higher. It also makes it more likely that you will have a hard delivery and need a cesarean section (C-section).
The new findings suggest that, by losing weight before getting pregnant, obese women can reduce their babies’ risk for congenital heart defects. Previous studies have shown that obese women are also at higher risk for pregnancy-related problems, such as high blood pressure, preeclampsia, and gestational diabetes, for having longer labors, and for giving birth by cesarean section. Babies whose mothers were obese during pregnancy are at higher risk for having large bodies, which can lead to injuries during delivery, and certain birth defects. They are also at higher risk for developing Type 2 diabetes, and for developing it at a younger age than those whose mothers weren’t obese during pregnancy.
Although it is important to get to a healthy weight before pregnancy, losing weight during pregnancy, even for obese women, can be dangerous to the developing fetus. Pregnant women need to get the right nutrition and gain the right amount of weight to promote healthy outcomes. Most women need only around 300 extra calories per day during pregnancy.
Gaining a healthy amount of weight also helps you have an easier pregnancy and delivery. It may also help make it easier for you to get back to your normal weight after delivery. Research shows that a healthy weight gain can also lower the chances that you or your child will have obesity and weight-related problems later in life.
- How much weight you should gain depends on how much you weighed before pregnancy.
- It is important to gain weight very slowly. The old myth that you are “eating for two” is not true.
- Do not try to lose weight if you are pregnant. Healthy food is needed to help your baby grow. Some women may lose a small amount of weight at the start of pregnancy. Speak to your health care provider if this happens to you.
During the first 3 months, your baby is only the size of a walnut and does not need very many extra calories. The following rate of weight gain is advised:
- 1 to 4 pounds total in the first 3 months
- 2 to 4 pounds each month from 4 months until delivery
Talk to your health care provider about how much weight you should gain. Work with him or her to set goals for your weight gain. Take into account your age, weight, and health. The total amount of weight you should gain during your pregnancy depends on your weight when you became pregnant. Women whose weight was in the healthy range before becoming pregnant should gain between 25 and 35 pounds while pregnant. The advice is different for those who were overweight or underweight before becoming pregnant.
- If you are gaining too much weight during pregnancy, cut back on the calories you are currently eating or drinking by limiting the calories from added sugars and saturated fats. They can be found in foods like soft drinks, desserts, fried foods, cheese, whole milk, and fatty meats. Look for choices that are low-fat, fat-free, unsweetened, or with no added-sugars. If you gain too much weight during pregnancy, it can be hard to lose the weight after your baby is born. Most women who gain the suggested amount of weight lose it with the birth of the baby and in the months that follow. Breastfeeding for more than 3 months can also help you lose weight gained during pregnancy.
- If you are not gaining enough weight during pregnancy, you need to eat more calories by eating a little more from each food group. Try adding a healthy snack each day, or increasing portion sizes at meals. If you keep losing weight faster than you want to, check with your doctor. If you gain too little weight during pregnancy, you may have a higher risk for a premature delivery and a low birth weight infant.
Weight Gain during Pregnancy
General weight-gain advice below refers to weight before pregnancy and is for women having only one baby.
Table 3. Recommendations for Total and Rate of Weight Gain During Pregnancy, by Pre-pregnancy BMI (body mass index)
| If you are | You should gain about |
|---|---|
| underweight (BMI* less than 18.5) | 28 to 40 pounds |
| normal weight (BMI of 18.5 to 24.9) | 25 to 35 pounds |
| overweight (BMI of 25 to 29.9) | 15 to 25 pounds |
| obese (BMI of 30+) | 11 to 20 pounds |
*The body mass index (BMI) measures your weight in relation to your height. See the additional links below for a link to an online BMI calculator.
[Source 30]BMI Calculator Adults. http://resources.nationalacademies.org/Pregnancy/WhatToGain.html
Women who are pregnant with twins are given provisional guidelines. Those in the normal BMI category should aim to gain 37-54 pounds; overweight women, 31-50 pounds; and obese women, 25-42 pounds 30.
What kinds of foods should you eat ?
A healthy eating plan for pregnancy includes nutrient-rich foods. Current U.S. dietary guidelines advise eating these foods each day:
- Fruits and veggies (provide vitamins and fiber)
- Whole grains, like oatmeal, whole-wheat bread, and brown rice (provide fiber, B vitamins, and other needed nutrients)
- Fat-free or low-fat milk and milk products or non-dairy soy, almond, rice, or other drinks with added calcium and vitamin D
- Protein from healthy sources, like beans and peas, eggs, lean meats, seafood (8 to 12 ounces per week), and unsalted nuts and seeds
- Fish
- Polyunsaturated and monounsaturated fats.
Recommendations from the Dietary Guidelines for Americans: The 2015–2020 Dietary Guidelines for Americans 31 states that women who are pregnant or breastfeeding should consume 8–12 ounces of seafood per week, choosing from varieties that are higher in polyunsaturated omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) and lower in methyl mercury, such as salmon, herring, sardines, and trout. These women should not consume certain types of fish, such as king mackerel, shark, swordfish, and tilefish that are high in methyl mercury, and they should limit the amount of white (albacore) tuna they consume to 6 ounces a week. The American Academy of Pediatrics has similar advice for breastfeeding women, recommending intakes of 200–300 mg docosahexaenoic acid (DHA) per day by consuming one to two servings of fish per week to guarantee a sufficient amount of docosahexaenoic acid (DHA) in breast milk 32.
Figure 1. Eating Fish: What Pregnant Women and Parents Should Know
 [Source 33]
[Source 33]
You should limit the amount of foods you eat that contain:
- Saturated fat
- Trans fat
- Cholesterol
- Sodium
- Added sugars
A healthy eating plan also limits salt, solid fats (like butter, lard, and shortening), and sugar-sweetened drinks and foods.
A MyPlate Daily Checklist 34 for Moms shows the foods and amounts that are right for you at your stage of pregnancy or when breastfeeding. Your plan will be personalized, based on your age, height, weight, physical activity level, and stage of pregnancy or breastfeeding status (pregnancy and breastfeeding options display upon providing your gender and age).
The MyPlate Daily Checklist 34 shows your food group targets – what and how much to eat within your calorie allowance. Your food plan is personalized, based on your age, sex, height, weight, and physical activity level.
Not sure how much to eat from each food group ?
- Use the MyPlate Checklist Calculator 35
Simply enter your age, sex, height, weight, and physical activity level to get a plan that’s right for you. The MyPlate Daily Checklist 35 shows your food group targets – what and how much to eat within your calorie allowance.
For a more advanced experience, you can create a personal daily food plan using the SuperTracker’s MyPlan 36. You will be asked to create a profile, and you can register to save it if you want. You can then use some or all of the SuperTracker’s other features.
- SuperTracker website: 36
To find out What and How Much To Eat, you can use a FREE, award-winning, state-of-the-art, online diet and activity tracking tool called SuperTracker 37 from the United States Department of Agriculture Center for Nutrition Policy and Promotion 37. This free application empowers you to build a healthier diet, manage weight, and reduce your risk of chronic diet-related diseases. You can use SuperTracker 37 to determine what and how much to eat; track foods, physical activities, and weight; and personalize with goal setting, virtual coaching, and journaling.
Table 4. Pregnancy Daily Food Checklist
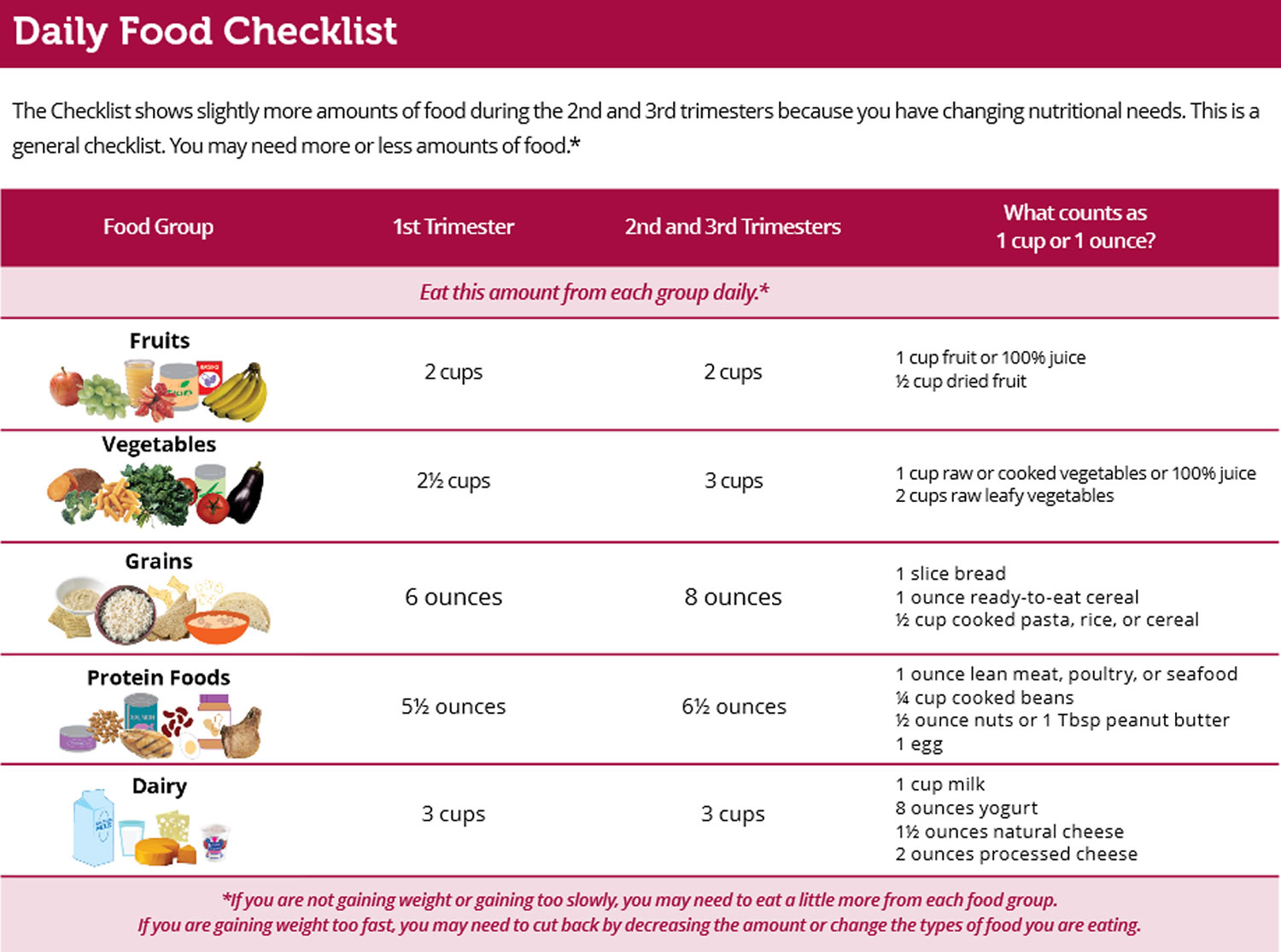 [Source 38]
[Source 38]
Being Physically Active
Unless your doctor advises you not to be physically active, include 2½ hours each week of physical activity such as brisk walking, dancing, gardening, or swimming. The activity can be done for at least 10 minutes at a time, and preferably spread throughout the week. Avoid activities with a high risk of falling or injury.
Almost all women can and should be physically active during pregnancy. Regular physical activity may:
- help you and your baby gain the right amounts of weight
- reduce backaches, leg cramps, and bloating
- reduce your risk for gestational diabetes (diabetes that develops when a woman is pregnant)
If you were physically active before you became pregnant, you may not need to change your exercise habits. Talk with your health care provider about how to change your workouts during pregnancy.
How much physical activity do you need ?
Most women need the same amount of physical activity as before they became pregnant. Aim for at least 30 minutes of aerobic activity per day on most days of the week. Aerobic activities use large muscle groups (back, chest, and legs) to increase heart rate and breathing.
The aerobic activity should last at least 10 minutes at a time and should be of moderate intensity. This means it makes you breathe harder but does not overwork or overheat you.
If you have health issues like obesity, high blood pressure, diabetes, or anemia (too few healthy red blood cells), ask your health care provider about a level of activity that is safe for you.
How can you stay active while pregnant ?
Even if you have not been active before, you can be active during your pregnancy by using the tips below:
- Go for a walk around the block, in a local park, or in a shopping mall with a family member or friend. If you already have children, take them with you and make it a family outing.
- Get up and move around at least once an hour if you sit in a chair most of the day. When watching TV, get up and move around during commercials. Even a simple activity like walking in place can help.
How can you stay safe while being active ?
For your health and safety, and for your baby’s, you should not do some physical activities while pregnant. Some of these are listed below. Talk to your health care provider about other physical activities that you should not do.
Make a plan to be active while pregnant. List the activities you would like to do, such as walking or taking a prenatal yoga class. Think of the days and times you could do each activity on your list, like first thing in the morning, during lunch break from work, after dinner, or on Saturday afternoon. Look at your calendar or planner to find the days and times that work best, and commit to those plans.
Table 5. Safety tips while being active
| Safety Dos and Dont’s | |
|---|---|
| Follow these safety tips while being active. | |
| Do… | Don’t… |
| Choose moderate activities that are not likely to injure you, such as walking or aqua aerobics. | Avoid brisk exercise outside during very hot weather. |
| Drink fluids before, during, and after being physically active. | Don’t use steam rooms, hot tubs, and saunas. |
| Wear comfortable clothing that fits well and supports and protects your breasts. | After the end of week 12 of your pregnancy, avoid exercises that call for you to lie flat on your back. |
| top exercising if you feel dizzy, short of breath, tired, or sick to your stomach. | |
- Emmett PM, Jones LR, Golding J. Pregnancy diet and associated outcomes in the Avon Longitudinal Study of Parents and Children. Nutrition Reviews. 2015;73(Suppl 3):154-174. doi:10.1093/nutrit/nuv053. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4586451/
- U.S. Preventive Services Task Force. (2016). Final Recommendation Statement: Folic Acid for the Prevention of Neural Tube Defects: Preventive Medication
- CDC. (2016). Spina Bifida. – https://www.cdc.gov/ncbddd/spinabifida/facts.html
- CDC. (2015). Facts about Anencephaly. – https://www.cdc.gov/ncbddd/birthdefects/anencephaly.html
- U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 27. Nutrient Data Laboratory home page, 2014. https://ndb.nal.usda.gov/ndb/
- Dawson EB, McGanity WJ. Protection of maternal iron stores in pregnancy. J Reprod Med 1987;32:478–87.
- Casanueva E, Pfeffer F, Drijanski A, et al. Iron and folate status before pregnancy and anemia during pregnancy. Ann Nutr Metab 2003;47:60–3.
- National Health and Medical Research Council. Nutrient reference value for Australia and New Zealand – iron. Available at www.nrv.gov.au/nutrients/iron.htm
- Scholl TO. Iron status during pregnancy: Setting the stage for mother and infant. Am J Clin Nutr 2005;81:1218–22S.
- National Health and Medical Research Council. Nutrient reference values for Australia and New Zealand 2005 – calcium. Available at www.nrv.gov.au/resources/_files/n35–calcium.pdf
- National Health and Medical Research Council. Nutrient reference values for Australia and New Zealand 2005 – zinc. Available at www.nrv.gov.au/resources/_files/n35-zinc.pdf
- National Health and Medical Research Council. Nutrient reference values for Australia and New Zealand 2005 – zinc. Available at www.nrv.gov.au/nutrients/zinc.htm
- Christian P, Khatry SK, Yamini S, et al. Zinc supplementation might potentate the effect of vitamin A in restoring night vision in pregnant Nepalese women. Am J Clin Nutr 2001;73:1045–51.
- Suharno D, West CE, Muhilal, Karyadi D, Hautvast JG. Supplementation with vitamin A and iron for nutritional anaemia in pregnant women in West Java, Indonesia. Lancet 1993;342:1325–8.
- National Health and Medical Research Council. Nutrient reference value for Australia and New Zealand – vitamin A. Available at www.nrv.gov.au/nutrients/vitamin%20a.htm
- Allen LH. Multiple micronutrients in pregnancy and lactation. Am J Clin Nutr 2005;81:1206–16S.
- Herbert B. Vitamin and minerals in pregnancy and lactation. New York: Raven Press, 1988.
- Bondevik GT, Schneede J, Refsum H, Lie RT, Ulstein M, Kvale G. Homocysteine and methylmalonic acid levels in pregnant Nepali women. Should cobalamin supplementation be considered? Eur J Clin Nutr 2001;55:856–64.
- Dror DK, Allen LH. Effect of vitamin B12 deficiency on neurodevelopment in infants: Current knowledge and possible mechanisms. Nutr Rev 2008;66:250–5.
- Lammi-Keefe CJ, Couch SC, Elliot P. Handbook of nutrition and pregnancy. Totowa NJ: Humana Press, 2008.
- Haider BA, Bhutta ZA. Multiple-micronutrient supplementation for women during pregnancy. Chichester, UK: John Wiley & Sons Ltd, 1993.
- National Health and Medical Research Council. Nutrient reference value for Australia and New Zealand – vitamin D. Available at www.nrv.gov.au/nutrients/vitamin%20d.htm
- Nath R. Health and diseases: Role of micronutrients and trace elements. APH 2000;67.
- National Health and Medical Research Council. Nutrient reference value for Australia and New Zealand – vitamin C. Available at www.nrv.gov.au/nutrients/vitamin%20c.htm
- National Health and Medical Research Council. Nutrient reference values for Australia and New Zealand – vitamin E. Available at www.nrv.gov.au/nutrients/vitamin%20e.htm
- National Health and Medical Research Council. Nutrient reference values for Australia and New Zealand 2005 – iodine. Available at www.nrv.gov.au/resources/_files/n35-iodine.pdf
- National Health and Medical Research Council. Nutrient reference values for Australia and New Zealand – selenium. Available at www.nrv.gov.au/nutrients/selenium.htm
- National Health and Medical Research Council. Nutrient reference values for Australia and New Zealand 2005 – phosphorus. Available at www.nrv.gov.au/resources/_files/n35-phosphorus.pdf
- Why take a prenatal supplement ? https://www.choosemyplate.gov/moms-pregnancy-prenatal-supplements
- Weight Gain During Pregnancy: Reexamining the Guidelines. http://nationalacademies.org/hmd/~/media/Files/Report%20Files/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines/Report%20Brief%20-%20Weight%20Gain%20During%20Pregnancy.pdf
- Dietary Guidelines for Americans. https://health.gov/dietaryguidelines/
- Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:2011-3552. https://www.ncbi.nlm.nih.gov/pubmed/22371471?dopt=Abstract
- Eating Fish: What Pregnant Women and Parents Should Know. U.S. Food and Drug Administration. https://www.fda.gov/Food/ResourcesForYou/Consumers/ucm393070.htm
- MyPlate Daily Checklist. https://www.choosemyplate.gov/MyPlate-Daily-Checklist
- MyPlate Checklist Calculator. https://www.choosemyplate.gov/MyPlate-Daily-Checklist-input
- SuperTracker. https://www.supertracker.usda.gov/createprofile.aspx
- https://supertracker.usda.gov/
- Tips for Pregnant Moms. https://wicworks.fns.usda.gov/wicworks//Topics/PregnancyFactSheet.pdf
- Health Tips for Pregnant Women. https://www.niddk.nih.gov/health-information/weight-management/health-tips-pregnant-women