Prostate cancer
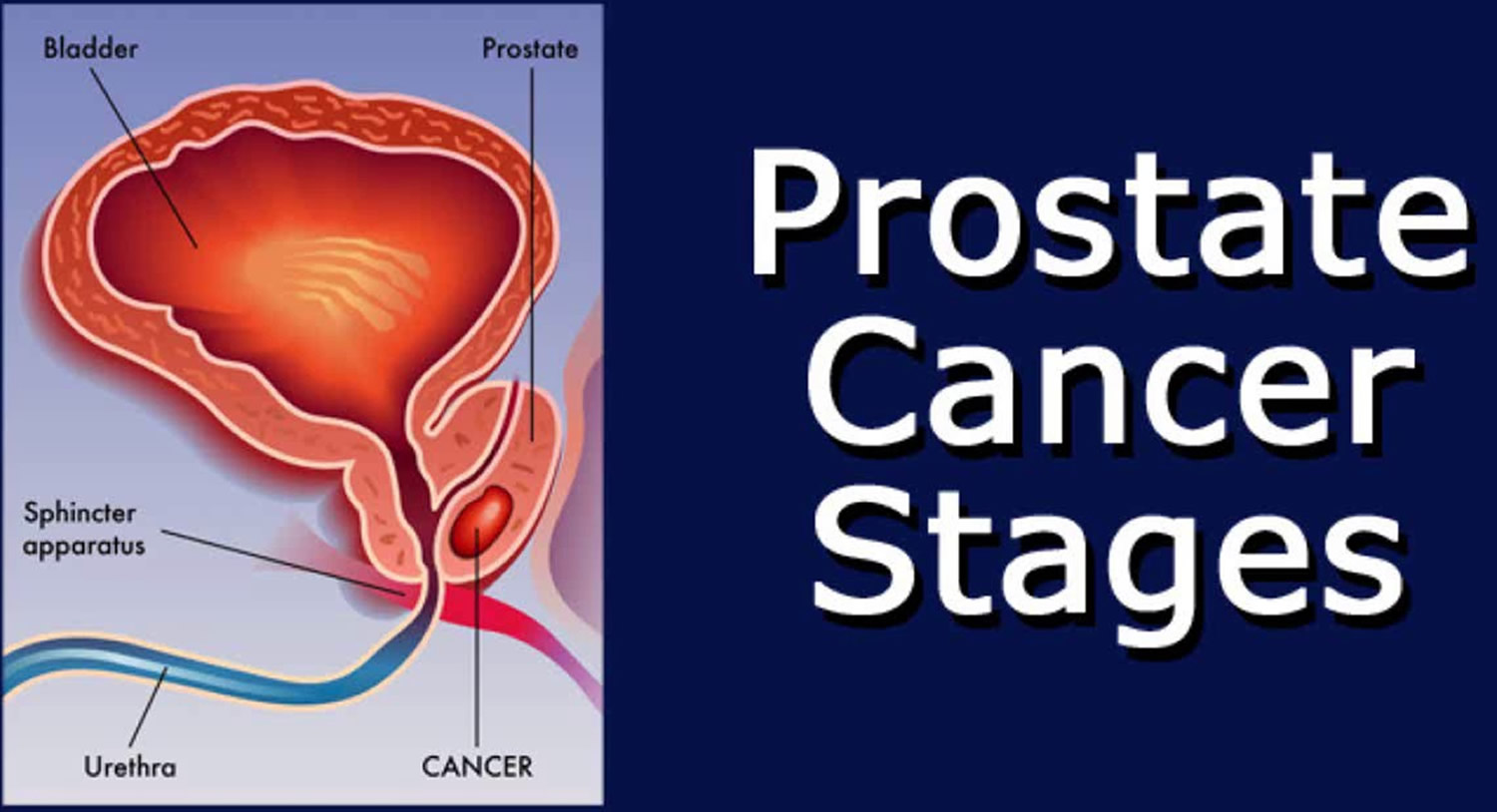
Prostate cancer is cancer of the prostate gland in the male reproductive system. The prostate gland makes seminal fluid that is part of the semen. Just behind the prostate are glands called seminal vesicles that make most of the fluid for semen. The prostate gland lies just below the bladder (the organ that collects and empties urine) and in front of the rectum (the lower part of the intestine), just above the pelvic floor (see Figure 1). The prostate gland is about the size of a walnut and surrounds part of the urethra (the tube that empties urine from the bladder). Prostate cancer is the most common cancer among older men (after skin cancer), but it can often be treated successfully 1. Other than skin cancer, prostate cancer is the most common cancer in American men (more common in older men than younger men) 2. In the U.S., about 1 out of 8 men will be diagnosed with prostate cancer during his lifetime. Prostate cancer is more likely to develop in older men and in non-Hispanic Black men. About 6 cases in 10 are diagnosed in men who are 65 or older, and it is rare in men under 40. The average age of men at diagnosis is about 66.
Many men with prostate cancer never experience symptoms and, without prostate cancer screening, would never know they have the disease 3. In autopsy studies of men who died of other causes, more than 20% of men aged 50 to 59 years and more than 33% of men aged 70 to 79 years were found to have prostate cancer 4. In some men, prostate cancer is more aggressive and leads to death. The median age of death from prostate cancer is 80 years, and more than two-thirds of all men who die of prostate cancer are older than 75 years 5. African American men have an increased lifetime risk of prostate cancer death compared with those of other races/ethnicities (4.2% for African American men, 2.9% for Hispanic men, 2.3% for white men, and 2.1% for Asian and Pacific Islander men) 5.
The American Cancer Society’s estimates for prostate cancer in the United States for 2022 are 5:
- About 268,490 new cases of prostate cancer
- About 34,500 deaths from prostate cancer
- The rate of new cases of prostate cancer was 112.7 per 100,000 men per year based on 2015–2019 cases, age-adjusted.
- In general prostate cancer has excellent survival rates, but death rates are higher in African American men, men who have advanced stage cancer, and men who are between the ages of 75 and 84.
- 5-Year Relative Survival: 96.8%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Percentage of All Cancer Deaths: 5.7%. Prostate cancer is the fifth leading cause of cancer death in the United States. The death rate was 18.9 per 100,000 men per year based on 2015–2019, age-adjusted.
- In 2019, there were an estimated 3,253,416 men living with prostate cancer in the United States.
Prostate cancer is the second leading cause of cancer death in American men, behind only lung cancer 6. About 1 man in 41 will die of prostate cancer.
Prostate cancer can be a serious disease, but most men diagnosed with prostate cancer do not die from it. In fact, more than 3.1 million men in the United States who have been diagnosed with prostate cancer at some point are still alive today 6.
Prostate cancer begins when cells in the prostate gland start to grow uncontrollably. The prostate is a gland found only in males. It makes some of the fluid that is part of semen.
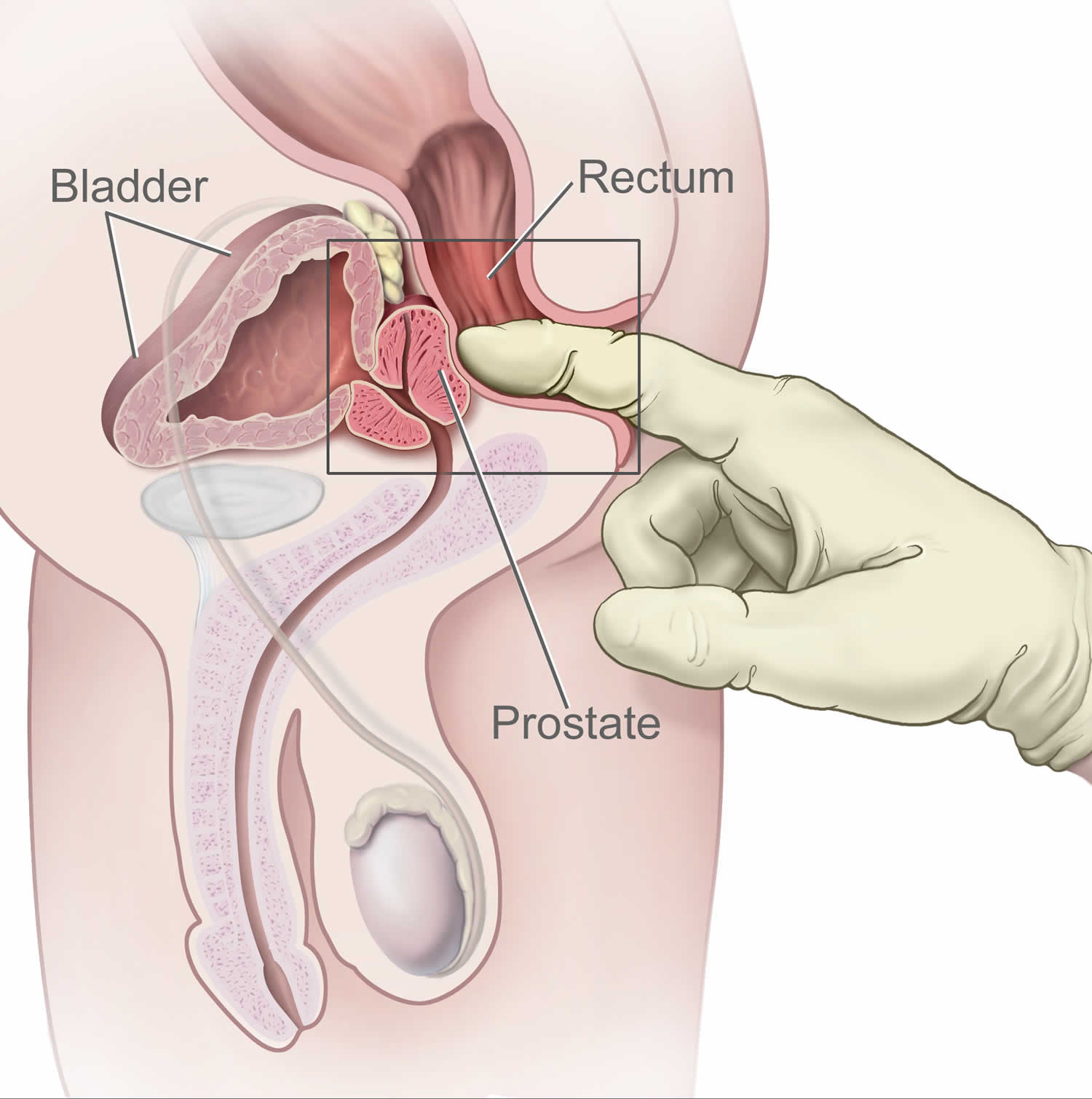
In men, the prostate gland can be felt by digital palpation during a rectal examination.The size of the prostate changes with age. In younger men, it is about the size of a walnut, but it can be much larger in older men.
Just behind the prostate are glands called seminal vesicles that make most of the fluid for semen. The urethra, which is the tube that carries urine and semen out of the body through the penis, goes through the center of the prostate.
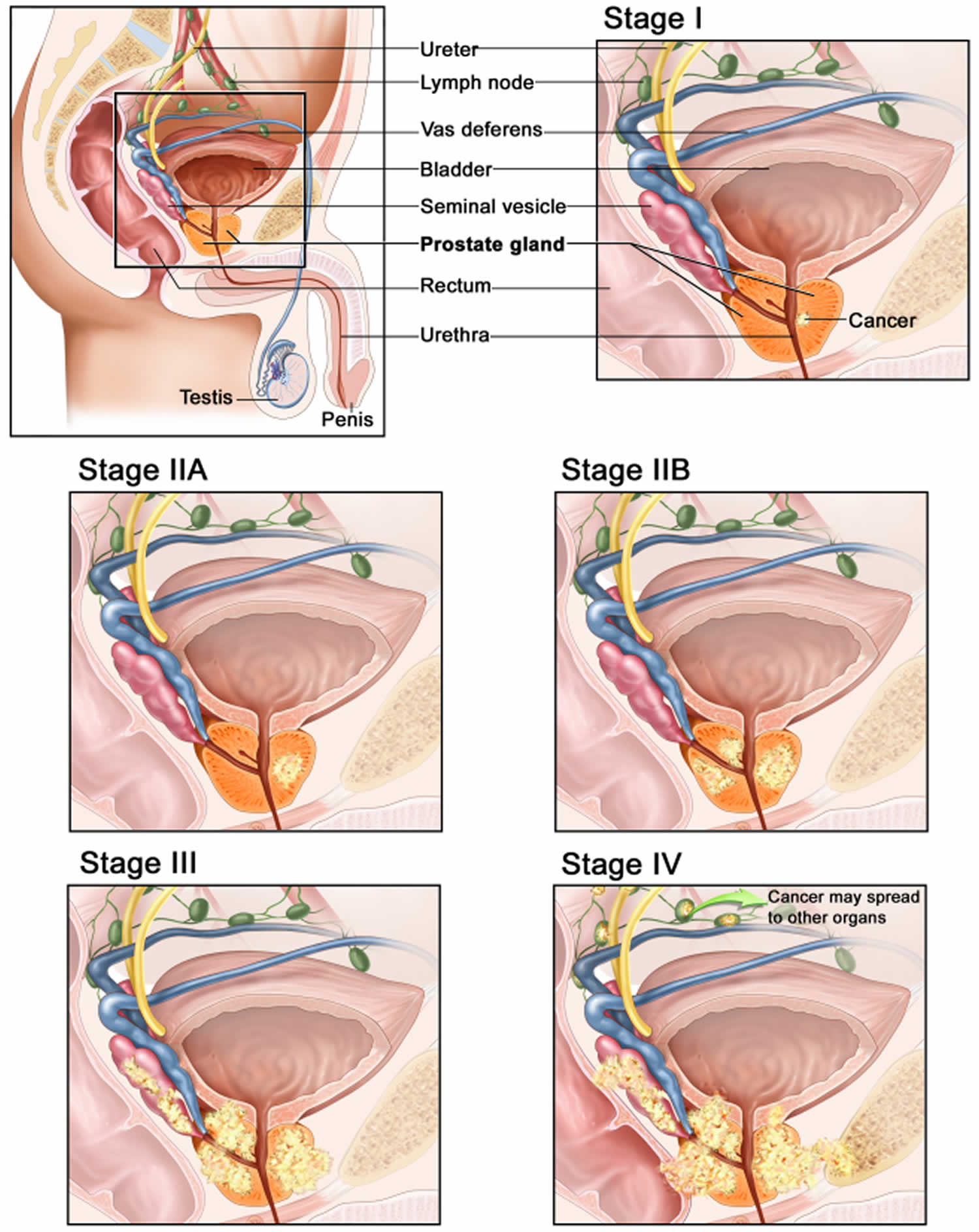
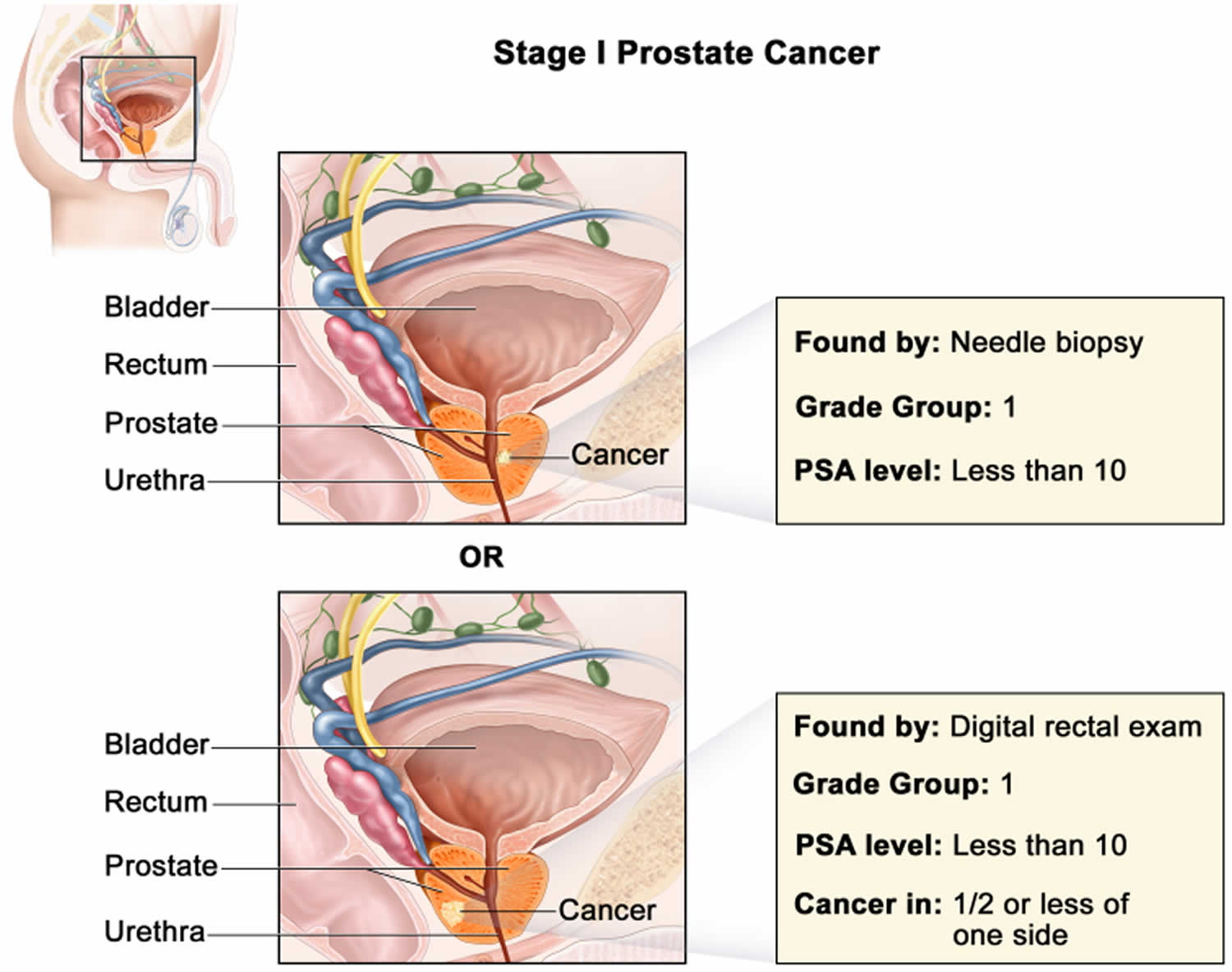
Your prostate cancer treatment options depend on several factors including how big the cancer is, how fast your cancer is growing and whether it has spread anywhere else in your body (also known as the stage), the type of prostate cancer, how abnormal the cells look under a microscope (the grade) and your general health and level of fitness as well as the potential benefits or side effects of the treatment. These are all things to think about when making decisions about treatment. A team of doctors and other professionals will discuss the best treatment and care for you.
The main treatments for prostate cancer are:
- active surveillance or watchful waiting
- surgery
- external radiotherapy
- internal radiotherapy (brachytherapy)
- hormone therapy
- high frequency ultrasound therapy (HIFU) (as part of a clinical trial)
- cryotherapy (as part of a clinical trial)
- chemotherapy in combination with other treatments
- immunotherapy
- targeted therapy
- symptom control treatment
You have one or more of these treatments depending on the stage of your cancer.
Your doctors and nurses will tell you what your options are and help you make the decision about your treatment.
Can I lower the risk of prostate cancer progressing or coming back?
If you have (or have had) prostate cancer, you probably want to know if there are things you can do that might lower your risk of the cancer growing or coming back, such as exercising, eating a certain type of diet, or taking nutritional supplements. While there are some things you can do that might be helpful, more research is needed to know for sure.
- Get regular physical activity. Some research has suggested that men who exercise regularly after treatment might be less likely to die from their prostate cancer than those who don’t. It’s not clear exactly how much activity might be needed, but more seems to be better. More vigorous activity might also be more helpful than less vigorous activity. Further studies are needed to follow up on these findings.
- Quit smoking. Some research has suggested that men who smoke are more likely to have their prostate cancer recur and are more likely to die from it than men who don’t smoke. More research is needed to see if quitting smoking can help lower these risks, although quitting is already known to have a number of other health benefits.
- Nutrition and dietary supplements. Some studies have linked eating a diet that is high in added sugars, meat, and fat to a higher chance of dying from prostate cancer. But eating a “Mediterranean” diet pattern with foods such as fruits, vegetables, and whole grains, has been associated with a lower chance of dying. So eating a diet rich in fruits and vegetables and lower in animal fats might be helpful, but more research is needed to be sure. We do know that a healthy diet can have positive effects on your overall health, with benefits that extend beyond your risk of prostate or other cancers. So far, no dietary supplements have been shown to clearly help lower the risk of prostate cancer progressing or coming back. In fact, some research has suggested that some supplements, such as selenium, might even be harmful. This doesn’t mean that no supplements will help, but it’s important to know that none have been proven to do so. Dietary supplements are not regulated like medicines in the United States – they do not have to be proven effective (or even safe) before being sold, although there are limits on what they’re allowed to claim they can do. If you are thinking about taking any type of nutritional supplement, talk to your health care team. They can help you decide which ones you can use safely while avoiding those that could be harmful.
Can I lower my risk of getting a second cancer?
Prostate cancer survivors can be affected by a number of health problems, but often a major concern is facing cancer again. Cancer that comes back after treatment is called a recurrence. But some cancer survivors may develop a new, unrelated cancer later. This is called a second cancer.
Unfortunately, being treated for prostate cancer doesn’t mean you can’t get another cancer. Men who have had prostate cancer can still get the same types of cancers that other men get. In fact, they might be at higher risk for certain types of cancer.
Men who have had prostate cancer can get any type of second cancer, but they have an increased risk of certain cancers, including:
- Small intestine cancer
- Soft tissue cancer
- Bladder cancer
- Thyroid cancer
- Thymus cancer
- Melanoma of the skin
Men who are treated with radiation therapy also have a higher risk of:
- Rectal cancer
- Acute myeloid leukemia (AML)
This risk is probably related to the dose of radiation. Newer methods of giving radiation therapy may have different effects on the risks of a second cancer. Because these methods are newer, the long-term effects have not been studied as well.
There are steps you can take to lower your risk and stay as healthy as possible. For example, prostate cancer survivors should do their best to stay away from all tobacco products and tobacco smoke. Smoking can increase the risk of bladder cancer, as well as increase the risk of many other cancers.
To help maintain good health, prostate cancer survivors should also:
- Get to and stay at a healthy weight
- Keep physically active and limit the time you spend sitting or lying down
- Follow a healthy eating pattern that includes plenty of fruits, vegetables, and whole grains, and limits or avoids red and processed meats, sugary drinks, and highly processed foods
- Not drink alcohol. If you do drink, have no more than 1 drink per day for women or 2 per day for men
These steps may also lower the risk of some other health problems.
Prostate gland
The prostate is a gland found only in men, which forms an important part of the male reproductive system. The prostate gland secretes a fluid that keeps sperm alive and healthy and that forms part of semen.
The prostate gland is located at the base of the bladder. It is about the size of a walnut but gets bigger as men get older. The prostate gland measures about 2 × 4 × 3 cm and is an aggregate of 30 to 50 compound tubuloacinar glands enclosed in a single fibrous capsule. These glands empty through about 20 pores in the urethral wall. The stroma of the prostate consists of connective tissue and smooth muscle, like that of the seminal vesicles. The thin, milky secretion of the prostate constitutes about 30% of the semen.
The prostate is a chestnut-shaped structure that surrounds the urethra (first part of the tube that carries urine from the bladder to the penis) and ejaculatory ducts. The urethra also carries semen, which is the fluid containing sperm. The prostate is found behind the base of the penis and immediately underneath the urinary bladder.
The prostate gland produces a protein called prostate specific antigen (PSA). A blood test can measure the level of PSA.
The prostate slowly increases in size from birth to puberty. It then expands rapidly until about age 30, after which time its size typically remains stable until about age 40-45, when further enlargement may occur, constricting the urethra and interfering with urine flow.
In addition to its susceptibility to prostate cancer and tumors, the prostate is also subject to infection in sexually transmitted diseases (STDs). Prostatitis, inflammation of the prostate, is the single most common reason that men consult a urologist.
Figure 1. Normal prostate gland
Normal PSA levels
PSA also callled Prostate-Specific Antigen, is a type of protein produced by cells in the prostate gland and found in the blood. Results are usually expressed as nanograms of PSA per milliliter (ng/mL) of blood. Normally, PSA is produced and released within the prostate gland, where it participates in the dissolution of the seminal fluid coagulum and plays an important role in fertility. Healthy prostates create low levels of PSA and only small amounts of PSA move out of the prostate and into the blood. PSA blood levels may be higher than normal in men who have prostate cancer, benign prostatic hyperplasia (BPH), or infection or inflammation of the prostate gland (prostatitis).
The PSA test uses a blood sample to measure a person’s PSA level. In some patients, the PSA test may be used for prostate cancer screening. The PSA test is also used to help with the diagnostic process for prostate cancer and noncancerous prostate conditions, as well as to monitor people who have been diagnosed with these conditions.
The PSA test result cannot diagnose prostate cancer. Only a prostate biopsy can diagnose prostate cancer.
There is no specific normal or abnormal level of PSA in the blood. In the past, PSA levels of 4.0 nanograms per milliliter (ng/mL) and lower were considered normal, but this varies by age. However, some individuals with PSA levels below 4.0 ng/mL have prostate cancer and many with higher PSA levels between 4 and 10 ng/mL do not have prostate cancer 7.
In addition, various factors can cause someone’s PSA level to fluctuate. For example, the PSA level tends to increase with age, prostate gland size, and inflammation or infection. A recent prostate biopsy will also increase the PSA level, as can ejaculation or vigorous exercise (such as cycling) in the 2 days before testing. Conversely, some drugs—including finasteride and dutasteride, which are used to treat BPH—lower the PSA level.
In general, however, the higher a man’s PSA level, the more likely it is that he has prostate cancer.
PSA test result meaning:
- For men in their 50s or younger, a PSA level should be below 2.5 ng/mL in most cases.
- Older men often have slightly higher PSA levels than younger men.
- When total prostate-specific antigen (PSA) concentration is below 2.0 ng/mL, the probability of prostate cancer in asymptomatic men is low. When total PSA concentration is above 10.0 ng/mL, the probability of cancer is high and prostate biopsy is generally recommended.
- The total PSA range of 4.0 to 10.0 ng/mL has been described as a diagnostic “gray zone,” in which the free PSA/total PSA ratio helps to determine the relative risk of prostate cancer (see Table 2 below). Therefore, some urologists recommend using the free PSA/total ratio to help select which men should undergo biopsy. However, even a negative result of prostate biopsy does not rule-out prostate cancer (see Table 3). Up to 20% of men with negative biopsy results have subsequently been found to have prostate cancer.
Table 1. Total PSA reference values
| Age (years) | PSA upper limit (ng/mL) |
|---|---|
| <40 | < or =2.0 |
| 40-49 | < or =2.5 |
| 50-59 | < or =3.5 |
| 60-69 | < or =4.5 |
| 70-79 | < or =6.5 |
| 80+ | < or =7.2 |
Table 2. When total PSA concentration is in the range of 4.0-10.0 ng/mL
| Probability of cancer | |||
|---|---|---|---|
| Free PSA/total PSA ratio | 50-59 years | 60-69 years | > or =70 years |
| < or =0.10 | 49% | 58% | 65% |
| 0.11-0.18 | 27% | 34% | 41% |
| 0.19-0.25 | 18% | 24% | 30% |
| >0.25 | 9% | 12% | 16% |
Table 3. Based on free PSA/total PSA ratio, the percent probability of finding prostate cancer on a needle biopsy by age in years
| Free PSA/total PSA ratio | 50-59 years | 60-69 years | 70 years and older |
|---|---|---|---|
| < or =0.10 | 49.00% | 58.00% | 65.00% |
| 0.11-0.18 | 27.00% | 34.00% | 41.00% |
| 0.19-0.25 | 18.00% | 24.00% | 30.00% |
| >0.25 | 9.00% | 12.00% | 16.00% |
PSA testing
Since PSA levels in the blood have been linked with prostate cancer, many doctors have used repeated PSA tests in the hope of finding “early” prostate cancer in men with no symptoms of the disease. Unfortunately, PSA is not as useful for screening as many have hoped because many men with prostate cancer do not have high PSA levels, and other conditions that are not cancer (such as benign prostate hyperplasia) can also increase PSA levels 9. Research has shown that men who receive PSA testing are less likely to die specifically from prostate cancer. However when accounting for deaths from all causes, no lives are saved, meaning that men who receive PSA screening have not been shown to live longer than men who do not have PSA screening. Men with medical conditions that limit their life expectancy to less than 10 years are unlikely to benefit from PSA screening as their probability of dying from the underlying medical problem is greater than the chance of dying from asymptomatic prostate cancer.
A doctor may order a PSA test for several reasons:
- Prostate cancer screening: Cancer screening checks for cancer in people who don’t have symptoms. People with prostate cancer often have elevated levels of PSA in their blood, but elevated levels are also found in people without prostate cancer. The decision about whether or not to use a PSA test to screen for prostate cancer is highly individualized based on a patient’s risk factors and health history. Patients should work with their doctor to understand the risks and benefits of PSA screening for their specific situation.
- Prostate disease diagnosis: If you have symptoms of a prostate condition, or if your prostate gland is not normal during a physical exam, your doctor may recommend a PSA test. An elevated level of PSA may indicate an issue in the prostate such as prostate cancer, benign prostatic hyperplasia (BPH), or inflammation of the prostate. This then may lead to more follow-up testing to determine the diagnosis.
- Prostate cancer or disease monitoring and follow-up: If you’ve been diagnosed with prostate cancer or BPH, your doctor may order PSA tests to monitor the effects of treatment. For those who have completed treatment for prostate cancer, the PSA test can be used to check for signs that the cancer has come back.
Your doctor might use other ways of interpreting PSA results before deciding whether to order a biopsy to test for cancerous tissue. These other methods are intended to improve the accuracy of the PSA test as a screening tool. Researchers continue to investigate variations of the PSA test to determine whether they provide a measurable benefit.
Variations of the PSA test include:
- PSA velocity. PSA velocity is the change in PSA levels over time. A rapid rise in PSA may indicate the presence of cancer or an aggressive form of cancer. However, recent studies have cast doubt on the value of PSA velocity in predicting a finding of prostate cancer from biopsy.
- Percentage of free PSA. PSA circulates in the blood in two forms — either attached to certain blood proteins or unattached (free). If you have a high PSA level but a low percentage of free PSA, it may be more likely that you have prostate cancer.
- PSA density. Prostate cancers can produce more PSA per volume of tissue than benign prostate conditions can. PSA density measurements adjust PSA values for prostate volume. Measuring PSA density generally requires an MRI or transrectal ultrasound.
What do experts recommend?
Most medical organizations encourage men aged 55 to 69 years to discuss the pros and cons of prostate cancer screening with their doctors 10. The discussion should include a review of your risk factors and your preferences about screening. You might consider starting the discussions sooner if you’re black, have a family history of prostate cancer or have other risk factors.
If you choose to have prostate cancer screening, most organizations recommend stopping around age 70 or if you develop other serious medical conditions that limit your life expectancy 10. The US Preventive Services Task Force (USPSTF) recommends against screening for prostate cancer in men aged 70 years or older 10. The USPSTF also concludes that at present, the balance between the benefits and the drawbacks of prostate cancer screening in men younger than age 70 years cannot be assessed, because the available evidence is insufficient 11.
If someone who has no symptoms of prostate cancer chooses to undergo prostate cancer screening and is found to have an elevated PSA level, the doctor may recommend another PSA test to confirm the original finding. If the PSA level is still high, the doctor may recommend that the person continue with PSA tests and digital rectal exams (DREs) at regular intervals to watch for any changes over time also called observation or watchful waiting.
If the PSA level continues to rise or a suspicious lump is detected during a digital rectal exam, the doctor may recommend additional tests to determine the nature of the problem. These may include imaging tests, such as magnetic resonance imaging (MRI) or high-resolution micro-ultrasound.
Alternatively, the doctor may recommend a prostate biopsy. During this procedure, multiple samples of prostate tissue are collected by inserting hollow needles into the prostate and then withdrawing them. The biopsy needle may be inserted through the wall of the rectum (transrectal biopsy) or through the perineum (transperineal biopsy). A pathologist then examines the collected tissue under a microscope. Although both biopsy techniques are guided by ultrasound imaging so the doctor can view the prostate during the biopsy procedure, ultrasound cannot be used alone to diagnose prostate cancer. An MRI-guided biopsy may be performed for patients with suspicious areas seen on MRI.
In the past, men with elevated PSA levels and no other symptoms were sometimes prescribed antibiotics to see if an infection might be causing the PSA increase. However, according to the American Urological Association, there is no evidence to support the use of antibiotics to reduce PSA levels in men who are not experiencing other symptoms.
Table 4. Benefits and Harms of PSA Screening in Men 55 to 69 Years of Age
| Outcome | Incidence per 1,000 men who undergo PSA screening every 1 to 4 years for 10 years | Incidence per 1,000 men who do not undergo PSA screening | Benefit or harm of PSA screening |
|---|---|---|---|
| Die of prostate cancer | 4 or 5 | 5 | 0 or 1 fewer prostate cancer death |
| Die of any cause | 200 | 200 | No difference |
| Still alive after 10 years | 800 | 800 | No difference |
| False-positive results | 100 to 120 | 0 | 100 to 120 more false-positive results (may cause anxiety; most lead to biopsy) |
| Additional prostate cancer diagnoses | 110 | 0 | 110 additional prostate cancer diagnoses (about 90% receive treatment) |
| Erectile dysfunction due to treatment | 29 | 0 | 29 more men with erectile dysfunction |
| Urinary incontinence due to treatment | 18 | 0 | 18 more men with urinary incontinence |
| Cardiovascular events due to treatment | 2 | 0 | 2 additional cardiovascular events |
| Deep venous thrombosis or pulmonary embolus due to treatment | 1 | 0 | 1 additional deep venous thrombosis or pulmonary embolus |
Abbreviations: DVT = deep venous thrombosis; PE = pulmonary embolus; PSA = prostate-specific antigen.
[Source 12 ]PSA testing disadvantages
You may wonder how getting a test for prostate cancer could have a downside. After all, there’s little risk involved in the test itself — it requires simply drawing blood for evaluation in a lab.
However, there are some potential downsides once the PSA results are in. These include:
- Elevated PSA levels can have other causes, such as benign prostate enlargement (benign prostatic hyperplasia) or prostate infection (prostatitis). Also, PSA levels normally increase with age. These false-positives are common.
- Some prostate cancers may not produce much PSA. And it’s possible to have prostate cancer and also have a normal PSA level. It’s possible to have what’s known as a “false-negative” — a test result that incorrectly indicates you don’t have prostate cancer when you do.
- Certain drugs used to treat benign prostatic hyperplasia (BPH) or urinary conditions, and large doses of certain chemotherapy medications, may lower PSA levels. Obesity also can lower PSA levels.
- Overdiagnosis. Some prostate cancers detected by PSA tests will never cause symptoms or lead to death. These symptom-free cancers are considered overdiagnoses — identification of cancer not likely to cause poor health or to present a risk of death.
- Follow-up tests to check out the cause of an elevated PSA test can be invasive, stressful, expensive or time-consuming.
- Living with a slow-growing prostate cancer that doesn’t need treatment might cause stress and anxiety.
PSA screening for prostate cancer may reduce risk of prostate cancer mortality but is associated with harms including false-positive results, biopsy complications, and overdiagnosis in 20 percent to 50 percent of screen-detected prostate cancers 13. Early, active treatment for screen-detected prostate cancer may reduce the risk of metastatic disease, although the long-term impact of early, active treatment on prostate cancer mortality remains unclear. Active treatments for prostate cancer are frequently associated with sexual and urinary difficulties.
What have randomized trials of prostate cancer screening found?
Several large, randomized trials of prostate cancer screening have been carried out. One of the largest is the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, to determine whether certain screening tests can help reduce the numbers of deaths from several common cancers 14. In the prostate portion of the trial, the PSA test and digital rectal exam were evaluated for their ability to decrease a man’s chances of dying from prostate cancer.
The Prostate, Lung, Colorectal, and Ovarian (PLCO) investigators found that men who underwent annual prostate cancer screening had a higher incidence of prostate cancer than men in the control group but had about the same rate of deaths from the disease 14. Overall, the results suggest that many men were treated for prostate cancers that would not have been detected in their lifetime without screening. Consequently, these men were exposed unnecessarily to the potential harms of treatment.
A second large trial, the European Randomized Study of Screening for Prostate Cancer (ERSPC), compared prostate cancer deaths in men randomly assigned to PSA-based screening or no screening 15, 16. As in the PLCO, men in European Randomized Study of Screening for Prostate Cancer (ERSPC) who were screened for prostate cancer had a higher incidence of the disease than control men. In contrast to the PLCO, however, men who were screened had a lower rate of death from prostate cancer 15, 16.
A subsequent analysis of data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial used a statistical model to account for the fact that some men in the PLCO trial who were assigned to the control group had nevertheless undergone PSA screening. This analysis suggested that the level of benefit in the PLCO and ERSPC trials was similar and that both trials showed some reduction in prostate cancer death in association with prostate cancer screening 17. Such statistical modeling studies have important limitations and rely on unverified assumptions that can render their findings questionable (or more suitable for further study than to serve as a basis for screening guidelines). More important, the model could not provide an assessment of the balance of benefits versus harms from screening.
The third and largest trial, the Cluster Randomized Trial of PSA Testing for Prostate Cancer (CAP), conducted in the United Kingdom, compared prostate cancer mortality among men whose primary care practices were randomly assigned to offer their patients a single PSA screening test or to provide usual care in which screening was not offered 18. After a median follow-up of 10 years, more low-risk prostate cancers were detected in the single PSA test group than in the usual (unscreened) care group (even though only about a third of men in the screening group actually had the PSA test), but there was no difference in prostate cancer mortality 18.
A systematic review and meta-analysis of all randomized controlled trials comparing PSA screening with usual care in men without a diagnosis of prostate cancer concluded that PSA screening for prostate cancer leads to a small reduction in prostate cancer mortality over 10 years but does not affect overall mortality 19.
The United States Preventive Services Task Force has estimated that, for every 1,000 men ages 55 to 69 years who are screened for 13 years 11:
- About 1.3 deaths from prostate cancer would be avoided (or 1 death avoided per 769 men screened). However, based on 3 additional years of follow-up in the ERSPC trial, about 1.8 deaths from prostate cancer would be avoided per every 1,000 men screened, or 1 death in 570 men screened 20.
- 3 men would avoid developing metastatic cancer
- 5 men would die from prostate cancer despite screening, diagnosis, and treatment
- 240 men would have a positive PSA test result, many of whom would have a biopsy that shows that the result was a false-positive; some men who had a biopsy would experience at least moderately bothersome symptoms (pain, bleeding, or infection) from the procedure (and 2 would be hospitalized).
- 100 men would be diagnosed with prostate cancer. Of those, 80 would be treated (either immediately or after a period of active surveillance) with surgery or radiation. Many of these men would have a serious complication from treatment, with 50 experiencing sexual dysfunction and 15 experiencing urinary incontinence.
- 200 men would die of causes other than prostate cancer
Benign prostatic hyperplasia
An enlarged prostate is also called benign prostatic hyperplasia (BPH) 21. Most men will have enlarged prostate (benign prostatic hyperplasia) as they get older. Symptoms often start after age 50.
In 2010, as many as 14 million men in the United States had lower urinary tract symptoms suggestive of benign prostatic hyperplasia 22. Although benign prostatic hyperplasia rarely causes symptoms before age 40, the occurrence and symptoms increase with age. Benign prostatic hyperplasia affects about 50 percent of men between the ages of 51 and 60 and up to 90 percent of men older than 80 23.
Benign prostatic hyperplasia (BPH) is not cancer, and it does not seem to increase your chance of getting prostate cancer 21. But the early symptoms are the same. Check with your doctor if you have:
- A frequent and urgent need to urinate, especially at night
- Trouble starting a urine stream or making more than a dribble
- A urine stream that is weak, slow, or stops and starts several times
- The feeling that you still have to go, even just after urinating
- Small amounts of blood in your urine
Severe benign prostatic hyperplasia (BPH) can cause serious problems over time. Untreated, prostate gland enlargement can block the flow of urine out of the bladder and cause bladder, urinary tract or kidney problems. If it is found early, you are less likely to develop these problems.
Tests for benign prostatic hyperplasia (BPH) include a digital rectal exam, blood and imaging tests, a urine flow study, and examination with a scope called a cystoscope. Treatments include watchful waiting, medicines, nonsurgical procedures, and surgery.
Benign prostatic hyperplasia symptoms
The severity of symptoms in people who have prostate gland enlargement varies, but symptoms tend to gradually worsen over time. Common signs and symptoms of benign prostatic hyperplasia include:
- Frequent or urgent need to urinate
- Increased frequency of urination at night (nocturia)
- Difficulty starting urination
- Weak urine stream or a stream that stops and starts
- Dribbling at the end of urination
- Straining while urinating
- Inability to completely empty the bladder
Less common signs and symptoms include:
- Urinary tract infection
- Inability to urinate
- Blood in the urine
The size of your prostate doesn’t necessarily mean your symptoms will be worse. Some men with only slightly enlarged prostates can have significant symptoms, while other men with very enlarged prostates can have only minor urinary symptoms.
In some men, symptoms eventually stabilize and might even improve over time.
Benign prostatic hyperplasia causes
The prostate gland is located beneath your bladder. The tube that transports urine from the bladder out of your penis (urethra) passes through the center of the prostate. When the prostate enlarges, it begins to block urine flow.
Most men have continued prostate growth throughout life. In many men, this continued growth enlarges the prostate enough to cause urinary symptoms or to significantly block urine flow.
It isn’t entirely clear what causes the prostate to enlarge. However, it might be due to changes in the balance of sex hormones as men grow older.
Risk factors for benign prostatic hyperplasia
Risk factors for prostate gland enlargement include:
- Aging. Prostate gland enlargement rarely causes signs and symptoms in men younger than age 40. About one-third of men experience moderate to severe symptoms by age 60, and about half do so by age 80.
- Family history. Having a blood relative, such as a father or brother, with prostate problems means you’re more likely to have problems.
- Ethnic background. Prostate enlargement is less common in Asian men than in white and black men. Black men might experience symptoms at a younger age than white men.
- Diabetes and heart disease. Studies show that diabetes, as well as heart disease and use of beta blockers, might increase the risk of benign prostatic hyperplasia.
- Lifestyle. Obesity increases the risk of benign prostatic hyperplasia, while exercise can lower your risk.
Benign prostatic hyperplasia complications
Complications of enlarged prostate can include:
- Sudden inability to urinate (urinary retention). You might need to have a tube (catheter) inserted into your bladder to drain the urine. Some men with an enlarged prostate need surgery to relieve urinary retention.
- Urinary tract infections (UTIs). Inability to fully empty the bladder can increase the risk of infection in your urinary tract. If UTIs occur frequently, you might need surgery to remove part of the prostate.
- Bladder stones. These are generally caused by an inability to completely empty the bladder. Bladder stones can cause infection, bladder irritation, blood in the urine and obstruction of urine flow.
- Bladder damage. A bladder that hasn’t emptied completely can stretch and weaken over time. As a result, the muscular wall of the bladder no longer contracts properly, making it harder to fully empty your bladder.
- Kidney damage. Pressure in the bladder from urinary retention can directly damage the kidneys or allow bladder infections to reach the kidneys.
Most men with an enlarged prostate don’t develop these complications. However, acute urinary retention and kidney damage can be serious health threats.
Having an enlarged prostate doesn’t affect your risk of developing prostate cancer.
Benign prostatic hyperplasia diagnosis
Your doctor will start by asking detailed questions about your symptoms and doing a physical exam. This initial exam is likely to include:
- Digital rectal exam. The doctor inserts a finger into the rectum to check your prostate for enlargement.
- Urine test. Analyzing a sample of your urine can help rule out an infection or other conditions that can cause similar symptoms.
- Blood test. The results can indicate kidney problems.
- Prostate-specific antigen (PSA) blood test. PSA is a substance produced in your prostate. PSA levels increase when you have an enlarged prostate. However, elevated PSA levels can also be due to recent procedures, infection, surgery or prostate cancer.
- Neurological exam. This brief evaluation of your mental functioning and nervous system can help identify causes of urinary problems other than enlarged prostate.
After that, your doctor might recommend additional tests to help confirm an enlarged prostate and to rule out other conditions. These additional tests might include:
- Urinary flow test. You urinate into a receptacle attached to a machine that measures the strength and amount of your urine flow. Test results help determine over time if your condition is getting better or worse.
- Postvoid residual volume test. This test measures whether you can empty your bladder completely. The test can be done using ultrasound or by inserting a catheter into your bladder after you urinate to measure how much urine is left in your bladder.
- 24-hour voiding diary. Recording the frequency and amount of urine might be especially helpful if more than one-third of your daily urinary output occurs at night.
If your condition is more complex, your doctor may recommend:
- Transrectal ultrasound. An ultrasound probe is inserted into your rectum to measure and evaluate your prostate.
- Prostate biopsy. Transrectal ultrasound guides needles used to take tissue samples (biopsies) of the prostate. Examining the tissue can help your doctor diagnose or rule out prostate cancer.
- Urodynamic and pressure flow studies. A catheter is threaded through your urethra into your bladder. Water — or, less commonly, air — is slowly injected into your bladder. Your doctor can then measure bladder pressure and determine how well your bladder muscles are working.
- Cystoscopy. A lighted, flexible cystoscope is inserted into your urethra, allowing your doctor to see inside your urethra and bladder. You will be given a local anesthetic before this test.
- Intravenous pyelogram or CT urogram. A tracer is injected into a vein. X-rays or CT scans are then taken of your kidneys, bladder and the tubes that connect your kidneys to your bladder (ureters). These tests can help detect urinary tract stones, tumors or blockages above the bladder.
Benign prostatic hyperplasia treatment
A wide variety of treatments are available for enlarged prostate, including medication, minimally invasive therapies and surgery. The best treatment choice for you depends on several factors, including:
- The size of your prostate
- Your age
- Your overall health
- The amount of discomfort or bother you are experiencing
If your symptoms are tolerable, you might decide to postpone treatment and simply monitor your symptoms. For some men, symptoms can ease without treatment.
Medication
Medication is the most common treatment for mild to moderate symptoms of prostate enlargement. The options include:
- Alpha blockers. These medications relax bladder neck muscles and muscle fibers in the prostate, making urination easier. Alpha blockers — which include alfuzosin (Uroxatral), doxazosin (Cardura), tamsulosin (Flomax), and silodosin (Rapaflo) — usually work quickly in men with relatively small prostates. Side effects might include dizziness and a harmless condition in which semen goes back into the bladder instead of out the tip of the penis (retrograde ejaculation).
- 5-alpha reductase inhibitors. These medications shrink your prostate by preventing hormonal changes that cause prostate growth. These medications — which include finasteride (Proscar) and dutasteride (Avodart) — might take up to six months to be effective. Side effects include retrograde ejaculation.
- Combination drug therapy. Your doctor might recommend taking an alpha blocker and a 5-alpha reductase inhibitor at the same time if either medication alone isn’t effective.
- Tadalafil (Cialis). Studies suggest this medication, which is often used to treat erectile dysfunction, can also treat prostate enlargement. However, this medication is not routinely used for enlarged prostate and is generally prescribed only to men who also experience erectile dysfunction.
Minimally invasive or surgical therapy
Minimally invasive or surgical therapy might be recommended if:
- Your symptoms are moderate to severe
- Medication hasn’t relieved your symptoms
- You have a urinary tract obstruction, bladder stones, blood in your urine or kidney problems
- You prefer definitive treatment
Minimally invasive or surgical therapy might not be an option if you have:
- An untreated urinary tract infection
- Urethral stricture disease
- A history of prostate radiation therapy or urinary tract surgery
- A neurological disorder, such as Parkinson’s disease or multiple sclerosis
Any type of prostate procedure can cause side effects. Depending on the procedure you choose, complications might include:
- Semen flowing backward into the bladder instead of out through the penis during ejaculation
- Temporary difficulty with urination
- Urinary tract infection
- Bleeding
- Erectile dysfunction
- Very rarely, loss of bladder control (incontinence)
There are several types of minimally invasive or surgical therapy.
Transurethral resection of the prostate (TURP)
A lighted scope is inserted into your urethra, and the surgeon removes all but the outer part of the prostate. TURP generally relieves symptoms quickly, and most men have a stronger urine flow soon after the procedure. After TURP you might temporarily need a catheter to drain your bladder, and you’ll be able to do only light activity until you’ve healed.
Transurethral incision of the prostate (TUIP)
A lighted scope is inserted into your urethra, and the surgeon makes one or two small cuts in the prostate gland — making it easier for urine to pass through the urethra. This surgery might be an option if you have a small or moderately enlarged prostate gland, especially if you have health problems that make other surgeries too risky.
Transurethral microwave thermotherapy (TUMT)
Your doctor inserts a special electrode through your urethra into your prostate area. Microwave energy from the electrode destroys the inner portion of the enlarged prostate gland, shrinking it and easing urine flow. This surgery is generally used only on small prostates in special circumstances because re-treatment might be necessary.
Transurethral needle ablation (TUNA)
In this outpatient procedure, a scope is passed into your urethra, allowing your doctor to place needles into your prostate gland. Radio waves pass through the needles, heating and destroying excess prostate tissue that’s blocking urine flow.
This procedure might be a good choice if you bleed easily or have certain other health problems. However, like TUMT, TUNA might only partially relieve your symptoms and it might take some time before you notice results.
Laser therapy
A high-energy laser destroys or removes overgrown prostate tissue. Laser therapy generally relieves symptoms right away and has a lower risk of side effects than does nonlaser surgery. Laser therapy might be used in men who shouldn’t have other prostate procedures because they take blood-thinning medications.
The options for laser therapy include:
- Ablative procedures. These procedures vaporize obstructive prostate tissue to increase urine flow. Examples include photoselective vaporization of the prostate (PVP) and holmium laser ablation of the prostate (HoLAP). Ablative procedures can cause irritating urinary symptoms after surgery, so in rare situations another resection procedure might be needed at some point.
- Enucleative procedures. Enucleative procedures, such as holmium laser enucleation of the prostate (HoLEP), generally remove all the prostate tissue blocking urine flow and prevent regrowth of tissue. The removed tissue can be examined for prostate cancer and other conditions. These procedures are similar to open prostatectomy.
Prostate lift
In this experimental transurethral procedure, special tags are used to compress the sides of the prostate to increase the flow of urine. Long-term data on the effectiveness of this procedure aren’t available.
Embolization
In this experimental procedure, the blood supply to or from the prostate is selectively blocked, causing the prostate to decrease in size. Long-term data on the effectiveness of this procedure aren’t available.
Open or robot-assisted prostatectomy
The surgeon makes an incision in your lower abdomen to reach the prostate and remove tissue. Open prostatectomy is generally done if you have a very large prostate, bladder damage or other complicating factors. The surgery usually requires a short hospital stay and is associated with a higher risk of needing a blood transfusion.
Follow-up care
Your follow-up care will depend on the specific technique used to treat your enlarged prostate.
Your doctor might recommend limiting heavy lifting and excessive exercise for seven days if you have laser ablation, transurethral needle ablation or transurethral microwave therapy. If you have open or robot-assisted prostatectomy, you might need to restrict activity for six weeks.
Whichever procedure you have, your doctor likely will suggest that you drink plenty of fluids afterward.
Home remedies for enlarged prostate
To help control the symptoms of an enlarged prostate, try to:
- Limit beverages in the evening. Don’t drink anything for an hour or two before bedtime to avoid middle-of-the-night trips to the toilet.
- Limit caffeine and alcohol. They can increase urine production, irritate the bladder and worsen symptoms.
- Limit decongestants or antihistamines. These drugs tighten the band of muscles around the urethra that control urine flow, making it harder to urinate.
- Go when you first feel the urge. Waiting too long might overstretch the bladder muscle and cause damage.
- Schedule bathroom visits. Try to urinate at regular times — such as every four to six hours during the day — to “retrain” the bladder. This can be especially useful if you have severe frequency and urgency.
- Follow a healthy diet. Obesity is associated with enlarged prostate.
- Stay active. Inactivity contributes to urine retention. Even a small amount of exercise can help reduce urinary problems caused by an enlarged prostate.
- Urinate — and then urinate again a few moments later. This practice is known as double voiding.
- Keep warm. Colder temperatures can cause urine retention and increase the urgency to urinate.
The Food and Drug Administration hasn’t approved any herbal medications for treatment of an enlarged prostate.
Studies on herbal therapies as a treatment for enlarged prostate have had mixed results. One study found that saw palmetto extract was as effective as finasteride in relieving symptoms of benign prostatic hyperplasia, although prostate volumes weren’t reduced. But a subsequent placebo-controlled trial found no evidence that saw palmetto is better than a placebo.
Other herbal treatments — including beta-sitosterol extracts, pygeum and rye grass — have been suggested as helpful for reducing enlarged prostate symptoms. But the safety and efficacy of these treatments hasn’t been proved.
If you take any herbal remedies, tell your doctor. Certain herbal products might increase the risk of bleeding or interfere with other medications you’re taking.
Prostate cancer signs and symptoms
Early prostate cancer usually causes no symptoms.
Prostate cancer that’s more advanced may cause signs and symptoms such as:
- Problems urinating (such as pain, difficulty starting or stopping the stream, or dribbling), including a slow or weak urinary stream or the need to urinate more often, especially at night
- Pain with ejaculation
- Blood in the urine or semen
- Trouble getting an erection (erectile dysfunction)
- Pain in the hips, back (spine), chest (ribs), or other areas from cancer that has spread to bones
- Weakness or numbness in the legs or feet, or even loss of bladder or bowel control from cancer pressing on the spinal cord
Most of these problems are more likely to be caused by something other than prostate cancer. For example, trouble urinating is much more often caused by benign prostatic hyperplasia (BPH), a non-cancerous growth of the prostate. Still, it’s important to tell your health care provider if you have any of these symptoms so that the cause can be found and treated, if needed. Some men might need more tests to check for prostate cancer.
Prostate cancer types
Almost all prostate cancers are adenocarcinomas 24. These cancers develop from the gland cells (the cells that make the prostate fluid that is added to the semen).
There are 2 types of adenocarcinoma of the prostate:
- Acinar adenocarcinoma of the prostate: Most people have this type. It develops in the gland cells that line the prostate gland.
- Ductal adenocarcinoma of the prostate: Ductal adenocarcinoma starts in the cells that line the tubes (ducts) of the prostate gland. It tends to grow and spread more quickly than acinar adenocarcinoma.
Other types of prostate cancer include:
- Sarcomas
- Small cell carcinomas. Small cell prostate cancer can also be classed as a type of neuroendocrine cancer. They tend to grow more quickly than other types of prostate cancer.
- Neuroendocrine tumors (other than small cell carcinomas)
- Squamous cell carcinoma of the prostate. Squamous cell carcinoma of the prostate develop from flat cells that cover the prostate. They tend to grow and spread more quickly than adenocarcinoma of the prostate.
- Transitional cell carcinomas also called urothelial carcinoma of the prostate. Transitional cell carcinoma of the prostate starts in the cells that line the tube carrying urine to the outside of the body (the urethra). This type of cancer usually starts in the bladder and spreads into the prostate. But rarely it can start in the prostate and may spread into the bladder entrance and nearby tissues. Between 2 and 4 out of 100 prostate cancers (between 2 and 4%) are transitional cell carcinoma.
These other types of prostate cancer are rare. If you have prostate cancer it is almost certain to be an adenocarcinoma 24.
Some prostate cancers can grow and spread quickly, but most grow slowly. In fact, autopsy studies show that many older men (and even some younger men) who died of other causes also had prostate cancer that never affected them during their lives. In many cases neither they nor their doctors even knew they had it.
Possible pre-cancerous conditions of the prostate
Some research suggests that prostate cancer starts out as a pre-cancerous condition, although this is not yet known for sure 24. These conditions are sometimes found when a man has a prostate biopsy (removal of small pieces of the prostate to look for cancer).
Prostatic intraepithelial neoplasia (PIN)
In prostatic intraepithelial neoplasia, there are changes in how the prostate gland cells look under a microscope, but the abnormal cells don’t look like they are growing into other parts of the prostate (like cancer cells would) 24. Based on how abnormal the patterns of cells look, they are classified as:
- Low-grade prostatic intraepithelial neoplasia: the patterns of prostate cells appear almost normal
- High-grade prostatic intraepithelial neoplasia: the patterns of cells look more abnormal
Prostatic intraepithelial neoplasia begins to appear in the prostates of some men as early as in their 20s.
Many men begin to develop low-grade prostatic intraepithelial neoplasia when they are younger but don’t necessarily develop prostate cancer. The possible link between low-grade prostatic intraepithelial neoplasia and prostate cancer is still unclear.
If high-grade prostatic intraepithelial neoplasia is found in your prostate biopsy sample, there is about a 20% chance that you also have cancer in another area of your prostate.
Proliferative inflammatory atrophy (PIA)
In proliferative inflammatory atrophy, the prostate cells look smaller than normal and there are signs of inflammation in the area 24. Proliferative inflammatory atrophy is not cancer, but researchers believe that proliferative inflammatory atrophy may sometimes lead to high-grade prostatic intraepithelial neoplasia, or perhaps to prostate cancer directly.
Prostate cancer causes
Researchers do not know exactly what causes prostate cancer. Doctors know that prostate cancer begins when cells in the prostate develop changes in their DNA. A cell’s DNA contains the instructions that tell a cell what to do. The changes tell the cells to grow and divide more rapidly than normal cells do. The abnormal cells continue living, when other cells would die.
The accumulating abnormal cells form a tumor that can grow to invade nearby tissue. In time, some abnormal cells can break away and spread (metastasize) to other parts of the body.
In the U.S., about 1 out of 8 men will be diagnosed with prostate cancer during his lifetime. Prostate cancer is more likely to develop in older men and in non-Hispanic Black men. About 6 cases in 10 are diagnosed in men who are 65 or older, and it is rare in men under 40. The average age of men at diagnosis is about 66.
Prostate cancer is more common in Black men than in White men. It is less common in Asian men. A man’s risk of developing prostate cancer depends on many factors. These include:
- age
- genetics and family history
- lifestyle factors
- other medical conditions
Inherited gene mutations
Some gene mutations can be passed from generation to generation (inherited) and are found in all cells in the body. Inherited gene changes are thought to play a role in about 10% of prostate cancers. Cancer caused by inherited genes is called hereditary cancer. Several inherited mutated genes have been linked to hereditary prostate cancer, including:
- BRCA1 and BRCA2: These tumor suppressor genes normally help repair mistakes in a cell’s DNA (or cause the cell to die if the mistake can’t be fixed). Inherited mutations in these genes more commonly cause breast and ovarian cancer in women. But changes in these genes (especially BRCA2) also account for a small number of prostate cancers.
- CHEK2, ATM, PALB2, and RAD51D: Mutations in these other DNA repair genes might also be responsible for some hereditary prostate cancers.
- DNA mismatch repair genes such as MSH2, MSH6, MLH1, and PMS2: These genes normally help fix mistakes (mismatches) in DNA that can be made when a cell is preparing to divide into 2 new cells. Cells must make a new copy of their DNA each time they divide. Men with inherited mutations in one of these genes have a condition known as Lynch syndrome (also known as hereditary non-polyposis colorectal cancer, or HNPCC), and are at increased risk of colorectal, prostate, and some other cancers.
- RNASEL (formerly HPC1): The normal function of this tumor suppressor gene is to help cells die when something goes wrong inside them. Inherited mutations in this gene might let abnormal cells live longer than they should, which can lead to an increased risk of prostate cancer.
- HOXB13: This gene is important in the development of the prostate gland. Mutations in this gene have been linked to early-onset prostate cancer (prostate cancer diagnosed at a young age) that runs in some families. Fortunately, this mutation is rare.
Other inherited gene mutations may account for some hereditary prostate cancers, and research is being done to find these genes.
Acquired gene mutations
Some genes mutate during a person’s lifetime, and the mutation is not passed on to children. These changes are found only in cells that come from the original mutated cell. These are called acquired mutations. Most gene mutations related to prostate cancer seem to develop during a man’s life rather than having been inherited.
Every time a cell prepares to divide into 2 new cells, it must copy its DNA. This process isn’t perfect, and sometimes errors occur, leaving defective DNA in the new cell. It’s not clear how often these DNA changes might be random events, and how often they are influenced by other factors (such as diet, hormone levels, etc.). In general, the more quickly prostate cells grow and divide, the more chances there are for mutations to occur. Therefore, anything that speeds up this process may make prostate cancer more likely.
For example, androgens (male hormones), such as testosterone, promote prostate cell growth. Having higher levels of androgens might contribute to prostate cancer risk in some men.
Some research has found that men with high levels of another hormone, insulin-like growth factor-1 (IGF-1), are more likely to get prostate cancer. However, other studies have not found such a link. Further research is needed to make sense of these findings.
Prostate Cancer Risk Factors
A risk factor is anything that affects your chance of getting a disease such as cancer. But having a risk factor, or even several, does not mean that you will get the disease. Many people with one or more risk factors never get cancer, while others who get cancer may have had few or no known risk factors.
Researchers have found several factors that might affect a man’s risk of getting prostate cancer.
- Age. Prostate cancer is rare in men younger than 40, but the chance of having prostate cancer rises rapidly after age 50. About 6 in 10 prostate cancers are found in men older than 65.
- Race/ethnicity. Prostate cancer occurs more often in African-American men and Caribbean men of African ancestry than in men of other races. African-American men are also more than twice as likely to die of prostate cancer than white men. Prostate cancer occurs less often in Asian-American and Hispanic/Latino men than in non-Hispanic whites. The reasons for these racial and ethnic differences are not clear.
- Geography. Prostate cancer is most common in North America, northwestern Europe, Australia, and on Caribbean islands. It is less common in Asia, Africa, Central America, and South America. The reasons for this are not clear. More intensive screening in some developed countries probably accounts for at least part of this difference, but other factors such as lifestyle differences (diet, etc.) are likely to be important as well. For example, Asian Americans have a lower risk of prostate cancer than white Americans, but their risk is higher than that of men of similar backgrounds living in Asia.
- Family history. Prostate cancer seems to run in some families, which suggests that in some cases there may be an inherited or genetic factor. Still, most prostate cancers occur in men without a family history of it. Having a father or brother with prostate cancer more than doubles a man’s risk of developing this disease. The risk is higher for men who have a brother with the disease than for those who have a father with it. The risk is much higher for men with several affected relatives, particularly if their relatives were young when the cancer was found.
- Gene changes. Several inherited gene changes (mutations) seem to raise prostate cancer risk, but they probably account for only a small percentage of cases overall. For example:
- Inherited mutations of the BRCA1 or BRCA2 genes raise the risk of breast and ovarian cancers in some families. Mutations in these genes (especially in BRCA2) may also increase prostate cancer risk in some men.
- Men with Lynch syndrome also known as hereditary non-polyposis colorectal cancer (HNPCC), a condition caused by inherited gene changes, have an increased risk for a number of cancers, including prostate cancer.
- Other inherited gene changes can also raise a man’s risk of prostate cancer.
Factors with less clear effect on prostate cancer risk
- Diet. The exact role of diet in prostate cancer is not clear, but several factors have been studied. Men who eat a lot of red meat or high-fat dairy products appear to have a slightly higher chance of getting prostate cancer. These men also tend to eat fewer fruits and vegetables. Doctors aren’t sure which of these factors is responsible for raising the risk. Some studies have suggested that men who consume a lot of calcium (through food or supplements) may have a higher risk of developing prostate cancer. Dairy foods (which are often high in calcium) might also increase risk. But most studies have not found such a link with the levels of calcium found in the average diet, and it’s important to note that calcium has other important health benefits.
- Obesity. Being obese (very overweight) does not seem to increase the overall risk of getting prostate cancer. Some studies have found that obese men have a lower risk of getting a low-grade (slower growing) form of the disease, but a higher risk of getting more aggressive (faster growing) prostate cancer. The reasons for this are not clear. Some studies have also found that obese men may be at greater risk for having more advanced prostate cancer and of dying from prostate cancer, but not all studies have found this.
- Smoking. Most studies have not found a link between smoking and getting prostate cancer. Some research has linked smoking to a possible small increased risk of dying from prostate cancer, but this finding needs to be confirmed by other studies.
- Chemical exposures. There is some evidence that firefighters can be exposed to chemicals that may increase their risk of prostate cancer. A few studies have suggested a possible link between exposure to Agent Orange, a chemical used widely during the Vietnam War, and prostate cancer, although not all studies have found such a link. The Institute of Medicine considers there to be “limited/suggestive evidence” of a link between Agent Orange exposure and prostate cancer.
- Inflammation of the prostate. Some studies have suggested that prostatitis (inflammation of the prostate gland) may be linked to an increased risk of prostate cancer, but other studies have not found such a link. Inflammation is often seen in samples of prostate tissue that also contain cancer. The link between the two is not yet clear, and is an active area of research.
- Sexually transmitted infections (STIs). Researchers have looked to see if sexually transmitted infections (like gonorrhea or chlamydia) might increase the risk of prostate cancer, because they can lead to inflammation of the prostate. So far, studies have not agreed, and no firm conclusions have been reached.
- Vasectomy. Some studies have suggested that men who have a vasectomy (minor surgery to make men infertile) have a slightly increased risk for prostate cancer, but other studies have not found this. Research on this possible link is still being done.
Prostate cancer prevention
There is no sure way to prevent prostate cancer. Many risk factors such as age, race, and family history can’t be controlled. But there are some things you can do that might lower your risk for this disease.
Body weight, physical activity, and diet
The effects of body weight, physical activity, and diet on prostate cancer risk are not clear, but there are things you can do that might lower your risk.
Some studies have found that men who are overweight may have a slightly lower risk of prostate cancer overall, but a higher risk of prostate cancers that are likely to be fatal.
Studies have found that men who are regularly physically active have a slightly lower risk of prostate cancer. Vigorous activity may have a greater effect, especially on the risk of advanced prostate cancer.
Several studies have suggested that diets high in certain vegetables (including tomatoes, cruciferous vegetables, soy, beans, and other legumes) or fish may be linked with a lower risk of prostate cancer, especially more advanced cancers. Examples of cruciferous vegetables include cabbage, broccoli, and cauliflower.
Although not all studies agree, several have found a higher risk of prostate cancer in men whose diets are high in calcium. There may also be an increased risk from consuming dairy foods.
For now, the best advice about diet and activity to possibly reduce the risk of prostate cancer is to:
- Follow a healthy eating pattern, which includes a variety of colorful fruits and vegetables and whole grains, and avoids or limits red and processed meats, sugar-sweetened beverages, and highly processed foods.
- Be physically active.
- Stay at a healthy weight.
It may also be sensible to limit calcium supplements and to not get too much calcium in the diet. This does not mean that men who are being treated for prostate cancer should not take calcium supplements if their doctor recommends them.
Vitamin, mineral, and other supplements
- Vitamin E and selenium: Some earlier studies suggested that taking vitamin E or selenium supplements might lower prostate cancer risk. But in a large study known as the Selenium and Vitamin E Cancer Prevention Trial (SELECT), neither vitamin E nor selenium supplements were found to lower prostate cancer risk. In fact, men in the study taking the vitamin E supplements were later found to have a slightly higher risk of prostate cancer.
- Soy and isoflavones: Some early research has suggested possible benefits from soy proteins called isoflavones in lowering prostate cancer risk. Several studies are now looking more closely at the possible effects of these proteins.
Taking any supplements can have both risks and benefits. Before starting vitamins or other supplements, talk with your doctor.
Medicines
Some drugs might help reduce the risk of prostate cancer.
- 5-alpha reductase inhibitors. 5-alpha reductase is an enzyme in the body that changes testosterone into dihydrotestosterone (DHT), the main hormone that causes the prostate to grow. Drugs called 5-alpha reductase inhibitors, such as finasteride (Proscar) and dutasteride (Avodart), block this enzyme from making DHT. These drugs are used to treat benign prostatic hyperplasia (BPH), a non-cancerous growth of the prostate. Large studies of both of these drugs have been done to see if they might also be useful in lowering prostate cancer risk. In these studies, men taking either drug were less likely to develop prostate cancer after several years than men getting an inactive placebo. When the results were looked at more closely, the men who took these drugs had fewer low-grade prostate cancers, but they had about the same (or a slightly higher) risk of higher-grade prostate cancers, which are more likely to grow and spread. Long term, it’s not clear if these drugs affect death rates, as men in these studies had similar survival whether or not they took one of these drugs. These drugs can cause sexual side effects such as lowered sexual desire and erectile dysfunction (impotence), as well as the growth of breast tissue in some men. But they can help with urinary problems from BPH such as trouble urinating and leaking urine (incontinence). These drugs aren’t approved by the FDA specifically to help prevent prostate cancer, although doctors can prescribe them “off label” for this use. Right now, it isn’t clear that taking one of these drugs just to lower prostate cancer risk is very helpful. Still, men who want to know more about these drugs should discuss them with their doctors.
- Aspirin. Some research suggests that men who take a daily aspirin might have a lower risk of getting and dying from prostate cancer. But more research is needed to show if the possible benefits outweigh the risks. Long-term aspirin use can have side effects, including an increased risk of bleeding in the digestive tract. While aspirin can also have other health benefits, at this time most doctors don’t recommend taking it just to try to lower prostate cancer risk.
- Other drugs. Other drugs and dietary supplements that might help lower prostate cancer risk are now being studied. But so far, no drug or supplement has been found to be helpful in studies large enough for experts to recommend them.
Prostate cancer screening
Screening is testing to find cancer in people before they have symptoms. For some types of cancer, screening can help find cancers at an early stage, when they are likely to be easier to treat. However, testing healthy men with no symptoms for prostate cancer is controversial. There is some disagreement among medical organizations whether the benefits of testing outweigh the potential risks. Most medical organizations encourage men in their 50s to discuss the pros and cons of prostate cancer screening with their doctors. The discussion should include a review of your risk factors and your preferences about screening. You might consider starting the discussions sooner if you’re a Black person, have a family history of prostate cancer or have other risk factors.
Prostate cancer can often be found before symptoms start by testing the amount of prostate-specific antigen (PSA) in a man’s blood. Another way to find prostate cancer is the digital rectal exam (DRE), in which the doctor puts a gloved, lubricated finger into the rectum to feel the prostate gland.
Prostate screening tests might include:
- Digital rectal exam (DRE). During a digital rectal exam (DRE), your doctor inserts a gloved, lubricated finger into your rectum to examine your prostate, which is adjacent to the rectum. This exam can be uncomfortable (especially for men who have hemorrhoids), but it usually isn’t painful and only takes a short time. If your doctor finds any abnormalities in the texture, shape or size of the gland, you may need further tests.
- Prostate-specific antigen (PSA) test. Prostate-specific antigen (PSA) is a protein made by cells in the prostate gland (both normal cells and cancer cells). PSA is mostly found in semen, but a small amount is also found in blood. The PSA level in blood is measured in units called nanograms per milliliter (ng/mL). The chance of having prostate cancer goes up as the PSA level goes up, but there is no set cutoff point for PSA level that can tell for sure if a man does or doesn’t have prostate cancer. Many doctors use a PSA cutoff point of 4 ng/mL or higher when deciding if a man might need further testing, while others might recommend it starting at a lower level, such as 2.5 or 3 ng/mL.
- Most men without prostate cancer have PSA levels under 4 ng/mL of blood. When prostate cancer develops, the PSA level often goes above 4 ng/mL. Still, a level below 4 ng/mL is not a guarantee that a man doesn’t have cancer. About 15% of men with a PSA below 4 ng/mL will have prostate cancer if a biopsy is done.
- Men with a PSA level between 4 and 10 ng/mL (often called the “borderline range”) have about a 1 in 4 chance of having prostate cancer.
- If the PSA is more than 10, the chance of having prostate cancer is over 50%.
- If your PSA level is high, you might need further tests to look for prostate cancer (e.g., prostate biopsy). For some men, getting a prostate biopsy might be the best option, especially if the initial PSA level is high. A biopsy is a procedure in which small samples of the prostate are removed and then looked at under a microscope. This test is the only way to know for sure if a man has prostate cancer. If prostate cancer is found on a biopsy, this test can also help tell how likely it is that the cancer will grow and spread quickly.
One reason it’s hard to use a set cutoff point with the PSA test when looking for prostate cancer is that a number of factors other than cancer can also affect PSA levels.
Factors that might raise PSA levels include:
- An enlarged prostate: Conditions such as benign prostatic hyperplasia (BPH), a non-cancerous enlargement of the prostate that affects many men as they grow older, can raise PSA levels.
- Older age: PSA levels normally go up slowly as you get older, even if you have no prostate abnormality.
- Prostatitis: This is an infection or inflammation of the prostate gland, which can raise PSA levels.
- Ejaculation: This can make the PSA go up for a short time. This is why some doctors suggest that men abstain from ejaculation for a day or two before testing.
- Riding a bicycle: Some studies have suggested that cycling may raise PSA levels for a short time (possibly because the seat puts pressure on the prostate), although not all studies have found this.
- Certain urologic procedures: Some procedures done in a doctor’s office that affect the prostate, such as a prostate biopsy or cystoscopy, can raise PSA levels for a short time. Some studies have suggested that a digital rectal exam (DRE) might raise PSA levels slightly, although other studies have not found this. Still, if both a PSA test and a DRE are being done during a doctor visit, some doctors advise having the blood drawn for the PSA before having the DRE, just in case.
- Certain medicines: Taking male hormones like testosterone (or other medicines that raise testosterone levels) may cause a rise in PSA.
Some things might lower PSA levels (even if a man has prostate cancer):
- 5-alpha reductase inhibitors: Certain drugs used to treat BPH or urinary symptoms, such as finasteride (Proscar or Propecia) or dutasteride (Avodart), can lower PSA levels. These drugs can also affect prostate cancer risk (discussed in Can Prostate Cancer Be Prevented?). Tell your doctor if you are taking one of these medicines. Because they can lower PSA levels, the doctor might need to adjust for this.
- Herbal mixtures: Some mixtures that are sold as dietary supplements might mask a high PSA level. This is why it’s important to let your doctor know if you are taking any type of supplement, even ones that are not necessarily meant for prostate health. Saw palmetto (an herb used by some men to treat BPH) does not seem to affect PSA.
- Certain other medicines: Some research has suggested that long-term use of certain medicines, such as aspirin, statins (cholesterol-lowering drugs), and thiazide diuretics (such as hydrochlorothiazide) might lower PSA levels. More research is needed to confirm these findings. If you take any of the medicines regularly, talk to your doctor before you stop taking it for any reason.
For men who might be screened for prostate cancer, it’s not always clear if lowering the PSA is helpful. In some cases the factor that lowers the PSA may also lower a man’s risk of prostate cancer. But in other cases, it might lower the PSA level without affecting a man’s risk of cancer. This could actually be harmful, if it were to lower the PSA from an abnormal level to a normal one, as it might result in not detecting a cancer. This is why it’s important to talk to your doctor about anything that might affect your PSA level.
Special types of PSA tests
Some doctors might consider using different types of PSA tests (discussed below) to help decide if you need a prostate biopsy, but not all doctors agree on how to use these other PSA tests. If your PSA test result isn’t normal, ask your doctor to discuss your cancer risk and your need for further tests.
- Percent-free PSA: PSA occurs in 2 major forms in the blood. One form is attached to blood proteins, while the other circulates free (unattached). The percent-free PSA (fPSA) is the ratio of how much PSA circulates free compared to the total PSA level. The percentage of free PSA is lower in men who have prostate cancer than in men who do not. This test is sometimes used to help decide if you should have a prostate biopsy if your PSA results are in the borderline range (like between 4 and 10). A lower percent-free PSA means that your chance of having prostate cancer is higher and you should probably have a biopsy. Many doctors recommend biopsies for men whose percent-free PSA is 10% or less, and advise that men consider a biopsy if it is between 10% and 25%. Using these cutoffs detects most cancers and helps some men avoid unnecessary prostate biopsies. This test is widely used, but not all doctors agree that 25% is the best cutoff point to decide on a biopsy, and the cutoff may change depending on the overall PSA level.
- Complexed PSA: This test directly measures the amount of PSA that is attached to other proteins (the portion of PSA that is not “free”). This test could be done instead of checking the total and free PSA, and it could give the same amount of information as the other tests done separately. This test is being studied to see if it provides the same level of accuracy. Tests that combine different types of PSA: Some newer tests, such as the prostate health index (phi) and the 4Kscore test, combine the results of different types of PSA to get an overall score that reflects the chance a man has prostate cancer. These tests might be useful in men with a slightly elevated PSA, to help determine if they should have a prostate biopsy. Some tests might be used to help determine if a man who has already had a prostate biopsy that didn’t find cancer should have another biopsy.
- The Prostate Health Index (PHI), which combines the results of total PSA, free PSA, and proPSA
- The 4Kscore test, which combines the results of total PSA, free PSA, intact PSA, and human kallikrein 2 (hK2), along with some other factors
- PSA velocity: The PSA velocity is not a separate test. It is a measure of how fast the PSA rises over time. Normally, PSA levels go up slowly with age. Some research has found that these levels go up faster if a man has cancer, but studies have not shown that the PSA velocity is more helpful than the PSA level itself in finding prostate cancer. For this reason, the American Cancer Society guidelines do not recommend using the PSA velocity as part of screening for prostate cancer.
- PSA density: PSA levels are higher in men with larger prostate glands. The PSA density (PSAD) is sometimes used for men with large prostate glands to try to adjust for this. The doctor measures the volume (size) of the prostate gland with transrectal ultrasound and divides the PSA number by the prostate volume. A higher PSA density indicates a greater likelihood of cancer. PSA density has not been shown to be as useful as the percent-free PSA test.
- Age-specific PSA ranges: PSA levels are normally higher in older men than in younger men, even when there is no cancer. A PSA result within the borderline range might be very worrisome in a 50-year-old man but cause less concern in an 80-year-old man. For this reason, some doctors have suggested comparing PSA results with results from other men of the same age. But because the usefulness of age-specific PSA ranges is not well proven, most doctors and professional organizations (as well as the makers of the PSA tests) do not recommend their use at this time.
Figure 2. Digital rectal exam (DRE)
American Cancer Society Recommendations for Prostate Cancer Early Detection
The American Cancer Society recommends that men have a chance to make an informed decision with their health care provider about whether to be screened for prostate cancer 25. The decision should be made after getting information about the uncertainties, risks, and potential benefits of prostate cancer screening. Men should not be screened unless they have received this information. The discussion about screening should take place at:
- Age 50 for men who are at average risk of prostate cancer and are expected to live at least 10 more years.
- Age 45 for men at high risk of developing prostate cancer. This includes African Americans and men who have a first-degree relative (father, brother, or son) diagnosed with prostate cancer at an early age (younger than age 65).
- Age 40 for men at even higher risk (those with more than one first-degree relative who had prostate cancer at an early age).
After this discussion, men who want to be screened should be tested with the prostate-specific antigen (PSA) blood test. The digital rectal exam may also be done as a part of screening.
If, after this discussion, a man is unable to decide if testing is right for him, the screening decision can be made by the health care provider, who should take into account the man’s general health preferences and values.
If no prostate cancer is found as a result of screening, the time between future screenings depends on the results of the PSA blood test:
- Men who choose to be tested who have a PSA of less than 2.5 ng/mL may only need to be retested every 2 years.
- Screening should be done yearly for men whose PSA level is 2.5 ng/mL or higher.
Because prostate cancer often grows slowly, men without symptoms of prostate cancer who do not have a 10-year life expectancy should not be offered testing since they are not likely to benefit. Overall health status, and not age alone, is important when making decisions about screening.
Even after a decision about testing has been made, the discussion about the pros and cons of testing should be repeated as new information about the benefits and risks of testing becomes available. Further discussions are also needed to take into account changes in a man’s health, values, and preferences.
Recommended general guidelines to PSA Testing
- An initial PSA test at 40 to 45 years of age is recommended because it is highly predictive of future prostate cancer risk.
- Some experts recommend routine PSA screenings only in reasonably healthy men from 45 to 75 years of age who wish it after a frank discussion of the benefits, limitations and potential risks of screening.
- Some experts do not recommend screening in patients who would not accept treatment even if cancer were found.
- Some doctors do not recommend routine screening in healthy men over age 75 with normal PSA levels up to that point, as they are not likely to benefit from treatment.
- Some doctors encourage screening only in men who are reasonably expected to have at least a 10-year life expectancy from the time of diagnosis. For most newly discovered localized prostate cancers, the survival benefit from treatment does not begin until at least 10 years after therapy.
- Some doctors encourage screening in men at high risk due to ethnicity or family history.
- Some doctors recommend PSA testing in men with an abnormal digital rectal examination suggestive of cancer regardless of age.
- Finally, regardless of the above, some doctors recommend doing PSA testing in all men who request it as long as they are fully aware of the risks, benefits, and limitations of screening, even if they fall outside the usual guidelines.
Prostate Cancer Screening Pros and Cons
Routine screening with a digital rectal exam and particularly a PSA test has become very controversial. Here are some of the arguments for and against 26, 27:
Against PSA Screenings
- No real change in overall survival for most patients for at least the first ten years after the initial diagnosis.
- Many patients (about three quarters) are getting biopsies which are negative or show only low-risk disease which is often overtreated.
- Screenings are only likely to catch relatively slow-growing tumors and will miss the rapidly growing, aggressive tumors that are the most lethal.
- Increased patient anxiety from low-risk, a low-grade prostate cancer that ultimately will not affect survival.
- “Unnecessary” biopsies contribute to patient anxiety, are uncomfortable, add cost and may have complications like infections and bleeding.
- Several recent large studies show little or no survival benefit to large-scale screenings.
- There is little point in doing prostate cancer screenings if treatment offers little or no survival benefit, as suggested by some recent studies (PIVOT).
- Foreign countries with good healthcare systems which do not perform widespread PSA testing have noted similar reductions in prostate cancer-specific survival compared to countries like the United States with extensive PSA screenings.
In Favor of PSA Screenings
- Prostate cancer is still the second leading cause of cancer death in men, and the incidence is increasing.
- Ignoring the best diagnostic screening test for prostate cancer is not going to reduce its mortality.
- Doctors now have active surveillance, MRI imaging, and MRI-TRUS fusion biopsies as well as genomic testing so that they can avoid overtreating patients.
- Eliminating routine PSA screenings, as recommended by the earlier USPSTF report of 2012, has already caused a significant reduction of about 30% in prostate cancer diagnosis. At least some of these cancers will ultimately be high-grade and will undoubtedly increase prostate cancer mortality.
- Many of the larger studies suggesting a lack of survival benefit to large scale PSA screenings have been shown to be poorly done, significantly biased, severely contaminated, and full of major statistical errors.
- Well done studies comparing PSA screened and unscreened populations, clearly show a cancer-specific survival advantage that is consistently at or above 50% for the screened groups if followed for more than 10 years.
- According to the National Institute of Health, prostate cancer mortality has dropped over 44% since 1992 when PSA testing became widely available in the United States. This is almost double the benefit in foreign countries that do not perform extensive PSA testing.
- The prostate cancer death rate in Sweden, where PSA testing is minimal, is higher than for lung cancer and more than double the mortality rate for prostate cancer in the United States.
- Long-term studies from Scandinavia and elsewhere prove that definitive treatment works, but it may take more than 10 to 15 years to become evident.
- It has been estimated by the National Institute of Health that in 10 years, an additional 25,000 to 30,000 men could die each year from preventable, potentially curable prostate cancer if doctors completely stopped all PSA screenings.
- Only 9% of all new prostate cancer cases present with advanced disease, compared with 32% before the PSA era. This represents a 72% reduction!
- Less than 4% of all new cases initially present with metastatic disease compared to 21% before widespread PSA screenings. This is an 80% reduction in the incidence of metastatic prostate cancer at the time of initial diagnosis that can only be explained by the benefits of PSA screenings.
- Researchers are constantly improving diagnostic testing and treatment options to lower costs and minimize side effects while increasing survival and improving quality of life; but without early PSA screening, these new minimally invasive technologies cannot be used.
If screening test results aren’t normal
If you are screened for prostate cancer and your initial blood PSA level is higher than normal, it doesn’t always mean that you have prostate cancer. Many men with higher than normal PSA levels do not have cancer. Still, further testing will be needed to help find out what is going on. Your doctor may advise one of these options:
- Waiting a while and having a second PSA test
- Getting another type of test to get a better idea of if you might have cancer (and therefore should get a prostate biopsy)
- Getting a prostate biopsy to find out if you have cancer
It’s important to discuss your options, including their possible pros and cons, with your doctor to help you choose one you are comfortable with. Factors that might affect which option is best for you include:
- Your age and overall health
- The likelihood that you have prostate cancer (based on tests done so far)
- Your own comfort level with waiting or getting further tests
If your initial PSA test was ordered by your primary care provider, you may be referred to a urologist (a doctor who treats cancers of the genital and urinary tract, which includes the prostate gland) for this discussion or for further testing.
Repeating the PSA test
A man’s blood PSA level can vary over time (for a number of reasons), so some doctors recommend repeating the test after a month or so if the initial PSA result is abnormal. This is most likely to be a reasonable option if the PSA level is on the lower end of the borderline range (typically 4 to 7 ng/mL). For higher PSA levels, doctors are more likely to recommend getting other tests, or going straight to a prostate biopsy.
Getting other tests
If the initial PSA result is abnormal, another option might be to get another type of test (or tests) to help you and your doctor get a better idea if you might have prostate cancer (and therefore need a biopsy). Some of the tests that might be done include:
- A digital rectal exam (DRE), if it hasn’t been done already
- One or more of the other special types of PSA tests discussed above, such as the Prostate Health Index (PHI), 4Kscore test, or percent-free PSA, or other lab tests, such as the ExoDx Prostate (IntelliScore).
- An imaging test of the prostate gland, such as MRI (especially multiparametric MRI) or transrectal ultrasound (TRUS).
If the initial abnormal test was a digital rectal exam (DRE), the next step is typically to get a PSA blood test and possibly other tests, such as a transrectal ultrasound (TRUS).
Getting a prostate biopsy
For some men, getting a prostate biopsy might be the best option, especially if the initial PSA level is high. A biopsy is a procedure in which small samples of the prostate are removed and then looked at under a microscope. This test is the only way to know for sure if a man has prostate cancer. If prostate cancer is found on a biopsy, this test can also help tell how likely it is that the cancer will grow and spread quickly.
Prostate cancer complications
Complications of prostate cancer and its treatments include:
- Cancer that spreads (metastasizes). Prostate cancer can spread to nearby organs, such as your bladder, or travel through your bloodstream or lymphatic system to your bones or other organs. Prostate cancer that spreads to the bones can cause pain and broken bones. Once prostate cancer has spread to other areas of the body, it may still respond to treatment and may be controlled, but it’s unlikely to be cured.
- Urinary incontinence. Both prostate cancer and its treatment can cause urinary incontinence. Treatment for incontinence depends on the type you have, how severe it is and the likelihood it will improve over time. Treatment options may include medications, catheters and surgery.
- Erectile dysfunction. Erectile dysfunction can result from prostate cancer or its treatment, including surgery, radiation or hormone treatments. Medications, vacuum devices that assist in achieving erection and surgery are available to treat erectile dysfunction.
Prostate cancer diagnosis
Most prostate cancers are first found during screening with a prostate-specific antigen (PSA) blood test or a digital rectal exam. Early prostate cancers usually don’t cause symptoms, but more advanced cancers are sometimes first found because of symptoms they cause.
If cancer is suspected based on results of screening tests or symptoms, tests will be needed to confirm the diagnosis. The actual diagnosis of prostate cancer can only be made with a prostate biopsy.
Medical history and physical exam
If your doctor suspects you might have prostate cancer, he or she will ask you about any symptoms you are having, such as any urinary or sexual problems, and how long you have had them. You might also be asked about possible risk factors, including your family history.
Your doctor will also examine you. This might include a digital rectal exam, during which the doctor’s gloved, lubricated finger is inserted into your rectum to feel for any bumps or hard areas on the prostate that might be cancer. If you do have cancer, the digital rectal exam can sometimes help tell if it’s only on one side of the prostate, if it’s on both sides, or if it’s likely to have spread beyond the prostate to nearby tissues.
Your doctor may also examine other areas of your body. He or she might then order some tests.
PSA blood test
The prostate-specific antigen (PSA) blood test is used mainly to screen for prostate cancer in men without symptoms. It’s also one of the first tests done in men who have symptoms that might be caused by prostate cancer.
PSA in the blood is measured in units called nanograms per milliliter (ng/mL). The chance of having prostate cancer goes up as the PSA level goes up, but there is no set cutoff point that can tell for sure if a man does or doesn’t have prostate cancer. Many doctors use a PSA cutoff point of 4 ng/mL or higher when deciding if a man might need further testing, while others might recommend it starting at a lower level, such as 2.5 or 3 ng/mL 28. Other factors, such as your age, race, and family history, may affect this decision.
Still, a level below 4 is not a guarantee that a man doesn’t have cancer. About 15% of men with a PSA below 4 ng/mL will have prostate cancer on a biopsy 29.
Men with a PSA level between 4 and 10 ng/mL (often called the “borderline range”) have about a 1 in 4 chance of having prostate cancer 28. If the PSA is more than 10 ng/mL, the chance of having prostate cancer is over 50% 28.
The PSA test can also be useful if you have already been diagnosed with prostate cancer.
- In men just diagnosed with prostate cancer, the PSA test can be used together with physical exam results and tumor grade (determined on the biopsy, described further on) to help decide if other tests (such as CT scans or bone scans) are needed.
- The PSA test is a part of staging (determining the stage of your cancer) and can help tell if your cancer is likely to still be confined to the prostate gland. If your PSA level is very high, your cancer is more likely to have spread beyond the prostate. This may affect your treatment options, since some forms of therapy (such as surgery and radiation) are not likely to be helpful if the cancer has spread to the lymph nodes, bones, or other organs.
- PSA tests are also an important part of monitoring prostate cancer during and after treatment.
Transrectal ultrasound (TRUS)
For this test, a small probe about the width of a finger is lubricated and placed in your rectum. The probe gives off sound waves that enter the prostate and create echoes. The probe picks up the echoes, and a computer turns them into a black and white image of the prostate.
The procedure often takes less than 10 minutes and is done in a doctor’s office or outpatient clinic. You will feel some pressure when the probe is inserted, but it is usually not painful. The area may be numbed before the procedure.
Transrectal ultrasound is often used to look at the prostate when a man has a high PSA level or has an abnormal digital rectal exam result. It is also used during a prostate biopsy to guide the needles into the correct area of the prostate.
Transrectal ultrasound is useful in other situations as well. It can be used to measure the size of the prostate gland, which can help determine the PSA density and may also affect which treatment options a man has. Transrectal ultrasound is also used as a guide during some forms of treatment such as brachytherapy (internal radiation therapy) or cryotherapy.
Prostate biopsy
If certain symptoms or the results of tests such as a PSA blood test or digital rectal exam suggest that you might have prostate cancer, your doctor will do a prostate biopsy.
A biopsy is a procedure in which small samples of the prostate are removed and then looked at under a microscope. A core needle biopsy is the main method used to diagnose prostate cancer. It is usually done by a urologist, a surgeon who treats cancers of the genital and urinary tract, which includes the prostate gland.
Using transrectal ultrasound to “see” the prostate gland, the doctor quickly inserts a thin, hollow needle through the wall of the rectum and into the prostate (a transrectal biopsy) or through the skin between the scrotum and anus (a transperineal biopsy). When the needle is pulled out it removes a small cylinder (core) of prostate tissue. This is repeated several times. Most urologists will take about 12 core samples from different parts of the prostate.
Though the procedure sounds painful, each biopsy usually causes only a brief uncomfortable sensation because it is done with a special spring-loaded biopsy instrument. The device inserts and removes the needle in a fraction of a second. Most doctors who do the biopsy will numb the area first by injecting a local anesthetic alongside the prostate. You might want to ask your doctor if he or she plans to do this.
The biopsy itself takes about 10 minutes and is usually done in the doctor’s office. You will likely be given antibiotics to take before the biopsy and possibly for a day or 2 after to reduce the risk of infection.
For a few days after the procedure, you may feel some soreness in the area and will probably notice blood in your urine. You may also have some light bleeding from your rectum, especially if you have hemorrhoids. Many men notice blood in their semen or have rust colored semen, which can last for several weeks after the biopsy, depending on how often you ejaculate.
Your biopsy samples will be sent to a lab, where they will be looked at a microscope to see if they contain cancer cells. If cancer is seen, it will also be assigned a grade (see the next section). Getting the results (in the form of a pathology report) usually takes at least 1 to 3 days, but it can sometimes take longer.
Even when taking many samples, biopsies can still sometimes miss a cancer if none of the biopsy needles pass through it. This is known as a false-negative result. If your doctor still strongly suspects you have prostate cancer (because your PSA level is very high, for example) a repeat biopsy might be needed to help be sure or your doctor might suggest:
- Getting other lab tests (of blood, urine, or the prostate biopsy samples) to help get a better idea of whether or not you might have prostate cancer. Examples of such tests include the Prostate Health Index (PHI), 4Kscore test, PCA3 tests (such as Progensa), and ConfirmMDx.
- Getting a repeat prostate biopsy. This might include getting additional samples of parts of the prostate not biopsied the first time, or using imaging tests such as MRI (described below) to look more closely for abnormal areas to target.
If the prostate biopsy results are negative (that is, if they don’t show cancer), and the chance that you have prostate cancer isn’t very high based on your PSA level and other tests, you might not need any more tests, other than repeat PSA tests (and possibly digital rectal exams) sometime later.
Imaging tests to look for prostate cancer spread
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body.
If you are found to have prostate cancer, your doctor will use your digital rectal exam results, prostate-specific antigen (PSA) level, and Gleason score from the biopsy results to figure out how likely it is that the cancer has spread outside your prostate. This information is used to decide if any imaging tests need to be done to look for possible cancer spread. Men with a normal digital rectal exam result, a low PSA, and a low Gleason score may not need any other tests because the chance that the cancer has spread is so low.
The imaging tests used most often to look for prostate cancer spread include:
Bone scan
If prostate cancer spreads to distant sites, it often goes to the bones first. A bone scan can help show whether cancer has reached the bones.
For this test, you are injected with a small amount of low-level radioactive material, which settles in damaged areas of bone throughout the body. A special camera detects the radioactivity and creates a picture of your skeleton.
A bone scan may suggest cancer in the bone, but to make an accurate diagnosis, other tests such as plain x-rays, CT or MRI scans, or even a bone biopsy might be needed.
Positron emission tomography (PET) scan
A PET scan is similar to a bone scan, in that a slightly radioactive substance (known as a tracer) is injected into the blood, which can then be detected with a special camera. But PET scans use different tracers that collect mainly in cancer cells. The most common tracer for standard PET scans is FDG, which is a type of sugar. Unfortunately, this type of PET scan isn’t very useful in finding prostate cancer cells in the body.
However, newer tracers, such as fluciclovine F18, sodium fluoride F18, and choline C11, have been found to be better at detecting prostate cancer cells.
Other newer tracers, such as Ga 68 PSMA-11, 18F-DCFPyl (also known as piflufolastat F 18 or Pylarify), and Ga 68 gozetotide (Locametz), attach to prostate-specific membrane antigen (PSMA), a protein that is often found in large amounts on prostate cancer cells. Tests using these types of tracers are sometimes referred to as PSMA PET scans.
These newer types of PET scans are most often used if it’s not clear if (or exactly where) prostate cancer has spread. For example, one of these tests might be done if the results of a bone scan aren’t clear, or if a man has a rising PSA level after initial treatment but it’s not clear where the cancer is in the body. PSMA PET scans can also be used to help determine if the cancer can be treated with a radiopharmaceutical that targets PSMA.
The pictures from a PET scan aren’t as detailed as MRI or CT scan images, but they can often show areas of cancer anywhere in the body. Some machines can do a PET scan and either an MRI (PET-MRI) or a CT scan (PET-CT) at the same time, which can give more detail about areas that show up on the PET scan.
Doctors are still learning about the best ways to use these newer types of PET scans, and some of them might not be available yet in all imaging centers.
Computed tomography (CT) scan
A CT scan uses x-rays to make detailed, cross-sectional images of your body. This test isn’t often needed for newly diagnosed prostate cancer if the cancer is likely to be confined to the prostate based on other findings (DRE result, PSA level, and Gleason score). Still, it can sometimes help tell if prostate cancer has spread into nearby lymph nodes. If your prostate cancer has come back after treatment, the CT scan can often tell if it is growing into other organs or structures in your pelvis.
CT scans are not as useful as magnetic resonance imaging (MRI) for looking at the prostate gland itself.
Magnetic resonance imaging (MRI)
Like CT scans, MRI scans show detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. A contrast material called gadolinium may be injected into a vein before the scan to better see details.
MRI scans can give a very clear picture of the prostate and show if the cancer has spread outside the prostate into the seminal vesicles or other nearby structures. This can be very important in determining your treatment options. But like CT scans, MRI scans aren’t usually needed for newly diagnosed prostate cancers that are likely to be confined to the prostate based on other factors.
MRI might be used in different situations:
- It can be used to help determine if a man with an abnormal screening test or with symptoms that might be from prostate cancer should get a prostate biopsy. (The type of MRI often used for this, known as multiparametric MRI, is described below.)
- If a prostate biopsy is planned, an MRI might be done to help locate and target areas of the prostate that are most likely to contain cancer. This is often done as an MRI/ultrasound fusion biopsy, which is described below.
- MRI can be used during a prostate biopsy to help guide the needles into the prostate.
- If prostate cancer has been found, MRI can be done to help determine the extent (stage) of the cancer. MRI scans can show if the cancer has spread outside the prostate into the seminal vesicles or other nearby structures. This can be very important in determining your treatment options. But MRI scans aren’t usually needed for newly diagnosed prostate cancers that are likely to be confined to the prostate based on other factors.
To improve the accuracy of the MRI, you might have a probe, called an endorectal coil, placed inside your rectum for the scan. This can be uncomfortable for some men. If needed, you can be given medicine to make you feel sleepy (sedation).
Multiparametric MRI: This newer MRI technique can be used to help better define possible areas of cancer in the prostate, as well as to get an idea of how quickly a cancer might grow. It can also help show if the cancer has grown outside the prostate or spread to other parts of the body. For this test, a standard MRI is done to look at the anatomy of the prostate, and then at least one other type of MRI (such as diffusion weighted imaging [DWI], dynamic contrast enhanced [DCE] MRI, or MR spectroscopy) is done to look at other parameters of the prostate tissue. The results of the different scans are then compared to help find abnormal areas. When this test is done to help determine if a man might have prostate cancer, the results are typically reported using the Prostate Imaging Reporting and Data System or PI-RADS. In this system, abnormal areas in the prostate are assigned a category on a scale ranging from PI-RADS 1 (very unlikely to be a clinically significant cancer) to PI-RADS 5 (very likely to be a clinically significant cancer).
MRI/ultrasound fusion-guided prostate biopsy: In this approach, a man gets an MRI scan a few days or weeks before the biopsy to look for abnormal areas in the prostate. During the biopsy itself, TRUS is used to view to prostate, and a special computer program is used to fuse the MRI and transrectal ultrasound (TRUS) images on a computer screen. This can help ensure the doctor gets biopsy samples from any suspicious areas seen on the images.
Lymph node biopsy
In a lymph node biopsy, also known as lymph node dissection or lymphadenectomy, one or more lymph nodes are removed to see if they have cancer cells. This isn’t done very often for prostate cancer, but can be used to find out if the cancer has spread from the prostate to nearby lymph nodes.
Biopsy during surgery to treat prostate cancer
The surgeon may remove lymph nodes in the pelvis during the same operation as the removal of the prostate, which is known as a radical prostatectomy.
If there is more than a very small chance that the cancer might have spread (based on factors such as a high PSA level or a high Gleason score), the surgeon may remove some lymph nodes before removing the prostate gland.
Sometimes the nodes will be looked at right away, while you are still under anesthesia, to help the surgeon decide whether to continue with the radical prostatectomy. This is called a frozen section exam because the tissue sample is frozen before thin slices are taken to check under a microscope. If the nodes contain cancer cells, the operation might be stopped (leaving the prostate in place). This could happen if the surgeon feels that removing the prostate would be unlikely to cure the cancer, but would still probably result in serious complications or side effects.
More often (especially if the chance of cancer spread is low), a frozen section exam is not done. Instead the lymph nodes and the prostate are removed and are then sent to the lab to be looked at. The lab results are usually available several days after surgery.
Lymph node biopsy as a separate procedure
A lymph node biopsy is rarely done as a separate procedure. It’s sometimes used when a radical prostatectomy isn’t planned (such as for some men who choose treatment with radiation therapy), but when it’s still important to know if the lymph nodes contain cancer.
Laparoscopic biopsy: A laparoscope is a long, slender tube with a small video camera on the end that is inserted into the abdomen through a small cut. It lets the surgeon see inside the abdomen and pelvis without needing to make a large cut (incision). Other small incisions are made to insert long instruments to remove the lymph nodes around the prostate gland, which are then sent to the lab.
Because there are no large incisions, most people recover fully in only 1 or 2 days, and the operation leaves very small scars.
Fine needle aspiration (FNA): If your lymph nodes appear enlarged on an imaging test (such as a CT or MRI scan) a doctor may take a sample of cells from an enlarged node by using a technique called fine needle aspiration.
To do this, the doctor uses a CT scan image to guide a long, hollow needle through the skin in the lower abdomen and into the enlarged node. The skin is numbed with local anesthesia before inserting the needle. A syringe attached to the needle lets the doctor take a small tissue sample from the node, which is then sent to the lab to look for cancer cells.
You will be able to return home a few hours after the procedure.
Genetic testing for some men with prostate cancer
Some doctors now recommend that some men with prostate cancer be tested to look for certain inherited gene changes. This includes men in whom a family cancer syndrome (such as a BRCA gene mutation or Lynch syndrome) is suspected, as well as men with prostate cancer that has certain high-risk features or that has spread to other parts of the body. Talk to your doctor about the possible pros, cons, and limitations of such testing.
Some types of lab tests, known as genomic, molecular, or proteomic tests, can be used along with other information (such as the risk groups described below) to help better predict how quickly a prostate cancer might grow or spread, and as a result, help decide what treatment options might be best and when they should be given. These tests look at which genes or proteins are active inside the prostate cancer cells. Examples of such tests include:
- Oncotype DX Prostate: This test measures the activity of certain genes in prostate cancer cells taken from biopsy tissue and reports it as a score on a scale from 0 to 100 (higher scores indicate a cancer that is more likely to grow and spread quickly, as well as a higher risk of dying from prostate cancer).
- Prolaris: This test measures the activity of a different set of genes in prostate cancer cells taken from biopsy tissue and reports it as a score on a scale from 0 to 10 (higher scores indicate a cancer that is more likely to grow and spread quickly, as well as a higher risk of dying from prostate cancer).
- ProMark: This test measures the activity of a set of proteins in prostate cancer cells taken from biopsy tissue and reports it as a score that helps predict how likely a cancer is to grow and spread quickly.
- Decipher: For men who choose surgery to treat their cancer, this test measures the activity of certain genes in prostate cancer cells from the surgery tissue. This test can help determine the risk that the cancer will come back in other parts of the body after surgery, and as a result, if these men should consider additional treatment.
These tests continue to be studied to find more areas where they can be useful in prostate cancer risk and treatment decisions.
Grade (Gleason score) of prostate cancer
The Gleason score is the most common system doctors use to grade prostate cancer. The Gleason system assigns a Gleason grade based on how much the cancer looks like normal prostate cells. This gives your doctor an idea of how the cancer might behave and what treatment you need.
To find out the Gleason score or Grade Group, a pathologist looks at several samples of cells (biopsies) from your prostate.
The pathologist grades each sample of prostate cancer cells from 3 to 5 based on how quickly they are likely to grow or how aggressive the cells look (grades 1 and 2 are not often used). You may hear this score being called the Gleason Grade.
Doctors then work out an overall Gleason score (also called the Gleason sum) by adding together the 2 most common Gleason grades. So for example, if the most common Gleason grade is 3, and the second most common is 4, then the overall Gleason score is 7. Or they might write the scores separately as 3 + 4 = 7. This combined score is also now called the Grade Group.
Although most often the Gleason score is based on the 2 areas that make up most of the prostate cancer, there are some exceptions when a biopsy sample has either a lot of high-grade cancer or there are 3 grades including high-grade cancer. In these cases, the way the Gleason score is determined is modified to reflect the aggressive (fast-growing) nature of the cancer.
In theory, the Gleason score can be between 2 and 10, but scores below 6 are rarely used.
Based on the Gleason score, prostate cancers are often divided into 3 groups:
- Cancers with a Gleason score of 6 or less may be called well-differentiated or low-grade prostate cancer.
- Cancers with a Gleason score of 7 may be called moderately-differentiated or intermediate-grade prostate cancer.
- Cancers with Gleason scores of 8 to 10 may be called poorly-differentiated or high-grade prostate cancer.
In recent years, doctors have come to realize that the Gleason score might not always be the best way to describe the grade of the cancer, for a couple of reasons:
- Prostate cancer outcomes can be divided into more than just the 3 groups mentioned above. For example, men with a Gleason score 3+4=7 cancer tend to do better than those with a 4+3=7 cancer. And men with a Gleason score 8 cancer tend to do better than those with a Gleason score of 9 or 10.
- The scale of the Gleason score can be misleading for patients. For example, a man with a Gleason score 6 cancer might assume that his cancer is in the middle of the range of grades (which in theory go from 2 to 10), even though grade 6 cancers are actually the lowest grade seen in practice. This assumption might lead a man to think his cancer is more likely to grow and spread quickly than it really is, which might affect his decisions about treatment.
Because of this, doctors have developed 5 Grade Groups, ranging from 1 (most likely to grow and spread slowly [least aggressive]) to 5 (most likely to grow and spread quickly [most aggressive]). The Grade Groups will likely replace the Gleason score over time, but currently you might see either one (or both) on a biopsy pathology report.
This is how the Gleason score and Grade Groups match up and what it means:
Table 5. Gleason score and Grade Groups
| Gleason score | Grade Group | What it means |
|---|---|---|
| Gleason score 6 (or 3 + 3 = 6) | Grade Group 1 | The cells look similar to normal prostate cells. The cancer is likely to grow very slowly, if at all |
| Gleason score 7 (or 3 + 4 = 7) | Grade Group 2 | Most cells still look similar to normal prostate cells. The cancer is likely to grow slowly |
| Gleason score 7 (or 4 + 3 = 7) | Grade Group 3 | The cells look less like normal prostate cells. The cancer is likely to grow at a moderate rate |
| Gleason score 8 (or 4 + 4 = 8) | Grade Group 4 | Some cells look abnormal. The cancer might grow quickly or at a moderate rate |
| Gleason score 9 or 10 (or 4 + 5 = 9, 5 + 4 = 9 or 5 + 5 = 10) | Grade Group 5 | The cells look very abnormal. The cancer is likely to grow quickly |
Along with the grade of the cancer (if it is present), the pathology report often contains other information about the cancer, such as:
- The number of biopsy core samples that contain cancer (for example, “7 out of 12”)
- The percentage of cancer in each of the cores
- Whether the cancer is on one side (left or right) of the prostate or on both sides (bilateral)
Suspicious results
Sometimes when the prostate cells are seen, they don’t look like cancer, but they’re not quite normal, either. These results are often reported as suspicious.
Prostatic intraepithelial neoplasia (PIN): In prostatic intraepithelial neoplasia, there are changes in how the prostate cells look, but the abnormal cells don’t look like they’ve grown into other parts of the prostate (like cancer cells would). PIN is often divided into 2 groups:
- Low-grade PIN: the patterns of prostate cells appear almost normal
- High-grade PIN: the patterns of cells look more abnormal
Many men begin to develop low-grade prostatic intraepithelial neoplasia at an early age but don’t necessarily develop prostate cancer. The importance of low-grade prostatic intraepithelial neoplasia in relation to prostate cancer is still unclear. If low-grade prostatic intraepithelial neoplasia is reported on a prostate biopsy, the follow-up for patients is usually the same as if nothing abnormal was seen.
If high-grade prostatic intraepithelial neoplasia is found on a biopsy, there is about a 20% chance that cancer may already be present somewhere else in the prostate gland. This is why doctors often watch men with high-grade prostatic intraepithelial neoplasia carefully and may advise a repeat prostate biopsy, especially if the original biopsy did not take samples from all parts of the prostate.
Atypical small acinar proliferation: This is sometimes just called atypia. In atypical small acinar proliferation, the cells look like they might be cancerous when viewed under the microscope, but there are too few of them to be sure. If atypical small acinar proliferation is found, there’s a high chance that cancer is also present in the prostate, which is why many doctors recommend getting a repeat biopsy within a few months.
Proliferative inflammatory atrophy: In proliferative inflammatory atrophy, the prostate cells look smaller than normal, and there are signs of inflammation in the area. Proliferative inflammatory atrophy is not cancer, but researchers believe that proliferative inflammatory atrophy may sometimes lead to high-grade PIN or to prostate cancer directly.
Prostate cancer stages
Prostate cancer staging can be complex. If you have any questions about your stage, please ask your someone on your cancer care team to explain it to you in a way you understand.
The stage (extent) of a prostate cancer is one of the most important factors in choosing treatment options and predicting a man’s outlook for survival (prognosis).
Prostate cancer stage is based on:
- The prostate biopsy results (including the Gleason score and Grade Group)
- The blood PSA level at the time of diagnosis
- The results of any other exams or tests that were done to find out how far the cancer has spread
You might also be told about the TNM stage or you may see this on your pathology report. Another way doctors may describe your prostate cancer is as localized, locally advanced or advanced. In addition to the risk groups below, doctors are still learning about the best use of other types of tests and prognostic models to help decide the most effective treatment options for someone. If your doctor suggests using one of these ways to help determine your treatment options, have them explain what it can tell you, as well as how accurate it’s likely to be.
- Localized prostate cancer is cancer that is completely inside the prostate gland. It hasn’t spread outside of the prostate gland or to any other parts of the body. Doctors divide localized prostate cancer into 5 risk groups (very low risk, low risk, medium risk, high risk and very high risk) depending on how likely it is that the prostate cancer will grow quickly or spread.
- Your localized prostate cancer risk group depends on:
- the size of your tumor (T stage)
- how the cells look under the microscope (the grade) and the pattern of the cells in the prostate tissue (this is called your Gleason score)
- your prostate specific antigen (PSA) blood test
- Very-low-risk localized prostate cancer. Very-low-risk localized prostate cancers are small, not felt on exam, can only be found in a small area of the prostate, and have not grown outside the prostate (cT1c). They have a Grade Group of 1 (Gleason score of 6 or less) and low PSA levels (less than 10 ng/ml) and few other classification criteria. They usually grow very slowly and are unlikely to ever cause any symptoms or other health problems.
- Low risk localized prostate cancer. Low risk localized prostate cancers have not yet grown outside of the prostate and are unlikely to grow or spread for many years. Your cancer is low risk if you have all of the following:
- a T stage of cT1 to cT2a (slightly larger than very-low-risk cancers)
- Grade Group of 1 (Gleason score no higher than 6)
- a PSA level less than 10 ng/ml
- Medium (intermediate) risk localized prostate cancer. Medium (intermediate) risk localized prostate cancers can be felt on exam or can be seen on an imaging test and are unlikely to grow or spread for a few years. Your cancer is medium risk if you have one of the following:
- the cancer might be found in more than half of one side of the prostate (cT2b) or in both sides of the prostate (cT2c)
- a Grade Group of 2 or 3 (Gleason score of 7)
- a PSA level between 10 and 20 ng/ml
- Additional classification split the intermediate-risk prostate cancers into favorable and unfavorable categories.
- High risk localized prostate cancer. High risk localized prostate cancers might grow or spread within a few years. Localized prostate cancer is high risk if you have one of the following:
- the cancer have grown outside the prostate (cT3a)
- a Grade Group of 4 or 5 (Gleason score 8 to 10)
- a PSA level higher than 20 ng/ml
- High risk localized prostate cancer is also a locally advanced prostate cancer. This means that even if your cancer is contained within the prostate gland, your doctor might describe it as locally advanced.
- Very-high-risk localized prostate cancer. Very-high-risk localized prostate cancers have a very high risk for the tumor growing, coming back, or spreading to the nearby lymph nodes and have one or more of the following traits:
- The tumor has spread to the seminal vesicles (cT3b) or into other tissues next to the prostate (cT4)
- The biopsy tissue shows areas with a Gleason 5 pattern (Gleason score 9 or 10 or Grade Group 5)
- They have 2 or 3 of the features found in the high-risk group (see above)
- More than 4 biopsy pieces are Grade Group 4 or 5 (Gleason score 8 to 10)
- Your localized prostate cancer risk group depends on:
- Locally advanced prostate cancer means the cancer has broken through the capsule (covering) of the prostate gland. It may have spread into the:
- tissue around the prostate
- the tubes that carry semen (seminal vesicles)
- body organs nearby such as the back passage (rectum) or neck of the bladder
- lymph nodes close to the prostate gland
- Advanced prostate cancer also called metastatic prostate cancer, means the cancer has spread (metastasize) from the prostate to other parts of the body. Prostate cancer most commonly spreads to lymph nodes in other parts of the body or to the bones. It can also spread to other organs.
The risk group can help determine if any further tests should be done, as well as help guide initial treatment options. Cancers in lower risk groups have a smaller chance of growing and spreading compared to those in higher risk groups.
If you have prostate cancer that has not spread to nearby lymph nodes or to other parts of the body, you might want to ask your doctor what risk group your cancer falls into to understand your treatment choices.
TNM staging system
A staging system is a standard way for the cancer care team to describe how far a cancer has spread. The most widely used staging system for prostate cancer is the American Joint Committee on Cancer (AJCC) TNM system.
The TNM system for prostate cancer is based on 5 key pieces of information:
- The extent of the main (primary) tumor (T category)*
- Whether the cancer has spread to nearby lymph nodes (N category)
- Whether the cancer has spread (metastasized) to other parts of the body (M category)
- The PSA level at the time of diagnosis
- The Gleason score, based on the prostate biopsy (or surgery)
*There are 2 types of T categories for prostate cancer:
- The clinical T category (written as cT) is your doctor’s best estimate of the extent of your disease, based on the results of the physical exam (including a digital rectal exam) and prostate biopsy, and any imaging tests you have had.
- If you have surgery to remove your prostate, your doctors can also determine the pathologic T category (written as pT). The pathologic T category is likely to be more accurate than the clinical T category, as it is done after all of your prostate has been examined in the lab.
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once the T, N, and M categories have been determined, this information is combined (along with the Grade Group and PSA level if they are available) in a process called stage grouping to get the overall stage of the cancer.
The main stages of prostate cancer range from I (1) through IV (4). Some stages are split further (A, B, etc). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
Prostate cancer stages
Footnotes: As prostate cancer progresses from Stage I (1) to Stage IV (4), the cancer cells grow within the prostate, through the outer layer of the prostate into nearby tissue, and then to lymph nodes or other parts of the body.
[Source 30 ]T categories (clinical)
There are 4 categories for describing the local extent of a prostate tumor, ranging from T1 to T4. Most of these have subcategories as well.
- T1: Your doctor can’t feel the tumor or see it with imaging such transrectal ultrasound.
- T1a: Cancer is found incidentally (by accident) during a transurethral resection of the prostate (TURP) that was done for benign prostatic hyperplasia (BPH), a non-cancerous growth of the prostate. Cancer is in no more than 5% of the tissue removed.
- T1b: Cancer is found during a TURP but is in more than 5% of the tissue removed.
- T1c: Cancer is found by needle biopsy that was done because of an increased PSA.
- T2: Your doctor can feel the cancer with a digital rectal exam (DRE) or see it with imaging such as transrectal ultrasound, but it still appears to be confined to the prostate.
- T2a: The cancer is in one half or less of only one side (left or right) of your prostate.
- T2b: The cancer is in more than half of only one side (left or right) of your prostate.
- T2c: The cancer is in both sides of your prostate.
- T3: The cancer has grown outside your prostate and may have grown into the seminal vesicles.
- T3a: The cancer extends outside the prostate but not to the seminal vesicles.
- T3b: The cancer has spread to the seminal vesicles.
- T4: The cancer has grown into tissues next to your prostate (other than the seminal vesicles), such as the urethral sphincter (a muscle that helps control urination), the rectum, the bladder, and/or the wall of the pelvis.
N categories
N categories describe whether the cancer has spread to nearby (regional) lymph nodes.
- NX: Nearby lymph nodes were not assessed.
- N0: The cancer has not spread to any nearby lymph nodes.
- N1: The cancer has spread to one or more nearby lymph nodes.
M categories
M categories describe whether the cancer has spread to distant parts of the body. The most common sites of prostate cancer spread are to the bones and to distant lymph nodes, although it can also spread to other organs, such as the lungs and liver.
- M0: The cancer has not spread beyond nearby lymph nodes.
- M1: The cancer has spread beyond nearby lymph nodes.
- M1a: The cancer has spread to distant (outside of the pelvis) lymph nodes.
- M1b: The cancer has spread to the bones.
- M1c: The cancer has spread to other organs such as lungs, liver, or brain (with or without spread to the bones).
Stage grouping
Once the T, N, and M categories have been determined, this information is combined (along with the Gleason score and PSA level if they are available) to get the overall stage of the cancer. The stage is expressed in Roman numerals from I (the least advanced) to IV (the most advanced). The stage helps determine treatment options and a man’s outlook for survival (prognosis).
Table 6. Prostate cancer stages
| Stage | Stage grouping | Stage description |
|---|---|---|
| 1 | T1, N0, M0 Gleason score 6 or less PSA less than 10 | The doctor can’t feel the tumor or see it with an imaging test such as transrectal ultrasound (it was either found during a transurethral resection or was diagnosed by needle biopsy done for a high PSA) [T1]. The cancer is still within the prostate and has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The Gleason score is 6 or less and the PSA level is less than 10. |
| OR | ||
| T2a, N0, M0 Gleason score 6 or less PSA less than 10 | The tumor can be felt by digital rectal exam or seen with imaging such as transrectal ultrasound and is in one half or less of only one side (left or right) of the prostate [T2a]. The cancer is still within the prostate and has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The Gleason score is 6 or less and the PSA level is less than 10. | |
| 2A | T1, N0, M0 Gleason score of 7 PSA less than 20 | The doctor can’t feel the tumor or see it with imaging such as transrectal ultrasound (it was either found during a transurethral resection or was diagnosed by needle biopsy done for a high PSA level) [T1]. The cancer has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The tumor has a Gleason score of 7. The PSA level is less than 20. |
| OR | ||
| T1, N0, M0 Gleason score of 6 or less PSA at least 10 but less than 20 | The doctor can’t feel the tumor or see it with imaging such as transrectal ultrasound (it was either found during a transurethral resection or was diagnosed by needle biopsy done for a high PSA) [T1]. The cancer has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The tumor has a Gleason score of 6 or less. The PSA level is at least 10 but less than 20. | |
| OR | ||
| T2a or T2b, N0, M0 Gleason score of 7 or less PSA less than 20 | The tumor can be felt by digital rectal exam or seen with imaging such as transrectal ultrasound and is in only one side of the prostate [T2a or T2b]. The cancer has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. It has a Gleason score of 7 or less. The PSA level is less than 20. | |
| 2B | T2c, N0, M0 Any Gleason score Any PSA | The tumor can be felt by digital rectal exam or seen with imaging such as transrectal ultrasound and is in both sides of the prostate [T2c]. The cancer has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The tumor can have any Gleason score and the PSA can be any value. |
| OR | ||
| T1 or T2, N0, M0 Any Gleason score PSA of 20 or more | The cancer has not yet spread outside the prostate. It may (or may not) be felt by digital rectal exam or seen with imaging such as transrectal ultrasound [T1 or T2]. The cancer has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The tumor can have any Gleason score. The PSA level is at least 20. | |
| OR | ||
| T1 or T2, N0, M0 Gleason score of 8 or higher Any PSA | The cancer has not yet spread outside the prostate. It may (or may not) be felt by digital rectal exam or seen with imaging such as transrectal ultrasound [T1 or T2]. The cancer has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The Gleason score is 8 or higher. The PSA can be any value. | |
| 3 | T3, N0, M0 Any Gleason score Any PSA | The cancer has grown outside the prostate and may have spread to the seminal vesicles [T3], but it has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The tumor can have any Gleason score and the PSA can be any value. |
| 4 | T4, N0, M0 Any Gleason score Any PSA | The cancer has grown into tissues next to the prostate (other than the seminal vesicles), such as the urethral sphincter (muscle that helps control urination), rectum, bladder, and/or the wall of the pelvis [T4]. The cancer has not spread to nearby lymph nodes [N0] or elsewhere in the body [M0]. The tumor can have any Gleason score and the PSA can be any value. |
| OR | ||
| Any T, N1, M0 Any Gleason score Any PSA | The tumor may or may not be growing into tissues near the prostate [any T]. The cancer has spread to nearby lymph nodes [N1] but has not spread elsewhere in the body [M0]. The tumor can have any Gleason score and the PSA can be any value. | |
| OR | ||
| Any T, any N, M1 Any Gleason score Any PSA | The cancer may or may not be growing into tissues near the prostate [any T] and may or may not have spread to nearby lymph nodes [any N]. It has spread to other, more distant sites in the body [M1]. The tumor can have any Gleason score and the PSA can be any value. | |
Stage 1 prostate cancer
Footnote: Stage 1 prostate cancer. Cancer is found in the prostate only. The cancer is not felt during a digital rectal exam and is found by needle biopsy done for high prostate-specific antigen (PSA) level or in a sample of tissue removed during surgery for other reasons. The PSA level is less than 10 and the Grade Group is 1; OR the cancer is felt during a digital rectal exam and is found in one-half or less of one side of the prostate. The PSA level is less than 10 and the Grade Group is 1.
[Source 32 ]Stage 2A prostate cancer
Footnote: Stage 2A prostate cancer. Cancer is found in the prostate only. Cancer is found in one-half or less of one side of the prostate. The prostate-specific antigen (PSA) level is at least 10 but less than 20 and the Grade Group is 1; OR cancer is found in more than one-half of one side of the prostate or in both sides of the prostate. The PSA level is less than 20 and the Grade Group is 1.
[Source 33 ]Stage 2B prostate cancer
Footnote: Stage 2B prostate cancer. Cancer is found in the prostate only. Cancer is found in one or both sides of the prostate. The prostate-specific antigen level is less than 20 and the Grade Group is 2.
[Source 34 ]Stage 2C prostate cancer
Footnote: Stage 2C prostate cancer. Cancer is found in the prostate only. Cancer is found in one or both sides of the prostate. The prostate-specific antigen level is less than 20 and the Grade Group is 3 or 4.
[Source 35 ]Stage 3A prostate cancer
Footnote: Stage 3A prostate cancer. Cancer is found in the prostate only. Cancer is found in one or both sides of the prostate. The prostate-specific antigen level is at least 20 and the Grade Group is 1, 2, 3, or 4.
[Source 36 ]Stage 3B prostate cancer
Footnote: Stage 3B prostate cancer. Cancer has spread from the prostate to the seminal vesicles or to nearby tissue or organs, such as the rectum, bladder, or pelvic wall. The prostate-specific antigen can be any level and the Grade Group is 1, 2, 3, or 4.
[Source 37 ]Stage 3C prostate cancer
Footnote: Stage 3C prostate cancer. Cancer is found in one or both sides of the prostate and may have spread to the seminal vesicles or to nearby tissue or organs, such as the rectum, bladder, or pelvic wall. The prostate-specific antigen can be any level and the Grade Group is 5.
[Source 38 ]Stage 4A prostate cancer
Footnote: Stage 4A prostate cancer. Cancer is found in one or both sides of the prostate and may have spread to the seminal vesicles or to nearby tissue or organs, such as the rectum, bladder, or pelvic wall. Cancer has spread to nearby lymph nodes. The prostate-specific antigen can be any level and the Grade Group is 1, 2, 3, 4, or 5.
[Source 39 ]Stage 4B prostate cancer
Footnote: Stage 4B prostate cancer. Cancer has spread to other parts of the body, such as the bones or distant lymph nodes.
[Source 40 ]Prostate cancer prognosis
Survival rates tell you what percentage of people with the same type and stage of cancer are still alive a certain amount of time (usually 5 years) after they were diagnosed. They can’t tell you how long you will live, but they may help give you a better understanding of how likely it is that your treatment will be successful. Some men want to know the survival rates for their cancer, and some don’t. If you don’t want to know, you don’t have to.
What is a 5-year survival rate ?
Statistics on the outlook for a certain type and stage of cancer are often given as 5-year survival rates, but many people live longer – often much longer – than 5 years. The 5-year survival rate is the percentage of people who live at least 5 years after being diagnosed with cancer. For example, a 5-year survival rate of 90% means that an estimated 90 out of 100 people who have that cancer are still alive 5 years after being diagnosed. Keep in mind, however, that many of these people live much longer than 5 years after diagnosis.
Relative survival rates are a more accurate way to estimate the effect of cancer on survival. These rates compare men with prostate cancer to men in the overall population. For example, if the 5-year relative survival rate for a specific stage of prostate cancer is 90%, it means that men who have that cancer are, on average, about 90% as likely as men who don’t have that cancer to live for at least 5 years after being diagnosed.
But remember, all survival rates are estimates – your outlook can vary based on a number of factors specific to you.
Cancer survival rates don’t tell the whole story
Survival rates are often based on previous outcomes of large numbers of men who had the disease, but they can’t predict what will happen in any particular man’s case. There are a number of limitations to remember:
- The numbers below are among the most current available. But to get 5-year survival rates, doctors have to look at men who were treated at least 5 years ago. As treatments are improving over time, men who are now being diagnosed with prostate cancer may have a better outlook than these statistics show.
- These statistics are based on the stage of the cancer when it was first diagnosed. They don’t apply to cancers that later come back or spread.
- The outlook for men with prostate cancer varies by the stage (extent) of the cancer – in general, the survival rates are higher for men with earlier stage cancers. But many other factors can affect a man’s outlook, such as age and overall health, and how well the cancer responds to treatment. The outlook for each man is specific to his circumstances.
Your doctor can tell you how these numbers may apply to you, as he or she is familiar with your particular situation.
Survival rates for prostate cancer
According to the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) 2012–2018 data, when including all stages of prostate cancer 5:
- The 5-year relative survival rate is 96.8%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- While patients presenting with distant metastases have a 5-year overall survival rate of only 32.3%.
Keep in mind that just as 5-year survival rates are based on men diagnosed and first treated more than 5 years ago.
In patients who undergo treatment, the most important prognostic indicators are patient age and general health at the time of diagnosis, as well as the cancer stage, pre-therapy PSA level, and Gleason score 27. A poorer prognosis is associated with higher grade disease, more advanced stage, younger age, increased PSA levels and a shorter “PSA doubling time” 41.
Prostate cancer survival rates by stage
The National Cancer Institute maintains a large national database on survival statistics for different types of cancer, known as the SEER database. The SEER database does not group cancers by American Joint Committee TNM stages (stage 1, stage 2, stage 3, etc.). Instead it groups cancers into localized, regional, and distant stages 5.
- Local stage means that there is no sign that the cancer has spread outside of the prostate. This corresponds to American Joint Committee on Cancer stages I and II. About 4 out of 5 prostate cancers are found in this early stage. The relative 5-year survival rate for local stage prostate cancer is nearly 100%.
- Regional stage means the cancer has spread from the prostate to nearby structures or lymph nodes. This includes stage 3 cancers and the stage 4 cancers that haven’t spread to distant parts of the body, such as T4 tumors and cancers that have spread to nearby lymph nodes (N1). The relative 5-year survival rate for regional stage prostate cancer is nearly 100%.
- Distant stage includes the rest of the stage 4 cancers – cancers that have spread to distant lymph nodes, bones, or other organs such as the lungs or liver (M1). The relative 5-year survival rate for distant stage prostate cancer is about 32.3%.
Remember, these survival rates are only estimates – they can’t predict what will happen to any one man. We understand that these statistics can be confusing and may lead you to have more questions. Talk with your doctor to better understand your situation.
Prostate cancer Life Expectancy
There is no clear evidence that either radical prostate surgery or radiation therapy have a significant survival advantage over the other, so treatment selection has relatively little effect on life expectancy 42.
- Patients with localized, low-grade disease (Gleason 2 + 2 = 4 or less) are unlikely to die of prostate cancer within 15 years.
- After 15 years, untreated patients are more likely to die from prostate cancer than any other identifiable disease or disorder.
- Older men with low-grade disease have approximately a 20% overall survival at 15 years, due primarily to death from other unrelated causes.
- Men with high-grade disease (Gleason 4 + 4 = 8 or higher) typically experience higher prostate cancer mortality rates within 15 years of diagnosis.
Prostate cancer treatment
Your prostate cancer treatment options depend on several factors including how big the cancer is, how fast your cancer is growing and whether it has spread anywhere else in your body (also known as the stage), the type of prostate cancer, how abnormal the cells look under a microscope (the grade) and your general health and level of fitness as well as the potential benefits or side effects of the treatment. These are all things to think about when making decisions about treatment. A team of doctors and other professionals will discuss the best treatment and care for you.
The main treatments for prostate cancer are 43:
- Active surveillance or watchful waiting
- Surgery
- External radiotherapy
- Internal radiotherapy (brachytherapy)
- Hormone therapy
- High frequency ultrasound therapy (HIFU)
- Cryotherapy (cryosurgery)
- Chemotherapy in combination with other treatments
- Immunotherapy
- Targeted Therapy
- Symptom control treatment
- Vaccine treatment
- Bone-directed treatment
You have one or more of these treatments depending on the stage of your cancer.
Your doctors and nurses will tell you what your options are and help you make the decision about your treatment.
Making treatment decisions
It’s important to discuss all of your treatment options, including their goals and possible side effects, with your doctors to help make the decision that best fits your needs. Some important things to consider include:
- The stage and grade of your cancer
- Your age and expected life span
- Any other serious health conditions you have
- Your feelings (and your doctor’s opinion) about the need to treat the cancer right away
- The likelihood that treatment will cure your cancer (or help in some other way)
- Your feelings about the possible side effects from each treatment
You may feel that you must make a decision quickly, but it’s important to give yourself time to absorb the information you have just learned. It’s also very important to ask questions if there is anything you’re not sure about.
Watchful Waiting or Active Surveillance for Prostate Cancer
Because prostate cancer often grows very slowly, some men (especially those who are older or have other serious health problems) might never need treatment for their prostate cancer. Instead, their doctors may recommend approaches known as watchful waiting (observation) or active surveillance. Other terms sometimes used include observation or expectant management.
Some doctors use the terms active surveillance and watchful waiting to mean the same thing. For other doctors these terms mean something slightly different:
- Active surveillance is often used to mean monitoring the cancer closely. Usually this approach includes a doctor visit with a prostate-specific antigen (PSA) blood test about every 6 months and digital rectal exam about every 12 months. Prostate biopsies and imaging tests may be done every 1 to 3 years as well. If your test results change, your doctor would then talk to you about treatment options to try and cure the cancer.
- Watchful waiting (observation) is sometimes used to describe a less intensive type of follow-up that may mean fewer tests and relying more on changes in a man’s symptoms to decide if treatment is needed. This treatment is most often meant to control symptoms from the cancer, but not to cure it.
Not all doctors agree with these definitions or use them exactly this way. In fact, some doctors prefer to no longer use the term watchful waiting. They feel it implies that nothing is being done, when in fact a man is still being closely monitored.
No matter which term your doctor uses, it’s very important for you to understand exactly what he or she means when they refer to it.
Comparing watchful waiting or active surveillance with active treatment
A few large studies have compared observation (watchful waiting) (where men were treated only if they developed symptoms from their cancer) and surgery for early-stage prostate cancer, but the evidence from these studies has been mixed. Some have found that men who have surgery might live longer, while others have not found a difference in survival.
So far, a few studies have compared active surveillance to treatments such as surgery or radiation therapy. Men who undergo surgery or radiation do not appear to live longer than those that undergo active surveillance, but their cancer might stay away longer and spread less.
When might watchful waiting or active surveillance for prostate cancer be an option?
One of these approaches might be recommended if your cancer:
- Isn’t causing any symptoms
- Is expected to grow slowly (based on Gleason score)
- Is small
- Is just in the prostate
- Is associated with low PSA level (<10ng/ml)
These approaches are not likely to be a good option if you have a fast-growing cancer (for example, a high Gleason score) or if the cancer is likely to have spread outside the prostate (based on PSA levels). Men who are young and healthy are less likely to be offered active surveillance, out of concern that the cancer might become a problem over the next 20 or 30 years.
Watchful waiting and active surveillance are reasonable options for some men with slow-growing cancers because it is not known whether treating the cancer with surgery or radiation will actually help them live longer. These treatments have definite risks and side effects that may outweigh the possible benefits for some men. Some men are not comfortable with this approach, and are willing to accept the possible side effects of active treatments to try to remove or destroy the cancer.
In active surveillance, only men whose cancer is growing (and therefore have a more serious form of cancer) are treated. This lets men with less serious cancer avoid the side effects of a treatment that might not have helped them live longer. A possible downside of this approach is that it might give the cancer a chance to grow and spread. This might limit your treatment options, and could possibly affect the chances of the cancer being treated successfully.
Not all experts agree how often testing should be done during active surveillance. There is also debate about when is the best time to start treatment if things change.
Prostate cancer surgery
Surgery is a common choice to try to cure prostate cancer if it is not thought to have spread outside the prostate gland.
There are different types of surgery for prostate cancer.
You might have an operation to remove your prostate gland or radical prostatectomy to try to cure your cancer. In this operation, the surgeon removes the entire prostate gland plus some of the tissue around it, including the seminal vesicles. A radical prostatectomy can be done in different ways. This can be done during an open surgery or by using a robotic system (also called Da Vinci surgery).
If your prostate cancer is pressing on the tube that carries urine from the bladder (the urethra), your doctor might suggest that you have an operation to remove some of the prostate. This is called trans urethral resection of the prostate (TURP). It won’t cure your cancer but can help you pass urine more easily and make you feel better.
Your doctor might also suggest that you have an operation to remove your testicles and stop you from making the hormone testosterone. This is called orchidectomy and is a type of hormone therapy.
Open radical prostatectomy
In the more traditional approach to doing a prostatectomy, the surgeon operates through a single long skin incision (cut) to remove the prostate and nearby tissues. This type of surgery, sometimes referred to as an open approach, is now done less often than in the past.
There are 2 main ways to do this operation.
Radical retropubic prostatectomy
For this open operation, the surgeon makes an incision (cut) in your lower abdomen, from the belly button down to the pubic bone, as shown in the picture below. You will either be under general anesthesia (asleep) or be given spinal or epidural anesthesia (numbing the lower half of the body) along with sedation during the surgery.
If there is a reasonable chance the cancer might have spread to nearby lymph nodes (based on your PSA level, prostate biopsy results, and other factors), the surgeon may also remove some of these lymph nodes at this time (known as a pelvic lymph node dissection). The nodes are sent to the lab to see if they have cancer cells in them. If cancer cells are found in any of the nodes, the surgeon might not continue with the surgery. This is because it’s unlikely that the cancer can be cured with surgery, and removing the prostate could lead to serious side effects.
After the prostate is removed, while you are still under anesthesia, a catheter (thin, flexible tube) will be put in your penis to help drain your bladder. The catheter will usually stay in place for 1 to 2 weeks while you heal. You will be able to urinate on your own after the catheter is removed.
You will probably stay in the hospital for a few days after the surgery, and your activities will be limited for several weeks.
Radical perineal prostatectomy
In this open operation, the surgeon makes the cut (incision) in the skin between the anus and scrotum (the perineum), as shown in the picture above. This approach is used less often because it’s more likely to lead to erection problems and because the nearby lymph nodes can’t be removed. But it is often a shorter operation and might be an option if you aren’t concerned about erections and you don’t need lymph nodes removed. It also might be used if you have other medical conditions that make retropubic surgery difficult for you. It can be just as curative as the retropubic approach if done correctly. The perineal operation may result in less pain and an easier recovery than the retropubic prostatectomy.
After the surgery, while you are still under anesthesia, a catheter will be put in your penis to help drain your bladder. The catheter usually stays in place for 1 to 2 weeks while you are healing. You will be able to urinate on your own after the catheter is removed.
You will probably stay in the hospital for a few days after the surgery, and your activities will be limited for several weeks.
Laparoscopic radical prostatectomy
Laparoscopic approaches use several smaller incisions and special long surgical tools to remove the prostate. The surgeon either holds the tools directly, or uses a control panel to precisely move robotic arms that hold the tools. This approach to prostatectomy has become more common in recent years.
If you’re thinking about treatment with laparoscopic surgery, it’s important to understand what is known and what is not yet known about this approach. The most important factors are likely to be the skill and experience of your surgeon. If you decide that laparoscopic surgery is the right treatment for you, be sure to find a surgeon with a lot of experience.
Laparoscopic radical prostatectomy
For a laparoscopic radical prostatectomy (LRP), the surgeon inserts special long instruments through several small incisions in the abdominal wall to remove the prostate. One of the instruments has a small video camera on the end, which lets the surgeon see inside the body.
Laparoscopic prostatectomy has some advantages over open radical prostatectomy, including less blood loss and pain, shorter hospital stays (usually no more than a day), faster recovery times, and the catheter will need to remain in the bladder for less time.
The rates of major side effects from laparoscopic radical prostatectomy, such as erection problems and trouble holding urine (incontinence) seem to be about the same as for open prostatectomies. Recovery of bladder control may be delayed slightly with this approach.
Even though more long-term studies are needed to compare side effects and chances of recurrence between open prostatectomy and laparoscopic radical prostatectomy, success of either procedure seems to be determined mainly by the experience and skill of the surgeon.
Robotic-assisted laparoscopic radical prostatectomy
In this approach, also known as robotic prostatectomy, the laparoscopic surgery is done using a robotic interface called the da Vinci system. The surgeon sits at a control panel in the operating room and moves robotic arms to operate through several small incisions in the patient’s abdomen.
Robotic prostatectomy has advantages over the open approach in terms of less pain, blood loss, and recovery time. But in terms of the side effects men are most concerned about, such as urinary or erection problems, there doesn’t seem to be a difference between robotic prostatectomy and other approaches.
For the surgeon, the robotic system may provide more maneuverability and more precision when moving the instruments than standard laparoscopic radical prostatectomy. Still, the most important factor in the success of either type of laparoscopic surgery is the surgeon’s experience and skill.
Prostate surgery risks
The risks with any type of radical prostatectomy are much like those with any major surgery. Problems during or shortly after the operation can include:
- Reactions to anesthesia
- Bleeding from the surgery
- Blood clots in the legs or lungs
- Damage to nearby organs
- Infections at the surgery site.
Rarely, part of the intestine might be injured during surgery, which could lead to infections in the abdomen and might require more surgery to correct. Injuries to the intestines are more common with laparoscopic and robotic surgeries than with the open approach.
If lymph nodes are removed, a collection of lymph fluid (called a lymphocele) can form and may need to be drained.
In extremely rare cases, people die because of complications of this operation. Your risk depends, in part, on your overall health, your age, and the skill of your surgical team.
Prostate surgery side effects
The major possible side effects of radical prostatectomy are urinary incontinence (being unable to control urine) and erectile dysfunction (impotence; problems getting or keeping erections). These side effects can also occur with other forms of prostate cancer treatment.
Urinary incontinence: You may not be able to control your urine or have leakage or dribbling. There are different levels of incontinence. Being incontinent can affect you not only physically but emotionally and socially as well. There are 3 major types of incontinence:
Men with stress incontinence might leak urine when they cough, laugh, sneeze, or exercise. Stress incontinence is the most common type after prostate surgery. It’s usually caused by problems with the valve that keeps urine in the bladder (the bladder sphincter). Prostate cancer treatments can damage the muscles that form this valve or the nerves that keep the muscles working.
Men with overflow incontinence have trouble emptying their bladder. They take a long time to urinate and have a dribbling stream with little force. Overflow incontinence is usually caused by blockage or narrowing of the bladder outlet by scar tissue.
Men with urge incontinence have a sudden need to urinate. This happens when the bladder becomes too sensitive to stretching as it fills with urine.
Rarely after surgery, men lose all ability to control their urine. This is called continuous incontinence.
After surgery for prostate cancer, normal bladder control usually returns within several weeks or months. This recovery usually occurs slowly over time.
Doctors can’t predict for sure how any man will be affected after surgery. In general, older men tend to have more incontinence problems than younger men. Large cancer centers, where prostate surgery is done often and surgeons have a lot of experience, generally report fewer problems with incontinence.
Incontinence can be treated. Even if your incontinence can’t be corrected completely, it can still be helped.
Erectile dysfunction (impotence): This means you can’t get an erection sufficient for sexual penetration.
Erections are controlled by 2 tiny bundles of nerves that run on either side of the prostate. If you can have erections before surgery, the surgeon will try not to injure these nerves during the prostatectomy. This is known as a nerve-sparing approach. But if the cancer is growing into or very close to the nerves, the surgeon will need to remove them.
If both nerves are removed, you won’t be able to have spontaneous erections, but you might still be able to have erections using some of the aids described below. If the nerves on only one side are removed, you might still have erections, but the chance is lower than if neither were removed. If neither nerve bundle is removed you might have normal erections at some point after surgery.
Your ability to have an erection after surgery depends on your age, your ability to get an erection before the operation, and whether the nerves were cut. All men can expect some decrease in the ability to have an erection, but the younger you are, the more likely it is that you will keep this ability.
Surgeons who do many radical prostatectomies tend to report lower impotence rates than doctors who do the surgery less often. A wide range of impotency rates have been reported in the medical literature, but each man’s situation is different, so the best way to get an idea of your chances for recovering erections is to ask your doctor about his or her success rates and what the outcome is likely to be in your case.
If your ability to have erections does return after surgery, it often occurs slowly. In fact, it can take from a few months up to 2 years. During the first few months, you will probably not be able to have a spontaneous erection, so you may need to use medicines or other treatments.
Most doctors feel that regaining potency is helped along by trying to get an erection as soon as possible once the body has had a chance to heal (usually several weeks after the operation). Some doctors call this penile rehabilitation. Medicines (see below) may be helpful at this time. Be sure to talk to your doctor about your situation.
There are several options for treating erectile dysfunction:
- Phosphodiesterase-5 (PDE5) inhibitors such as sildenafil (Viagra), vardenafil (Levitra), and tadalafil (Cialis) are pills that can help with erections. These drugs won’t work if both nerves that control erections have been damaged or removed. Common side effects of these drugs are headache, flushing (skin becomes red and feels warm), upset stomach, light sensitivity, and runny or stuffy nose. Rarely, these drugs can cause vision problems, possibly even blindness. Some other drugs such as nitrates, which are drugs used to treat heart disease, can cause problems if you are taking a PDE5 inhibitor, so be sure your doctor knows what medicines you take.
- Alprostadil is a man-made version of prostaglandin E1, a substance naturally made in the body that can produce erections. It can be injected almost painlessly into the base of the penis 5 to 10 minutes before intercourse or placed into the tip of the penis as a suppository. You can even increase the dosage to prolong the erection. You might have side effects, such as pain, dizziness, and prolonged erection, but they are not usually serious.
- Vacuum devices are another option to create an erection. These mechanical pumps are placed over the penis. The air is sucked out of the pump, which draws blood into the penis to produce an erection. The erection is maintained after the pump is removed by a strong rubber band placed at the base of the penis. The band is removed after sex.
- Penile implants might restore your ability to have erections if other methods don’t help. An operation is needed to put them inside the penis. There are several types of penile implants, including those using silicone rods or inflatable devices.
Changes in orgasm: After surgery, the sensation of orgasm should still be pleasurable, but there is no ejaculation of semen – the orgasm is “dry.” This is because the glands that made most of the fluid for semen (the seminal vesicles and prostate) were removed during the prostatectomy, and the pathways used by sperm (the vas deferens) were cut. In some men, orgasm becomes less intense or goes away completely. Less often, men report pain with orgasm.
Loss of fertility: Radical prostatectomy cuts the vas deferens, which are the pathways between the testicles (where sperm are made) and the urethra (through which sperm leave the body). Your testicles will still make sperm, but they can’t leave the body as a part of the ejaculate. This means that a man can no longer father a child the natural way. Often, this is not an issue, as men with prostate cancer tend to be older. But if it is a concern for you, you might want to ask your doctor about “banking” your sperm before the operation. To learn more, see Fertility and Men With Cancer.
Lymphedema: This is a rare but possible complication of removing many of the lymph nodes around the prostate. Lymph nodes normally provide a way for fluid to return to the heart from all areas of the body. When nodes are removed, fluid can collect in the legs or genital region over time, causing swelling and pain. Lymphedema can usually be treated with physical therapy, although it may not go away completely. You can learn more on our lymphedema page.
Change in penis length: A possible effect of surgery is a small decrease in penis length. This is probably due to a shortening of the urethra when a portion of it is removed along with the prostate.
Inguinal hernia: A prostatectomy increases a man’s chances of developing an inguinal (groin) hernia in the future.
Transurethral resection of the prostate (TURP)
This operation is more often used to treat men with non-cancerous enlargement of the prostate called benign prostatic hyperplasia (BPH). But it is also sometimes used in men with advanced prostate cancer to help relieve symptoms, such as urination problems. (It is not used to try to cure the cancer.)
During this operation, the surgeon removes the inner part of the prostate gland that surrounds the urethra (the tube through which urine exits the bladder). The skin is not cut with this surgery. An instrument called a resectoscope is passed through the tip of the penis into the urethra to the level of the prostate. Once it is in place, either electricity is passed through a wire to heat it or a laser is used to cut or vaporize the tissue. Spinal anesthesia (which numbs the lower half of your body) or general anesthesia (where you are asleep) is used.
The operation usually takes about an hour. After surgery, a catheter (thin, flexible tube) is inserted through the penis and into the bladder. It remains in place for about a day to help urine drain while the prostate heals. You can usually leave the hospital after 1 to 2 days and return to normal activities in 1 to 2 weeks.
You will probably have some blood in your urine after surgery. Other possible side effects from TURP include infection and any risks that come with the type of anesthesia used.
Radiation Therapy for Prostate Cancer
Radiation therapy uses high-energy rays or particles to kill cancer cells.
Depending on the stage of the prostate cancer and other factors, radiation therapy might be used:
- As the first treatment for cancer that is still just in the prostate gland and is low grade. Cure rates for men with these types of cancers are about the same as those for men treated with radical prostatectomy.
- As part of the first treatment (along with hormone therapy) for cancers that have grown outside the prostate gland and into nearby tissues.
- If the cancer is not removed completely or comes back (recurs) in the area of the prostate after surgery.
- If the cancer is advanced, to help keep the cancer under control for as long as possible and to help prevent or relieve symptoms.
Types of radiation therapy
The main types of radiation therapy used for prostate cancer are:
- External beam radiation
- Brachytherapy (internal radiation)
- Radiopharmaceuticals (medicines containing radiation that are injected into the body)
External beam radiation therapy (EBRT)
In external beam radiation therapy (EBRT), beams of radiation are focused on the prostate gland from a machine outside the body. This type of radiation can be used to try to cure earlier stage cancers, or to help relieve symptoms such as bone pain if the cancer has spread to a specific area of bone.
You will usually go for treatment 5 days a week in an outpatient center for at least several weeks, depending on why the radiation is being given. Each treatment is much like getting an x-ray. The radiation is stronger than that used for an x-ray, but the procedure typically is painless. Each treatment lasts only a few minutes, although the setup time — getting you into place for treatment — takes longer.
Newer external beam radiation therapy techniques focus the radiation more precisely on the tumor. This lets doctors give higher doses of radiation to the tumor while reducing the radiation exposure to nearby healthy tissues.
Three-dimensional conformal radiation therapy (3D-CRT)
3D-CRT uses special computers to precisely map the location of your prostate. Radiation beams are then shaped and aimed at the prostate from several directions, which makes it less likely to damage surrounding normal tissues and organs.
Intensity modulated radiation therapy (IMRT)
Intensity modulated radiation therapy (IMRT), an advanced form of 3D-CRT therapy, is the most common type of external beam radiation therapy for prostate cancer. It uses a computer-driven machine that moves around the patient as it delivers radiation. Along with shaping the beams and aiming them at the prostate from several angles, the intensity (strength) of the beams can be adjusted to limit the doses of radiation reaching nearby normal tissues. This lets doctors deliver an even higher radiation dose to the cancer.
Some newer radiation machines have imaging scanners built into them. This advance, known as image guided radiation therapy (IGRT), lets the doctor take pictures of the prostate just before giving the radiation to make minor adjustments in aiming. This appears to help deliver the radiation even more precisely and results in fewer side effects.
A variation of intensity modulated radiation therapy is called volumetric modulated arc therapy (VMAT). It uses a machine that delivers radiation quickly as it rotates once around the body. This allows each treatment to be given over just a few minutes. Although this can be more convenient for the patient, it hasn’t yet been shown to be more effective than regular intensity modulated radiation therapy.
Stereotactic body radiation therapy (SBRT)
This technique uses advanced image guided techniques to deliver large doses of radiation to a precise area, such as the prostate. Because there are large doses of radiation in each dose, the entire course of treatment is given over just a few days.
Stereotactic body radiation therapy (SBRT) is often known by the names of the machines that deliver the radiation, such as Gamma Knife, X-Knife, CyberKnife, and Clinac.
The main advantage of stereotactic body radiation therapy (SBRT) over intensity modulated radiation therapy (IMRT) is that the treatment takes less time (days instead of weeks). The side effects, though, are not better. In fact, some research has shown that some side effects might actually be worse with stereotactic body radiation therapy than with intensity modulated radiation therapy (IMRT).
Proton beam radiation therapy
Proton beam therapy focuses beams of protons instead of x-rays on the cancer. Unlike x-rays, which release energy both before and after they hit their target, protons cause little damage to tissues they pass through and release their energy only after traveling a certain distance. This means that proton beam radiation can, in theory, deliver more radiation to the prostate while doing less damage to nearby normal tissues. Proton beam radiation can be aimed with techniques similar to 3D-CRT and IMRT.
Although in theory proton beam therapy might be more effective than using x-rays, so far studies have not shown if this is true. Right now, proton beam therapy is not widely available. The machines needed to make protons are very expensive, and they aren’t available in many centers in the United States. Proton beam radiation might not be covered by all insurance companies at this time.
Possible side effects of external beam radiation therapy (EBRT)
Some of the side effects from EBRT are the same as those from surgery, while others are different.
Bowel problems: Radiation can irritate the rectum and cause a condition called radiation proctitis. This can lead to diarrhea, sometimes with blood in the stool, and rectal leakage. Most of these problems go away over time, but in rare cases normal bowel function does not return. To help lessen bowel problems, you may be told to follow a special diet during radiation therapy to help limit bowel movement during treatment. Sometimes a balloon-like device is put in the rectum during each treatment to keep the bowel as still as possible while treatment is given.
Urinary problems: Radiation can irritate the bladder and lead to a condition called radiation cystitis. You might need to urinate more often, have a burning sensation while you urinate, and/or find blood in your urine. Urinary problems usually improve over time, but in some men they never go away.
Some men develop urinary incontinence after treatment, which means they can’t control their urine or have leakage or dribbling. As described in the surgery section, there are different levels and types of incontinence. Overall, this side effect occurs less often than after surgery. The risk is low at first, but it goes up each year for several years after treatment.
Rarely, the tube that carries urine from the bladder out of the body (the urethra) may become very narrow or even close off, which is known as a urethral stricture. This might require further treatment to open it up again.
Erection problems, including impotence: After a few years, the impotence rate after radiation is about the same as that after surgery. Problems with erections usually do not occur right after radiation therapy but slowly develop over time. This is different from surgery, where impotence occurs immediately and may get better over time.
As with surgery, the older you are, the more likely it is you will have problems with erections. Erection problems can often be helped by treatments such as those listed in the surgery section, including medicines.
Feeling tired: Radiation therapy can cause fatigue that might not go away until a few weeks or months after treatment stops.
Lymphedema: The lymph nodes normally provide a way for fluid to return to the heart from all areas of the body. If the lymph nodes around the prostate are damaged by radiation, fluid may collect in the legs or genital region over time, causing swelling and pain. Lymphedema can usually be treated with physical therapy, although it may not go away completely.
Brachytherapy (internal radiation therapy)
Brachytherapy also called seed implantation or interstitial radiation therapy uses small radioactive pellets, or “seeds,” each about the size of a grain of rice. These pellets are placed directly into your prostate.
- Brachytherapy alone is generally used only in men with early-stage prostate cancer that is relatively slow growing (low-grade).
- Brachytherapy combined with external radiation is sometimes an option for men who have a higher risk of the cancer growing outside the prostate.
The use of brachytherapy is also limited by some other factors. For men who have had a transurethral resection of the prostate (TURP) or for those who already have urinary problems, the risk of urinary side effects may be higher. Brachytherapy might not work as well in men with large prostate glands because it might not be possible to place the seeds into all of the correct locations. One way to get around this may be to get a few months of hormone therapy beforehand to shrink the prostate.
Imaging tests such as transrectal ultrasound, CT scans, or MRI are used to help guide the placement of the radioactive pellets. Special computer programs calculate the exact dose of radiation needed.
There are 2 types of prostate brachytherapy. Both are done in an operating room. You will get either spinal anesthesia (where the lower half of your body is numbed) or general anesthesia (where you are asleep), and you might need to stay in the hospital overnight.
Permanent (low dose rate, or LDR) brachytherapy
In this approach, pellets (seeds) of radioactive material (such as iodine-125 or palladium-103) are placed inside thin needles, which are inserted through the skin in the area between the scrotum and anus and into the prostate. The pellets are left in place as the needles are removed and give off low doses of radiation for weeks or months. Radiation from the seeds travels a very short distance, so the seeds can give off a large amount of radiation in a very small area. This limits the amount of damage to nearby healthy tissues.
Usually, around 100 seeds are placed, but this depends on the size of the prostate. Because the seeds are so small, they seldom cause discomfort, and are simply left in place after their radioactive material is used up.
You may also get external beam radiation along with brachytherapy, especially if there is a higher risk that your cancer has spread outside the prostate (for example, if you have a higher Gleason score).
Temporary (high dose rate, or HDR) brachytherapy
This technique is done less often. It leaves higher doses of radiation in place for a short time. Hollow needles are placed through the skin between the scrotum and anus and into the prostate. Soft nylon tubes (catheters) are placed in these needles. The needles are then removed but the catheters stay in place. Radioactive iridium-192 or cesium-137 is then placed in the catheters, usually for 5 to 15 minutes. Generally, about 1 to 4 brief treatments are given over 2 days, and the radioactive substance is removed each time. After the last treatment the catheters are removed. For about a week after treatment, you may have some pain or swelling in the area between your scrotum and rectum, and your urine may be reddish-brown.
These treatments are usually combined with external beam radiation given at a lower dose than if used by itself. The advantage of this approach is that most of the radiation is concentrated in the prostate itself, sparing nearby normal tissues.
Possible risks and side effects of brachytherapy
Radiation precautions: If you get permanent (LDR) brachytherapy, the seeds will give off small amounts of radiation for several weeks or months. Even though the radiation doesn’t travel far, your doctor may advise you to stay away from pregnant women and small children during this time. If you plan on traveling, you might want to get a doctor’s note regarding your treatment, as low levels of radiation can sometimes be picked up by detection systems at airports.
There’s also a small risk that some of the seeds might move (migrate). You may be asked to strain your urine for the first week or so to catch any seeds that might come out. You may be asked to take other precautions as well, such as wearing a condom during sex. Be sure to follow any instructions your doctor gives you. There have also been reports of the seeds moving through the bloodstream to other parts of the body, such as the lungs. As far as doctors can tell, this is uncommon and doesn’t seem to cause any ill effects.
These precautions aren’t needed after HDR brachytherapy, because the radiation doesn’t stay in the body after treatment.
Bowel problems: Brachytherapy can sometimes irritate the rectum and cause a condition called radiation proctitis. Bowel problems such as rectal pain, burning, and/or diarrhea (sometimes with bleeding) can occur, but serious long-term problems are uncommon.
Urinary problems: Severe urinary incontinence (trouble controlling urine) is not a common side effect. But some men have problems with frequent urination or other symptoms due to irritation of the urethra, the tube that drains urine from the bladder. This tends to be worse in the weeks after treatment and gets better over time. Rarely, the urethra may actually close off (known as a urethral stricture) and need to be opened with a catheter or surgery.
Erection problems: Some studies have found rates of erection problems to be lower after brachytherapy, but other studies have found that the rates were no lower than with external beam radiation or surgery. The younger you are and the better your sexual function before treatment, the more likely you will be to regain function after treatment.
Erection problems can often be helped by treatments such as those listed in the surgery section, including medicines.
Radiopharmaceuticals
Radiopharmaceuticals are drugs that contain radioactive elements. They are injected into a vein and travel through the blood to reach cancer cells that have spread to other parts of the body. These drugs then give off radiation that kills the cancer cells. The type of radiation they use travels only a short distance, which helps limit side effects. Unlike other types of radiation, these drugs can reach cancer anywhere in the body.
Radiopharmaceuticals that target prostate-specific membrane antigen (PSMA)
Prostate-specific membrane antigen (PSMA) is a protein that is often found in large amounts on prostate cancer cells. Lutetium Lu 177 vipivotide tetraxetan also known as 177Lu-PSMA-617 or Pluvicto is a radiopharmaceutical that attaches to PSMA, bringing radiation directly to the prostate cancer cells. This drug can be used to treat prostate cancer that has spread and that has already been treated with hormone therapy and chemotherapy. The cancer cells must also have the PSMA protein. Your doctor will order a PSMA PET scan before you get this drug to make sure the cancer cells have PSMA.
This drug is given as an injection or infusion into a vein (IV), typically once every 6 weeks for up to 6 doses.
Some of the more common side effects of this drug include:
- Feeling tired
- Dry mouth
- Nausea
- Loss of appetite
- Constipation
This drug can lower blood cell counts:
- A low red blood cell count can cause tiredness, weakness, pale skin, or shortness of breath.
- A low blood platelet count can lead to bleeding or bruising more easily than normal, or bleeding that is hard to stop.
- A low white blood cell count can lead to an increased risk of infections, which might show as a fever, chills, sore throat, or mouth sores.
This drug might damage the kidneys. Your doctor or nurse will likely advise you to drink plenty of fluids and to urinate often before and after getting this drug, to help protect the kidneys. Tell your doctor or nurse if you start to pass less urine than is normal for you.
This drug contains radiation that might stay in your body for several days after treatment, so your health care team will advise you on ways to protect yourself and others. You will likely be advised to drink plenty of fluids and to urinate often to help flush any excess drug from your body and help protect the bladder. You might also be advised to avoid close contact with other people, especially children and pregnant women, for at least a few days after each treatment.
Radiopharmaceuticals that target the bones
Some radiopharmaceuticals are designed to settle in the bones, where they can help treat prostate cancer that has spread there. Radiopharmaceuticals that treat prostate cancer spread to the bones include:
- Strontium-89 (Metastron)
- Samarium-153 (Quadramet)
- Radium-223 (Xofigo)
Cryotherapy for Prostate Cancer
Cryotherapy also called cryosurgery or cryoablation, is the use of very cold temperatures to freeze and kill prostate cancer cells. Despite it sometimes being called cryosurgery, it is not actually a type of surgery.
Cryotherapy is sometimes used if the cancer has come back after radiation therapy. It may be an option to treat men with low risk early-stage prostate cancer who cannot have surgery or radiation therapy. However, most doctors do not use cryotherapy as the first treatment for prostate cancer.
How is cryotherapy done?
Cryotherapy requires spinal or epidural anesthesia (the lower half of your body is numbed) or general anesthesia (you are asleep).
The doctor uses transrectal ultrasound (TRUS) to guide several hollow probes (needles) through the skin between the anus and scrotum and into the prostate. Very cold gases are then passed through the needles to freeze and destroy the prostate. To be sure the prostate is destroyed without too much damage to nearby tissues, the doctor carefully watches the ultrasound during the procedure. Warm saltwater is circulated through a catheter in the urethra during the procedure to keep it from freezing. The catheter is left in place for several weeks afterward to allow the bladder to empty while you recover.
After the procedure, you might need to stay in the hospital overnight, but many patients leave the same day.
Cryotherapy is less invasive than surgery, so there is usually less blood loss, a shorter hospital stay, shorter recovery period, and less pain. But compared with surgery or radiation therapy, doctors know much less about the long-term effectiveness of cryotherapy. And as with brachytherapy, this may not be a good option for men with large prostate glands.
Possible side effects of cryotherapy
Side effects from cryotherapy tend to be worse if it is done in men who have already had radiation therapy, compared to men who have it as the first form of treatment.
Most men have blood in their urine for a day or two after the procedure, as well as soreness in the area where the needles were placed. Swelling of the penis or scrotum is also common.
Freezing might also affect the bladder and rectum, which can lead to pain, burning sensations, and the need to empty the bladder and bowels often. Most men recover normal bowel and bladder function over time.
Freezing often damages the nerves near the prostate that control erections. Erectile dysfunction is more common after cryotherapy than after radical prostatectomy.
Urinary incontinence (having problems controlling urine) is rare in men who have cryotherapy as their first treatment for prostate cancer, but it is more common in men who have already had radiation therapy.
After cryotherapy, less than 1% of men develop a fistula (an abnormal connection) between the rectum and bladder. This rare but serious problem can allow urine to leak into the rectum and often requires surgery to repair.
Hormone Therapy for Prostate Cancer
Hormone therapy is also called androgen deprivation therapy (ADT) or androgen suppression therapy. The goal is to reduce levels of male hormones, called androgens, in the body, or to stop them from fueling prostate cancer cells.
Androgens stimulate prostate cancer cells to grow. The main androgens in the body are testosterone and dihydrotestosterone (DHT). Most androgens are made by the testicles, but the adrenal glands (glands that sit above your kidneys) as well as the prostate cancer itself, can also make a fair amount.
Lowering androgen levels or stopping them from getting into prostate cancer cells often makes prostate cancers shrink or grow more slowly for a time. But hormone therapy alone does not cure prostate cancer.
Hormone therapy may be used:
- If the cancer has spread too far to be cured by surgery or radiation, or if you can’t have these treatments for some other reason
- If the cancer remains or comes back after treatment with surgery or radiation therapy
- Along with radiation therapy as the initial treatment, if you are at higher risk of the cancer coming back after treatment (based on a high Gleason score, high PSA level, and/or growth of the cancer outside the prostate)
- Before radiation to try to shrink the cancer to make treatment more effective
Types of hormone therapy used to treat prostate cancer
Several types of hormone therapy can be used to treat prostate cancer.
Treatments to lower testicular androgen levels
Androgen deprivation therapy (ADT) uses surgery or medicines to lower the levels of androgens made in the testicles.
Orchiectomy (surgical castration)
Even though this is a type of surgery, its main effect is as a form of hormone therapy. In this operation, the surgeon removes the testicles, where most of the androgens (testosterone and DHT) are made. This causes most prostate cancers to stop growing or shrink for a time.
This is done as an outpatient procedure. It is probably the least expensive and simplest form of hormone therapy. But unlike some of the other treatments, it is permanent, and many men have trouble accepting the removal of their testicles.
Some men having this surgery are concerned about how it will look afterward. If wanted, artificial testicles that look much like normal ones can be inserted into the scrotum.
LHRH agonists
Luteinizing hormone-releasing hormone (LHRH) agonists also called LHRH analogs or GnRH agonists are drugs that lower the amount of testosterone made by the testicles. Treatment with these drugs is sometimes called chemical castration or medical castration because they lower androgen levels just as well as orchiectomy.
Even though LHRH agonists cost more than orchiectomy and require more frequent doctor visits, most men choose this method. With these drugs, the testicles remain in place, but they will shrink over time, and they may even become too small to feel.
LHRH agonists are injected or placed as small implants under the skin. Depending on the drug used, they are given anywhere from once a month up to once a year. The LHRH agonists available in the United States include:
- Leuprolide (Lupron, Eligard)
- Goserelin (Zoladex)
- Triptorelin (Trelstar)
- Leuprolide mesylate (Camcevi)
When LHRH agonists are first given, testosterone levels go up briefly before falling to very low levels. This effect is called tumor flare and results from the complex way in which these drugs work. Men whose cancer has spread to the bones may have bone pain. Men whose prostate gland has not been removed may have trouble urinating. If the cancer has spread to the spine, even a short-term increase in tumor growth as a result of the flare could press on the spinal cord and cause pain or paralysis. A flare can be avoided by giving drugs called anti-androgens (discussed below) for a few weeks when starting treatment with LHRH agonists.
LHRH antagonist
LHRH antagonists can be used to treat advanced prostate cancer. These drugs work in a slightly different way from the LHRH agonists, but they lower testosterone levels more quickly and don’t cause tumor flare like the LHRH agonists do. Treatment with these drugs can also be considered a form of medical castration.
- Degarelix (Firmagon) is given as a monthly injection under the skin. Some men may notice problems at the injection site (pain, redness, and swelling).
- Relugolix (Orgovyx) is taken as pills, once a day, so it might allow for less frequent office visits.
Treatments to lower testicular androgen levels side effects
Orchiectomy and LHRH agonists and antagonists can all cause similar side effects from lower levels of hormones such as testosterone. These side effects can include:
- Reduced or absent sexual desire
- Erectile dysfunction (impotence)
- Shrinkage of testicles and penis
- Hot flashes, which may get better or go away with time
- Breast tenderness and growth of breast tissue (gynecomastia)
- Osteoporosis (bone thinning), which can lead to broken bones
- Anemia (low red blood cell counts)
- Decreased mental sharpness
- Loss of muscle mass
- Weight gain
- Fatigue
- Increased cholesterol levels
- Depression
Some research has suggested that the risk of high blood pressure, diabetes, strokes, heart attacks, and even death from heart disease is higher in men treated with hormone therapy, although not all studies have found this.
Many side effects of hormone therapy can be prevented or treated. For example:
- Hot flashes can often be helped by treatment with certain antidepressants or other drugs.
- Brief radiation treatment to the breasts can help prevent their enlargement, but this is not effective once breast enlargement has occurred.
- Several drugs can help prevent and treat osteoporosis.
- Depression can be treated with antidepressants and/or counseling.
- Exercise can help reduce many side effects, including fatigue, weight gain, and the loss of bone and muscle mass.
There is growing concern that hormone therapy for prostate cancer may lead to problems thinking, concentrating, and/or with memory, but this has not been studied thoroughly. Still, hormone therapy does seem to lead to memory problems in some men. These problems are rarely severe, and most often affect only some types of memory. More studies are being done to look at this issue.
Treatment to lower androgen levels from the adrenal glands
LHRH agonists and antagonists can stop the testicles from making androgens, but cells in other parts of the body, such as the adrenal glands, and prostate cancer cells themselves, can still make male hormones, which can fuel cancer growth. Some drugs can block the formation of androgens made by these cells.
Abiraterone (Zytiga) blocks an enzyme (protein) called CYP17, which helps stop these cells from making androgens.
Abiraterone (Zytiga) can be used in men with advanced prostate cancer that is either:
- High risk (cancer with a high Gleason score, spread to several spots in the bones, or spread to other organs)
- Castrate-resistant (cancer that is still growing despite low testosterone levels from an LHRH agonist, LHRH antagonist, or orchiectomy)
Abiraterone (Zytiga) is taken as pills every day. It doesn’t stop the testicles from making testosterone, so men who haven’t had an orchiectomy need to continue treatment with an LHRH agonist or antagonist. Because abiraterone also lowers the level of some other hormones in the body, prednisone (a corticosteroid drug) needs to be taken during treatment as well to avoid certain side effects.
Ketoconazole (Nizoral), first used for treating fungal infections, also blocks production of androgens made in the adrenal glands, much like abiraterone. It’s most often used to treat men just diagnosed with advanced prostate cancer who have a lot of cancer in the body, as it offers a quick way to lower testosterone levels. It can also be tried if other forms of hormone therapy are no longer working.
Ketoconazole also can block the production of cortisol, an important steroid hormone in the body, so men treated with this drug often need to take a corticosteroid (such as prednisone or hydrocortisone).
Possible side effects: Abiraterone can cause joint or muscle pain, high blood pressure, fluid buildup in the body, hot flashes, upset stomach, and diarrhea. Ketoconazole can cause elevated liver blood tests, nausea, vomiting, gynecomastia (enlargement of breast tissue in men) and a skin rash.
Drugs that stop androgens from working
Anti-androgens
For most prostate cancer cells to grow, androgens have to attach to a protein in the prostate cancer cell called an androgen receptor. Anti-androgens are drugs that also connect to these receptors, keeping the androgens from causing tumor growth. Anti-androgens are also sometimes called androgen receptor antagonists.
Androgen receptor antagonists include:
- Flutamide (Eulexin)
- Bicalutamide (Casodex)
- Nilutamide (Nilandron)
They are taken daily as pills.
In the United States, anti-androgens are not often used by themselves:
- An anti-androgen may be added to treatment if orchiectomy or an LHRH agonist or antagonist is no longer working by itself.
- An anti-androgen is also sometimes given for a few weeks when an LHRH agonist is first started. This can help prevent a tumor flare.
- An anti-androgen can also be combined with orchiectomy or an LHRH agonist as first-line hormone therapy. This is called combined androgen blockade (CAB). There is still some debate as to whether combined androgen blockade (CAB) is more effective in this setting than using orchiectomy or an LHRH agonist alone. If there is a benefit, it appears to be small.
- In some men, if an anti-androgen is no longer working, simply stopping the anti-androgen can cause the cancer to stop growing for a short time. This is called the anti-androgen withdrawal effect, although it is not clear why it happens.
Possible side effects: Anti-androgens have similar side effects to LHRH agonists, LHRH antagonists, and orchiectomy, but they may have fewer sexual side effects. When these drugs are used alone, sexual desire and erections can often be maintained. When these drugs are given to men already being treated with LHRH agonists, diarrhea is the major side effect. Nausea, liver problems, and tiredness can also occur.
Newer anti-androgens
Enzalutamide (Xtandi), apalutamide (Erleada) and darolutamide (Nubeqa) are newer types of anti-androgens.
- All of these drugs can be helpful in men with cancer that has not spread but is no longer responding to other forms of hormone therapy known as non-metastatic castrate-resistant prostate cancer (CRPC).
- Enzalutamide can also be used for metastatic prostate cancer (cancer that has spread), whether it is castrate-resistant or castrate-sensitive (still responding to other forms of hormone therapy).
- Apalutamide can also be used for metastatic castrate-sensitive prostate cancer.
These drugs are taken as pills each day.
Side effects can include diarrhea, fatigue, rash, and worsening of hot flashes. These drugs can also cause some nervous system side effects, including dizziness and, rarely, seizures. Men taking one of these drugs are more likely to fall, which may lead to injuries. Some men have also had heart problems when taking these newer types of anti-androgens.
Other androgen-suppressing drugs
Estrogens (female hormones) were once the main alternative to removing the testicles (orchiectomy) for men with advanced prostate cancer. Because of their possible side effects (including blood clots and breast enlargement), estrogens have been replaced by other types of hormone therapy. Still, estrogens may be tried if other hormone treatments are no longer working.
Current issues in hormone therapy
There are many issues around hormone therapy that not all doctors agree on, such as the best time to start and stop it and the best way to give it. Studies are now looking at these issues. A few of them are discussed here.
- Treating early-stage cancer: Some doctors have used hormone therapy instead of observation or active surveillance in men with early-stage prostate cancer who do not want surgery or radiation. Studies have not found that these men live any longer than those who don’t get any treatment until the cancer progresses or symptoms develop. Because of this, hormone treatment is not usually advised for early-stage prostate cancer.
- Early versus delayed treatment: For men who need (or will eventually need) hormone therapy, such as men whose PSA levels are rising after surgery or radiation or men with advanced prostate cancer who don’t yet have symptoms, it’s not always clear when it is best to start hormone treatment. Some doctors think that hormone therapy works better if it’s started as soon as possible, even if a man feels well and is not having any symptoms. Some studies have shown that hormone treatment may slow the disease down and perhaps even help men live longer. But not all doctors agree with this approach. Some are waiting for more evidence of benefit. They feel that because of the side effects of hormone therapy and the chance that the cancer could become resistant to therapy sooner, treatment shouldn’t be started until a man has symptoms from the cancer. This issue is being studied.
- Intermittent versus continuous hormone therapy: Most prostate cancers treated with hormone therapy become resistant to this treatment over a period of months or years. Some doctors believe that constant androgen suppression might not be needed, so they advise intermittent (on-again, off-again) treatment. This can allow for a break from side effects like decreased energy, sexual problems, and hot flashes. In one form of intermittent hormone therapy, treatment is stopped once the PSA drops to a very low level. If the PSA level begins to rise, the drugs are started again. Another form of intermittent therapy uses hormone therapy for fixed periods of time – for example, 6 months on followed by 6 months off. At this time, it isn’t clear how this approach compares to continuous hormone therapy. Some studies have found that continuous therapy might help men live longer, but other studies have not found such a difference.
- Combined androgen blockade (CAB): Some doctors treat patients with androgen deprivation (orchiectomy or an LHRH agonist or antagonist) plus an anti-androgen. Some studies have suggested this may be more helpful than androgen deprivation alone, but others have not. Most doctors are not convinced there’s enough evidence that this combined therapy is better than starting with one drug alone when treating prostate cancer that has spread to other parts of the body.
- Triple androgen blockade (TAB): Some doctors have suggested taking combined therapy one step further, by adding a drug called a 5-alpha reductase inhibitor – either finasteride (Proscar) or dutasteride (Avodart) – to the combined androgen blockade. There is very little evidence to support the use of this triple androgen blockade at this time.
- Castrate-resistant versus hormone-refractory prostate cancer: These terms are sometimes used to describe how well a man’s prostate cancer is responding to hormone therapy.
- Castrate-sensitive prostate cancer means the cancer is being controlled by keeping the testosterone level as low as what would be expected if the testicles were removed (called the castrate level). Levels can be kept this low with an orchiectomy, or by taking an LHRH agonist or an LHRH antagonist.
- Castrate-resistant prostate cancer means the cancer is still growing even when the testosterone levels are at or below the castrate level. Some of these cancers might still be helped by other forms of hormone therapy, such as abiraterone or one of the newer anti-androgens.
- Hormone-refractory prostate cancer refers to prostate cancer that is no longer helped by any type of hormone therapy, including the newer medicines.
Chemotherapy for Prostate Cancer
Chemotherapy (chemo) uses anti-cancer drugs injected into a vein or given by mouth. These drugs enter the bloodstream and go throughout the body, making this treatment potentially useful for cancers that have spread (metastasized) to distant organs.
Chemo is sometimes used if prostate cancer has spread outside the prostate gland and hormone therapy isn’t working. Recent research has also shown that chemo might be helpful if given along with hormone therapy.
Chemo is not a standard treatment for early prostate cancer, but some studies are looking to see if it could be helpful if given for a short time after surgery.
Chemo drugs used to treat prostate cancer
For prostate cancer, chemo drugs are typically used one at a time. Some of the chemo drugs used to treat prostate cancer include:
- Docetaxel (Taxotere)
- Cabazitaxel (Jevtana)
- Mitoxantrone (Novantrone)
- Estramustine (Emcyt)
In most cases, the first chemo drug given is docetaxel, combined with the steroid drug prednisone. If this does not work (or stops working), cabazitaxel is often the next chemo drug tried (although there may be other treatment options as well).
Docetaxel and cabazitaxel have been shown to help men live longer, on average, than older chemo drugs. They may slow the cancer’s growth and also reduce symptoms, resulting in a better quality of life. Still, chemo is very unlikely to cure prostate cancer.
Other chemo drugs being studied for use in prostate cancer include carboplatin, oxaliplatin, and cisplatin.
Chemo drugs for prostate cancer are typically given into a vein (IV), either as an infusion over a certain period of time. This can be done in a doctor’s office, chemotherapy clinic, or in a hospital setting. Some drugs, such as estramustine, are given as a pill.
Often, a slightly larger and sturdier IV is required in the vein system to administer chemo. They are known as central venous catheters (CVCs), central venous access devices (CVADs), or central lines. They are used to put medicines, blood products, nutrients, or fluids right into your blood. They can also be used to take out blood for testing.
Many different kinds of CVCs are available. The most common types are the port and the PICC line.
Doctors give chemo in cycles, with each period of treatment followed by a rest period to give you time to recover from the effects of the drugs. Cycles are most often 2 or 3 weeks long. The schedule varies depending on the drugs used. For example, with some drugs, the chemo is given only on the first day of the cycle. With others, it is given for a few days in a row, or once a week. Then, at the end of the cycle, the chemo schedule repeats to start the next cycle.
The length of treatment for advanced prostate cancer is based on how well it is working and what side effects you have.
Possible side effects of chemotherapy
Chemo drugs attack cells that are dividing quickly, which is why they work against cancer cells. But other cells in the body, such as those in the bone marrow (where new blood cells are made), the lining of the mouth and intestines, and the hair follicles, also divide quickly. These cells can also be affected by chemo, which can lead to side effects.
The side effects of chemo depend on the type and dose of drugs given and how long they are taken. Some common side effects can include:
- Hair loss
- Mouth sores
- Loss of appetite
- Nausea and vomiting
- Diarrhea
- Increased chance of infections (from having too few white blood cells)
- Easy bruising or bleeding (from having too few blood platelets)
- Fatigue (from having too few red blood cells)
These side effects usually go away once treatment is finished. There are often ways to lessen these side effects. For example, drugs can be given to help prevent or reduce nausea and vomiting.
Along with the risks above, some side effects are seen more often with certain chemo drugs. For example:
- Docetaxel and cabazitaxel sometimes cause severe allergic reactions. Medicines are given before each treatment to help prevent this. These drugs can also damage nerves (known as peripheral neuropathy), which can cause numbness, tingling, or burning sensations in the hands or feet.
- Mitoxantrone can, very rarely, cause leukemia several years later.
- Estramustine carries an increased risk of blood clots.
If you notice any side effects while getting chemo report them to your cancer care team so that they can be treated promptly. In some cases, the doses of the chemo drugs may need to be reduced or treatment may need to be delayed or stopped to prevent the effects from getting worse.
Immunotherapy for Prostate Cancer
Immunotherapy is the use of medicines to stimulate a person’s own immune system to recognize and destroy cancer cells more effectively. Certain types of immunotherapy can be used to treat prostate cancer.
Cancer vaccine for prostate cancer
Sipuleucel-T (Provenge) is a cancer vaccine. Unlike traditional vaccines, which boost the body’s immune system to help prevent infections, this vaccine boosts the immune system to help it attack prostate cancer cells. The vaccine is used to treat advanced prostate cancer that’s no longer responding to hormone therapy but is causing few or no symptoms.
This vaccine is made specifically for each man. To make it, white blood cells (cells of the immune system) are removed from your blood over a few hours while you are hooked up to a special machine. The cells are then sent to a lab, where they are mixed with a protein from prostate cancer cells called prostatic acid phosphatase (PAP). The white blood cells are then sent back to the doctor’s office or hospital, where they are given back to you by infusion into a vein (IV). This process is repeated 2 more times, 2 weeks apart, so that you get 3 doses of cells. The cells help your other immune system cells attack the prostate cancer.
The vaccine hasn’t been shown to stop prostate cancer from growing, but it seems to help men live several months longer. As with hormone therapy and chemotherapy, this type of treatment has not been shown to cure prostate cancer.
Possible side effects of vaccine treatment
Common side effects from the prostate cancer vaccine can include fever, chills, fatigue, back and joint pain, nausea, and headache. These most often start during the cell infusions and last no more than a couple of days. A few men may have more severe symptoms, including problems breathing and high blood pressure, which usually get better after treatment.
Immune checkpoint inhibitors
An important part of the immune system is its ability to keep itself from attacking the body’s normal cells. To do this, it uses “checkpoint” proteins on immune cells, which act like switches that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to keep the immune system from attacking them. But drugs that target these checkpoints hold a lot of promise as cancer treatments.
Drugs called checkpoint inhibitors can be used for people whose prostate cancer cells have tested positive for specific gene changes, such as a high level of microsatellite instability (MSI-H), or changes in one of the mismatch repair (MMR) genes. Changes in MSI or in MMR genes (or both) are often seen in people with Lynch syndrome.
The drugs are used for people whose cancer starts growing again after chemotherapy. They might also be used to treat people whose cancer can’t be removed with surgery, has come back (recurred) after treatment, or has spread to other parts of the body (metastasized).
PD-1 inhibitor
Pembrolizumab (Keytruda) is a drug that targets PD-1, a checkpoint protein on immune system cells called T cells, that normally helps keep these cells from attacking normal cells in the body. By blocking PD-1, this drug boosts the immune response against prostate cancer cells. It has shown promising results in some men with prostate cancer and continues to be studied.
This drug is given as an intravenous (IV) infusion every 2 or 3 weeks.
Side effects can include fatigue, cough, nausea, itching, skin rash, decreased appetite, constipation, joint pain, and diarrhea.
Other, more serious side effects occur less often. This drug works by basically removing the brakes from the body’s immune system. Sometimes the immune system starts attacking other parts of the body, which can cause serious or even life-threatening problems in the lungs, intestines, liver, hormone-making glands, kidneys, or other organs.
It’s very important to report any new side effects to your health care team promptly. If serious side effects do occur, treatment may need to be stopped and you may get high doses of corticosteroids to suppress your immune system.
Targeted Therapy for Prostate Cancer
Targeted therapy is a type of cancer treatment that uses drugs to identify and attack cancer cells while doing little damage to normal cells. These therapies attack the cancer cells’ inner workings − the programming that makes them different from normal, healthy cells. Each type of targeted therapy works differently, but they all change the way a cancer cell grows, divides, repairs itself, or interacts with other cells.
PARP inhibitors
Rucaparib (Rubraca) and olaparib (Lynparza) are drugs known as a PARP (poly(ADP)-ribose polymerase) inhibitors. PARP enzymes are normally involved in one pathway to help repair damaged DNA inside cells. The BRCA genes (BRCA1 and BRCA2) are also normally involved in a different pathway of DNA repair, and mutations in those genes can block that pathway. By blocking the PARP pathway, these drugs make it very hard for tumor cells with an abnormal BRCA gene to repair damaged DNA, which often leads to the death of these cells. If you are not known to have a BRCA mutation, your doctor might test your blood or saliva and your tumor to be sure you have one before starting treatment with this drug.
These drugs are taken twice a day by mouth as pills.
- Rucaparib (Rubraca) can be used to treat advanced castration-resistant prostate cancer that has grown after taxane chemotherapy (such as docetaxel or cabazitaxel) or anti-androgens have been tried. It can be used in men with a mutation in one of the BRCA genes. This drug is given with a LHRH agonist or to men who have had an orchiectomy.
- Olaparib (Lynparza) can be used to treat advanced castration-resistant prostate cancer that has grown after the hormone therapy drugs, enzalutamide or abiraterone, have been tried. It can be used in men with a mutation in one of the BRCA genes. This drug is given with a LHRH agonist or to men who have had an orchiectomy.
Side effects of PARP inhibitors can include nausea, vomiting, diarrhea, fatigue, loss of appetite, low red blood cell counts (anemia), constipation, skin rash, abnormal liver blood tests, low blood platelet counts, cough and shortness of breath. Rarely, some people treated with these drugs have developed a blood cancer, such as myelodysplastic syndrome or acute myeloid leukemia. Some men taking olaparib had problems with blood clots in the lungs or legs.
Treatments for Prostate Cancer Spread to Bones
If prostate cancer spreads to other parts of the body, it nearly always goes to the bones first. Bone metastasis can be painful and can cause other problems, such as fractures (breaks), spinal cord compression (an area of cancer is pressing on the spinal cord), or high blood calcium levels, which can be dangerous or even life threatening.
If the cancer has grown outside the prostate, preventing or slowing the spread of the cancer to the bones is a major goal of treatment. If the cancer has already reached the bones, controlling or relieving pain and other complications is also a very important part of treatment.
Treatments such as hormone therapy, chemotherapy, and vaccines may help with this, but other treatments specifically target bone metastasis and the problems it may cause.
Bisphosphonates
Bisphosphonates are drugs that work by slowing down bone cells called osteoclasts. These cells normally break down the hard mineral structure of bones to help keep them healthy. Osteoclasts often become overactive when prostate cancer spreads to the bones, which can cause problems. Bisphosphonates can be used:
- To help relieve pain and high calcium levels caused by cancer that has spread to the bones
- To help slow the growth of cancer that has spread to the bones and help delay or prevent fractures
- To help strengthen bones in men who are getting hormone therapy
Zoledronic acid (Zometa) is a commonly used bisphosphonate for prostate cancer. This drug is given as an intravenous (IV) injection, usually either once every 3 or 4 weeks, or once every 12 weeks. Men given this drug are advised to take a supplement containing calcium and vitamin D to prevent problems with low calcium levels.
Sometimes other bisphosphonates are used to treat prostate cancer that has spread to bone.
Bisphosphonates can have side effects, including flu-like symptoms and bone or joint pain. They can also cause kidney problems, so patients with poor kidney function might not be able to be treated with these medicines.
A rare but very serious side effect of these drugs is osteonecrosis of the jaw. With this condition, part of the jaw bone loses its blood supply and dies. This can lead to tooth loss and infections of the jaw bone that are hard to treat. Some people develop osteonecrosis of the jaw when dental work is done during treatment. Many times men are advised to have a dental checkup and have any tooth or jaw problems treated before they start taking a bisphosphonate. Maintaining good oral hygiene by flossing and brushing, making sure that dentures fit properly, and having regular dental checkups may also help prevent osteonecrosis of the jaw.
Denosumab
Denosumab (Xgeva) is another drug that can help when prostate cancer spreads to bone. Like the bisphosphonates, denosumab also blocks osteoclasts, but it does so in a different way. This drug can be used:
- To help prevent or delay problems like fractures in men whose cancer has already spread to the bones. It may be helpful even if zoledronic acid is no longer working.
- To help strengthen bones in men who are getting hormone therapy
This drug is injected under the skin every 4 weeks. Men given this drug are often advised to take a supplement containing calcium and vitamin D to prevent problems with low calcium levels.
Common side effects include nausea, diarrhea, and feeling weak or tired. Like the bisphosphonates, denosumab can also cause osteonecrosis of the jaw, so doctors recommend taking the same precautions (such as having teeth and jaw problems treated before starting the drug).
Corticosteroids
Some studies suggest that corticosteroid drugs (such as prednisone and dexamethasone) can help relieve bone pain in some men. They also can help lower PSA levels. These drugs are often already a part of prostate cancer treatment that has spread.
External radiation therapy
Radiation therapy can help reduce bone pain, especially if the pain is limited to one or only a few areas of bone. Radiation can be aimed at tumors on the spine, which can help relieve pressure on the spinal cord in some cases, and prevent paralysis. Radiation therapy may also help relieve other symptoms by shrinking tumors in other parts of the body.
Radiopharmaceuticals
Radiopharmaceuticals are drugs that contain radioactive elements. They are injected into a vein and settle in areas of damaged bones (like those containing cancer spread). Once there, they give off radiation that kills cancer cells. These drugs can be used to treat prostate cancer that has spread to many bones. Unlike external beam radiation, these drugs can reach all the affected bones at the same time.
The radiopharmaceuticals that can be used to treat prostate cancer spread to bone include:
- Strontium-89 (Metastron)
- Samarium-153 (Quadramet)
- Radium-223 (Xofigo)
All of these drugs can help relieve pain caused by bone metastases. Radium-223 has also been shown to help men who have prostate cancer spread only to their bones (as opposed to spread to other organs such as the lungs) to live longer. For these men, radium-223 may be an early part of treatment.
The major side effect of these drugs is a decrease in blood cell counts, which could increase risks for infections or bleeding, especially if your counts are already low. Other side effects have also been seen, so ask your doctor what you can expect.
Surgery
Kyphoplasty is a minor surgery to stabilize a painful collapsed bone in a spine weakened by prostate cancer. During this procedure a small incision is made in the middle of the back and a balloon is placed into the weak spinal bone. The balloon is first filled with air and then a cement-like mixture (which will harden) to stabilize the bone and spine.
Pain medicines
When properly prescribed, pain medicines are very effective. Pain medicines work best when they’re taken on a regular schedule. They don’t work as well if they’re only used when the pain becomes severe.
If you have bone pain from prostate cancer, it’s very important that it’s treated. This can help you feel better and let you focus on the things that are most important to you. Don’t hesitate to discuss pain, other symptoms, or any quality of life concerns with your cancer care team. Pain and most other symptoms of prostate cancer can often be treated.
Initial Treatment of Prostate Cancer, by Stage
The stage of your cancer is one of the most important factors in choosing the best way to treat it. Prostate cancer is staged based on the extent of the cancer (using T, N, and M categories) and the PSA level and Gleason score at the time of diagnosis.
But other factors, such as your age, overall health, life expectancy, and personal preferences should also be taken into account when looking at treatment options. In fact, many doctors determine a man’s possible treatment options based not just on the stage, but on the risk of cancer coming back (recurrence) after the initial treatment and on the man’s life expectancy.
You might want to ask your doctor what factors he or she is considering when discussing your treatment options. Some doctors might recommend options that are different from those listed here.
- Very-low-risk group. For men in this group without any other serious health problems that may limit their lifespan, active surveillance is often recommended because these tumors are unlikely to harm the patient, while radiation and surgery can have side effects that can change a man’s quality of life. For men who wish to start treatment, radiation therapy (external beam or brachytherapy) or radical prostatectomy may be options. For men who have medical problems that might shorten their lifespan, observation is another possibility.
- Low-risk group. Most men whose prostate cancers are in the low-risk group and who don’t have serious health issues will be offered active surveillance since very few of these cancers will spread to distant sites. Other options, depending on your preferences, include radiation therapy (external beam or brachytherapy) or radical prostatectomy. If the findings after surgery show that the cancer has features that make it more likely to come back, then the following treatments might be considered:
- External beam radiation to the prostate bed (the area where the prostate gland used to rest before it was removed) with or without androgen deprivation therapy (ADT) OR
- Close follow-up of the PSA levels with the plan to consider radiation treatment when the PSA level starts to go up.
- Observation is often a good option for men whose cancer is not causing any symptoms and who have other serious health problems.
- Intermediate-risk group. Radiation therapy (external beam or brachytherapy), often with androgen deprivation therapy, is an option for men in this group. A radical prostatectomy with pelvic lymph node dissection is also an option. Depending on the findings from surgery, treatments that might be discussed include:
- External beam radiation therapy with or without androgen deprivation therapy if the cancer is found in the lymph nodes or if it has features that make it more likely to come back (recur)
- Close follow-up of the PSA level with the plan to consider radiation treatment when the PSA level starts to rise.
- Active surveillance is an option for people in this group whose cancers have favorable features. But people with intermediate-risk prostate cancers with favorable features that are under active surveillance should keep in mind that there is a slightly higher risk of the cancer spreading compared to getting radiation treatment or radical prostatectomy with pelvic lymph node dissection as the initial therapy.
- Men who have other serious medical problems may choose less aggressive treatment such as radiation alone or observation.
- High-risk group. People with cancer in this group might be offered:
- Radiation therapy (external beam with brachytherapy OR external beam radiation alone) along with androgen deprivation therapy for 1 to 3 years.
- Radical prostatectomy with pelvic lymph node dissection. If cancer is found in the lymph nodes taken during surgery or if it has features that make it more likely to come back (recur), androgen deprivation therapy with or without radiation might be recommended. In some cases, instead of radiation or androgen deprivation therapy therapy, watching the PSA closely after surgery might be considered with the plan to consider androgen deprivation therapy with or without radiation treatment when the PSA level rises.
- For men with other serious health problems and symptoms from their prostate cancer, androgen deprivation therapy alone might be a good choice. For men with no symptoms from the cancer and who have major health issues, androgen deprivation therapy alone, external beam radiation therapy alone, or observation are options.
- Very-high-risk group. Treatment options for people in this group include:
- External beam radiation therapy (with or without brachytherapy) along with androgen deprivation therapy for 1 to 3 years. Sometimes, the chemotherapy drug docetaxel or the hormone drug abiraterone might be added to radiation plus androgen deprivation therapy.
- Radical prostatectomy with pelvic lymph node dissection (especially for younger men). If cancer is found in the lymph nodes taken during surgery, androgen deprivation therapy with or without external beam radiation treatment might be given. Radiation therapy with or without androgen deprivation therapy might be recommended if the cancer is not found in the lymph nodes but does have features that make it more likely to come back (recur). In some cases, instead of radiation or androgen deprivation therapy therapy, watching the PSA level closely after surgery might be done with the plan to consider androgen deprivation therapy with or without radiation treatment when the PSA level rises.
- For men with no symptoms from the cancer but who have major health issues, treatment options include androgen deprivation therapy alone, external beam radiation therapy alone, or observation.
Prostate Cancer Stage 1
These prostate cancers are small (T1 or T2a) and have not grown outside the prostate. They have low Gleason scores (6 or less) and low PSA levels (less than 10). They usually grow very slowly and may never cause any symptoms or other health problems.
For men without any prostate cancer symptoms who are elderly and/or have other serious health problems that may limit their lifespan, watchful waiting or active surveillance is often recommended. For men who wish to start treatment, radiation therapy (external beam or brachytherapy) or radical prostatectomy may be options.
Men who are younger and healthy may consider active surveillance (knowing that they may need to be treated later on), radical prostatectomy, or radiation therapy (external beam or brachytherapy).
Prostate Cancer Stage 2
Stage 2 cancers have not yet grown outside of the prostate, but are larger, have higher Gleason scores, and/or have higher PSA levels than stage 1 cancers. Stage 2 cancers that are not treated with surgery or radiation are more likely than stage I cancers to eventually spread beyond the prostate and cause symptoms.
As with stage 1 cancers, active surveillance is often a good option for men whose cancer is not causing any symptoms and who are elderly and/or have other serious health problems. Radical prostatectomy and radiation therapy (external beam or brachytherapy) may also be appropriate options.
Treatment options for men who are younger and otherwise healthy might include:
- Radical prostatectomy (often with removal of the pelvic lymph nodes). This may be followed by external beam radiation if your cancer is found to have spread beyond the prostate at the time of surgery, or if the PSA level is still detectable a few months after surgery.
- External beam radiation only*
- Brachytherapy only*
- Brachytherapy and external beam radiation combined*
- Taking part in a clinical trial of newer treatments
*All of the radiation options may be combined with several months of hormone therapy if there is a greater chance of cancer recurrence based on PSA level and/or Gleason score.
Prostate Cancer Stage 3
Stage 3 cancers have grown outside the prostate but have not reached the bladder or rectum (T3). They have not spread to lymph nodes or distant organs. These cancers are more likely to come back after treatment than earlier stage tumors.
Treatment options at this stage may include:
- External beam radiation plus hormone therapy
- Radiation (external beam plus brachytherapy), possibly with a short course of hormone therapy
- Radical prostatectomy in selected cases (often with removal of the pelvic lymph nodes). This may be followed by radiation therapy.
Men who are older or who have other medical problems may choose less aggressive treatment such as hormone therapy (by itself) or even active surveillance.
Taking part in a clinical trial of newer treatments is also an option for many men with stage 3 prostate cancer.
Prostate Cancer Stage 4
Stage 4 cancers have already spread to nearby areas such as the bladder or rectum (T4), to nearby lymph nodes, or to distant organs such as the bones. A small portion of T4 cancers may be curable using some of the same treatments for stage 3 cancers. Most stage 4 cancers can’t be cured, but are treatable. The goals of treatment are to keep the cancer under control for as long as possible and to improve a man’s quality of life.
Initial treatment options may include:
- Hormone therapy, possibly along with chemotherapy
- External beam radiation (sometimes along with brachytherapy), plus hormone therapy
- Radical prostatectomy in some men whose cancer has not spread to the lymph nodes or other parts of the body. This might be followed by external radiation therapy.
- Surgery (TURP) to relieve symptoms such as bleeding or urinary obstruction
- Treatments aimed at bone metastases, such as denosumab (Xgeva), a bisphosphonate like zoledronic acid (Zometa), external radiation aimed at bones, or a radiopharmaceutical such as strontium-89, samarium-153 or radium-223
- Active surveillance (for those who are older or have other serious health issues and do not have major symptoms from the cancer)
- Taking part in a clinical trial of newer treatments
Treatment of stage 4 prostate cancer may also include treatments to help prevent or relieve symptoms such as pain.
The options above are for the initial treatment of prostate cancer at different stages. But if these treatments aren’t working (the cancer continues to grow and spread) or if the cancer comes back, other treatments might be used.
Stage 4A prostate cancer
Stage 4A prostate cancers have spread to nearby lymph nodes but not to distant sites. For men who are healthy enough to get treatment or have symptoms from the cancer, options include:
- External beam radiation treatment with androgen deprivation therapy(with or without abiraterone)
androgen deprivation therapy with or without abiraterone - Radical prostatectomy with pelvic lymph node dissection. If cancer is found in the lymph nodes taken during surgery or it has features that make it more likely to come back (recur), androgen deprivation therapy with or without external beam radiation treatment might be given. In some cases, instead of radiation or androgen deprivation therapy therapy, watching the
- PSA closely after surgery might be done with the plan to consider androgen deprivation therapy with or without radiation treatment when the PSA level starts to go up.
For men with Stage 4A cancer without symptoms or with other serious health problems, observation or androgen deprivation therapy alone might be recommended.
Stage 4B prostate cancer
Stage 4B cancers have spread to distant organs such as the bones. Most stage 4B cancers can’t be cured, but are treatable. The goals of treatment are to keep the cancer under control for as long as possible and to improve a man’s quality of life.
Initial treatment options may include:
- Androgen deprivation therapy with abiraterone
- Androgen deprivation therapy with apalutamide
- Androgen deprivation therapy with chemotherapy, specifically docetaxel
- Androgen deprivation therapy with enzalutamide
- Androgen deprivation therapy with external beam radiation to the tumor in the prostate
- Androgen deprivation therapy alone
- Surgery (TURP) to relieve symptoms such as bleeding or urinary obstruction
- Treatments aimed at painful bone metastases, such as external radiation
- Denosumab (Xgeva), a bisphosphonate like zoledronic acid (Zometa), external radiation aimed at bones, or a radiopharmaceutical such as radium-223, strontium-89, or samarium-153
- Observation (for those who are older or have other serious health issues and do not have major symptoms from the cancer)
- Taking part in a clinical trial of newer treatments
Treatment of stage 4 prostate cancer may also include treatments to help prevent or relieve symptoms such as pain from bone metastases with drugs like denosumab (Xgeva), a bisphosphonate like zoledronic acid (Zometa), or a radiopharmaceutical such as radium-223, strontium-89, or samarium-153.
The options above are for the initial treatment of prostate cancer at different risk groups and stages. But if these treatments aren’t working (the cancer continues to grow and spread) or if the cancer comes back, other treatments might be used, such as immunotherapy or chemotherapy.
Treating Prostate Cancer That Doesn’t Go Away or Comes Back After Treatment
If your prostate-specific antigen (PSA) blood level or another test shows that your prostate cancer has not been cured or has come back (recurred) after the initial treatment, further treatment can often still be helpful. Follow-up treatment will depend on where the cancer is thought to be and what treatment(s) you’ve already had. Imaging tests such as CT, MRI, or bone scans may be done to get a better idea about where the cancer is.
Cancer that is still thought to be in or around the prostate
If the cancer is still thought to be just in the area of the prostate, a second attempt to cure the cancer might be possible.
- After surgery: If you’ve had a radical prostatectomy, radiation therapy might be an option, sometimes along with hormone therapy.
- After radiation therapy: If your first treatment was radiation, treatment options might include cryotherapy or radical prostatectomy, but when these treatments are done after radiation, they carry a higher risk for side effects such as incontinence. Having radiation therapy again is usually not an option because of the increased potential for serious side effects, although in some cases brachytherapy may be an option as a second treatment after external radiation.
Sometimes it might not be clear exactly where the remaining cancer is in the body. If the only sign of cancer recurrence is a rising PSA level (as opposed to the cancer being seen on imaging tests), another option for some men might be active surveillance instead of active treatment. Prostate cancer often grows slowly, so even if it does come back, it might not cause problems for many years, at which time further treatment could then be considered.
Factors such as how quickly the PSA is going up and the original Gleason score of the cancer can help predict how soon the cancer might show up in distant parts of the body and cause problems. If the PSA is going up very quickly, some doctors might recommend that you start treatment even before the cancer can be seen on tests or causes symptoms.
Observation might be a more appealing option to certain groups of men, such as those who are older and in whom the PSA level is rising slowly. Still, not all men might be comfortable with this approach.
If the PSA is rising quickly enough to warrant treatment, but localized treatments (such as surgery, radiation therapy, or cryotherapy) aren’t likely to be helpful, hormone therapy is often the next option. If one type of hormone therapy isn’t helpful, another can be tried.
Cancer that clearly has spread
If the cancer has spread outside the prostate, it will most likely go to nearby lymph nodes first, and then to bones. Much less often the cancer will spread to the liver or other organs.
When prostate cancer has spread to other parts of the body (including the bones), hormone therapy is probably the most effective treatment. But it isn’t likely to cure the cancer, and at some point it might stop working. Usually the first treatment is a luteinizing hormone-releasing hormone (LHRH) agonist, LHRH antagonist, or orchiectomy, sometimes along with an anti-androgen drug or abiraterone. Another option might be to get chemotherapy along with the hormone therapy. Other treatments aimed at bone metastases might be used as well.
Castrate-resistant and hormone-refractory prostate cancer
Hormone therapy is often very effective at shrinking or slowing the growth of prostate cancer that has spread, but it usually becomes less effective over time. Doctors use different terms to describe cancers that are no longer responding to hormones.
- Castrate-resistant prostate cancer is cancer that is still growing despite the fact that hormone therapy (an orchiectomy or an LHRH agonist or antagonist) is keeping the testosterone level in the body as low as what would be expected if the testicles were removed (called castrate levels). The cancer might still respond to other forms of hormone therapy, though.
- Hormone-refractory prostate cancer is cancer that is no longer helped by any form of hormone therapy.
Men whose prostate cancer is still growing despite initial hormone therapy now have many more treatment options than they had even a few years ago.
If an anti-androgen drug was not part of the initial hormone therapy, it is often added at this time. If a man is already getting an anti-androgen but the cancer is still growing, stopping the anti-androgen (while continuing other hormone treatments) seems to help sometimes.
Other forms of hormone therapy may also be helpful for a while, especially if the cancer is causing few or no symptoms. These include abiraterone (Zytiga), enzalutamide (Xtandi), apalutamide (Erleada), darolutamide (Nubeqa), ketoconazole, estrogens (female hormones), and corticosteroids.
The prostate cancer vaccine sipuleucel-T (Provenge) is another option for men whose cancer is causing few or no symptoms. This might not lower PSA levels, but it can often help men live longer.
For cancers that are no longer responding to initial hormone therapy and are causing symptoms, several options might be available. Chemotherapy with the drug docetaxel (Taxotere) is often the first choice because it has been shown to help men live longer, as well as to reduce pain. If docetaxel doesn’t work or stops working, other chemo drugs, such as cabazitaxel (Jevtana), may help.
Other options after chemotherapy might include:
- Immunotherapy with pembrolizumab (Keytruda), if the cancer is has certain gene changes (MSI-H or dMMR)
- A different type of hormone therapy, such as abiraterone, enzalutamide, or apalutamide (if they haven’t been tried yet)
- The radiopharmaceutical lutetium Lu 177 vipivotide tetraxetan (Pluvicto), if the cancer cells have the PSMA protein
- A targeted therapy drug, such as rucaparib (Rubraca) or olaparib (Lynparza), for men with a BRCA gene mutation
Bisphosphonates or denosumab can often help if the cancer has spread to the bones. These drugs can reduce pain and even slow cancer growth in many men. Other medicines and methods can also help keep pain and other symptoms under control. External radiation therapy can help treat bone pain if it’s only in a few spots. Radiopharmaceutical drugs can often reduce pain if it’s more widespread, and may also slow the growth of the cancer.
If you are having pain from prostate cancer, make sure your doctor and health care team know about it.
Several promising new medicines are now being tested against prostate cancer, including vaccines, monoclonal antibodies, and other new types of drugs. Because the ability to treat hormone-refractory prostate cancer is still not good enough, men are encouraged to explore new options by taking part in clinical trials.
Following PSA Levels During and After Prostate Cancer Treatment
A man’s prostate-specific antigen (PSA) blood level is often a good indicator of how effective treatment is or has been. Generally speaking, your PSA level should get very low after treatment. But PSA results aren’t always reliable, and sometimes doctors aren’t sure what they mean.
Before starting treatment, you might want to ask your doctor what your PSA level is expected to be during and after treatment, and what levels might cause concern. It’s important to know that the PSA level is only one part of the overall picture. Other factors can also play a role in determining if cancer is still there, if it is growing, or if it has come back.
It’s also important to know that PSA levels can sometimes fluctuate a bit on their own, even during or after treatment, so they may not always be a sign of what is actually happening with your cancer. Understandably, many men being treated for prostate cancer are very concerned about even very small changes in their PSA levels. The PSA level is an important tool to monitor the cancer, but not every rise in PSA means that the cancer is growing and requires treatment right away. To help limit unnecessary anxiety, be sure you understand what change in your PSA level might concern your doctor.
PSA level during watchful waiting (observation) or active surveillance
If you choose observation or active surveillance, your PSA level will be monitored closely (most likely along with other tests) to help decide if the cancer is growing and if treatment should be considered.
Your doctor will watch your PSA level and how quickly it is rising. Not all doctors agree on exactly what PSA level might require further action (such as a prostate biopsy or treatment). Again, talk to your doctor so you understand what change in your PSA might be considered cause for concern.
PSA level after surgery
Your PSA should fall to a very low or even undetectable level within a couple of months after radical prostatectomy. Because some PSA can remain in the blood for several weeks after surgery, even if all of the prostate cells were removed, doctors often advise waiting at least 6 to 8 weeks after surgery before checking the PSA level.
Some men might worry if their PSA is still detectable even at a very low level after surgery, but this does not always mean cancer is still in the body. Modern PSA blood tests can detect even tiny amounts of PSA, but these amounts might not always be significant, especially if they are not rising over time. It could just mean that you have some cells in the body making PSA, but these aren’t necessarily cancer cells.
Still, having any detectable PSA after surgery can be stressful for men and their families. If your PSA is still detectable after surgery, even at a very low level, talk to your doctor about what it might mean, and what the best course of action might be. Some doctors advise following such low PSA levels over time to get a better idea of what’s going on. Other doctors might recommend further treatment.
If your PSA increases after surgery, your doctor might also want to know how fast it is rising. Some evidence shows that faster-rising PSA levels may be a sign of cancer. Men who have a PSA level that doubles within a 3-month period tend to have a worse prognosis (outlook) compared to men whose PSA level does not double. This is also known as PSA doubling time.
PSA level after radiation therapy
Radiation therapy doesn’t kill all of the cells in the prostate gland, so it’s not expected to cause the PSA to drop to an undetectable level. The remaining normal prostate cells will still make some PSA.
The pattern of the drop in PSA after radiation therapy is also different from after surgery. PSA levels after radiation tend to drop slowly, and might not reach their lowest level until 2 years or more after treatment.
Doctors tend to follow the PSA levels every few months to look for trends. A one-time, small rise in PSA might cause closer monitoring, but it might not mean that the cancer is still there (or has returned), as PSA levels can fluctuate slightly from time to time. However, a PSA that is rising on consecutive tests after treatment might indicate that cancer is still there. Some medical groups have proposed that if the PSA rises more than 2 ng/mL above the lowest level reached, further treatment should be considered, but some doctors might advise tests to look for cancer in the body even if the PSA has not yet risen this much.
There is also a phenomenon called a PSA bounce that sometimes happens after external beam radiation and brachytherapy. The PSA rises slightly for a short time within the first couple of years after treatment, but then goes back down. Doctors aren’t sure why this happens, but it doesn’t seem to affect a man’s prognosis.
PSA level during treatment for advanced prostate cancer
When treatments such as hormone therapy, chemotherapy, or immunotherapy are used for more advanced prostate cancer, the PSA level can help show how well the treatment is working or when it might be time to try a different treatment.
Treatments should lower the PSA level (at least at first), although in some cases they may just help keep it from rising further, or even just slow the rise. Of course, other factors, such as whether you’re having symptoms from your cancer and whether imaging tests show it is growing, are also important when deciding if it might be time to change treatments.
If the cancer has spread outside the prostate, the actual PSA level is often not as important as whether it changes, and how quickly it changes. The PSA level itself does not predict whether or not a man will have symptoms or how long he will live. Many men have very high PSA levels and feel just fine. Other men with low PSA levels can have symptoms.
References- Prostate Cancer. American Cancer Society. https://www.cancer.org/cancer/prostate-cancer.html
- https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf
- Final Recommendation Statement: Prostate Cancer: Screening. https://www.uspreventiveservicestaskforce.org/uspstf/document/RecommendationStatementFinal/prostate-cancer-screening
- Jahn, J. L., Giovannucci, E. L., & Stampfer, M. J. (2015). The high prevalence of undiagnosed prostate cancer at autopsy: implications for epidemiology and treatment of prostate cancer in the Prostate-specific Antigen-era. International journal of cancer, 137(12), 2795–2802. https://doi.org/10.1002/ijc.29408
- Prostate Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/prost.html
- Key Statistics for Prostate Cancer. https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html
- Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, Minasian LM, Ford LG, Lippman SM, Crawford ED, Crowley JJ, Coltman CA Jr. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med. 2004 May 27;350(22):2239-46. doi: 10.1056/NEJMoa031918. Erratum in: N Engl J Med. 2004 Sep 30;351(14):1470.
- https://www.mayocliniclabs.com/test-catalog/overview/81944#Clinical-and-Interpretive
- https://www.aafp.org/afp/recommendations/viewRecommendation.htm?recommendationId=147
- Final Recommendation Statement – Prostate Cancer: Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/prostate-cancer-screening
- US Preventive Services Task Force. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(18):1901–1913. doi:10.1001/jama.2018.3710
- How to Counsel Men About PSA Screening. Am Fam Physician. 2016 Nov 15;94(10):782-784. https://www.aafp.org/afp/2016/1115/p782.html
- Fenton JJ, Weyrich MS, Durbin S, et al. Prostate-Specific Antigen-Based Screening for Prostate Cancer: A Systematic Evidence Review for the U.S. Preventive Services Task Force [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 May. (Evidence Synthesis, No. 154.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK518890
- Pinsky, P. F., Prorok, P. C., Yu, K., Kramer, B. S., Black, A., Gohagan, J. K., Crawford, E. D., Grubb, R. L., & Andriole, G. L. (2017). Extended mortality results for prostate cancer screening in the PLCO trial with median follow-up of 15 years. Cancer, 123(4), 592–599. https://doi.org/10.1002/cncr.30474
- Schröder, F. H., Hugosson, J., Roobol, M. J., Tammela, T. L., Ciatto, S., Nelen, V., Kwiatkowski, M., Lujan, M., Lilja, H., Zappa, M., Denis, L. J., Recker, F., Páez, A., Määttänen, L., Bangma, C. H., Aus, G., Carlsson, S., Villers, A., Rebillard, X., van der Kwast, T., … ERSPC Investigators (2012). Prostate-cancer mortality at 11 years of follow-up. The New England journal of medicine, 366(11), 981–990. https://doi.org/10.1056/NEJMoa1113135
- Schröder, F. H., Hugosson, J., Roobol, M. J., Tammela, T. L., Zappa, M., Nelen, V., Kwiatkowski, M., Lujan, M., Määttänen, L., Lilja, H., Denis, L. J., Recker, F., Paez, A., Bangma, C. H., Carlsson, S., Puliti, D., Villers, A., Rebillard, X., Hakama, M., Stenman, U. H., … ERSPC Investigators (2014). Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet (London, England), 384(9959), 2027–2035. https://doi.org/10.1016/S0140-6736(14)60525-0
- Tsodikov, A., Gulati, R., Heijnsdijk, E., Pinsky, P. F., Moss, S. M., Qiu, S., de Carvalho, T. M., Hugosson, J., Berg, C. D., Auvinen, A., Andriole, G. L., Roobol, M. J., Crawford, E. D., Nelen, V., Kwiatkowski, M., Zappa, M., Luján, M., Villers, A., Feuer, E. J., de Koning, H. J., … Etzioni, R. (2017). Reconciling the Effects of Screening on Prostate Cancer Mortality in the ERSPC and PLCO Trials. Annals of internal medicine, 167(7), 449–455. https://doi.org/10.7326/M16-2586
- Martin, R. M., Donovan, J. L., Turner, E. L., Metcalfe, C., Young, G. J., Walsh, E. I., Lane, J. A., Noble, S., Oliver, S. E., Evans, S., Sterne, J., Holding, P., Ben-Shlomo, Y., Brindle, P., Williams, N. J., Hill, E. M., Ng, S. Y., Toole, J., Tazewell, M. K., Hughes, L. J., … CAP Trial Group (2018). Effect of a Low-Intensity PSA-Based Screening Intervention on Prostate Cancer Mortality: The CAP Randomized Clinical Trial. JAMA, 319(9), 883–895. https://doi.org/10.1001/jama.2018.0154
- Ilic, D., Djulbegovic, M., Jung, J. H., Hwang, E. C., Zhou, Q., Cleves, A., Agoritsas, T., & Dahm, P. (2018). Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ (Clinical research ed.), 362, k3519. https://doi.org/10.1136/bmj.k3519
- Hugosson, J., Roobol, M. J., Månsson, M., Tammela, T., Zappa, M., Nelen, V., Kwiatkowski, M., Lujan, M., Carlsson, S. V., Talala, K. M., Lilja, H., Denis, L. J., Recker, F., Paez, A., Puliti, D., Villers, A., Rebillard, X., Kilpeläinen, T. P., Stenman, U. H., Godtman, R. A., … ERSPC investigators (2019). A 16-yr Follow-up of the European Randomized study of Screening for Prostate Cancer. European urology, 76(1), 43–51. https://doi.org/10.1016/j.eururo.2019.02.009
- Prostate Enlargement (Benign Prostatic Hyperplasia). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia
- Deters LA. Benign prostatic hypertrophy. https://emedicine.medscape.com/article/437359-overview
- BPH: surgical management. Urology Care Foundation. http://www.urologyhealth.org/urologic-conditions/benign-prostatic-hyperplasia-(bph)/treatment/surgery?article=31
- What Is Prostate Cancer ? American Cancer Society. https://www.cancer.org/cancer/prostate-cancer/about/what-is-prostate-cancer.html
- American Cancer Society Recommendations for Prostate Cancer Early Detection. American Cancer Society. https://www.cancer.org/cancer/prostate-cancer/early-detection/acs-recommendations.html
- Roumeguère T, Van Velthoven R. Le point sur le dépistage du cancer de la prostate par le PSA [Focus on the screening for prostate cancer by PSA]. Rev Med Brux. 2013 Sep;34(4):311-9. French.
- Leslie SW, Soon-Sutton TL, Sajjad H, et al. Prostate Cancer. [Updated 2022 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470550
- Tests to Diagnose and Stage Prostate Cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/how-diagnosed.html
- Tests for Prostate Cancer. American Cancer Society. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/how-diagnosed.html
- PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, As prostate cancer progresses from…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65951/figure/CDR0000520552__2
- Prostate Cancer Stages. American Cancer Society. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/staging.html
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage I prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1356
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIA prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1357
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIB prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1358
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIC prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1359
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIIA prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1360
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIIB prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1361
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIIC prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1362
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IVA prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1363
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Patient Version. 2021 Nov 12. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IVB prostate cancer. Cancer…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65915/figure/CDR0000062965__1364
- Uchio E, Aslan M, Ko J, Wells CK, Radhakrishnan K, Concato J. Velocity and doubling time of prostate-specific antigen: mathematics can matter. J Investig Med. 2016 Feb;64(2):400-4. doi: 10.1136/jim-2015-000008
- Hawken SR, Auffenberg GB, Miller DC, Lane BR, Cher ML, Abdollah F, Cho H, Ghani KR; Michigan Urological Surgery Improvement Collaborative. Calculating life expectancy to inform prostate cancer screening and treatment decisions. BJU Int. 2017 Jul;120(1):9-11. doi: 10.1111/bju.13812
- Treating Prostate Cancer. American Cancer Society. https://www.cancer.org/cancer/prostate-cancer/treating.html