Pulmonary capillary wedge pressure
Pulmonary capillary wedge pressure or PCWP, provides an indirect estimate of left atrial pressure 1 or left ventricular end-diastolic pressure 2, which is the “gold standard” for determining left ventricular filling pressure 3. However, recent studies have shown that, in pulmonary arterial hypertension (PAH) patients, PCWP can lead to erroneous pulmonary hypertension classification compared with a diagnosis based on left ventricular end-diastolic pressure 4. Many factors can interfere with the accurate measurement of pulmonary capillary wedge pressure (PCWP) 5, including factors related to the measurement techniques themselves 6 and patient-specific factors, such as obesity, hypoxemia 7 and ventilation 8.
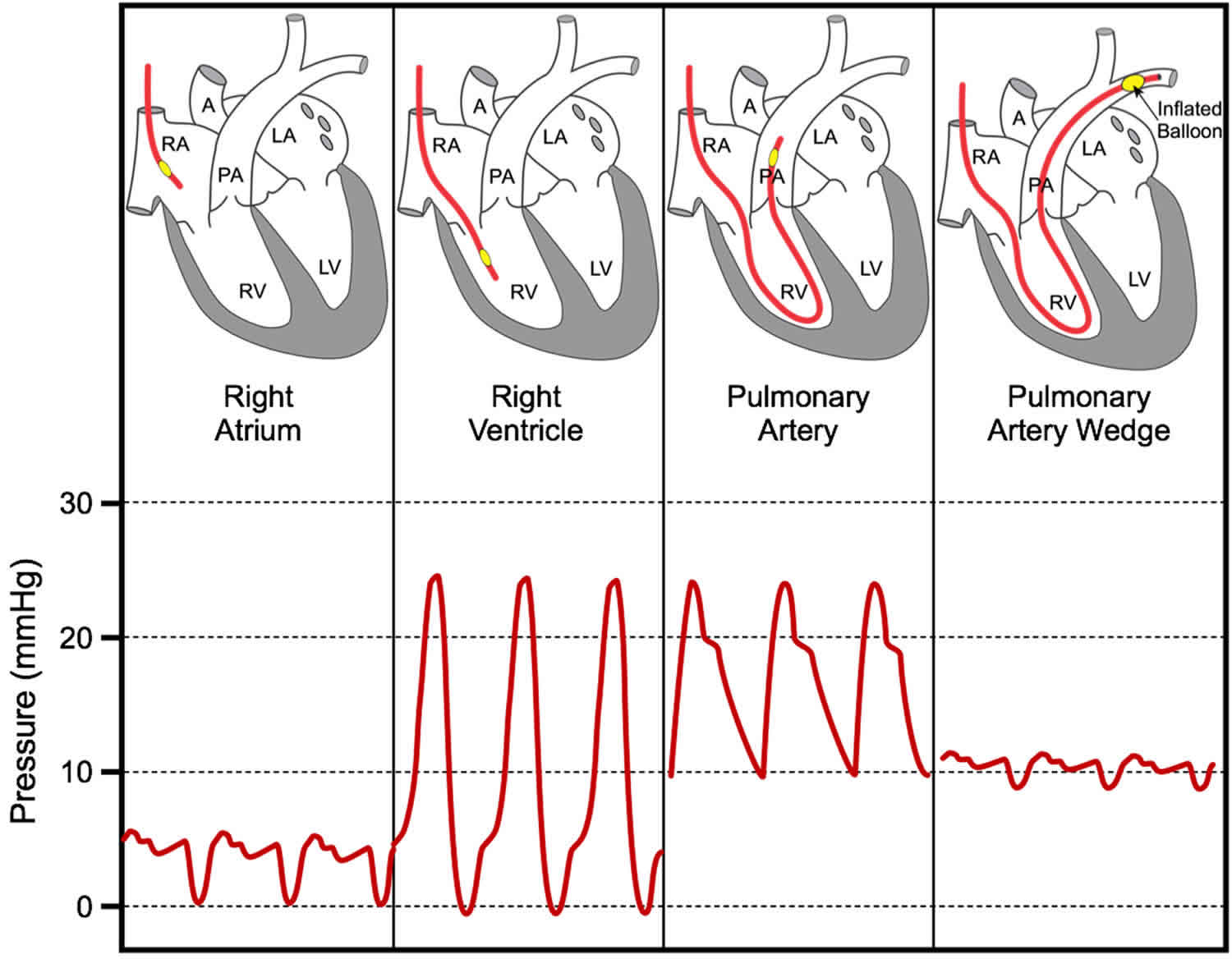
Normal right-sided hemodynamics include a right atrial pressure less than 7 mm Hg, right ventricular (RV) pressure below 30/7 mm Hg, pulmonary pressure less than 30/18 mm Hg, pulmonary capillary wedge pressure (PCWP) below 18 mm Hg, and cardiac index above 2.2 L/min/m² 9.
PCWP can be measured by using a pulmonary arterial catheter (Swan-Ganz catheter). This helps to differentiate cardiogenic causes of decompensated heart failure from noncardiogenic causes, such as acute respiratory distress syndrome (ARDS), which occurs secondary to injury to the alveolar-capillary membrane rather than to alteration in Starling forces 9. A PCWP exceeding 18 mm Hg in a patient not known to have chronically elevated left atrial pressure is indicative of cardiogenic decompensated heart failure 9. In patients with chronic pulmonary capillary hypertension, capillary wedge pressures exceeding 25 mm Hg are generally required to overcome the pumping capacity of the lymphatics and produce pulmonary edema.
Large V waves may be observed in the PCWP tracing in patients with significant mitral regurgitation because large volumes of blood regurgitate into a poorly compliant left atrium. This raises the pulmonary venous pressure and may cause pulmonary edema.
Pulmonary hypertension is defined by a mean pulmonary artery pressure ≥ 25 mm Hg at rest, measured during right heart catheterization 10. The term pulmonary arterial hypertension (PAH) describes a subpopulation of patients with pulmonary hypertension characterized hemodynamically by the presence of pre-capillary pulmonary hypertension including an end-expiratory pulmonary artery wedge pressure (PAWP) ≤ 15 mm Hg and a pulmonary vascular resistance >3 Wood units (mm Hg/L/min/m2). Right heart catheterization remains essential for a diagnosis of pulmonary hypertension or pulmonary arterial hypertension. This procedure requires further standardization, including uniformity of the pressure transducer zero level at the midthoracic line, which is at the level of the left atrium. One of the most common problems in the diagnostic workup of patients with pulmonary hypertension is the distinction between pulmonary arterial hypertension and pulmonary hypertension due to left heart failure with preserved ejection fraction (HFpEF). A normal pulmonary artery wedge pressure (PAWP) does not rule out the presence of left heart failure with preserved ejection fraction. Volume or exercise challenge during right heart catheterization may be useful to unmask the presence of left heart disease, but both tools require further evaluation before their use in general practice can be recommended. Early diagnosis of pulmonary arterial hypertension remains difficult, and screening programs in asymptomatic patients are feasible only in high-risk populations, particularly in patients with systemic sclerosis, for whom recent data suggest that a combination of clinical assessment and pulmonary function testing including diffusion capacity for carbon monoxide, biomarkers, and echocardiography has a higher predictive value than echocardiography alone.
Although left ventricular pressure can be directly measured by placing a catheter within the left ventricle, it is not feasible to advance this catheter back into the left atrium. Left atrial pressure can be measured by placing a special catheter into the right atrium then punching through the interatrial septum; however, for obvious reasons, this is not usually performed because of damage to the septum and potential harm to the patient. Therefore, it is important to use other tools to confirm the accuracy and reliability of pulmonary capillary wedge pressure measurements during right-heart catheterization. In this context, clinical characteristics are often helpful for distinguishing between pulmonary arterial hypertension patients and patients with pulmonary hypertension caused by left-side heart disease 11. Determining the likelihood of each disease may help interpret the right heart catheterization results and improve the reliability of pulmonary capillary wedge pressure measurements. Although PCWP is a widely used diagnostic measurement, left ventricular end-diastolic pressure is not analyzed in the majority of hemodynamic laboratories.
It is helpful to measure pulmonary capillary wedge pressure to diagnose the severity of left ventricular failure and to quantify the degree of mitral valve stenosis. Both of these conditions elevate left atrial pressure and therefore PCWP. Aortic valve stenosis and regurgitation, and mitral regurgitation also elevate left atrial pressure. When these pressures are above 20 mmHg, pulmonary edema is likely to occur, which is a life-threatening condition. Note that left atrial pressure is the outflow or venous pressure for the pulmonary circulation and therefore increases in left atrial pressure are transmitted almost fully back to the pulmonary capillaries thereby increasing their hydrostatic pressure and filtration of fluid. By measuring PCWP, the physician can titrate the dose of diuretic drugs and other drugs that are used to reduce pulmonary venous and capillary pressure, and thereby reduce pulmonary edema. Therefore, measurement of pulmonary capillary wedge pressure can help guide therapeutic efficacy.
Pulmonary capillary wedge pressure is also important to measure when evaluating pulmonary hypertension. Pulmonary hypertension is often caused by increased pulmonary vascular resistance. To calculate this, pulmonary blood flow (usually measured by the thermodilution technique), pulmonary artery pressure and pulmonary venous pressure measurements are required. Pulmonary hypertension can also result from increases in pulmonary venous pressure and pulmonary blood volume secondary to left ventricular failure or mitral or aortic valve disease.
PCWP is also useful in evaluating blood volume status when fluids are administered during hypotensive shock. One practice is to administer fluids at a rate that maintains pulmonary capillary wedge pressure between 12-14 mmHg.
How is pulmonary capillary wedge pressure measured?
PCWP is measured by inserting balloon-tipped, multi-lumen catheter (Swan-Ganz catheter) into a peripheral vein (e.g., jugular or femoral vein), then advancing the catheter into the right atrium, right ventricle, pulmonary artery, and then into a branch of the pulmonary artery. The catheter has a lumen (port) that opens at the tip of the catheter distal to the balloon. This port is connected to a pressure transducer. As illustrated below, the location of the catheter can be determined by viewing the pressure measured from the tip of the catheter. In the right atrium, the pressure usually averages <5 mmHg and fluctuates a few mmHg. When the catheter is advanced into the right ventricle, the systolic pressure increases to ~25 mmHg and the diastolic pressure remains similar to right atrial diastolic pressure. When the catheter enters the pulmonary artery, the systolic pressure normally is similar to the right ventricular systolic pressure, but the diastolic pressure increases to about 10 mmHg because of pulmonic valve closure at the beginning of diastole. Just behind the tip of the catheter is a small balloon that can be inflated with air (~1 cc). When properly positioned in a branch of the pulmonary artery, the distal port measures pulmonary artery pressure (~ 25/10 mmHg; systolic/diastolic pressure). The balloon is then inflated, which occludes the branch of the pulmonary artery. When this occurs, the pressure in the distal port rapidly falls, and after several seconds, reaches a stable lower value that is very similar to left atrial pressure (mean pressure normally 8-10 mmHg). The pressure flucuates during the cardiac cycle and normally shows a, c and v waves similar to the right atrial pressure tracing. The balloon is then deflated. The same catheter can be used to measure cardiac output by the thermodilution technique.
The pressure recorded during balloon inflation is similar to left atrial pressure because the occluded vessel and its distal branches that eventually form the pulmonary veins act as a long catheter that measures the blood pressures within the pulmonary veins and left atrium.
Pulmonary artery wedge pressure
Current guidelines recommend using a pulmonary artery wedge pressure (PAWP) or left ventricular end-diastolic pressure (LVEDP) ≤15 mm Hg to define pre-capillary pulmonary hypertension. Higher pulmonary artery wedge pressure values are commonly viewed as indicators of left heart disease. However, patients with the diagnosis of heart failure with preserved ejection fraction (HFpEF) can have a resting pulmonary artery wedge pressure (PAWP) <15 mm Hg and patients with features otherwise indicating the presence of pulmonary arterial hypertension may present with higher pulmonary artery wedge pressure values 12. In addition, pulmonary artery wedge pressure measurements vary between centers, and standardization is necessary to ensure comparisons of patient populations.
Pulmonary artery wedge pressure measurements may be largely affected by swings in the intrathoracic pressure, especially in patients with lung disease 13. This effect is least pronounced at the end of a normal expiration, which is the point at which pulmonary artery wedge pressure should be determined. Many available devices do not provide end-expiratory but digitized mean pulmonary artery wedge pressure and therefore tend to underestimate the pulmonary artery wedge pressure. For standardization of pulmonary artery wedge pressure measurements, values should be determined at the end of normal expiration (breath holding is not required). Ideally, high-fidelity tracings on paper should be used, rather than small moving tracings on a cardiac monitor.
Normal pulmonary artery wedge pressure values have been explored since the advent of cardiac catheterization and have been found to range from 5 to 12 mm Hg in healthy volunteers. However, these data were generated in younger patients, and it remains unclear whether there is a physiological increase in pulmonary artery wedge pressure with aging. In a comprehensive analysis of the medical literature, Kovacs et al. 14 found that pulmonary artery wedge pressure at rest was independent of age, with values of 9 ± 2 mm Hg found in patients ranging from <24 to ≥70 years. Of note, the data of the oldest patient population were derived from 17 patients only. Prasad et al. 15 performed a small but meticulous study comparing hemodynamics and left ventricular function in elderly patients with and without heart failure with preserved ejection fraction, demonstrating that the normal pulmonary artery wedge pressure slightly increased with age, although usually not beyond 15 mm Hg. Most importantly, pulmonary artery wedge pressure levels ≤15 mm Hg did not rule out the presence of heart failure with preserved ejection fraction. On the basis of these and other data, it has been suggested to lower the pulmonary artery wedge pressure cutoff for pre-capillary pulmonary hypertension to 12 mm Hg. Reasons to reduce the pulmonary artery wedge pressure threshold to 12 mm Hg include the notion that pulmonary artery wedge pressure of 15 mm Hg is associated with a higher chance of misclassifying patients with heart failure with preserved ejection fraction as pulmonary arterial hypertension and that the use of 15 mm Hg has probably contributed to the labeling of patients with heart failure with preserved ejection fraction as pulmonary arterial hypertension with consequences for medical therapy as well as inclusions in clinical trials.
On the other hand, pulmonary artery wedge pressure ≤15 mm Hg has a high sensitivity to identify patients with pre-capillary pulmonary hypertension, and this cutoff value has been used for decades and has been widely memorized among physicians. Almost all pulmonary arterial hypertension trials have included patients with pulmonary artery wedge pressure ≤15 mm Hg, which means that the safety and efficacy of pulmonary arterial hypertension drugs have been evaluated in this patient population. Lowering the pulmonary artery wedge pressure threshold to 12 mm Hg decreases the likelihood of falsely labeling patients with pulmonary hypertension due to heart failure with preserved ejection fraction as pulmonary arterial hypertension but at the same time increases the rate at which the presence of pulmonary arterial hypertension is mistakenly excluded.
There is no single pulmonary artery wedge pressure value that allows for correct classification of all patients. Pulmonary artery wedge pressure is not a constant number but a biological variable that is affected by various factors, including fluid balance, intrathoracic pressure, and others. In many patients with left heart disease, it will be possible to at least temporarily lower pulmonary artery wedge pressure below 15 mm Hg with meticulous afterload reduction and diuretic medication 16. A comprehensive assessment of the patient’s medical history and risk factors together with echocardiographic assessment will provide a more reliable diagnosis than a single pulmonary artery wedge pressure (or left ventricular end-diastolic pressure) measurement. The presence of clinical risk factors (systemic hypertension, older age, obesity, diabetes mellitus, obstructive sleep apnea, coronary artery disease), atrial fibrillation, and echocardiographic findings such as left atrial enlargement or left ventricle hypertrophy indicate a high likelihood of heart failure with preserved ejection fraction 17.
A recent study showed that more than 50% of the patients with pulmonary hypertension and pulmonary artery wedge pressure ≤15 mm Hg had left ventricular end-diastolic pressure values >15 mm Hg during simultaneous right and left heart catheterization 18. These data raised a debate as to whether the hemodynamic classification as pre- or post-capillary pulmonary hypertension might be improved with routine left ventricular end-diastolic pressure measurements. The additional risks and costs associated with routine left heart catheterizations are considerable but might be offset by a more accurate diagnosis and the avoidance of the expensive and potentially harmful use of pulmonary arterial hypertension medications in patients with heart failure with preserved ejection fraction. The World Symposium on Pulmonary Hypertension working group felt that the current evidence does not support recommending left heart catheterization in all patients with pulmonary arterial hypertension, especially when neither the patient’s history nor clinical and echocardiographic findings suggest the presence of left ventricular dysfunction. However, the threshold to perform left heart catheterization should be low in patients with echocardiographic signs of systolic and/or diastolic left ventricular dysfunction as well as in patients with risk factors for coronary heart disease or heart failure with preserved ejection fraction. In addition, the finding of an elevated pulmonary artery wedge pressure in a patient when this is unexpected (normal left atrial size, absence of echocardiographic markers of elevated left ventricular filling pressures, absence of risk factors for heart failure with preserved ejection fraction should prompt the performing physician to measure left ventricular end-diastolic pressure to avoid misclassification.
Recommendations for pulmonary artery wedge pressure at rest 13:
- The World Symposium on Pulmonary Hypertension working group does not recommend lowering the threshold to 12 mm Hg in clinical practice.
- The cutoff for pre-capillary pulmonary hypertension should remain at ≤15 mm Hg because this value has been used in almost all clinical trials generating evidence for the safety and efficacy of pulmonary arterial hypertension-targeted therapies in patients fulfilling these criteria.
- Invasive hemodynamics need to be placed in clinical and echocardiographic context with regard to probability of existence of left heart disease.
- The current evidence does not support recommending left heart catheterization in all patients with pulmonary arterial hypertension.
- Pulmonary Capillary Wedge Pressure. https://cvphysiology.com/Heart%20Failure/HF008
- Walston, A. and Kendall, M.E. Comparison of pulmonary wedge and left atrial pressure in man. Am Heart J. 1973; 86: 159–164
- Usefulness of pulmonary capillary wedge pressure as a correlate of left ventricular filling pressures in pulmonary arterial hypertension. de Oliveira, Rudolf K.F. et al. The Journal of Heart and Lung Transplantation, Volume 33, Issue 2, 157 – 162 https://doi.org/10.1016/j.healun.2013.10.008
- Halpern, S.D. and Taichman, D.B. Misclassification of pulmonary hypertension due to reliance on pulmonary capillary wedge pressure rather than left ventricular end-diastolic pressure. Chest. 2009; 136: 37–43
- Bernstein, W., Fierer, E., Laszlo, M. et al. The interpretation of pulmonary artery wedge (pulmonary capillary) pressures. Br Heart J. 1960; 22: 37–44
- Tonelli, A.R., Mubarak, K.K., Li, N. et al. Effect of balloon inflation volume on pulmonary artery occlusion pressure in patients with and without pulmonary hypertension. Chest. 2011; 139: 115–121
- Ryan, J., Rich, J., Thiruvoipati, T. et al. Current practice for determining pulmonary capillary wedge pressure predisposes to serious errors in the classification of patients with pulmonary hypertension. Am Heart J. 2012; 163: 589–594
- Al-kharrat, T., Zarich, S., Amoateng-adjepong, Y. et al. Analysis of observer variability in measurement of pulmonary artery occlusion pressures. Am J Respir Crit Care Med. 1999; 160: 415–420
- Heart Failure Workup. https://emedicine.medscape.com/article/163062-workup
- Definitions and Diagnosis of Pulmonary Hypertension. J Am Coll Cardiol. 2013 Dec 24;62(25 Suppl):D42-50. doi: 10.1016/j.jacc.2013.10.032. https://doi.org/10.1016/j.jacc.2013.10.032
- Leung, C.C., Moondra, V., Catherwood, E. et al. Prevalence and risk factors of pulmonary hypertension in patients with elevated pulmonary venous pressure and preserved ejection fraction. Am J Cardiol. 2010; 106: 284–286
- A.E. Frost, H.W. Farber, R.J. Barst, D.P. Miller, C.G. Elliott, M.D. McGoon. Demographics and outcomes of patients diagnosed with pulmonary hypertension with pulmonary capillary wedge pressures 16 to 18 mm Hg: insights from the REVEAL registry. Chest, 143 (2013), pp. 185-195
- Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013 Dec 24;62(25 Suppl):D42-50. doi: 10.1016/j.jacc.2013.10.032. https://doi.org/10.1016/j.jacc.2013.10.032
- G. Kovacs, A. Olschewski, A. Berghold, H. Olschewski. Pulmonary vascular resistances during exercise in normal subjects: a systematic review. Eur Respir J, 39 (2012), pp. 319-328
- A. Prasad, J.L. Hastings, S. Shibata, et al. Characterization of static and dynamic left ventricular diastolic function in patients with heart failure with a preserved ejection fraction. Circ Heart Fail, 3 (2010), pp. 617-626
- W.T. Abraham, P.B. Adamson, R.C. Bourge, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet, 377 (2011), pp. 658-666
- M.M. Hoeper, J.A. Barbera, R.N. Channick, et al. Diagnosis, assessment, and treatment of non-pulmonary arterial hypertension pulmonary hypertension. J Am Coll Cardiol, 54 (2009), pp. S85-S96
- S.D. Halpern, D.B. Taichman. Misclassification of pulmonary hypertension due to reliance on pulmonary capillary wedge pressure rather than left ventricular end-diastolic pressure. Chest, 136 (2009), pp. 37-43