Pulse pressure
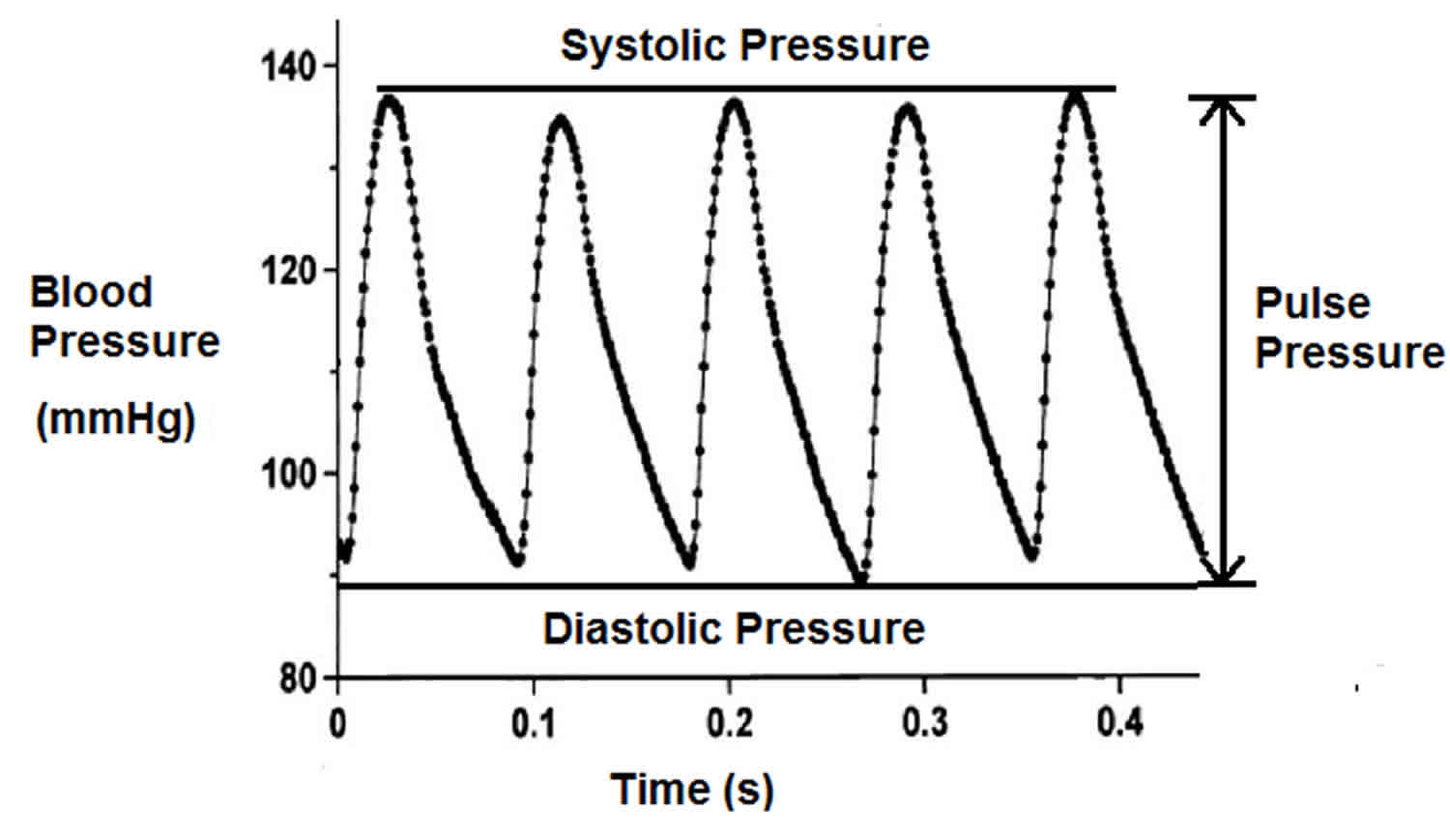
Pulse pressure is the difference between systolic and diastolic blood pressure (systolic blood pressure-diastolic blood pressure). Pulse pressure is measured in millimeters of mercury (mmHg). Pulse pressure represents the force that the heart generates each time it contracts. Resting blood pressure is normally approximately 120/80 mmHg, which yields a pulse pressure of approximately 40 mmHg. The normal pulse pressure is 30-40 mmHg. A pressure that exceeds this is called a wide pulse pressure. A pressure that is smaller than this (<25 mmHg) is a narrow pulse pressure. In some cases a low pulse pressure (less than 40 mmHg) may indicate poor heart function.
- Pulse Pressure = Systolic Blood Pressure – Diastolic Blood Pressure
Blood pressure readings are given in two numbers. The top number the systolic blood pressure is defined as the maximum pressure your heart exerts when the heart contracts and ejects blood into the aorta from the left ventricle (usually approximately 120 mm Hg). And the bottom number the diastolic blood pressure is defined as the minimum pressure experienced in the aorta when your heart is relaxing before ejecting blood into the aorta from the left ventricle, often approximately 80 mm Hg. Normal pulse pressure is, therefore, approximately 40 mm Hg. However, systolic and diastolic pressure should also be considered alongside pulse pressure values. Higher systolic and diastolic pairs imply higher risk than lower pairs with the same pulse pressure: 160/120 mmHg indicates a higher risk than 110/70 mm Hg even though the pulse pressure in each pair is 40 mm Hg.
A pulse pressure that is less than 25% of the systolic pressure is inappropriately low or “narrowed pulse pressure,” whereas, a pulse pressure of greater than 100 is high or “widened pulse pressure” 1.
Pulse pressure markedly rises after the 5th decade of life, due to arterial stiffening with increasing age 2. Several studies have shown a close relationship between high pulse pressure and the occurrence of cardiovascular death 3. Furthermore, high pulse pressure is a risk factor for the development of coronary heart disease, myocardial infarction, and heart failure in normotensive and hypertensive persons 4. For adults older than age 60, a pulse pressure greater than 60 mmHg (wide pulse pressure) can be a useful predictor of heart attacks or other cardiovascular disease; this is especially true for men. A higher pulse pressure (greater than 60) may reflect leaky heart valves (valve regurgitation), often due to age-related losses in aortic elasticity.
The research done by Blacher et al. 5 has shown that pulse pressure is a significant risk factor in the development of heart disease. Pulse pressure has even been shown to be more of a determinant than the mean arterial pressure (MAP), which is the average blood pressure that a patient experiences in a single cardiac cycle. In fact, as little as a 10-mm Hg increase in the pulse pressure increases the cardiovascular risk by as much as 20%. This finding was found to be consistent in both Caucasian and Asian populations 5.
Pulse pressure is also independently associated with an increased risk of developing atrial fibrillation. A study done by Mitchell et al. 6 showed that patients with a pulse pressure of 40 mm Hg or less developed atrial fibrillation at a rate of 5.6%, whereas patients with a pulse pressure greater than 61 mm Hg developed atrial fibrillation at a rate of 23.3%. In fact, for every 20-mm Hg increase in pulse pressure, the adjusted hazard ratio for developing atrial fibrillation is 1.28. This risk is independent of mean arterial pressure 7.
A recently published 20 year follow up study of almost 20 000 normotensive and hypertensive subjects aged 40–69 years found pulse pressure to be an independent predictor of all cause, total cardiovascular, and especially coronary mortality in men of all age and mean blood pressure groups 8. In a series of 5730 untreated hypertensives followed for an average of five years, pulse pressure was found to be the only measure of blood pressure significantly and independently related to the in-treatment incidence of heart attack (myocardial infarction) 9. The use of ambulatory blood pressure measurement in hypertension also strongly supports the prognostic importance of pulse pressure 10. This effect seems to be most pronounced in older subjects. The Framingham data restricted to those over 50 years old showed that the association with coronary heart disease risk, although positive for systolic and diastolic blood pressure, was strongest for pulse pressure 11. Coronary risk increased with lower diastolic blood pressure at any level of systolic blood pressure greater than 120 mm Hg. A study conducted by the Veterans Administration 12 showed that when systolic and diastolic blood pressure were considered jointly in a multivariate model containing clinical variables, systolic but not diastolic blood pressure was related to cardiovascular death in men aged < 60 years. By contrast, in older men systolic blood pressure was positively and diastolic blood pressure negatively related to outcome, suggesting that pulse pressure was the best haemodynamic determinant of outcome in the elderly 13.
Other research has focused on helping to maintain a normal pulse pressure. One of the most effective ways to do this is to increase arterial compliance. According to Thorin-Trescases et al. 14, endurance aerobic exercise is the only intervention that has been shown to help mitigate age-related arterial stiffening by reducing age-related increases in collagen 1 and 3 and calcification. These same benefits were not seen with resistance training, such as bench press, as this actually decreases the arterial compliance and increases the pulse pressure.
In addition to aerobic exercise training, Dart et al. 15 demonstrated that one could also increase arterial compliance by increasing estrogen compounds (as in hormone replacement in post-menopausal women), increasing the consumption of n-3 fatty acids, and decreasing salt intake. There has also been some evidence that supports the notion that ACE inhibitors have beneficial arterial wall effects and may be of use. Finally, research by Williams et al 16. showed that folic acid supplementation (a 3-week treatment with 5 mg of folic acid per day) could decrease the plasma homocysteine concentrations, which improves endothelial dysfunction and causes a reduction in the stiffness of large arteries.
Wide pulse pressure
The most important cause of wide pulse pressure is stiffness of the aorta, the largest artery in the body. The stiffness may be due to high blood pressure or fatty deposits damaging the walls of the arteries, leaving them less elastic (atherosclerosis). The greater your pulse pressure, the stiffer and more damaged the vessels are thought to be.
Valvular disease states such as aortic regurgitation and aortic stenosis result in changes in pulse pressure. In aortic regurgitation, the aortic valve insufficiency results in a backward, or regurgitant, flow of blood from the aorta back into the left ventricle, so that blood that was ejected during systole returns during diastole. This leads to an increase in the systolic pressure and a decrease in the diastolic pressure, which results in an increase in pulse pressure.
Aging impacts pulse pressure and arterial compliance. With aging, there is a decrease in the compliance of the large elastic arteries. This is due to structural molecular changes in the arterial wall, including decreased elastin content, increased collagen 1 deposition, and calcification which increases the stiffness of the wall. This process is often called “hardening of the arteries.” As the left ventricle contracts against stiffer, less compliant arteries, systolic and diastolic pressures increase and can result in a widening of the pulse pressure. In response, the left ventricular tends to hypertrophy. When excessive pulse pressure is transmitted through the microcirculation of vital organs such as the brain and kidneys, extensive tissue damage tends to occur.
An increase in pulse pressure can also be seen in a well-conditioned endurance runner 1. As he or she continues to exercise, the systolic pressure will progressively increase due to an increase in stroke volume and cardiac output. Diastolic pressure, on the contrary, will continually decrease due to a decrease in the total peripheral resistance. This is due to the accumulation of red (slow twitch) muscle tissue in the arterioles instead of white (fast twitch) tissue. As a result, the pulse pressure is going to increase. This can also be seen in individuals with larger amounts of muscle mass 17.
Other conditions — including severe iron deficiency (anemia) and an overactive thyroid (hyperthyroidism) — can increase pulse pressure as well.
Treating high blood pressure often reduces pulse pressure, although different medications may have varying impacts.
Wide pulse pressure causes
Wide pulse pressure can result from a variety of causes, with anemia being the most common.
Wide pulse pressure common causes
The most common cause of wide pulse pressure is anemia, other causes include:
- Aortic coarctation
- Aortic Regurgitation
- Arteriosclerosis of the aorta
- Arteriosclerosis of renal arteries
- Arteriovenous fistula
- Beriberi heart disease
- Cirrhosis
- Hyperthyroidism
- Pregnancy, particularly in the first trimester
- Isolated systolic hypertension
Narrow pulse pressure
A pulse pressure that is less than 25% of the systolic pressure is inappropriately low or “narrowed pulse pressure”. In aortic stenosis, there is a narrowing of the aortic valve which interferes with the ejection of blood from the left ventricle into the aorta, which results in a decrease in stroke volume and subsequent decrease in pulse pressure.
Significant blood loss, such as seen in trauma or acute hemorrhage, leads to a decrease in both the preload and stroke volume and subsequently a decrease in pulse pressure.
Narrow pulse pressure causes
Narrowed pulse pressure can be result from a variety of causes, with congestive heart failure being the most common.
Narrowed pulse pressure common causes:
- Ascites
- Congestive heart failure
- Constructive pericarditis
- Pericardial effusion
- Severe aortic stenosis
- Shock
- Tachycardia.
- Homan TD, Cichowski E. Physiology, Pulse Pressure. [Updated 2019 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482408
- Franklin SS, Gustin W 4th, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation 1997;96(1):308–15.
- Domanski MJ, Sutton-Tyrrell K, Mitchell GF, Faxon DP, Pitt B, Sopko G. Determinants and prognostic information provided by pulse pressure in patients with coronary artery disease undergoing revascularization. The Balloon Angioplasty Revascularization Investigation (BARI). Am J Cardiol 2001; 87(6):675–9.
- Kostis JB, Lawrence-Nelson J, Ranjan R, Wilson AC, Kostis WJ, Lacy CR. Association of increased pulse pressure with the development of heart failure in SHEP. Systolic Hypertension in the Elderly (SHEP) Cooperative Research Group. Am J Hypertens 2001;14(8 Pt 1):798–803.
- Blacher J, Staessen JA, Girerd X, et al. Pulse Pressure Not Mean Pressure Determines Cardiovascular Risk in Older Hypertensive Patients. Arch Intern Med. 2000;160(8):1085–1089. doi:10.1001/archinte.160.8.1085
- Mitchell GF, Vasan RS, Keyes MJ, et al. Pulse Pressure and Risk of New-Onset Atrial Fibrillation. JAMA. 2007;297(7):709–715. doi:10.1001/jama.297.7.709
- Anstey DE, Moise N, Kronish I, Abdalla M. Masked Hypertension: Whom and How to Screen? Curr. Hypertens. Rep. 2019 Apr 04;21(4):26.
- Benetos A, Rudnichi A, Safar M, et al. (1998) Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension 32:560–564.
- Fang J, Madhavan S, Cohen H, et al. (1995) Measures of blood pressure and myocardial infarction in treated hypertensive patients. J Hypertension 13:413–419.
- Khattar RS, Swales JD, Dore C, et al. (1999) Prediction of coronary and cerebrovascular morbidity and mortality by direct continuous ambulatory blood pressure monitoring in essential hypertension. Circulation 100:1071–1076.
- Franklin SS, Khan SA, Wong ND, et al. (1999) Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham heart study. Circulation 100:354–360.
- Lee ML, Rosner BA, Weiss ST. (1999) Relationship of blood pressure to cardiovascular death: the effects of pulse pressure in the elderly. Ann Epidemiol 9:101–107.
- KHATTAR RS, SWALES JD. Pulse pressure and prognosis. Heart 2001;85:484-486. http://dx.doi.org/10.1136/heart.85.5.484
- Thorin-Trescases N, Hayami D, Yu C, et al. Exercise Lowers Plasma Angiopoietin-Like 2 in Men with Post-Acute Coronary Syndrome. PLoS One. 2016;11(10):e0164598. Published 2016 Oct 13. doi:10.1371/journal.pone.0164598 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5063321
- Hormonal Therapy Increases Arterial Compliance inPostmenopausal Women. J Am Coll Cardiol 1997;30:350–6
- Plasma homocysteine concentration is increased in preeclampsia and is associated with evidence of endothelial activation. American Journal of Obstetrics and Gynecology Volume 179, Issue 6, Part 1, December 1998, Pages 1605-1611 https://doi.org/10.1016/S0002-9378(98)70033-X
- Rêgo ML, Cabral DA, Costa EC, Fontes EB. Physical Exercise for Individuals with Hypertension: It Is Time to Emphasize its Benefits on the Brain and Cognition. Clin Med Insights Cardiol. 2019;13:1179546819839411