Pyostomatitis vegetans
Pyostomatitis vegetans is a very rare benign oral disorder of unknown etiology characterized by pustules and vegetative lesions on an erythematous base that affect oral mucosa 1. Multiple white or yellow pustules on erythematous base may rupture lead to widespread ulceration and form folded, fissured appearance resembling a ‘snail trail’ appearance 2. The labial gingiva, soft and hard palate, buccal and labial mucosa are most commonly affected 3. Histopathology of gingival and tongue lesions showed a diffuse dermal and epidermal infiltrate with neutrophils and eosinophils, forming microabscesses. Tongue and floor of the mouth is rarely involved 4. Skin and other mucous membrane involvement may also be seen.
Pyostomatitis vegetans is a rare oral lesion which may affect any age group but it is commonest in young and middle aged adults between 20 and 59 years, with an average of 34 years and has a predilection for males with male to female ratio of 2:1 to 3:1 3. Pyostomatitis vegetans has strong association with inflammatory bowel disease (ulcerative colitis or Crohn’s disease) especially Crohn’s disease 5 and may be the first sign of it 1. Thus, a presumptive diagnosis of pyostomatitis vegetans should suggest a complete gastrointestinal investigation 3. The management of pyostomatitis vegetans is usually based on the management of underlying bowel disease.
The term pyostomatitis vegetans has long been a matter of great confusion. Several authors considered this disease as a mucosal variant of pyodermatitis vegetans and therefore both diseases would represent a single identity 3. This claim is corroborated by the finding of identical histological features and association with IBD (inflammatory bowel disease) for both conditions 6. Other authors identify the pyodermatitis vegetans as a variant of pemphigus vulgaris or pemphigus vegetans of Hallopeau. In support of this thesis there is the finding of clear suprabasal acantholysis, positivity both of direct immunofluorescence that reveals deposits of IgG and C3 in the intercellular spaces of the epider-mis and of indirect immunofluorescence that reveals circulating antiepithelial IgG antibodies 6. Thus, pyostomatitis and pyodermitis would be distinct conditions. Femiano et al 3 prefer distinguish between two different entities with identical clinical manifestations but with different pathogenesis: pyodermatitis vegetans as cutaneous variant of pyostomatitis vegetans and pyodermite vegetans or pemphigus vegetans of Hallopeau 7. The main difference between pyostomatitis vegetans and pemphigus vulgaris and pemphigus vegetans is the blistering nature of pemphigus. On the other hand, the association of pyostomatitis vegetans with inflammatory bowel disease (IBD) is another important differentiating feature. Considering histopathology of the lesions, the characteristic feature of pyostomatitis vegetans is intraepithelial abscesses filled with numerous eosinophils 8. Histopathologic findings in pemphigus vulgaris is suprabasal clefting, row of tombstone, acantholysis, and presence of Tzank cells 8. Pemphigus vegetans (Neumann type) showed intra-epidermal vesicles with suprabasal acantholysis without eosinophilic microabscesses. Hallopeau type pemphigus vegetans, showed eosinophilic spongiosis and microabscesses 3. Direct and indirect immunofluorescence in pemphigus is positive 9. Some authors believe that immunofluorescence is the only way to distinguish between pyostomatitis vegetans and pemphigus 3. But the others suggest that there is heterogeneity in the findings and the possibility of both false positive and false negative results must be considered 10.
One of the characteristic feature of pemphigus vegetans is tongue involvement with typical sulci and gyri pattern over the dorsum of the tongue called cerebriform tongue 11 and accepted as “Premalatha sign” 12. Conversely, in pyostomatitis vegetans tongue involvement is rare 4.
Nico et al. 9, reported a case of pyostomatitis vegetans with oral lesions and prolonged course of disease (several years) that never exacerbated into cutaneous lesions. This is unlike what usually occurs in non treated pemphigus. They suggested this finding as one of the issues while differentiating Pyostomatitis vegetans from pemphigus vegetans 9.
Consistently today’s the literature is inclined to believe that pyodermatitis-pyostomatitis vegetans is an identical entity belonging to the spectrum of chronic pustular dermatoses and that it must be differentiated from pemphigus vegetans of Hallopeau (first described as “pyodermite vegetans” ) even if the cutaneous lesions of both disease do not show significant clinical differences 13.
In fact, the association of pyodermite vegetans and ulcerative colitis has rarely been reported in literature 6, unlike pyodermatitis-pyostomatitis vegetans, which is strongly associated with inflammatory bowel diseases 14.
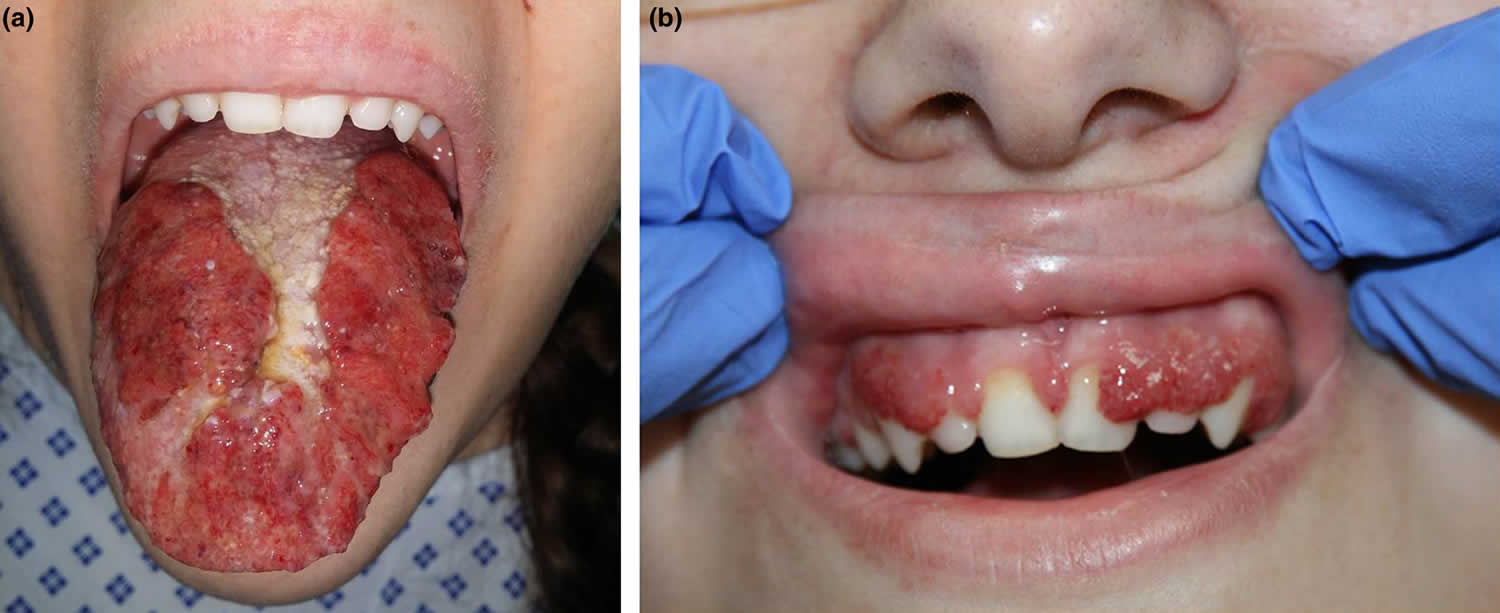
Figure 1. Pyostomatitis vegetans
Footnote: Multiple exophytic pustules on the erythematous base that covered the gingiva and oral mucosa resembling “snail tracks”.
Pyostomatitis vegetans causes
Pyostomatitis vegetans exact cause is unknown, although immunological and microbial factors have been suggested as possible etiological factors 15. Deposits of proteins in skin vessels in pyoderma gangrenosum lesions are suggestive of an Arthus-like reaction 16. Although some authors have considered microbial pathogenesis for this disease, no bacteria, fungi or viruses have been found in research 17.
Pyostomatitis vegetans differential diagnosis
The differential diagnosis of pyostomatitis vegetans includes blistering disease affecting the oral cavity such as pemphigus vegetans, pemphigus vulgaris and especially its rare variation pemphigus vegetans 3, bullous pemphigoid, erythema multiforme, herpes simplex and bullous drug eruption. However, clinically the presence of pustules with characteristic “snail track” ulcers and histopathological features of intraepithelial eosinophilic abscesses suggests pyostomatitis vegetans rather than other blistering diseases 3. The differential diagnosis should be established with Neumann type pemphigus vegetans since in both cases lesions are clinically similar and histology reveals an important eosinophil response, acanthosis and the formation of intraepithelial miliary microabscesses 18.
Pyostomatitis vegetans symptoms
Clinical presentation and distribution of the disease may vary among patients. Pyostomatitis vegetans is characterized by erythematous, thickened oral mucosa with multiple pustules and superficial erosions. A peripheral eosinophilia has been observed in most cases reported.
Oral mucosa is usually thickened and vegetating lesions on erythematous mucosa are seen. Multiple white to yellow pustules that often easily rupture and convert to erosive-ulcerative chronic lesions are usually observed. Granular appearance of oral mucosa, degeneration of vegetative pustules and erosive lesions always lead to a folded, fissured appearance named “snail tracks” 19.
All parts of the oral mucosa may be involved, but labial mucosa, attached gingiva, soft and hard palate and buccal mucosa are more commonly affected 20.
Cutaneous lesions are usually seen in the armpits, groin and scalp areas in an asymmetrical pattern. They present as crusted, erythematous papulo-pustules that extend peripherally and coalesce to form large vegetating plaques 21.
Oral lesions of pyostomatitis vegetans can be seen without skin lesions but it is rare for them to be present in the absence of gastrointestinal disturbances 22.
Pyostomatitis vegetans is associated with inflammatory bowel disease in 75% of cases 23. Inflammatory bowel disease (IBD) often appears months or years before oral and skin findings, sometimes the symptoms may be minimal and not sufficient to make an early diagnosis 5. In these cases the identification of pyostomatitis vegetans could represent a reason to encourage diagnostic investigations intended to reveal subclinical intestinal diseases 5.
Nigen in 2003 20 reported two patients with pyodermatitis-pyostomatitis vegetans. Both patients had lesions on the skin and mouth 20.
Leibovitch 24 also reported the first case of pyodermatitis-pyostomatitis vegetans in 2005 that involved the eyelid in addition to the skin and mouth.
If pyostomatitis vegetans is associated with pyodermatitis vegetans, cutaneous lesions are included of vesicopustular, vegetating plaques that are observed in 58% of patients 19.
Nigen 20 reported pseudoepitheliomatous hyperplasia in two cases with pyodermatitis-pyostomatitis vegetans. Deleporte 23 suggested that pyodermatitis-pyostomatitis vegetans belongs to the spectrum of neutrophilic dermatoses.
Pyostomatitis vegetans diagnosis
The diagnosis of pyostomatitis vegetans is based on clinical features (snail tracks appearance), presence of inflammatory bowel disease (ulcerative colitis or Crohn’s disease), peripheral eosinophilia, negative culture of pus from lesions and characteristic histological features (intraepithelial abscesses with large amount of eosinophils) 1. Direct and indirect immunofluorescence in pyostomatitis vegetans lesions is usually negative or may be weakly positive in direct immunofluorescence and the results are inconclusive 25.
Histopathological findings are similar in the skin and oral lesions. Epidermal hyperplasia is a constant feature in skin specimens. Focal acanthosis and hyperkeratosis may be seen in oral lesions. Intraepithelial and subepithelial microabscesses with abundant eosinophils and neutrophils are another finding in biopsy specimens 3. The inflammatory infiltrate shows a predominance of cytotoxic (CD3+/CD8+) lymphocytes 26. As the lesion matures there are fewer eosinophils 25. Viral, bacterial and fungal cultures of oral lesions of pyostomatitis vegetans are usually negative. Both direct and indirect immunofluorescence studies are usually negative 3.
Pyostomatitis vegetans treatment
Management of pyostomatitis vegetans is often based on treating the underlying gastrointestinal disease (ulcerative colitis or Crohn’s disease). The oral lesions can be managed with local therapies utilizing antiseptic mouthwashes such as chlorhexidine, and topical corticosteroids such as triamcinolone acetonide paste or betamethasone mouthwash. However, topical steroid therapy has limited success. Strategic treatment initially consists of systemic steroid therapy aimed at resolving and controlling the lesions 27. This therapy can be associated with azathioprine and sulfamethoxypyridazine that can be used for their steroid sparing effect. Dapsone has been effectively employed as a second line agent to control a relapse when steroid therapy has been halted or tapered down. Unfortunately, dapsone’s utility is limited by its side effects, which include hemolytic anemia, hepatitis, agranulocytosis, and the possibility of a drug mediated allergic reaction 28. A recent study declare that three injections of infliximab and successive maintenance therapy with methotrexate can cause a rapid and complete regression of both the pyostomatitis vegetans and the Crohn’s disease 29. Surgical treatment in severe IBD cases involves total colectomy and has resulted in permanent remission of symptoms 30.
References- Atarbashi-Moghadam S, Lotfi A, Atarbashi-Moghadam F. Pyostomatitis Vegetans: A Clue for Diagnosis of Silent Crohn’s Disease. J Clin Diagn Res. 2016;10(12):ZD12-ZD13. doi:10.7860/JCDR/2016/22573.9032 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5296587
- Saghafi S, Falaki F, Bashardoost N. Pyostomatitis vegetans: Report of a rare case. Pol J Pathol. 2011;62(2):125–28.
- Femiano F, Lanza A, Buonaiuto C, Perillo L, Dell’Ermo A, Cirillo N. Pyostomatitis vegetans: a review of the literature. Med Oral Patol Oral Cir Bucal. 2009 Mar 1;14(3):E114-7. http://www.medicinaoral.com/pubmed/medoralv14_i3_pE114.pdf
- Hegarty AM, Barrett AW, Scully C. Pyostomatitis vegetans. Clin Exp Dermatol. 2004;29(1):1–7.
- Hegarty AM, Barrett AW, Scullt C. Pyostomatitis vegetans. Clin Exp Dermatol 2004; 29: 1-7.
- Trost LB, McDonnell JK. Important cutaneous manifestations of inflammatory bowel disease. Postgrad Med J. 2005;81:580-5.
- O’Hagan AH, Irvine AD, Allen GE, Walsh M. Pyodermatitis-pyostomatitis vegetans: evidence for an entirely mucocutaneous variant. Br J Dermatol. 1998;139:552-3.
- Abellaneda C, Mascaro JM Jr, Vazquez MG, Pablo IM, Iranzo P. All that glitters is not pemphigus: Pyodermatitis-pyostomatitis vegetans misdiagnosed as IgA pemphigus for 8 years. The American Journal of Dermatopathology. 2011;33(1):e1–6.
- Nico MM, Hussein TP, Aoki V, Lourenco SV. Pyostomatitis vegetans and its relation to inflammatory bowel disease, pyoderma gangrenosum, pyodermatitis vegetans, and pemphigus. J Oral Pathol Med. 2012;41(8):584–88.
- Wolz MM, Camilleri MJ, McEvoy MT, Bruce AJ. Pemphigus vegetans variant of IgA pemphigus, a variant of IgA pemphigus and other autoimmune blistering disorders. The American Journal of Dermatopathology. 2013;35(3):e53–56.
- Rebello MS, Ramesh BM, Sukumar D, Alapatt GF. Cerebriform cutaneous lesions in pemphigus vegetans. Indian J Dermatol. 2016;61(2):206–08.
- Ganapati S. Eponymous dermatological signs in bullous dermatoses. Indian J Dermatol. 2014;59(1):21–23.
- Hegarty AM, Barrett AW, Scully C. Pyostomatitis vegetans. Clin Exp Dermatol. 2004;29:1-7.
- Markopoulos AK, Antoniades DZ, Zaraboukas T. Pemphigus vegetans of the oral cavity. Int J Dermatol. 2006;45:425-8.
- Saghafi S, Falaki F, Bashardoost N. Pyostomatitis vegetans: report of a rare case. Pol J Pathol. 2011;62(2):125-8. https://www.termedia.pl/Pyostomatitis-vegetans-report-of-a-rare-case,55,17120,1,1.html
- Su WP, Schroeter AL, Perry HO, Powell FC. Histopathologic and immunopathologic study of pyoderma gangrenosum. J Cutan Pathol 1986; 13: 323-330.
- Konstantopoulou M, O’Dwyer EM, Steele JC, et al. Pyodermatitis-pyostomatitis vegetans complicated by methicillin-resistant Staphylococcus aureus infection. Clin Exp Dermatol 2005; 30: 666-668.
- Ruiz-Roca JA, Berini-Aytes L, Gay-Escoda C. Pystomatitis vegetans. Report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol 2005; 99: 447-454.
- Ko HC, Jung DS, Jwa SW, et al. Two cases of pyodermatitis – pyostomatitis vegetans. J Dermatol 2009; 36: 293-297.
- Nigen S, Poulin Y, Rochette L, et al. Pyodermatitis-pyostomatitis vegetans: Two cases and a review of the literature. J Cutan Med Surg 2003; 7: 250-255.
- Harish K, Varghese T, Najeeba R, Harikumar R. Pyoderma vegetans and ulcerative colitis. J. Postgrad Med 2006; 52: 302-303.
- Bianchi L, Carrozzo AM, Orlandi A, Campione E, Hagman JH, Chimenti S. Pyoderma vegetans and ulcerative colitis. Br J Derma-tol. 2001;144:1224-7.
- Delaporte E, Viget N, Pasturel-Michon U, et al. Pyodermatitis-pyostomatitis vegetans uncovering a case of Crohn disease. Ann Dermatol Venereol 1998; 125: 331-334.
- Leibovitch I, Ooi C, Huilgol SC, et al. Pyodermatitis-pyostomatitis vegetans of the eyelids case report and review of the literature. Ophthalmology 2005; 112: 1809-1813.
- Markiewic M, Suresh L, Margarone J, et al. Pyostomatitis vegetans: a clinical marker of silent ulcerative colitis. J Oral Maxillofac Surg 2007; 65: 346-348.
- Ficarra G, Baroni G, Massi D. Pyostomatitis vegetans: cellular immune profile and expression of IL-6, IL-8 and TNF-alpha. Head Neck Pathol. 2010;4(1):1-9. doi:10.1007/s12105-009-0149-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2825530
- Trost LB, McDonnell JK. Important cutaneous manifestations of inflammatory bowel disease. Postgrad Med J 2005; 81: 580-585.
- Werchniak AE, Storm CA, Plunkett RW, Beutner EH, Dinulos JG. Treatment of pyostomatitis vegetans with topical tacrolimus. J Am Acad Dermatol. 2005;52:722-3.
- Bens G, Laharie D, Beylot-Barry M, Vergier B, Noblesse I, Bey-lot C, et al. Successful treatment with infliximab and methotrexate of pyostomatitis vegetans associated with Crohn’s disease. Br J Der-matol. 2003;149:181-4.
- Campisi G, Compilato D, Cirillo N, Ciavarella D, Panzarella V, Amato S, et al. Oral ulcers: three questions on their physiopathology. Minerva Stomatol. 2007;56:293-302.