Quadrilateral space syndrome
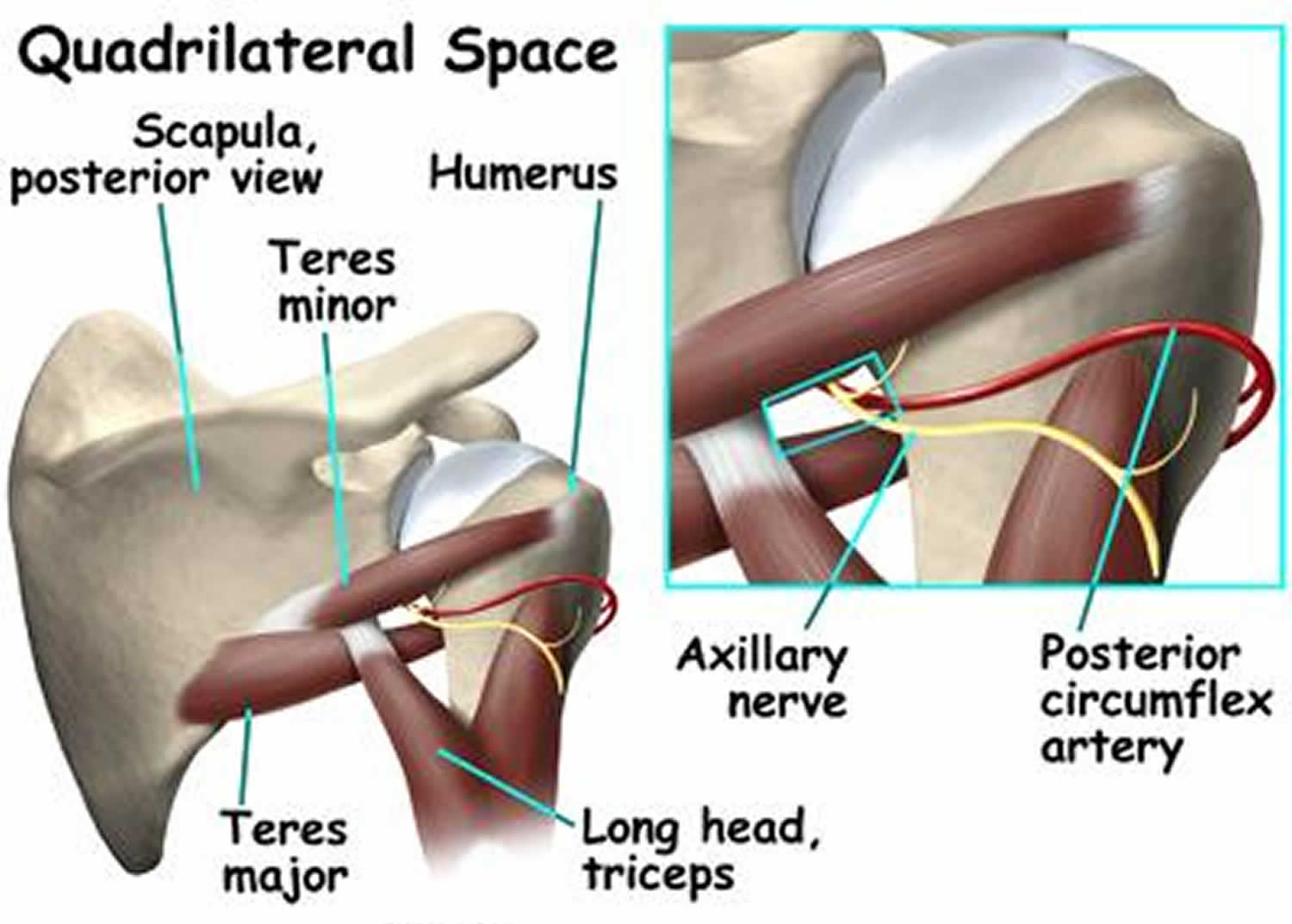
Quadrilateral space syndrome is a rare disorder characterized by compression of the axillary nerve and posterior humeral circumflex artery within the quadrilateral space 1. The quadrilateral space is located posterior and inferior to the glenohumeral joint and contains the axillary nerve and posterior humeral circumflex artery. The space is bounded superiorly by the teres minor muscle, inferiorly by the teres major muscle, medially by the long head of the triceps, and laterally by the humeral shaft.
Cahill and Palmer in 1983 2 originally described four distinct features of quadrilateral space syndrome: (1) diffuse pain around the shoulder; (2) paresthesia in a nondermatomal distribution; (3) point tenderness above the quadrilateral space; and (4) positive angiogram finding in provocative positioning. Quadrilateral space syndrome is commonly attributed to repeated overhead activity (such as baseball or volleyball athletes), but a variety of other pathologies including lipomas, hematomas, and labral cysts may cause compression in the quadrilateral space 3. Fibrous bands are most commonly implicated as the cause, with true space-occupying lesions being less common.
Quadrilateral space syndrome is characterized by intermittent insidious onset of poorly localized shoulder pain and paresthesia over the lateral aspect of the shoulder and arm in a nondermatomal pattern and at times present with deltoid and teres minor denervation 4. These symptoms are aggravated by shoulder abduction and external rotation. Point tenderness is typically present over the quadrilateral space; however, diagnosis on physical examination can be difficult. Pain relief after lidocaine block of the axillary nerve within the quadrilateral space is a useful finding in the evaluation of patients with suspected quadrilateral space syndrome. Diagnosis can be complicated by the presence of concurrent traumatic injuries, particularly in athletes. Since many other conditions (e.g., other musculoskeletal, vascular, or nerve-related syndromes in the area) can mimic quadrilateral space syndrome, it is often a diagnosis of exclusion. No definitive diagnostic imaging exists, although radiographs and magnetic resonance imaging are recommended to rule out other pathology. A review of the patient’s medical history may also be useful; particularly the absence of significant relief following attempted therapeutic interventions may be noted.
Diagnoses to rule out in the workup of quadrilateral space syndrome include rotator cuff injuries, referred pain syndromes, cervical spine pathologies, and labral injuries 5. Other important conditions that should be considered in the differential diagnosis include brachial plexus pathologies, such as thoracic outlet syndrome and brachial neuritis, glenohumeral joint arthritis, and suprascapular nerve injury 6. Fracture of the head of the humerus, anterior shoulder dislocation, and blunt trauma can all be sources of axillary nerve injury independent of axillary nerve compression. In one report, a patient presenting with quadrilateral space syndrome symptoms (shoulder pain and upper limb numbness when throwing) was ultimately found to have compression of the axillary nerve between the proximal humerus and the latissimus dorsi tendon 7. In this situation, the clinical complications can be identical, but the nerve compression occurs outside of the quadrilateral space.
Conservative treatment is often first trialed, including nonsteroidal anti-inflammatory drugs (NSAIDs), physical exercise modification, physical therapy for at least 6 months is recommended before pursuing operative intervention and therapeutic massage. In patients unrelieved by conservative measures, surgical decompression of the quadrilateral space may be indicated and has good outcomes, with resolution of pain and return to sport 3.
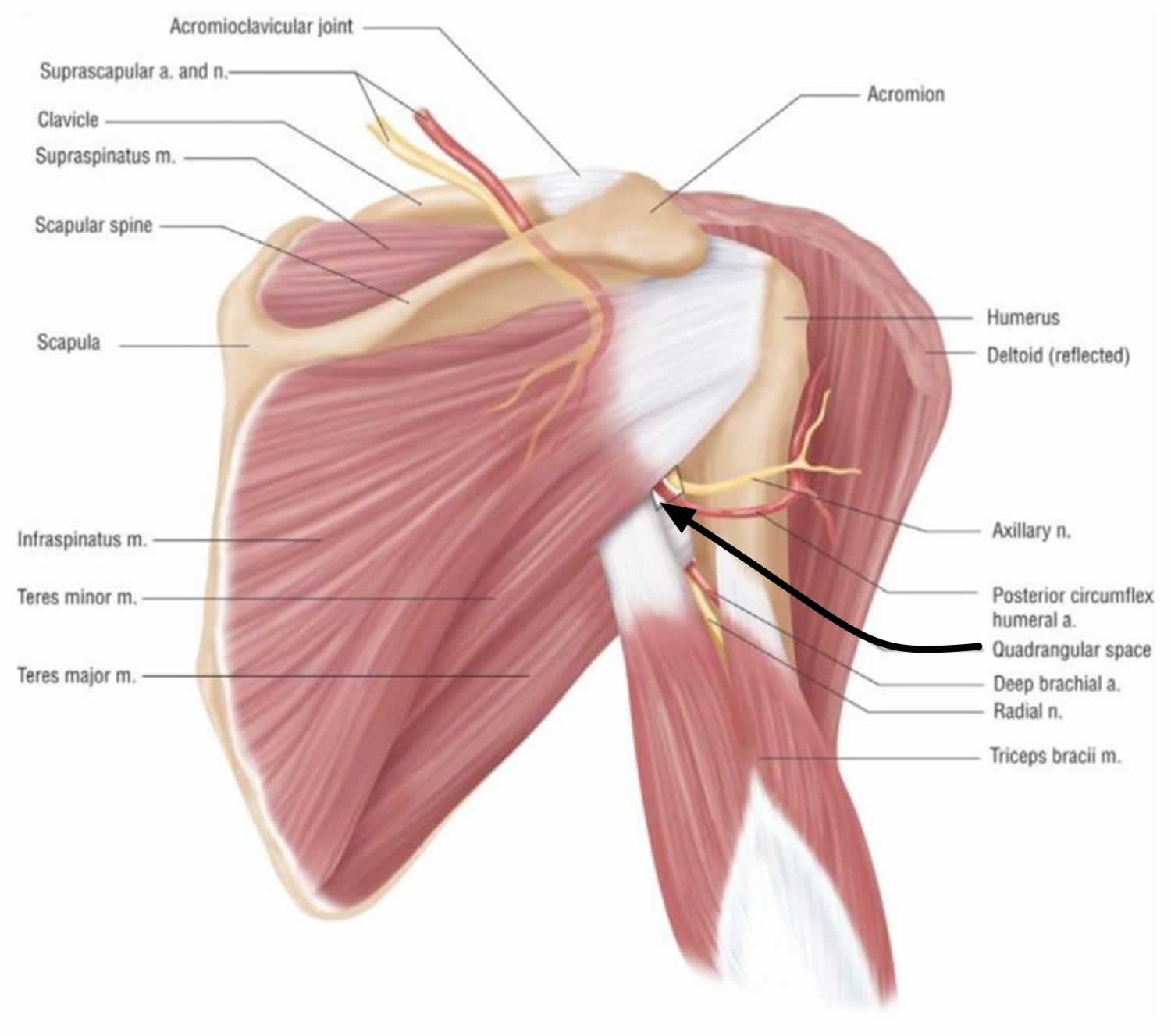
Quadrilateral space anatomy
The quadrilateral space is bounded superiorly by the teres minor muscle, inferiorly by the teres major muscle, medially by the long head of the triceps, and laterally by the humeral shaft (Figure 1) 6. The axillary nerve and posterior humeral circumflex artery reside in the quadrilateral space. The axillary nerve innervates the teres minor and deltoid muscles, which are primarily responsible for abduction and external rotation. Characteristic fibrous bands are found within the quadrilateral space, which exacerbate symptoms, particularly pain, elicited by movements associated with the deltoid and teres minor muscles 8. The anatomical differences in innervation patterns in the glenohumeral joint between patients can make it difficult to distinguish whether pain is due to suprascapular nerve palsy or axillary nerve compression 9. Because the posterior humeral circumflex artery stretches around the neck of the humerus, repetitive tension and mechanical stress to the posterior humeral circumflex artery wall can lead to thrombosis and aneurysmal degeneration 10.
Figure 1. Quadrilateral space anatomy
Footnote: Anatomy of the quadrilateral space. This posterior view of the right shoulder shows the quadrilateral space which is bounded superiorly by the teres minor muscle, inferiorly by the teres major muscle, medially by the long head of the triceps, and laterally by the humeral shaft.
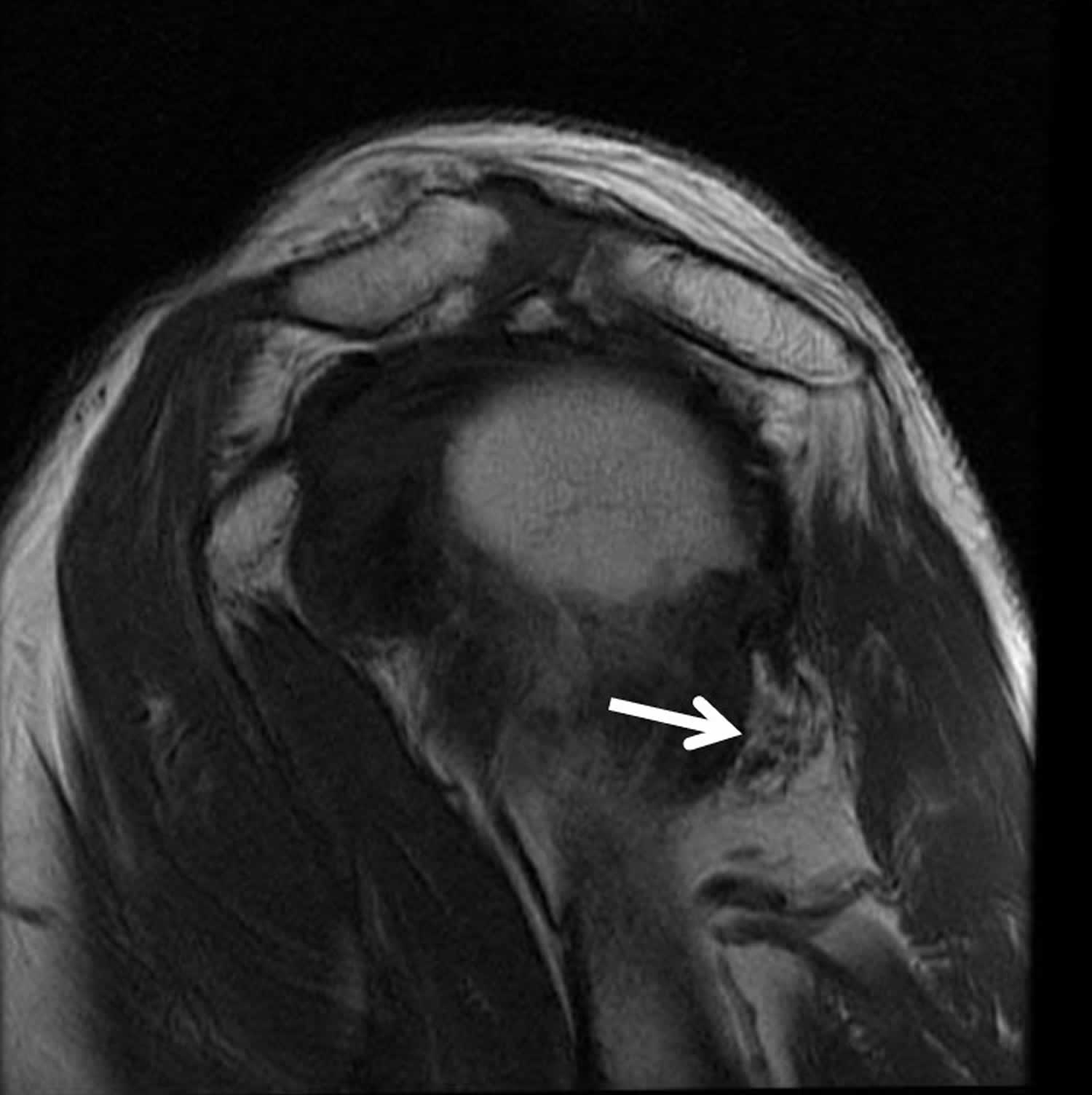
[Source 1 ]Figure 2. Quadrilateral space syndrome MRI image
Footnote: Atrophic left teres minor on magnetic resonance imaging (MRI) of shoulder in patient with quadrilateral space syndrome.
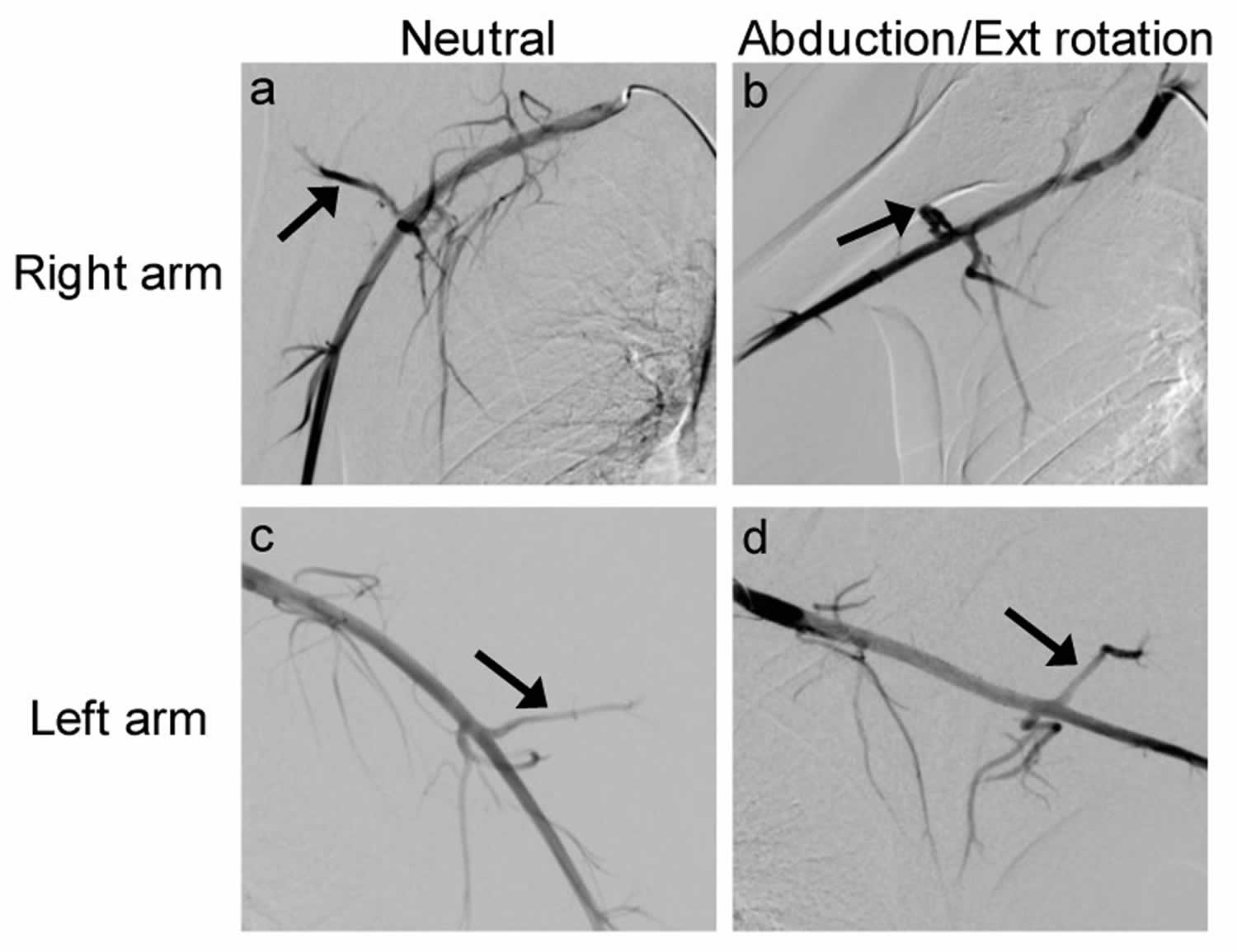
[Source 1 ]Figure 3. Quadrilateral space syndrome arteriography
Footnote: A 27-year-old right hand-dominant man presented with right shoulder pain and weakness, which had been nonresponsive to conservative measures. His pain was located in the right posterior shoulder with point tenderness directly over the quadrilateral space. This pain was aggravated by abduction and external and internal rotation. Following clinical examination, bilateral upper extremity arteriography was performed in neutral position and following provocative maneuvers. Bilateral provocative digital subtraction angiography of posterior humeral circumflex artery (posterior circumflex humoral artery) in patient with chronic right-sided shoulder pain. (a) Arrow pointing to normal flow of right posterior circumflex humoral artery with patient in neutral, supine position. (b) Arrow pointing to external compression of right posterior circumflex humoral artery following abduction and external (Ext) rotation of right shoulder. (c) Arrow pointing to normal flow of left posterior circumflex humoral artery with patient in neural, supine position. (d) Arrow pointing to normal flow of left posterior circumflex humoral artery following abduction and external rotation of left shoulder.
[Source 1 ]Quadrilateral space syndrome causes
The cause of quadrilateral space syndrome is unclear, but impingement is most frequently due to trauma, fibrous bands, or hypertrophy of a muscular border 1. In rare cases, quadrilateral space syndrome has also been caused by labral cysts, hematoma resulting from fracture, osteochondroma, lipomas, and axillary schwannomas. Compression of the axillary nerve can also follow aneurysms and traumatic pseudoaneurysms of the posterior circumflex humoral artery 11. Additionally, anatomical variations can predispose patients to quadrilateral space syndrome. For example, abnormal origin of the radial collateral artery from the posterior humeral circumflex artery, however rare, can also mimic the symptoms of quadrilateral space syndrome 12. In another case, the discovery of an accessory subscapularis muscle that originates from the anterior surface of the subscapularis, courses under the axillary nerve, and inserts onto the shoulder joint, can also serve as a rare risk factor for quadrilateral space syndrome 13. Quadrilateral space syndrome has also been described as a rare complication of thoracic surgery 14.
The typical causes of quadrilateral space syndrome are 1:
- Fibrous bands in the quadrilateral space, tightening in abduction and external rotation.
- Paralabral cysts, associated with inferior labral tears, especially in contact athletes.
- Very rarely: tumors (osteochondroma), muscular hypertrophy and hematomas
- Repetitive overuse or stress
- Poor training techniques.
Under those circumstances, cases of quadrilateral space syndrome in the literature commonly involve younger patients, less than forty years of age. Unlike Cahill’s original description of presenting symptoms, patients often present with vague complaints of pain without specifically localizing to the posterior shoulder, let alone directly overtop the quadrilateral space. Some patients may have their symptoms exacerbated with forward flexion or abduction and external rotation of the shoulder 4.
Quadrilateral space syndrome symptoms
Symptoms of quadrilateral space syndrome include:
- Vague shoulder pain (poorly localized pain of the posterior/lateral shoulder)
- often worse at night
- worse with overhead activity or late cocking/acceleration phase of throwing
- Numbness or tingling in the arm (paresthesia)
- Tenderness to pressure over the area
- Shoulder external rotation weakness
Quadrilateral space syndrome typically occurs in in young athletic adults with a history of repeated overhead activities, for example, in athletes of volleyball, baseball or swimming, in the age range of 25 to 35 years without a history of significant trauma. The pain is characterized clinically by a dull intermittent ache localized in the posterior and lateral shoulder. These symptoms are exacerbated by active and resisted abduction and external rotation of the humerus. Point tenderness is often present overlying the quadrilateral space posteriorly at the insertion site of the teres minor. Atrophy or weakness of the teres minor and deltoid muscle may also be noted. Paresthesias may occur in the cutaneous sensory distribution of the axillary nerve, overlying the deltoid muscle in the lateral shoulder and upper posterior arm.
Symptom presentation can be vague with involvement of neurogenic or vascular features. Neurogenic quadrilateral space syndrome is characterized by paresthesia, fasciculations, weakness, or neurogenic pain in a nonspecific pattern. Symptoms suggestive of vascular quadrilateral space syndrome include signs of acute ischemia (pain, pallor, absent pulses), thrombosis, or embolism (coolness or cyanosis of the hand or digits). In addition to vascular and neurogenic symptoms, patients with quadrilateral space syndrome can experience muscular atrophy and accompanying weakness, thought to be a result of denervation. Patients can also present with tenderness over the quadrilateral space. In severe cases, thrombosis of the posterior circumflex humoral artery can block flow from the axillary artery, causing embolization and subsequent cyanosis, digital ischemia, and cold intolerance 10.
Quadrilateral space syndrome diagnosis
The diagnosis of quadrilateral space syndrome can be difficult given its non-specific signs and symptoms and lack of a good diagnostic study and many patients with quadrilateral space syndrome are often diagnosed and treated for other conditions before the diagnosis is finally made 15. This can complicate the clinical picture. Often patients will have been misdiagnosed as impingement and had subacromial decompressions or other interventions.
In the workup of quadrilateral space syndrome, given the often vague patient presentation, imaging is important to both rule out and rule in quadrilateral space syndrome. Imaging of quadrilateral space syndrome can be challenging since compression of the axillary nerve may be intermittent, frequently due to positional dependence. Holding the arm in flexion, abduction, and external rotation for several minutes has been described as an effective method to reproduce symptoms and secure the diagnosis 16. When quadrilateral space syndrome is suspected, the diagnosis is often confirmed by imaging 5.
Imaging studies
- MRI scan – this will demonstrate the atrophy of teres minor (and rarely deltoid) and show any large paralabral cysts, tumors or hematomas.
- MR arthrogram – will demonstrate all the above, plus any associated labral lesions.
- Digital subtraction angiography to visualize posterior circumflex humoral artery occlusion.
Digital subtraction angiography, computed tomography angiography (CTA) and magnetic resonance angiography (MRA) have all been used to visualize posterior circumflex humoral artery occlusion 17. While there is no “gold standard” diagnostic test for quadrilateral space syndrome, magnetic resonance imaging (MRI) is typically the first choice of imaging 18. MRI often demonstrates focal fatty atrophy of the teres minor muscle and can exclude pathological causes of shoulder pain (see Figure 2) 18. Arteriography has been described as the cornerstone of diagnosis in quadrilateral space syndrome; it is used to reveal compression of the posterior circumflex humoral artery while the patient’s arm is in abduction and external rotation (Figure 3) 5. Bilateral upper extremity arteriography is useful in establishing the patient’s baseline healthy anatomy, as compared to the pathological shoulder. Decreased outflow from the posterior circumflex humoral artery would indicate compression of the adjacent axillary nerve leading to quadrilateral space syndrome 6. However, in one controlled study, 80% of asymptomatic controls demonstrated posterior circumflex humoral artery occlusion in arteriography, leading to low specificity 19.
A recent report described ultrasound diagnosis which demonstrated a dilated posterior circumflex humoral artery and mild atrophy of the deltoid muscle on the affected side 20. In another report, occlusion and stenosis of posterior circumflex humoral artery were detected using ultrasound 21. Although less common, teres minor atrophy can also be seen 22. Color Doppler sonography has also been used to compare differences in the posterior humeral circumflex arterial flow between neutral and provocative positions 23. Sonoelastography has also been used in the diagnosis of quadrilateral space syndrome secondary to axillary schwannoma 24. While no data exists regarding its superiority over traditional imaging methods using angiography, ultrasound offers a readily available, cheaper option to investigate quadrilateral space syndrome.
Others have described the potential usefulness of the electromyogram (EMG). EMG can detect denervation of muscles supplied by a compressed axillary nerve, such as the teres minor and deltoid muscles. However, the test has a high false-negative rate. In one study, four patients with established quadrilateral space syndrome underwent EMG and MRI testing. All four EMG scans were negative and half of the MRI scans were normal 25. While EMG can yield false negative results, it can still eliminate other etiologies of neuropathic pain, such as neurogenic thoracic outlet syndrome.
Quadrilateral space syndrome treatment
Owing to the fact that most literature on quadrilateral space syndrome is limited to case series and case reports, there continues to be much variability in the treatment of quadrilateral space syndrome 15. For minor symptoms, little weakness and no significant mass lesion on MRI scanning, conservative treatment is often trialed first, including nonsteroidal anti-inflammatory drugs (NSAIDs), physical exercise modification, physical therapy and functional strengthening can result in improvements over a few months. It is recommended at least 6 months of conservative measures are trialed before pursuing operative intervention 26. For significant weakness and functional disability, surgical decompression of the quadrilateral space may be indicated and has good outcomes, with resolution of pain and return to sport 3. Parlabral cysts can be approached arthroscopically and the associated labral tear repaired. Other large mass lesions require open surgical excision. In rare instances, quadrilateral space syndrome may spontaneously resolve 27.
Decompression has proven successful in reversing radial sensory neuropathy secondary to quadrilateral space syndrome 28. Since other conditions can mimic quadrilateral space syndrome, including effort thrombosis (also known as Paget–Schroetter syndrome) and arterial thoracic outlet syndrome, imaging and pertinent follow-up testing is essential before planning interventional decompression 29. Despite its lack of specificity, arteriography demonstrating compression of the posterior humeral circumflex artery and the accompanying presentation of classic quadrilateral space syndrome symptoms should raise a high index of suspicion for quadrilateral space syndrome and surgical decompression may be indicated. In surgical decompression, the axillary nerve is dissected free to ensure competency. During the procedure, the axillary nerve and posterior humeral circumflex artery can be palpated while the patient’s arm is placed in external rotation and abduction, to verify a freely gliding uncompressed nerve and a consistently strong pulse in the artery 30. It is also useful to check for fibrous bands around the neurovasculature, which may be indicative of structural compression 25. Postoperatively, patients can be placed in an arm sling for comfort with immediate physical therapy to avoid the development of adhesions. Physical therapy should be a central part to the postoperative recovery 25. Following successful operation, most athlete patients can return to their sport 31.
There are several other treatment modalities reported in literature, including thrombolysis in the setting of thrombus, thrombectomy in the setting of distal emboli formation, and aneurysm resection and endovascular treatment with coiling 32.
More recently, there is emerging reports of patients with quadrilateral space syndrome successfully treated with ultrasound-guided corticosteroid injection 33. This modality has the added benefit of quicker symptom relief. Chang et al. 33 have recently reported a case of quadrilateral space syndrome in a 42-year-old male weightlifter who presented symptoms consistent of quadrilateral space syndrome of a few weeks duration. MRI results demonstrated moderate atrophy and fatty infiltration of the teres minor. This patient was treated successfully with ultrasound-guided corticosteroid injections 33. Furthermore, Feng et al. 34 also reported a case of quadrilateral space syndrome in a 54-year-old female who presented with a six month history of progressive dull pain in her shoulder. Quadrilateral space syndrome with axillary nerve entrapment was suspected following an MRI. The patient reported immediate partial pain relief after an ultrasound-guided axillary nerve block using 2 mL 1% Xylocaine and later on reported greater than 50% pain reduction after a two-week follow-up 34. Fluoroscopic-guided procedures have the advantage over ultrasound in that typically they are easier and faster to perform, allow for more confident maintenance of a sterile field, and conclusive extravascular needle tip placement. The disadvantages include radiation exposure (albeit it an extremely low dose), and potentially less access to the modality.
Quadrilateral space syndrome prognosis
Successful appropriate treatment should result in full recovery. Case studies in the literature report full recovery within 3-6 months.
References- Hangge PT, Breen I, Albadawi H, Knuttinen MG, Naidu SG, Oklu R. Quadrilateral Space Syndrome: Diagnosis and Clinical Management. J Clin Med. 2018;7(4):86. Published 2018 Apr 21. doi:10.3390/jcm7040086 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5920460
- Cahill B.R., Palmer R.E. Quadrilateral space syndrome. J. Hand Surg. Am. 1983;8:65–69. doi: 10.1016/S0363-5023(83)80056-2
- Flynn LS, Wright TW, King JJ. Quadrilateral space syndrome: a review. J Shoulder Elbow Surg. 2018;27(5):950-956. doi:10.1016/j.jse.2017.10.024 https://doi.org/10.1016/j.jse.2017.10.024
- Flynn LS, Wright TW, King JJ. Quadrilateral space syndrome: a review. J Shoulder Elbow Surg. 2018;27(5):950-956. doi:10.1016/j.jse.2017.10.024
- Hoskins W.T., Pollard H.P., McDonald A.J. Quadrilateral space syndrome: A case study and review of the literature. Br. J. Sports Med. 2005;39:e9. doi: 10.1136/bjsm.2004.013367
- Cothran R.L., Helms C. Quadrilateral space syndrome: Incidence of imaging findings in a population referred for MRI of the shoulder. Am. J. Roentgenol. 2005;184:989–992. doi: 10.2214/ajr.184.3.01840989
- Koga R., Furushima K., Kusano H., Hamada J., Itoh Y. Quadrilateral space syndrome with involvement of the tendon of the latissimus dorsi. Orthopedics. 2017;40:e714–e716. doi: 10.3928/01477447-20170117-06
- McClelland D., Paxinos A. The anatomy of the quadrilateral space with reference to quadrilateral space syndrome. J. Shoulder Elbow Surg. 2008;17:162–164. doi: 10.1016/j.jse.2007.05.013
- Aszmann O.C., Dellon A.L., Birely B.T., McFarland E.G. Innervation of the human shoulder joint and its implications for surgery. Clin. Orthop. Relat. Res. 1996:202–207. doi: 10.1097/00003086-199609000-00027
- Brown S.A., Doolittle D.A., Bohanon C.J., Jayaraj A., Naidu S.G., Huettl E.A., Renfree K.J., Oderich G.S., Bjarnason H., Gloviczki P., et al. Quadrilateral space syndrome: The mayo clinic experience with a new classification system and case series. Mayo Clin. Proc. 2015;90:382–394. doi: 10.1016/j.mayocp.2014.12.012
- Cirpar M., Gudemez E., Cetik O., Uslu M., Eksioglu F. Quadrilateral space syndrome caused by a humeral osteochondroma: A case report and review of literature. HSS J. 2006;2:154–156. doi: 10.1007/s11420-006-9019-y
- Mohandas Rao K.G., Somayaji S.N., Ashwini L.S., Ravindra S., Abhinitha P., Rao A., Sapna M., Jyothsna P. Variant course of posterior circumflex humeral artery associated with the abnormal origin of radial collateral artery: Could it mimic the quadrangular space syndrome? Acta Med. Iran. 2012;50:572–576.
- Pires L.A.S., Souza C.F.C., Teixeira A.R., Leite T.F.O., Babinski M.A., Chagas C.A.A. Accessory subscapularis muscle—A forgotten variation? Morphologie. 2017;101:101–104. doi: 10.1016/j.morpho.2017.04.003
- Nishimura M., Kobayashi M., Hamagashira K., Noumi S., Ito K., Kato D., Shimada J. Quadrilateral space syndrome: A rare complication of thoracic surgery. Ann. Thorac. Surg. 2008;86:1350–1351. doi: 10.1016/j.athoracsur.2008.02.039
- Bourget-Murray J, Davison E, Frizzell B, LeBlanc J. Fluoroscopic-guided quadrilateral space block for the treatment of quadrilateral space syndrome – A case report. J Clin Orthop Trauma. 2019;10(4):655-658. doi:10.1016/j.jcot.2019.03.011 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6612044
- Aval S.M., Durand P., Jr., Shankwiler J.A. Neurovascular injuries to the athlete’s shoulder: Part II. J. Am. Acad. Orthop. Surg. 2007;15:281–289. doi: 10.5435/00124635-200705000-00006
- Chautems R.C., Glauser T., Waeber-Fey M.C., Rostan O., Barraud G.E. Quadrilateral space syndrome: Case report and review of the literature. Ann. Vasc. Surg. 2000;14:673–676. doi: 10.1007/s100169910120
- Chen H., Narvaez V.R. Ultrasound-guided quadrilateral space block for the diagnosis of quadrilateral syndrome. Case Rep. Orthop. 2015;2015:378627. doi: 10.1155/2015/378627
- Mochizuki T., Isoda H., Masui T., Ohkawa Y., Takahashi M., Takehara Y., Ichijo K., Kodaira N., Kitanaka H. Occlusion of the posterior humeral circumflex artery: Detection with MR angiography in healthy volunteers and in a patient with quadrilateral space syndrome. AJR Am. J. Roentgenol. 1994;163:625–627. doi: 10.2214/ajr.163.3.8079857
- Feng S.-H., Hsiao M.-Y., Wu C.-H., Özçakar L. Ultrasound-guided diagnosis and management for quadrilateral space syndrome. Pain Med. 2017;18:184–186. doi: 10.1093/pm/pnw256
- Robinson P., White L.M., Lax M., Salonen D., Bell R.S. Quadrilateral space syndrome caused by glenoid labral cyst. AJR Am. J. Roentgenol. 2000;175:1103–1105. doi: 10.2214/ajr.175.4.1751103
- Lopez Ovenza J.M., Ranalletta M., Alonso Hidalgo I., Tanoira I., Bongiovanni S., Maignon G. Quadrilateral space syndrome with compromise of the teres minor muscle. Medicina. 2011;71:49.
- Brestas P.S., Tsouroulas M., Nikolakopoulou Z., Malagari K., Drossos C. Ultrasound findings of teres minor denervation in suspected quadrilateral space syndrome. J. Clin. Ultrasound. 2006;34:343–347. doi: 10.1002/jcu.20239
- Hung C.Y., Chang K.V., Chen P.T., Ho Y.T., Han D.S., Chen W.S., Wang T.G. Sonoelastography for the evaluation of an axillary schwannoma in a case of quadrilateral space syndrome. Clin. Imaging. 2014;38:360–363. doi: 10.1016/j.clinimag.2013.12.019
- McAdams T.R., Dillingham M.F. Surgical decompression of the quadrilateral space in overhead athletes. Am. J. Sports Med. 2008;36:528–532. doi: 10.1177/0363546507309675
- Manske R.C., Sumler A., Runge J. Quadrilateral space syndrome. Hum. Kinet. 2009;14:45–47. doi: 10.1123/att.14.2.45
- Gregory T., Sangha H., Bleakney R. Spontaneous resolution of quadrilateral space syndrome: A case report. Am. J. Phys. Med. Rehabil. 2015;94:e1–e5. doi: 10.1097/PHM.0000000000000237
- Brown D.L., Chung K.C. Quadrangular space syndrome associated with superficial radial sensory neuropathy. Ann. Plast. Surg. 1999;43:207–210.
- Hangge P., Rotellini-Coltvet L., Deipolyi A.R., Albadawi H., Oklu R. Paget-schroetter syndrome: Treatment of venous thrombosis and outcomes. Cardiovasc. Diagn. Ther. 2017;7:S285–S290. doi: 10.21037/cdt.2017.08.15
- Francel T.J., Dellon A.L., Campbell J.N. Quadrilateral space syndrome: Diagnosis and operative decompression technique. Plast. Reconstr. Surg. 1991;87:911–916. doi: 10.1097/00006534-199105000-00016
- Van de Pol D., Kuijer P.P., Langenhorst T., Maas M. High prevalence of self-reported symptoms of digital ischemia in elite male volleyball players in the Netherlands: A cross-sectional national survey. Am. J. Sports Med. 2012;40:2296–2302. doi: 10.1177/0363546512456973
- Duwayri Y.M., Emery V.B., Driskill M.R., Earley J.A., Wright R.W., Paletta G.A., Jr., Thompson R.W. Positional compression of the axillary artery causing upper extremity thrombosis and embolism in the elite overhead throwing athlete. J. Vasc. Surg. 2011;53:1329–1340. doi: 10.1016/j.jvs.2010.11.031
- Chang P.S., Jacobson N., Chang K.U. Quadrilateral space syndrome treated with ultrasound-guided corticosteroid injection: a case of isolated teres minor atrophy and review of the literature. S. D. Med. 2017 Oct;70(10):444–447.
- Feng S.H., Hsiao M.Y., Wu C.H. Ultrasound-guided diagnosis and management for quadrilateral space syndrome. Pain Med. 2017 Jan 1;18(1):184–186.