Raccoon eyes
Raccoon eyes also known as bruising around the eyes or periorbital hematoma or periorbital bruising (ecchymosis) with tarsal plate sparing, is a sign of basal skull fracture. Raccoon eyes results from blood from skull fracture tracking down into the soft tissue around the eye. Raccoon eyes may also be referred to as panda eyes, especially in the UK. Raccoon eyes may also be a sign of disseminated neuroblastoma. The clinical triad comprising of unilateral or bilateral progressive proptosis, periorbital ecchymosis, and edema is called raccoon sign 1. Basal skull fractures are most commonly seen in younger people due to their propensity to do high-risk activities. The majority of basal skull fractures are managed with conservative care 2. However, conditions potentially associated with basal skull fracture that may require specific management include traumatic aneurysms, posttraumatic carotid-cavernous fistula, cerebrospinal fluid fistula, meningitis, cerebral abscess, cosmetic deformities and posttraumatic facial palsy.
Basal skull fractures, usually caused by substantial blunt force trauma, involve at least one of the bones that compose the base of the skull 3. Most basal skull fractures are caused by high-velocity blunt trauma such as motor vehicle collisions, motorcycle crashes, and pedestrian injuries. Falls and assaults are also important causes. Penetrating injuries such as gunshot wounds account for less than 10% of cases 4.
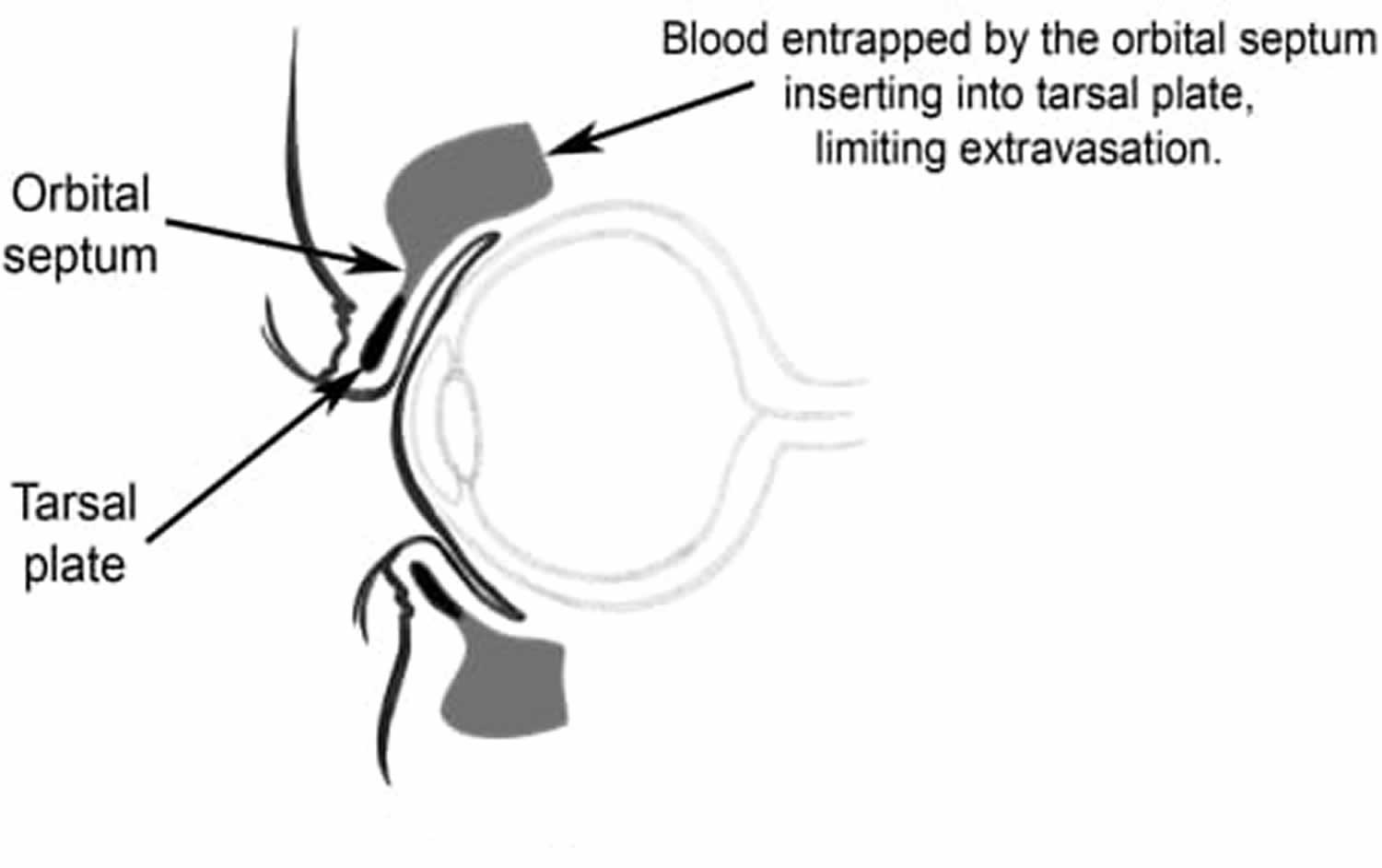
Basal skull fracture most commonly involve the temporal bones but may involve the occipital, sphenoid, ethmoid and the orbital plate of the frontal bone as well. Basal skull fracture are often missed on CT and plain skull x-rays. Clinical signs are usually more sensitive 2. Signs of basal skull fracture may take several hours to develop and include cerebrospinal fluid (CSF) otorrhea or rhinorrhea, hemotympanum, laceration of the external auditory canal, Battle’s sign (postauricular or mastoid ecchymosis) and periorbital ecchymosis with tarsal plate sparing (Raccoon eyes). Battle’s sign and unilateral blepharohematoma have the highest predictive value 5. Tarsal plate sparing is due to an anatomic structure called the orbital septum, which limits extravasation of blood beyond the tarsal plate (Figure 2). Indirect radiographic findings that suggest basal skull fracture include pneumocephalus and air-fluid levels within, or opacification of, an air sinus. Basilar skull fractures are commonly associated with facial fractures, cervical spine injury, intracranial hemorrhage, cranial nerve injury, vascular injury, and meningitis 6.
Figure 1. Raccoon eyes
Footnote: Photograph of patient with raccoon eyes. Note the tarsal plate sparing.
[Source 7 ]Figure 2. Racoon eyes tarsal plate sparing
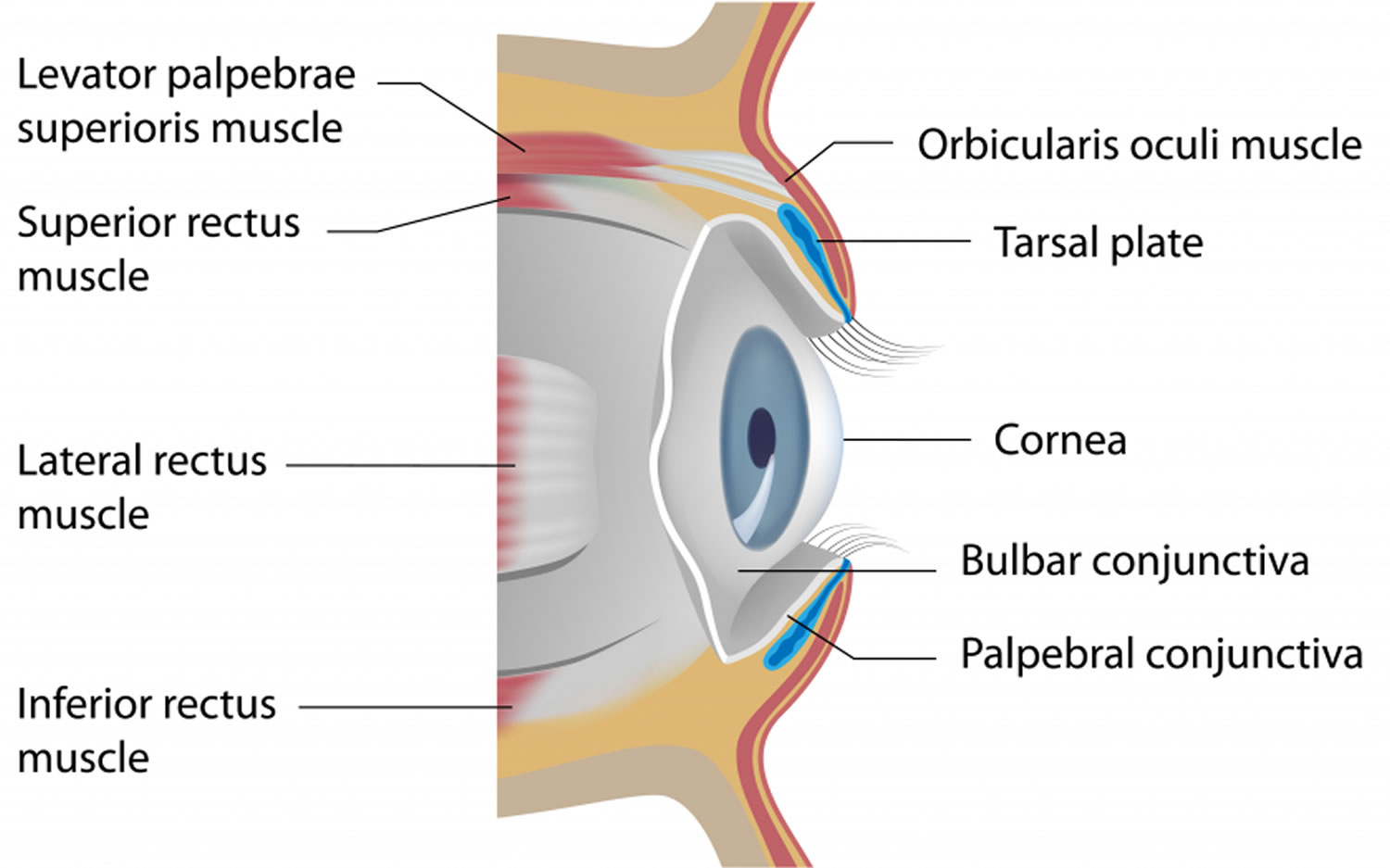
[Source 7 ]Figure 3. Eyelid anatomy
Racoon eyes causes
Although commonly associated with skull base fracture, raccoon eye sign may also present in a variety of other conditions (limited to case reports), which include:
- Traumatic: unilateral and bilateral orbital fractures 8:
- Minor periorbital trauma, like the plucking of eyebrows
- Non-accidental injuries
- Thoracic trauma and crush injuries
- Following vigorous sneezing, coughing or vomiting – probably due to periorbital venous hemorrhage
- Posttraumatic orbital emphysema (due to fracture of orbital wall and entrapment of air from paranasal sinuses)
- Vascular 9:
- Subarachnoid hemorrhage (SAH) from ophthalmic artery aneurysm
- Sinus thrombosis – dural, superior sagittal sinus, and cavernous sinus thrombosis
- Giant cell arteritis
- Trigeminal autonomic cephalalgia
- Benign intracranial hypertension
- Acute migraine (due to vasodilation and release of vasoactive substances including heparin)
- Infectious 10:
- Severe pediatric adenovirus infection
- Periorbital leukoderma
- Frontal sinus mucocele
- Immune-mediated 11:
- The neonatal lupus erythematosus (vasculitis may lead to facial and periorbital purplish-red plaques)
- Chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature (CANDLE) syndrome (neutrophilia and skin lesions containing mature neutrophils may also cause raccoon eyes appearance due to periorbital erythematous edema; due to a predilection to involve periorbital skin)
- Lichen planus pigmentosus (hyperpigmentation due to pigment incontinence)
- Sweet syndrome or acute febrile neutrophilic dermatosis is a skin disease characterized by the sudden onset of fever, an elevated white blood cell count, and tender, red, well-demarcated papules, and plaques that show dense infiltrates by neutrophil granulocytes on histologic examination
- Raccoon sign in this condition is due to secondary vascular damage caused by prolonged exposure to matrix metalloproteinases
- Toxic products of neutrophils in the infiltrate may be responsible for vascular damage leading to erythrocyte extravasation
- Metabolic 12:
- Amyloidosis (most commonly, light chain (AL) type) – due to increased vascular fragility as a result of amyloid deposition – this is one of the most common causes of raccoon eyes other than trauma; the finding presents in about one-fifth of patients with AL amyloidosis
- Myxedema
- Malignancies 13:
- Hematological malignancies: blastic plasmacytoid dendritic cell neoplasm, lymphoblastic lymphoma, acute myeloid leukemia
- Metastatic neuroblastoma (secondary to tumoral obstruction of the palpebral vessels): neuroblastoma can present as periorbital ecchymosis in 5.4% of cases
- Orbital metastasis of solid malignancies
- Kaposi sarcoma
- Multiple myelomas: Infiltration of amyloid proteins in the capillaries lead to increased fragility, which can burst under minor stress, resulting in raccoon sign – usually, such an ecchymosis is painful in multiple myeloma
- Genetic:
- Hemophilia
- Iatrogenic (perioperative raccoon eyes) 14:
- Usually associated with systemic amyloidosis of AL type .
- Post-rhinoplasty (due to a bleeding disorder)
- Post-endoscopic retrograde cholangiopancreatography (ERCP) (prone positioning, consumption of steroid and Valsalva maneuver might cause increased venous pressure which in turn lead to the rupture of fragile vessels in the orbit of an elderly patient)
Racoon eyes sign
The pooling of blood around the eyes is most commonly associated with fractures of the anterior cranial fossa. This finding is typically not present during the initial evaluation and delays by 1 to 3 days 6. If bilateral, this finding is highly predictive of a basilar skull fracture. Classically, the tarsal plate will be spared. Further extravasation of the blood beyond the periorbital region is limited owing to the orbital septum inserting into the tarsal plate 15.
When a skull base fracture is present, the raccoon sign is present in 50 to 60% of cases 16. This sign can be easily identified and is usually associated with anterior skull base fractures, especially of the frontal bone with an associated epidural hematoma. Thin-cuts computed tomogram of the skull (less than 5 mm) is needed to identify the fracture in some cases.
If the racoon eyes sign is present in a trauma victim, one should be aware of the following associated injuries or complications:
- Cerebrospinal fluid (CSF) rhinorrhea
- Injury to eyeballs
- Injury to cranial nerves I, II III, IV, VI, VII and VIII
- Intracranial misplacement of the nasogastric or nasotracheal tube
- Diffuse axonal injury
- Insult to the hypothalamic-pituitary axis (HPA) leading to endocrinopathies
- Maxillofacial injuries
- Cervical spine injury
- Meningitis, at a later stage.
Raccoon eyes complications
Raccoon eyes complications include:
- CSF leak
- Meningitis
- Cranial nerve palsies (cranial nerves I, II III, IV, VI, VII and VIII)
- Hearing loss
- Cavernous sinus thrombosis
- Vertigo
- Intracranial hemorrhage
- Death
The majority of CSF leaks resolve spontaneously within 5-10 days but some can persist for months. Meningitis may occur in less than 5% of patients but the risk increases with the duration of the CSF leak.
Conductive hearing loss usually resolves within 7-21 days.
Cranial nerve deficits involve loss of smell and facial palsy.
Basilar skull fractures can also be associated with a vascular injury resulting in occlusion, fistula formation, bleeding, or pseudoaneurysm formation.
Raccoon eyes diagnosis
The diagnosis may be obvious on a physical exam in some cases. Plain x-rays are not sensitive to detect basal skull fracture.
The initial evaluation is usually via a non-contrast computed tomography (CT) scan. Unfortunately, skull-based fractures that are linear or non-displaced may be difficult to detect. In patients where a high clinical suspicion for basilar skull fracture exists, multidetector CT (MDCT) thin-slice scanning through the face and skull base may aid in the detection of more subtle fractures. Conversely, the detailed small neural and vascular channels visualized on MDCT may be misread as fractures. Pneumocephalus should raise the suspicion for a basilar skull fracture. Further imaging with CT angiography and venography (CTA, CTV) to assess for vascular injury should be considered in the acute setting. MRI may be useful in assessing nerve injury and in evaluating for a cerebrospinal fluid leak 17.
CSF leak is not easy to diagnose and the fluid should be sent for analysis of beta transferrin.
Raccoon eyes treatment
Raccoon eyes treatment involves treating the underlying cause. Raccoon eyes by itself usually resolves within 2 to 3 weeks.
Patients with basal skull fractures require admission for observation. Those taking anticoagulants should be admitted to a facility with immediate neurosurgical capabilities and the ability to do frequent assessments of the neurologic decline, even if no hemorrhage is present on initial imaging. Patients with intracranial hemorrhage require emergent neurosurgical evaluation. Otherwise, skull base fractures are often managed expectantly. Surgical management is necessary for cases complicated by intracranial bleeding requiring decompression, vascular injury, significant cranial nerve injury, or persistent cerebrospinal fluid leak. One should avoid inserting a nasogastric tube in such patients as intracranial placement of the tube may occur accidentally. It is better to place the orogastric tube instead, if necessary. In addition, nasal intermittent positive pressure ventilation (NIPPV) should be avoided as it may induce pneumocephalus 3.
Basal skull fractures increase the risk of meningitis because of the increased possibility of bacteria from the paranasal sinuses, nasopharynx, and the ear canal making direct contact with the central nervous system. Patients with associated cerebrospinal fluid leaks, present in up to 45% of patients with basal skull fractures, are often treated with prophylactic antibiotics to prevent meningitis, but there is no good evidence to support this practice. A recent Cochrane review did not find sufficient evidence to recommend prophylactic antibiotics in patients with basal skull fractures even in the presence of documented cerebrospinal fluid leak. However, patients with persistent leaks should have cerebrospinal fluid cultures to guide antibiotic therapy, and patients with clinical presentations consistent with meningitis should be treated with empiric antibiotics until culture results are available. While prophylactic antibiotics are not indicated generally, use is still considered appropriate for coverage related to procedures such as insertion of intracranial pressure (ICP) monitor. Persistent leaks require neurosurgical intervention. Less invasive, endoscopic techniques are becoming common with fewer of these injuries requiring open repair 18.
Raccoon eyes prognosis
The outcome of patients with basal skull fractures depends on whether the fracture is displaced. For nondisplaced fractures, the management is conservative and the outcomes are good. However, for those with displaced fractures, intervention may be required and this also carries a risk of surgical complications. The key morbidity is meningitis which can be lethal. Those who have a dissection of the carotid artery can develop life-threatening bleeding. Overall, most patients with basilar skull fracture do have some type of residual functional or neurological deficit which may take months or even years to reverse 19.
References- Timmerman R. Images in clinical medicine. Raccoon eyes and neuroblastoma. N. Engl. J. Med. 2003 Jul 24;349(4):e4.
- Mark S. Handbook of Neurosurgery. New York, NY: Thieme; 2006. Greenberg.
- Simon LV, Newton EJ. Basilar Skull Fractures. [Updated 2019 Nov 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470175
- Wang H, Zhou Y, Liu J, Ou L, Han J, Xiang L. Traumatic skull fractures in children and adolescents: A retrospective observational study. Injury. 2018 Feb;49(2):219-225.
- Pretto FL, De Almeida CS, Casulari LA. Positive predictive values of selected clinical signs associated with skull base fractures. J of Neurosurgical Sciences. 2000;44:77–82.
- Solai CA, Domingues CA, Nogueira LS, de Sousa RMC. Clinical Signs of Basilar Skull Fracture and Their Predictive Value in Diagnosis of This Injury. J Trauma Nurs. 2018 Sep/Oct;25(5):301-306.
- Raccoon Eyes. https://westjem.com/articles/raccoon-eyes.html
- Satyarthee GD, Sharma BS. Posttraumatic orbital emphysema in a 7-year-old girl associated with bilateral raccoon eyes: Revisit of rare clinical emergency, with potential for rapid visual deterioration. J Pediatr Neurosci. 2015 Apr-Jun;10(2):166-8.
- Aalbers M, van Dijk JMC. Teaching NeuroImages: Raccoon eye in subarachnoid hemorrhage. Neurology. 2019 Mar 26;92(13):e1534-e1535.
- Mehta AA, Wagner LH, Blace N. Spontaneous upper eyelid ecchymosis: A rare presenting sign for frontal sinus mucocele. Orbit. 2017 Jun;36(3):183-187.
- Law DZ, Vahdani K, Ashdown M, Garrott H, Ford RL. Periorbital linear lichen planus pigmentosus-report of 2 cases and literature review. Can. J. Ophthalmol. 2019 Feb;54(1):e12-e14.
- Matsuura H, Anzai Y, Kuninaga N, Maeda T. Raccoon Eye Appearance: Amyloidosis. Am. J. Med. 2018 Jul;131(7):e305.
- Inokuchi R, Tagami S, Maehara H. An elderly woman with bilateral raccoon eyes. Emerg Med J. 2016 Nov;33(11):781.
- Nasiri J, Zamani F. Periorbital Ecchymosis (Raccoon Eye) and Orbital Hematoma following Endoscopic Retrograde Cholangiopancreatography. Case Rep Gastroenterol. 2017 Jan-Apr;11(1):134-141.
- McPheeters RA, White S, Winter A. Raccoon eyes. West J Emerg Med. 2010 Feb;11(1):97.
- Herbella FA, Mudo M, Delmonti C, Braga FM, Del Grande JC. ‘Raccoon eyes’ (periorbital haematoma) as a sign of skull base fracture. Injury. 2001 Dec;32(10):745-7.
- Johnston JJ. The Galasko report implemented: the role of emergency medicine in the management of head injuries. Eur J Emerg Med. 2007 Jun;14(3):130-3.
- Lin DT, Lin AC. Surgical treatment of traumatic injuries of the cranial base. Otolaryngol. Clin. North Am. 2013 Oct;46(5):749-57.
- Leibu S, Rosenthal G, Shoshan Y, Benifla M. Clinical Significance of Long-Term Follow-Up of Children with Posttraumatic Skull Base Fracture. World Neurosurg. 2017 Jul;103:315-321.