Radiation cystitis
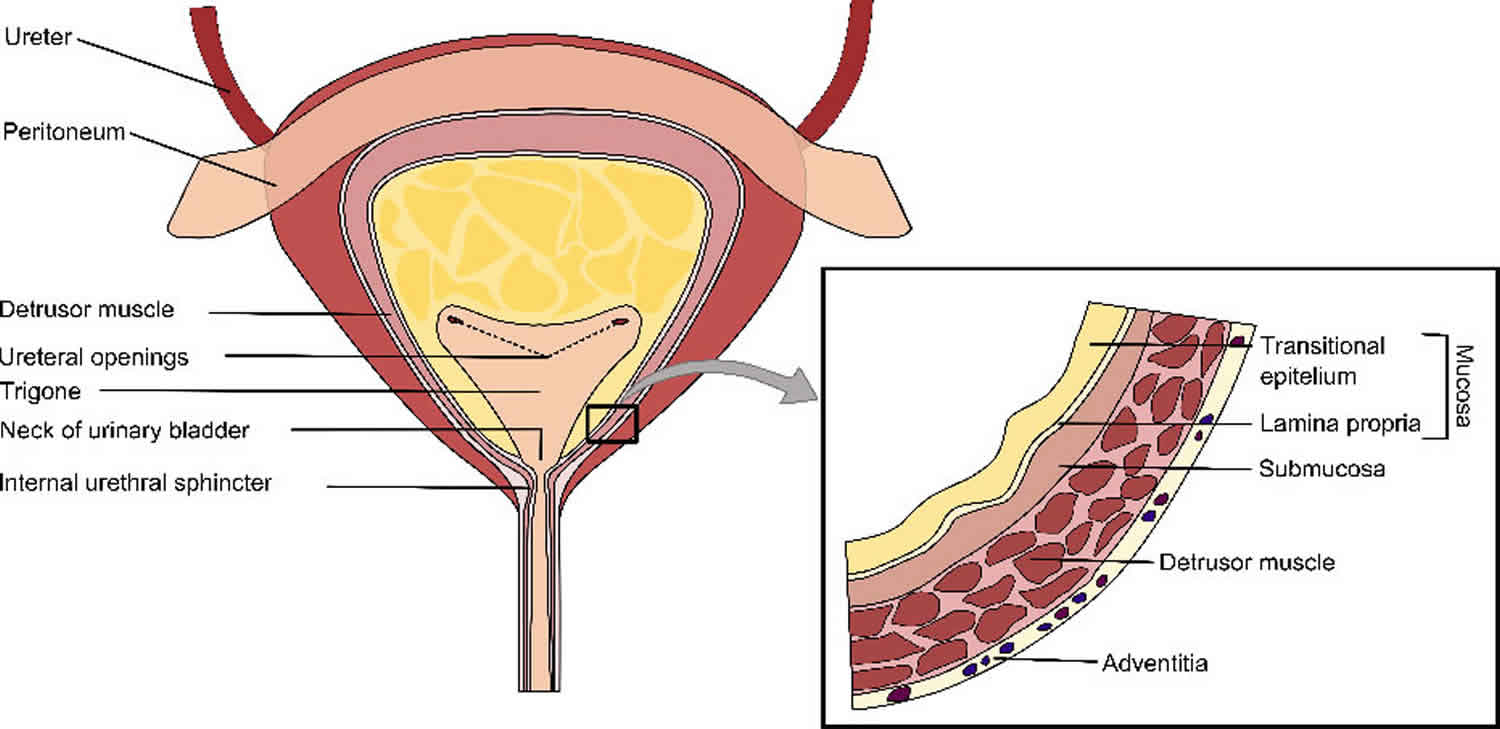
Radiation cystitis is a medical term to describe the side effect of inflammation and subsequent destruction to the normal anatomy of the urinary bladder at the cellular level after the use of radiation in the treatment of multiple cancer types, including, most commonly, pelvic cancers. The urinary bladder can be irradiated intentionally for the treatment of bladder cancer or incidentally for the treatment of other pelvic malignancies. Manifestations of radiation cystitis can range from minor, temporary, irritative voiding symptoms and painless, microscopic hematuria to more severe complications, such as gross hematuria; contracted, nonfunctional bladder; persistent incontinence; fistula formation; necrosis; and death.
Radiation therapy can be used for primary bladder cancer as well as for tumors in many organs surrounding the bladder, such as the colon, rectum, ovaries, uterus, and prostate. When the primary tumor is not located in the bladder, this leads to unintentional radiation exposure to the healthy bladder tissue.
Damage from the treatment can either be acute (less than six months from radiation therapy completion) or delayed (more than six months after treatment) and can have varying levels of irritation and functional impairment to the bladder mucosa. If on the mild end of the spectrum, symptoms may include increased frequency, urgency, and possibly some dysuria. Infection should be ruled out with a urinalysis which may show microscopic hematuria. These symptoms can resolve over time.
On the other end of the spectrum, patient’s may experience symptoms such as urinary incontinence, gross hematuria, and progression of damage to the extent of fistula formation or necrotic bladder tissue. The treatment varies on the degree of symptoms. Overall, radiation cystitis can be detrimental to a patient’s wellbeing after already having gone through a great deal in regards to cancer treatment. Health care providers are becoming more aware of the drastic effects a dysfunctional bladder can have on overall quality of life, but more investigation needs to be performed to best tailor radiation therapy while avoiding side effects such as radiation cystitis.
Variation in the incidence of radiation cystitis exists in the current literature. In general, the incidence of delayed radiation effects is estimated at 5% to 10%, and severe hematuria occurs 5% to 8% of the time 1. Differences in tumor type, the extent of cancer, type of radiation used, and total amount of radiation used create a wide range within the literature.
The average duration from completion of radiation therapy to the onset of symptoms is approximately 31.8 months. It develops more commonly in males than females (2.8:1) 1.
Acute radiation cystitis is usually self-limiting and is generally managed with conservative symptomatic therapy or observation. Late radiation cystitis, which can develop months to years after radiation therapy, presents principally as hematuria, which ranges from mild to life-threatening 2. A variety of intravesical agents has been used for these patients. Hypebaric oxygen therapy has shown success in severe or refractory cases 3.
Radiation cystitis grading
The level of severity of radiation cystitis symptoms is graded by Radiation Therapy Oncology Group as follows 4:
- Grade 1 – Any slight epithelial atrophy, microscopic hematuria, mild telangiectasia
- Grade 2 – Any moderate frequency, generalized telangiectasia, intermittent macroscopic hematuria, intermittent incontinence
- Grade 3 – Any severe frequency and urgency, severe telangiectasia, persistent incontinence, reduced bladder capacity (< 150mL), frequent hematuria
- Grade 4 – Any necrosis, fistula, hemorrhagic cystitis, bladder capacity (< 100mL), refractory incontinence requiring catheter or surgical intervention
- Grade 5 – Death directly due to hemorrhagic cystitis
Radiation cystitis symptoms
Acute complaints after completing radiation therapy may include frequency, urgency, dysuria, and hematuria (microscopic or macroscopic). Chronic effects can occur months to years later and are caused by fibrosis. In addition to the symptoms already mentioned, chronic effects can include urinary incontinence from detrusor dysfunction, hydronephrosis, mucosal ulceration, and fistula formation.
In general, symptoms associated with radiation cystitis can be grouped into acute and late-phase, or chronic, symptoms. Acute symptoms are caused by the inflammatory response to ionizing radiation and are similar to those for any inflammatory process of the bladder. They consist of urgency, frequency, dysuria, and hematuria.
Late-phase, or chronic, symptoms are the end result of the inflammatory process caused by radiation. Ischemia and fibrosis are the main factors responsible for symptoms. As a result, new symptoms can occur years after initial therapy, resulting from bladder contraction, ulcer formation, fistulas, and bladder dysfunction. Therefore, clinical presentation can include any of the following urinary symptoms:
- Frequency
- Urgency
- Dysuria
- Hematuria
- Incontinence
- Hydronephrosis
- Pneumaturia (air bubbles in urine)
- Fecaluria (feces in urine)
Radiation cystitis diagnosis
In patients presenting with hematuria post-radiation, a thorough assessment is needed to rule out secondary causes before a diagnosis of radiation cystitis can be made. Radiation cystitis can mimic many different diseases. Neoplasia, urinary tract infection (UTI) and stone disease produce similar findings. Consequently, a complete evaluation of the urinary tract is required. The initial evaluation should include the following:
- Urinalysis to assess for hematuria and pyuria and to measure urine pH
- Urine culture to confirm or rule out infection
- Urinary cytology to screen for tumor
If the patient has hematuria, a complete blood count (CBC) is required to assess hemoglobin, hematocrit, and adequate platelet count. Gross hematuria is an indication to evaluate volume status, coagulation status, and the need for red blood cell (RBC) transfusion. Cystoscopy and renal imaging are also indicated to rule out other possible causes of genitourinary bleeding. Prothrombin time (PT) and activated partial thromboplastin time (aPTT) are needed to rule out coagulopathies if the patient is bleeding.
A white blood cell (WBC) count is necessary to assess for infection if the patient is febrile. Electrolytes, blood urea nitrogen (BUN), and creatinine levels are needed to assess renal function; obstructive uropathy may result from stricturing of the urinary tract and poor emptying. Urodynamics may be required if a patient presents with more complicated symptoms, but most symptoms can be evaluated by a thorough history and physical examination.
Biopsy
Avoid bladder biopsy because it may cause persistent bleeding or even fistula formation. However, judicious use of bladder biopsies may be indicated if a suspicious lesion or recurrent tumor is suggested.
Urodynamic studies
Urodynamic studies are needed only when the diagnosis remains unclear after the history and physical examination. Urodynamics can help to assess for decreased bladder volume, postvoid residual urine, and detrusor instability. All are potentially present in radiation cystitis but are not specific for the disease.
Reported findings in acute cases include the following:
- Detrusor instability (40-50% of patients)
- Decreased peak flow rate
- Decreased bladder compliance
- Decreased bladder volume (approximately 20% volume reduction)
After the acute phase has passed (6 months), most bladder parameters return to normal. Some authors report a persistent loss of bladder compliance; however, it is not significantly different from that in control subjects.
Cystoscopy
Cystoscopy in patients with new-onset or suspected radiation cystitis can be both diagnostic and therapeutic. Cystoscopy is used to confirm the diagnosis and to rule out other conditions, such as bladder cancer or other recurrent metastatic tumors. Cystoscopy can be combined with retrograde pyelography, if needed.
On cystoscopy, acute radiation injury is characterized by changes such as the following:
- Telangiectasia
- Diffuse erythema
- Prominent submucosal vascularity
- Mucosal edema
The appearance of diffuse erythema, telangiectasia with or without ulcerations can help confirm the diagnosis of radiation cystitis. At the time of cystoscopy, fulguration of suspected vascular lesions may provide control of hematuria. In a case series assessing the effectiveness of cystoscopy and fulguration for hematuria control in patients with either radiation- or chemotherapy-induced symptoms, 61% (20/33) of patients achieved resolution of symptoms after initial endoscopic treatment 5. Only 36% (4/11) of patients who had refractory symptoms responded to a second cystoscopy and fulguration.
Multiple small case series have assessed alternatives to fulguration with Greenlight laser, KTP laser treatment, and argon beam coagulator 6. All series report laser therapy being well-tolerated and having a beneficial effect. In the future, they may play a larger role in the treatment of radiation cystitis; however, until larger studies can confirm their safety and effectiveness, they remain experimental in nature. Additional studies have investigated intravesical hemostatic gelatin matrix (Floseal) in six patients and was noted to be beneficial 7. Fibrin glue has been trialed in the treatment of post-hematological stem cell transplant patients and found to reduce hematuria 8, but it has yet to be investigated in the radiation cystitis population beyond individual case studies 9.
Imaging studies
Imaging studies may consist of intravenous pyelography (IVP), CT urography, or renal ultrasonography. IVP (intravenous pyelography) is useful to evaluate anatomic abnormalities of the genitourinary tract (eg, stricturing, fistula formation). If hematuria is present, IVP or CT urography is needed to rule out other causes of bleeding, such as calculus disease and neoplasia. As an alternative, ultrasonography can be used to assess for hydronephrosis due to scarring, renal tumors (as another cause of bleeding), and calculus disease.
CT scanning may also help in the diagnosis of bladder fistulas. Findings in patients with fistulas include the following 10:
- Intravesical air (90%)
- Passage of orally or rectally administered contrast medium into the bladder (20%)
- Focal bladder-wall thickening (90%)
- Thickening of adjacent bowel wall (85%)
- Extraluminal mass that often contains air (75%)
Radiation cystitis treatment
Treatment of radiation cystitis varies depending on the severity of symptoms. For grade 1 and grade 2 types, symptomatic relief is typically all that is necessary. If frequency and urgency are the predominant symptoms, anticholinergic medications can be used for relief. Additionally, bladder irrigation is usually considered the first-line treatment in all grades of the disease and can be used to remove clots if hematuria is present 11. Fulguration (destruction of small areas of tissue) with alum or silver nitrate may be used inside the bladder as well 12.
The use of endoscopic injection sclerotherapy has been reported with good results in a limited number of patients with intractable hemorrhagic cystitis 13. This treatment involves the injection of a sclerosing agent (eg, 1% ethoxysclerol) into the bleeding areas to control the severe hematuria in patients with otherwise intractable bleeding that is not responding to simpler methods. Further studies are necessary to determine the exact role of this novel type of therapy in selected patients with radiation cystitis.
Gacci et al 14 reported that instillation of the combination of hyaluronic acid and chondroitin sulfate was effective in reducing nocturnal voiding frequency in men with bladder pain following radiation therapy for prostate cancer. Study patients underwent bladder instillation therapy with hyaluronic acid and chondroitin sulfate weekly for the first month and, afterwards, on week 6, 8 and 12.
If symptoms become more severe or oral therapy is not satisfactory, the available literature suggests that Hyperbaric Oxygen Therapy yields the most consistent results 15.
Hyperbaric Oxygen Therapy is another form of noninvasive treatment that has become more prevalent in recent years. Hyperbaric Oxygen Therapy not only targets symptom relief but also has the capability of stopping the progression of the pathologic process. Hyperbaric Oxygen Therapy stimulates angiogenesis, which reestablishes blood flow to areas in danger of necrosis, and helps maintain bladder functionality. Studies have shown a complete response rate ranging from 27% to 100% of patients studied, with most showing more than 75% of patients with a complete response 16.
One study showed that, even with milder symptoms, patients treated within six months of hematuria onset had 96% complete or partial symptomatic resolution whereas those treated after six months had but a 66% response rate. This is supportive of (albeit not definitive for) the early use of hyperbaric oxygen therapy 17.
More invasive measures may be necessary if late-stage complications occur or if the radiation cystitis is resistant to more conservative methods. Such situations include persistent hematuria, fistulas, severe detrusor contraction, or hydronephrosis. Failure of more conservative measures leading to cystectomy is associated with a high risk of complications and mortality. Severe complications in almost half (42%) and 90-day mortality is reported to be 16%.
Medications for radiation cystitis
Symptomatic frequency and urgency are best treated with anticholinergic agents. Once all other causes of dysuria have been ruled out, phenazopyridine can be used to provide symptomatic relief.
If the symptoms of radiation cystitis are not severe but are significant enough for a patient to seek help, pentosan polysulfate sodium (Elmiron), with or without pentoxifylline for pain, is a reasonable first step 18.
A randomized, double-blind, placebo-controlled pilot study in 41 men receiving external beam radiation therapy for prostate cancer found that ingestion of cranberry capsules may help prevent or reduce the severity of radiation cystitis, particularly in patients those on low-hydration regimens or with baseline urinary symptoms. The capsules were standardized to contain 72 mg proanthocyanidins. Study patients took one capsule a day at breakfast during treatment and for 2 weeks after treatment completion 19.
Alum irrigation
Intravesical aluminous salts act as an astringent agent and exert their effect through protein precipitation causing decreased capillary permeability, contraction of intercellular space, vasoconstriction, and hardening of the capillary endothelium 20. It is typically administered as a 1% concentration of alum mixed with sterile water, irrigated through the bladder at 250–300 ml per hour, at a duration up to the discretion of the observing clinician. Ideally, the bladder should be irrigated free of clots prior to initiation of therapy. Historical case series have demonstrated the efficacy and tolerability of intravesical alum for a wide range of etiologies and presentations of intractable bladder hemorrhages 21. The common side effects are bladder spasms, suprapubic discomfort, and clotting of the catheter due to precipitant formation. Individual case studies have reported a risk of aluminum toxicity in individuals in renal failure 22.
The most recent, and largest case series reported the use of alum irrigation in 40 patients (38 of whom had previous radiation treatment) with symptoms of hemorrhagic cystitis 23; 60% of these patients demonstrated an improvement in their symptoms and required no further treatment prior to discharge. The treatment was well-tolerated and 90% of patients were able to receive their treatment as prescribed. Two patients discontinued due to inability to tolerate bladder spasms and two for altered level of consciousness. Overall, 35% of patients experienced bladder spasms. Asymptomatic elevation in serum aluminum was detected in one patient that resolved on discontinuation of the treatment. At a median followup of 16.5 months, only 32% of patients required no further treatment, bringing the durability of this treatment into question.
Hyaluronic acid
Hyaluronic acid is a mucopolysaccharide whose therapeutic benefit is believed to be mediated by the repair of the normal glycoaminoglycan layer of the bladder when applied as intravesical installations. It has been shown that radiation leads to defects in this protective layer, leading to chronic inflammatory changes and delayed or prevented healing of urothelial cells 24. Its use as an intravesical agent is well-studied in the treatment of interstitial cystitis and painful bladder syndrome, where it was recently recommended as a treatment option in the Canadian Urological Association guideline 25.
One of the few randomized trials comparing treatment modalities for radiation cystitis randomized 36 patients to either intravesical therapy with hyaluronic acid or treatment with hyperbaric oxygen therapy 26. In the hyaluronic acid group, patients received intravesical therapy once weekly for one month and then monthly for two months. Patients in the hyperbaric oxygen therapy group received daily treatments for 30 treatments. Followup assessment of symptoms were done at six, 12, and 18 months following therapy. Complete resolution of hematuria was noted in 88%, 75%, and 50% of hyaluronic acid patients at those intervals and in 75%, 50%, and 45% of patients in the hyperbaric oxygen therapy group. The difference was not statistically significant at any interval and the author concluded the hyaluronic acid therapy was at least as effective as hyperbaric oxygen therapy in the treatment of hematuria.
A prospective, observational study of 20 patients undergoing treatment with intravesical hyaluronic acid compared grading of radiation cystitis, including hematuria, as per Radiation Therapy Oncology Group classification (scale 1–5) before treatment and again three months after the completion of six scheduled treatments 27. The mean radiocystitis scores before and after hyaluronic acid treatment were 2.70 and 1.45, respectively, with only minor side effects described. It is notable that no patients with grade 4 or 5 toxicity, considered severe symptoms, were included in this study. Beyond hematuria, recent prospectively collected data suggests that intravesical treatment with hyaluronic acid in combination with chondroitin sulfate (another glycosamniglycan) produces a clinically significant improvement in post-radiation lower urinary tract symptoms and bother. In a study published by Gacci et al 28, 80 patients with previous radiation therapy and new-onset or worsening lower urinary tract symptoms were shown to have a statistically significant reduction in urgency, frequency, nocturia, and bladder pain, as measured by patient-reported outcomes after intravesical treatment with hyaluronic acid and chondroitin sulfate.
Other intravesical agents
Intravesical instillation of the antifibrinolytic agent epsilon aminocaproic acid was shown to improve hematuria in 34 patients in case series of 37 patients with intractable bladder hemorrhage, most of whom had either radiation- or cyclophosphamide-induced cystitis; however this has not been repeated in contemporary studies since its publication in 1992 29. Intravesical instillations of prostaglandins have been demonstrated in several smaller case series to be effective in treating hemorrhagic cystitis secondary to treatment with cyclophosphamide, but there are no large studies to suggest their effectiveness in radiation cystitis 30. Silver nitrate instillations have been tried and were found to be ineffective in limiting radiation cystitis 31.
Sodium pentosan polysulfate
Sodium pentosan polysulfate is a semisynthetic polyscaccharide formulated as an oral medication that serves as a synthetic glycosaminoglycan. It adheres to the bladder mucosa, where it supplements the bladder’s own glycosaminoglycan layer in a similar fashion as intravesical treatment with hyaluronic acid. It has been previously shown to be effective in the treatment of interstitial cystitis 32. The largest study to assess its effectiveness in hematuria secondary to radiation followed 60 consecutively enrolled patients who were treated with 100 mg orally of sodium pentosan polysulfate three times daily 33. In 10 patients, hematuria was noted to have resolved completely, and there was partial resolution in 21 patients. However, the applicability of this study was limited by the large number of participants not available for followup or who passed away during the study from causes unrelated to hematuria. Two other small case series have also demonstrated the benefits of oral sodium pentosan polysulfate 34. Its usefulness was noted primarily by its safety, tolerability, and ease of administration; however, the onset of action was found to be 1–8 weeks, limiting its use in the acute setting. A recent case series has suggested a risk of pigmentary maculopathy associated with long-term chronic use of sodium pentosan polysulfate (median duration of 186 months) 35.
Hyperbaric Oxygen Therapy
Therapy for radiation cystitis is primarily aimed at relief of symptoms. The exception is Hyperbaric Oxygen Therapy, which can potentially reverse the changes caused by radiation. Hyperbaric Oxygen Therapy stimulates angiogenesis, which reverses the vascular changes induced by ionizing radiation 36. The ability of Hyperbaric Oxygen Therapy to preserve bladder function and the noninvasive nature of this treatment are features that favor its use. However, if significant fibrosis and ischemia have already occurred, Hyperbaric Oxygen Therapy therapy does not reverse the changes and only prevents further injury 37.
Hyperbaric Oxygen Therapy has a reported response rate of 27-92%, and the recurrence rate is 8-63% 38. In adults, Hyperbaric Oxygen Therapy is administered as 100% oxygen at 2-2.5 ATM. Each session lasts from 90-120 minutes, and patients receive Hyperbaric Oxygen Therapy sessions 5 days weekly for a total of 40-60 sessions. Hyperbaric Oxygen Therapy therapy is a pregnancy category A treatment.
Nakada and colleagues 39 reported good long-term outcomes with Hyperbaric Oxygen Therapy treatment in 38 patients with radiation cystitis following irradiation of prostate cancer. At 7-year follow-up, objective and subjective improvements in symptoms were seen in 72-83% of patients. No recurrence was seen in 28 patients (74%); these patients had received an 18% lower radiation dose than patients who did experience recurrence.
Experimental therapy
WF10, an intravenously administered macrophage regulator, has shown promising results for treatment and decreased recurrence of radiation cystitis in two studies published at a single center 40.
Two small case studies explored the use of estrogen in treatment of hemorrhagic cystitis of multiple etiologies 41. While both showed reduction in hematuria, larger studies are needed before recommendations regarding effectiveness or safety can be made.
There is conflicting evidence that may point to a role for cranberry juice in preventing acute urinary symptoms in patients undergoing pelvic radiation; however, there is no data to suggest it has a role in management of late-effect radiation cystitis 42.
There is a growing body of evidence exploring the use of tranexamic acid in the control of hemorrhage of multiple etiologies. Its use has previously been suggested in the management of radiation cystitis 43. A randomized control trial recently assessed the use of intravenous tranexamic acid in controlling of hematuria of multiple causes in the acute setting. It found a decreased time on continuous bladder irrigation until resolution of hematuria; however, no significant difference in blood loss or transfusions rates were noticed in the treatment group 44. While further studies may demonstrate a benefit in treatment of patients with radiation cystitis with tranexamic acid, at this time there is insufficient published data to support this.
Surgery
Unfortunately, a small percentage of patients will present with life-threatening hemorrhagic cystitis that is refractory to conservative and non-operative measures. These patients can be successfully treated with urinary diversion and cystectomy, however, the associated morbidity with this procedure is high. Surgery is reserved for the management of severe complications that do not respond to medical management. Indications for surgery include the following:
- Ongoing gross hematuria that does not respond to bladder irrigations or that requires numerous transfusions
- Small, contracted bladder with incontinence or severe frequency
- Specific complications of radiation (eg, fistulas, hydronephrosis, strictures)
Surgical options for small-volume bladder include bladder augmentation, urinary diversion, and cystectomy.
Several case series have examined the use of cystectomy in patients who had previously failed less invasive therapies. One series identified 21 patients with hemorrhagic cystitis, 17 from radiation therapy, who underwent cystectomy 45. In this series, 42% of patients experienced severe complications (defined as Clavien grade III–V) and the 90-day mortality rate was 16%. This study echoes the findings of a larger case series looking at surgical outcomes from men undergoing urinary diversion via cystectomy for multiple adverse effects of radiation, including hematuria 46. In this series, 36% of patients experienced Clavian III or greater complications, including 15% who required a second operation, and death in 4.5% of patients within the first 90 days. These rates of complications outpace the comparable rates in patients undergoing radical cystectomy for bladder cancer. Both authors attributed this to baseline fragility and comorbidities in this patient population exacerbated with the challenge of operating in a previously radiated field.
Small case studies have evaluated the use of urinary diversion alone in those who may not tolerate a cystectomy, either through cutaneous ureterostomy 47 or bilateral nephrostomy tubes 48. Although both studies were quite small, they showed improvement in hematuria using urinary diversion alone; this may be a beneficial surgical alternative in patients for whom cystectomy is not a viable option. Caution should be advised, as long-term followup in urinary diversion without cystectomy for benign conditions has shown a high rate of complications in the remaining bladder 49.
Treatment of hemorrhagic cystitis
Hemorrhagic cystitis is a more serious complication of radiation cystitis. Cystoscopy is useful in the initial management, both diagnostically to rule out other pathology and for clot evacuation if bleeding is heavy. This can resolve symptoms in up to 61% of patients at initial presentation.
If bleeding is severe, bladder irrigation may be started either alone or in conjunction with hyperbaric therapy. Start continuous bladder irrigation alone first. If this is not successful, try bladder instillation. In order of increasing toxicity, these agents include 1% alum, aminocaproic acid (Amicar), and 1-10% formalin 50. Other options are oral pentosan polysulfate sodium, Hyperbaric Oxygen Therapy, and oral estrogens 51. If symptoms persist, however, cystoscopic intervention is rarely successful 52.
Surgical options for hemorrhagic cystitis include the following:
- Cystoscopy and fulguration
- Percutaneous nephrostomy tube insertions
- Internal iliac artery embolization
- Surgical diversion
- Cystectomy
Cystectomy for hemorrhagic cystitis is associated with high rates of perioperative complications and mortality. It should be used only after more conservative approaches have been attempted 53.
Refractory and life-threatening hematuria
Transarterial embolization
Advances in interventional radiology have allowed for accurate selective and super-selective transarterial embolizations (TAE) that provide clinicians with management alternatives to more radical surgical procedures in patients with persistent or life-threatening hematuria. The benefit of transarterial embolization is its safety and tolerability in comparison to more aggressive surgical procedures in the frail and elderly patients, who make up a significant proportion of patients with radiation cystitis. However, these procedures are not without their own risks and side effects.
Unfortunately, many of the studies on transarterial embolization for hematuria include urological bleeding of multiple etiologies and do not discriminate between blood loss from bladder or prostatic origins. In a case series of 44 patients looking at the role of transarterial embolization in the management of intractable hematuria hemorrhage of oncological origin, Liguori et al found that the majority of patients (82%) experienced an initial resolution of hematuria 54. The ability to perform selective and superselective transarterial embolization has reduced the risk of ischemic-related side effects. Historical studies have demonstrated ischemic-mediated side effects in as high as 65% in patients undergoing internal iliac artery embolization 55. Although most of these are transient post-embolization syndrome, they also include more serious complications, such as bladder necrosis and, in rare cases, Brown-Sequard syndrome. Comparable modern series published in the last decade quote minor and self-resolving complication rates from 9–31%, with a technical success rate of 88–100% 56.
Formalin
Intravesical formalin was first described in the treatment of bladder hemorrhage in the late 1960s, and was soon assessed in a radiation cystitis cohort. The proposed mechanism involved capillary occlusion and protein fixation at the urothelium level 57. Due to pain with administration, it must administered in an operating room setting with either a general or spinal anesthetic. While its rapid onset of action is appealing, its use is somewhat controversial because of its high morbidity, which appears to be proportional to the concentration of formalin used 58.
The largest review of the efficacy of formalin instillation to treat hemorrhagic cystitis of multiple etiologies was a systematic review of retrospective case series published in 1989 59. The article included 235 patients stratified into three groups by the concentration of formalin instilled (10% vs. 3–6% vs. 1–2%). The complete response rates were 88%, 78%, and 71%, respectively. One benefit of formalin instillations was that complete response was typically achieved within 48 hours of a single instillation. Major complications were typically associated with refluxing into the upper urinary tract and consisted of ureteric stricture function, ureteropelvic junction and uretrovesical junction obstruction requiring urinary diversion, decreased bladder capacity, and vesicular fistulas. The mortality rates for 10% and 4–6% formalin instillation were recorded at 5.7% and 2.2%, respectively. No mortalities occurred in the 21 patients treated with 1–2% concentration.
Several other studies were completed that found formalin to be associated with a high treatment efficacy, but with potentially severe complications. In a study of 35 patient with radiation cystitis post-cervical radiation, 89% were found to have complete response after a single instillations; however, 31% had major complications 60. One contemporary study investigated eight patients treated with formalin instillations after less invasive treatments had failed. In this study, each patient had a preoperative cystogram to assess for perforation or vesicoureteral reflux, and if any reflux was suspected, Fogarty catheters were used to obstruct the ureter 57. Formalin concentration ranged from 1–4% and contact time was kept to 10–15 minutes. The complete resolution rate was 75% and only one patient had major complications necessitating intensive care unit admission. A detailed description of the procedure can be found within this article for clinicians unfamiliar with this treatment option.
Procedural variations for decreasing the morbidity associated with formalin instillations have been proposed, from decreasing formalin concentration to alternative methods of formalin delivery. A small, prospective study compared intravesical instillation of 4% formalin in 11 patients to endoscopic placement of formalin soaked pledgets 61. Success rate was similar (82% and 75%, respectively), however the intravesicle instillation group suffered from four major complications, whereas the pledget group suffered only minor side effects. The differences were not statistically significant and while a comparable method was described in two individual case studies 62, follow-up with further larger or prospective studies is lacking.
Radiation cystitis prognosis
Acute symptoms of radiation injury to the bladder are self-limiting and generally respond to symptomatic therapy, such as anticholinergic medications and analgesics. Severe complications of radiation injuries are difficult to manage because they tend to be chronic or recurrent and are occasionally refractory to therapy. Proper interpretation of treatment outcome is limited by few follow-up studies and the small number of patients reported in these studies.
The available follow-up studies performed with various treatment regimens demonstrate that although all have some effectiveness, no single modality is superior. They also show the recurrent nature of radiation complications of the bladder. Complications of radiation cystitis include hemorrhagic cystitis (3%-5%), vesical fistula (2%), and bladder neck contracture (3%-5%). Neoplasia and contracted bladder can also occur but are rare.
References- Horan N, Cooper JS. Radiation Cystitis And Hyperbaric Management. [Updated 2019 Jan 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470594
- Smit SG, Heyns CF. Management of radiation cystitis. Nat Rev Urol. 2010 Apr. 7 (4):206-14.
- Zwaans BM, Chancellor MB, Lamb LE. Modeling and Treatment of Radiation Cystitis. Urology. 2016 Feb. 88:14-21.
- Cox JD, Stetz J, Pajak TF. Toxicity criteria of the radiation therapy oncology group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC) Int J Rad Oncol Biol Physics. 1995;31:1341–5. doi: 10.1016/0360-3016(95)00060-C
- Kaplan JR, Wolf JS., Jr Efficacy and survival associated with cystoscopy and clot evacuation for radiation or cyclophosphamide induced hemorrhagic cystitis. J Urol. 2009;181:641–6. doi: 10.1016/j.juro.2008.10.037
- Talab SS, McDougal WS, Wu CL, et al. Mucosa-sparing, KTP laser coagulation of submucosal telangiectatic vessels in patients with radiation-induced cystitis: A novel approach. Urology. 2014;84:478–83. doi: 10.1016/j.urology.2014.03.029
- Margreiter M, Sharma V, Schauer I, et al. Intravesical hemostatic gelatin matrix instillation in the management of intractable hematuria. Urology. 2013;82:724–8. doi: 10.1016/j.urology.2013.06.003
- Tirindelli MC, Flammia GP, Bove P, et al. Fibrin glue therapy for severe hemorrhagic cystitis after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20:1612–7. doi: 10.1016/j.bbmt.2014.06.018
- Ouwenga M, Langston M, Campbell S. Use of fibrin sealant in recalcitrant hemorrhagic cystitis. J Urol. 2004;172:1348. doi: 10.1097/01.ju.0000137723.38685.ff
- Goldman SM, Fishman EK, Gatewood OM, Jones B, Siegelman SS. CT in the diagnosis of enterovesical fistulae. AJR Am J Roentgenol. 1985 Jun. 144(6):1229-33.
- Cooper JS, Allinson P, Winn D, Keim L, Sippel J, Shalberg P, Fowler K. Continuous bladder irrigation in the monoplace hyperbaric chamber: Two case reports. Undersea Hyperb Med. 2015 Sep-Oct;42(5):419-23.
- Mallick S, Madan R, Julka PK, Rath GK. Radiation Induced Cystitis and Proctitis – Prediction, Assessment and Management. Asian Pac. J. Cancer Prev. 2015;16(14):5589-94.
- Tunuguntla HS, Bhandari M, Srivastava A, Kapoor R, Saha TK. Endoscopic injection sclerotherapy control of intractable hematuria following radiation-induced hemorrhagic cystitis. A novel approach. Arch Esp Urol. 2000 May. 53(4):396-402.
- Gacci M, Saleh O, Giannessi C, Detti B, Livi L, Monteleone Pasquetti E, et al. Sodium hyaluronate and chondroitin sulfate replenishment therapy can improve nocturia in men with post-radiation cystitis: results of a prospective pilot study. BMC Urol. 2015 Jul 7. 15:65.
- Weiss JP, Mattei DM, Neville EC, Hanno PM. Primary treatment of radiation-induced hemorrhagic cystitis with hyperbaric oxygen: 10-year experience. J Urol. 1994 Jun. 151(6):1514-7.
- Ribeiro de Oliveira TM, Carmelo Romão AJ, Gamito Guerreiro FM, Matos Lopes TM. Hyperbaric oxygen therapy for refractory radiation-induced hemorrhagic cystitis. Int. J. Urol. 2015 Oct;22(10):962-6.
- Chong KT, Hampson NB, Corman JM. Early hyperbaric oxygen therapy improves outcome for radiation-induced hemorrhagic cystitis. Urology. 2005 Apr;65(4):649-53.
- Sandhu SS, Goldstraw M, Woodhouse CR. The management of haemorrhagic cystitis with sodium pentosan polysulphate. BJU Int. 2004 Oct. 94(6):845-7.
- Hamilton K, Bennett NC, Purdie G, Herst PM. Standardized cranberry capsules for radiation cystitis in prostate cancer patients in New Zealand: a randomized double blinded, placebo controlled pilot study. Support Care Cancer. 2015 Jan. 23 (1):95-102.
- Choong SKS, Walkden M, Kirby R. The management of intractable hematuria. BJU Int. 2000;86:951–6. doi: 10.1046/j.1464-410x.2000.00900.x
- Takashi M, Kondo A, Kato K, et al. Evaluation of intravesical alum irrigation for massive bladder hemorrhage. Urol Int. 1988;43:286–8. doi: 10.1159/000281356
- Phelps KR, Naylor K, Brien TP, et al. Encephalopathy after bladder irrigation with alum: Case report and literature review. Am J Med Sci. 1999;318:181. doi: 10.1016/S0002-9629(15)40610-X
- Westerman ME, Boorjian SA, Linder BJ. Safety and efficacy of intravesical alum for intractable hemorrhagic cystitis: A contemporary evaluation. Int Braz J Urol. 2016;42:1144–9. doi: 10.1590/s1677-5538.ibju.2015.0588
- Lazzeri ML, Hurle R, Casale P, et al. Managing chronic bladder diseases with the administration of exogenous glycosaminoglycans: An update on the evidence. Ther Adv Urol. 2016;8:91–9. doi: 10.1177/1756287215621234
- Cox A, Golda N, Nadeau G, et al. CUA guideline: Diagnosis and treatment of interstitial cystitis/bladder pain syndrome. Can Urol Assoc J. 2016;10:E136–55. doi: 10.5489/cuaj.3786
- Shao Y, Lu GL, Shen ZJ. Comparison of intravesical hyaluronic acid instillation and hyperbaric oxygen in the treatment of radiation-induced hemorrhagic cystitis. BJU Int. 2012;109:691–4. doi: 10.1111/j.1464-410X.2011.10550.x
- Vasssilis K, Eftychia MA, Fotineas A, et al. Use of hyaluronic acid (cystistat) for the treatment of late radiation-induced cystitis in patients after prostate irradiation. J Bioequiv Availab. 2014;6:18–22. doi: 10.4172/jbb.1000174
- Gacci M, Saleh O, Giannessi C, et al. Bladder instillation therapy with hyaluronic acid and chondroitin sulfate improves symptoms of post-radiation cystitis: Prospective pilot study. Clin Genitourin Cancer. 2016;14:444–9. doi: 10.1016/j.clgc.2016.01.016
- Singh I, Laungani MD. Intravesical epsilon aminocaproic acid in management of intractable bladder hemorrhage. Urology. 1992;40:227–9. doi: 10.1016/0090-4295(92)90479-G
- Levine LA, Jarrard DF. Treatment of cyclophosphamide-induced hemorrhagic cystitis with intravesical carboprost tromethamine. J Urol. 1993;149:719–23. doi: 10.1016/S0022-5347(17)36192-X
- Montgomery BD, Boorjian SA, Ziegelmann MJ, et al. Intravesical silver nitrate for refractory hemorrhagic cystitis. Turk J Urol. 2016;42:197–201. doi: 10.5152/tud.2016.38445
- Hwang P, Auclair B, Beechinor DD, et al. Efficacy of pentosan polysulfate in the treatment of interstitial cystitis: A meta-analysis. Urology. 1997;50:39–43. doi: 10.1016/S0090-4295(97)00110-6
- Sandhu SS, Goldstraw M, Woodhouse CR. The management of hemorrhagic cystitis with sodium pentosan polysulphate. BJU Int. 2004;94:845–7. doi: 10.1111/j.1464-410X.2004.05044.x
- Hampson SJ, Woodhouse CR. Sodium pentosanpolysulphate in the management of haemorrhagic cystitis: Experience with 14 patients. Eur Urol. 1994;25:40–2. doi: 10.1159/000475245
- Pearce WA, Chen R, Jain N. Pigmentary maculopathy associated with chronic exposure to pentosan polysulfate sodium. Ophthalmology. 2018;125:1793–1802. doi: 10.1016/j.ophtha.2018.04.026
- Neheman A, Nativ O, Moskovitz B, Melamed Y, Stein A. Hyperbaric oxygen therapy for radiation-induced haemorrhagic cystitis. BJU Int. 2005 Jul. 96(1):107-9.
- Allen S, Kilian C, Phelps J, et al. The use of hyperbaric oxygen for treating delayed radiation injuries in gynecologic malignancies: a review of literature and report of radiation injury incidence. Support Care Cancer. 2012 Jan 14.
- Ribeiro de Oliveira TM, Carmelo Romão AJ, Gamito Guerreiro FM, Matos Lopes TM. Hyperbaric oxygen therapy for refractory radiation-induced hemorrhagic cystitis. Int J Urol. 2015 Oct. 22 (10):962-6.
- Nakada T, Nakada H, Yoshida Y, Nakashima Y, Banya Y, Fujihira T, et al. Hyperbaric oxygen therapy for radiation cystitis in patients with prostate cancer: a long-term follow-up study. Urol Int. 2012. 89(2):208-14.
- Veerasarn V, Boonnuch W, Kakanaporn C. A phase 2 study to evaluate WF10 in patients with late hemorrhagic radiation cystitis and proctitis. Gynecol Oncol. 2006;100:179–84. doi: 10.1016/j.ygyno.2005.08.014
- Miller J, Burfield GD, Moretti KL. Oral conjugated estrogen therapy for treatment of hemorrhagic cystitis. J Urol. 1994;151:1348–50. doi: 10.1016/S0022-5347(17)35249-7
- Hamilton K, Bennett NC, Purdie G, et al. Standardized cranberry capsules for radiation cystitis in prostate cancer patients in New Zealand: A randomized, double-blinded, placebo-controlled pilot study. Support Care Cancer. 2015;23:95–102. doi: 10.1007/s00520-014-2335-8
- Browne C, Davis NF, Mac Craith E, et al. A narrative review on the pathophysiology and management for radiation cystitis. Adv Urol. 2015 346812
- Moharamzadeh P, Ojaghihaghighi S, Amjadi M, et al. Effect of tranexamic acid on gross hematuria: A pilot randomized clinical trial study. Am J Emerg Med. 2017;35:1922–5. doi: 10.1016/j.ajem.2017.09.012
- Linder BJ, Tarrell RF, Boorjian SA. Cystectomy for refractory hemorrhagic cystitis: Contemporary etiology, presentation and outcomes. J Urol. 2014;192:1687–92. doi: 10.1016/j.juro.2014.06.030
- Bassett MR, Santiago-Lastra Y, Stoffel JT, et al. Urinary diversion for severe urinary adverse events of prostate radiation: Results from a multi-institutional study. J Urol. 2017;197:744–50. doi: 10.1016/j.juro.2016.10.091
- Pomer S, Karcher G, Simon W. Cutaneous ureterostomy as last resort treatment of intractable hemorrhagic cystitis following radiation. BJU Int. 1983;55:392–4. doi: 10.1111/j.1464-410X.1983.tb03329.x
- Zagoria RJ, Hodge RG, Dyer RB, et al. Percutaneous nephrostomy for treatment of intractable hemorrhagic cystitis. J Urol. 1993;149:1449–51. doi: 10.1016/S0022-5347(17)36412-1
- Fazili T, Bhat TR, Masood S, et al. Fate of the leftover bladder after supravesical urinary diversion for benign disease. J Urol. 2006;176:620–1. doi: 10.1016/j.juro.2006.03.056
- Dewan AK, Mohan GM, Ravi R. Intravesical formalin for hemorrhagic cystitis following irradiation of cancer of the cervix. Int J Gynaecol Obstet. 1993 Aug. 42(2):131-5.
- Liu YK, Harty JI, Steinbock GS, Holt HA Jr, Goldstein DH, Amin M. Treatment of radiation or cyclophosphamide induced hemorrhagic cystitis using conjugated estrogen. J Urol. 1990 Jul. 144(1):41-3.
- Kaplan JR, Wolf JS Jr. Efficacy and survival associated with cystoscopy and clot evacuation for radiation or cyclophosphamide induced hemorrhagic cystitis. J Urol. 2009 Feb. 181(2):641-6.
- Linder BJ, Tarrell RF, Boorjian SA. Cystectomy for Refractory Hemorrhagic Cystitis: Contemporary Etiology, Presentation and Outcomes. J Urol. 2014 Jun 14.
- Liguori G, Amodeo A, Mucelli FP, et al. Intractable hematuria: Long-term results after selective embolization of the internal iliac arteries. BJU Int. 2010;106:500–3. doi: 10.1111/j.1464-410X.2009.09192.x
- Pisco JM, Martins JM, Correia MG. Internal iliac artery: Embolization to control hemorrhage from pelvic neoplasms. Radiology. 1989;172:337–9. doi: 10.1148/radiology.172.2.2748811
- Korkmaz M, Sanal B, Aras B, et al. The short- and long-term effectiveness of transcatheter arterial embolization in patients with intractable hematuria. Diagn Interv Imaging. 2016;97:197–201. doi: 10.1016/j.diii.2015.06.020
- Ziegelmann MJ, Boorjian SA, Joyce DD, et al. Intravesical formalin for hemorrhagic cystitis: A contemporary cohort. Can Urol Assoc J. 2017;11:E79–82. doi: 10.5489/cuaj.4047
- McAchran SE, Rackley RR. Hemorrhagic and Radiation Cystitis. In: Potts JM, editor. Genitourinary Pain And Inflammation Current Clinical Urology. Humana Press; 2008. pp. 351–66.
- Donahue L, Frank I. Intravesical formalin for hemorrhagic cystitis: Analysis of therapy. J Urol. 1989;141:809–12. doi: 10.1016/S0022-5347(17)41016-0
- Dewan AKM, Mohan GM, Ravi R. Intravesical formalin for hemorrhagic cystitis following irradiation of cancer of the cervix. Int J Gynaecol Obstet. 1993;42:131–5. doi: 10.1016/0020-7292(93)90626-8
- Lojanapiwat B, Sripralakrit S, Soonthornphan S, et al. Intravesicle formalin instillation with a modified technique for controlling hemorrhage secondary to radiation cystitis. Asian J Surg. 2002;25:232–5. doi: 10.1016/S1015-9584(09)60181-0
- Haraguchi TY, Takechi Y. [Hemorrhagic radiation cystitis: A transurethral treatment with formalin-soaked pledgets]. Hinyokika Kiyo. 2007;53:585–7.