What is scrofula
Scrofula is an old term used to describe tuberculosis (TB) infecting the lymph nodes of the neck or cervical tuberculous lymphadenitis 1. Scrofula is usually the result of a primary infection of the lymph nodes with Mycobacterium tuberculosis. The bacteria can be spread by the lymphatic system or blood. Therefore, it could originate from a primary pulmonary focus. In adults, it is usually Mycobacterium tuberculosis and in children, nontuberculous mycobacteria 2.
The most common presentation of scrofula is a painless, often suppurative abscess that shows no signs of warmth or redness unless there is a secondary infection. Patients less frequently present with systemic signs such as weight loss and night sweats 3.
In the US and Europe, with the rapid decrease of tuberculosis (TB) in the second half of the twentieth century, scrofula has become a very rare disease. The marked decrease in prevalence amongst the more economically developed countries was due to the pasteurization of milk and the Bacillus Calmette-Guérin (BCG) vaccine. TB is still a major problem across the less economically developed countries, and therefore clinicians have a higher degree of suspicion when assessing patients. According to a study carried out in India, extrapulmonary tuberculosis (TB) constitutes about 15% to 20% of new tuberculosis (TB) cases in immunocompetent patients. This can rise to over 50% in immunocompromised patients, especially in patients positive for the human immunodeficiency virus (HIV) 4.
Patients over the age of 65 have waning immunity and are therefore a vulnerable group for acute tuberculosis (TB) infections as well as the re-activation of indolent Mycobacterium organisms. Post-splenectomy patients are at a major disadvantage during sepsis and when a cellular immune response is required, such as when faced with a Mycobacterium tuberculosis infection.
Aging is known to have detrimental effects on your immune system and is referred to as immunosenescence. It is a complex process that affects cell mediated immunity 5. As you age, you lose lymphoid tissue. T lymphocyte cell activation is reduced plus a larger percentage of activated T-cells responses start later and stop sooner. Natural Killer cell activity is also reduced significantly. It has been suggested that, as you age, the innate response prevails over the adaptive response (see immune response) 6.
The immune response to tuberculosis (TB) greatly relies on T lymphocytes and Natural Killer cells and so the aging immune system is much less capable of responding to Mycobacterium tuberculosis.
The spleen is an important organ in the defense against invading pathogens. It acts as a filtering system, permitting phagocytosis of bacteria by cells in the reticuloendothelial system. The spleen is also an important site capable of producing large quantities of antibodies, which has proven vital in preventing and tackling sepsis. Therefore, the major risk post-splenectomy is that of overwhelming sepsis 7.
The humoral role of the spleen has been well documented and recent studies have shown the spleen to have a significant role in cell mediated immunity. The spleen is an important organ for the differentiation and maturation of stem cells into immunocompetent B lymphocyte cells (B-cells). B-cells were once mostly associated with the humoral immune response. However, recent studies have shown a variety of interactions of B-cells with the cellular immune response, which is necessary against infection by Mycobacterium tuberculosis 8.
Scrofula is treated with a similar regime as pulmonary tuberculosis and has a near 100% success rate 1.
Is scrofula contagious?
Yes. Tuberculosis (TB) is a disease caused by bacteria called Mycobacterium tuberculosis that usually attack the lungs, but they can also damage other parts of the body. It is recommended that people in close contact, such as family members, should undergo testing for tuberculosis.
Tuberculosis spreads through the air when a person with tuberculosis of the lungs or throat coughs, sneezes, or talks. If you have been exposed, you should go to your doctor for tests. You are more likely to get tuberculosis if you have a weak immune system.
How your immune system responds to Mycobacterium tuberculosis has a major role in determining the clinical manifestations. Once the Mycobacterium tuberculosis bacteria have reached the lungs alveoli it has four potential fates 9: the immune system may destroy the Mycobacterium tuberculosis bacilli and the patient gains immunity; the Mycobacterium tuberculosis bacilli multiply and cause disease, that is, pulmonary TB; the Mycobacterium tuberculosis bacilli become dormant and never cause disease; or the patient may develop reactivation tuberculosis – active disease due to an existing impairment in the immune system through, for example, HIV, malignancy or malnutrition.
During the primary infection with tuberculosis and during any subsequent secondary active disease, the bacteria are spread by blood or through the lymphatic system to any part of the body. Usually the Mycobacterium tuberculosis bacteria are destroyed by the immune system; however, they may concentrate at a particular site and lie dormant for decades before causing disease.
Symptoms of tuberculosis in the lungs may include:
- A bad cough that lasts 3 weeks or longer
- Weight loss
- Loss of appetite
- Coughing up blood or mucus
- Weakness or fatigue
- Fever
- Night sweats
Skin tests, blood tests, x-rays, and other tests can tell if you have TB. If not treated properly, TB can be deadly. You can usually cure active TB by taking several medicines for a long period of time.
Scrofula causes
Scrofula is most often caused by the bacteria Mycobacterium tuberculosis. There are many other types of mycobacterium bacteria that cause scrofula.
Scrofula is usually caused by breathing in air that is contaminated with mycobacterium bacteria. The bacteria then travel from the lungs to lymph nodes in the neck.
Scrofula symptoms
Symptoms of scrofula are:
- Fevers (rare)
- Painless swelling of lymph nodes in the neck and other areas of the body
- Sores (rare)
- Sweating
Scrofula possible complications
These complications may occur from scrofula disease:
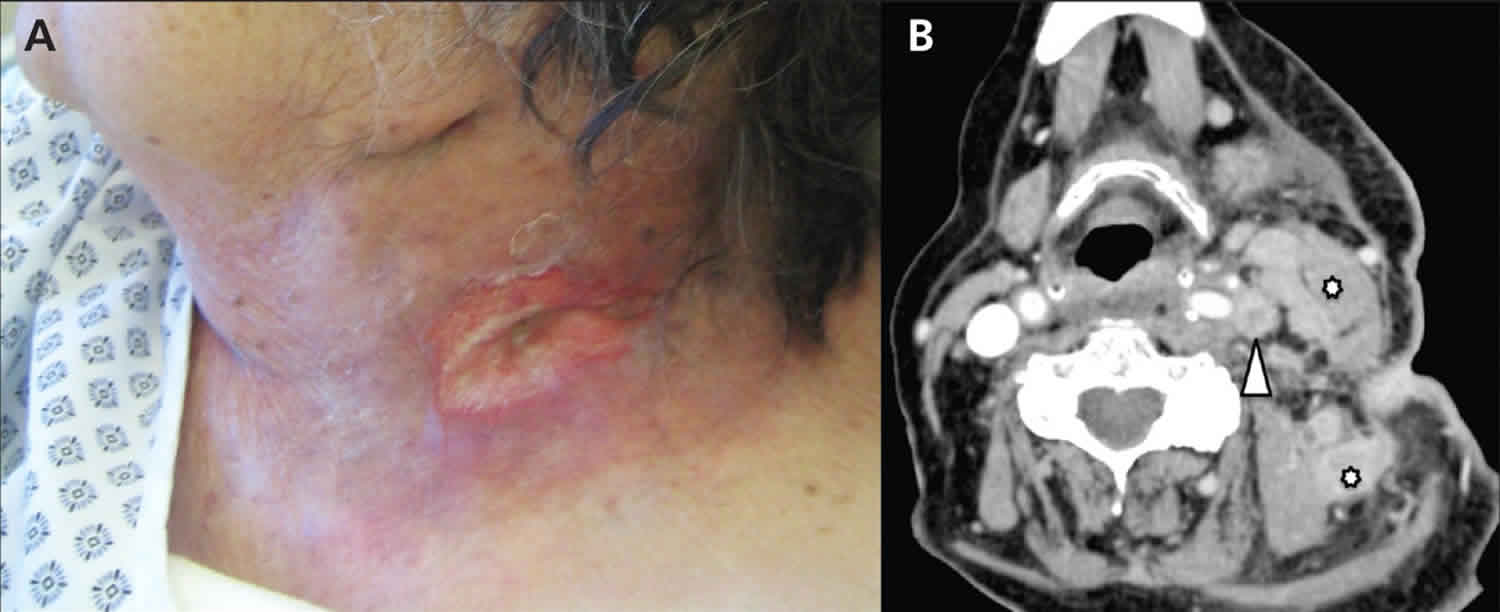
- Draining sore in the neck
- Scarring
Scrofula diagnosis
Tests to diagnose scrofula include:
- Biopsy of affected tissue
- Chest x-rays
- CT scan of the neck
- Cultures to check for the bacteria in tissue samples taken from the lymph nodes
- HIV blood test
- PPD test (also called TB test)
- Other tests for tuberculosis (TB) including blood tests to detect if you have been exposed to TB
It is difficult to culture tuberculosis (TB) from superficial swabs, resulting in a high proportion of false negative results. Where there is a high degree of clinical suspicion for tuberculosis, it is important to consider a biopsy with culture.
Scrofula treatment
Treatment is similar to that for pulmonary disease, which is with isoniazid, rifampicin, pyrazinamide and ethambutol for two months followed by a longer course of rifampicin and isoniazid. The length of time for treatment has long been debated, with no firm consensus. The duration depends on the patient, the response to treatment, the risk of relapse and the site and tissue involved. Where there is limited lymph node involvement, treatment is usually continued for at least four months. Surgery is usually not implicated. With adequate treatment, clinical remission is practically 100%.
It is very important that people who have TB disease are treated, finish the medicine, and take the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again; if they do not take the drugs correctly, the TB bacteria that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat.
Regimens for treating TB disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment).
When infection is caused by Mycobacterium tuberculosis, treatment usually involves 9 to 12 months of antibiotics. Several antibiotics need to be used at once. Common antibiotics for scrofula include:
- Ethambutol
- Isoniazid (INH)
- Pyrazinamide
- Rifampin
When infection is caused by another type of mycobacteria (which often occurs in children), treatment usually involves antibiotics such as:
- Rifampin
- Ethambutol
- Clarithromycin
Surgery is sometimes used first. It may also be done if the medicines are not working.
Table 1. Drug Susceptible TB Disease Treatment Regimens
Abbreviations: DOT = directly observed therapy; EMB = ethambutol; HIV = human immunodeficiency virus; INH = isoniazid; PZA = pyrazinamide; RIF = rifampin.
Footnote: Use of once-weekly therapy with INH 900 mg and rifapentine 600 mg in the continuation phase is not generally recommended. In uncommon situations where more than once-weekly DOT is difficult to achieve, once-weekly continuation phase therapy with INH 900 mg plus rifapentine 600 mg may be considered for use only in HIV uninfected persons without cavitation on chest radiography.
a Other combinations may be appropriate in certain circumstances; additional details are provided in the Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis (https://academic.oup.com/cid/article/63/7/e147/2196792).
b When DOT is used, drugs may be given 5 days per week and the necessary number of doses adjusted accordingly. Although there are no studies that compare 5 with 7 daily doses, extensive experience indicates this would be an effective practice. DOT should be used when drugs are administered less than 7 days per week.
c Based on expert opinion, patients with cavitation on initial chest radiograph and positive cultures at completion of 2 months of therapy should receive a 7-month (31-week) continuation phase.
d Pyridoxine (vitamin B6), 25–50 mg/day, is given with INH to all persons at risk of neuropathy (e.g., pregnant women; breastfeeding infants; persons with HIV; patients with diabetes, alcoholism, malnutrition, or chronic renal failure; or patients with advanced age). For patients with peripheral neuropathy, experts recommend increasing pyridoxine dose to 100 mg/day.
e Alternatively, some U.S. TB control programs have administered intensive-phase regimens 5 days per week for 15 doses (3 weeks), then twice weekly for 12 doses.
Continuation Phase of Treatment
The continuation phase of treatment is given for either 4 or 7 months. The 4-month continuation phase should be used in most patients. The 7-month continuation phase is recommended only for the following groups:
- Patients with cavitary pulmonary TB caused by drug-susceptible organisms and whose sputum culture obtained at the time of completion of 2 months of treatment is positive;
- Patients whose intensive phase of treatment did not include PZA;
- Patients with HIV who are not receiving antiretroviral treatment (ART) during TB treatment; and
- Patients being treated with once weekly INH and rifapentine and whose sputum culture obtained at the time of completion of the intensive phase is positive.
Note: Use of once-weekly therapy with INH 900 mg and rifapentine 600 mg in the continuation phase is not generally recommended. In uncommon situations where more than once-weekly DOT is difficult to achieve, once-weekly continuation phase therapy with INH 900 mg plus rifapentine 600 mg may be considered for use only in HIV uninfected persons without cavitation on chest radiography.
Treatment Completion
Treatment completion is determined by the number of doses ingested over a given period of time.
Treatment for Drug-Resistant TB
Drug-resistant TB is caused by TB bacteria that are resistant to at least one first-line anti-TB drug. Multidrug-resistant TB (MDR TB) is resistant to more than one anti-TB drug and at least isoniazid (INH) and rifampin (RIF).
Treating and curing drug-resistant TB is complicated. Inappropriate management can have life-threatening results. Drug-resistant TB should be managed by or in close consultation with an expert in the disease.
Scrofula prognosis
With treatment, people with scrofula often make a complete recovery.
References- Niblock AL. Recurrent neck abscesses due to cervical tuberculous lymphadenopathy in an elderly woman post-splenectomy: a case report. J Med Case Rep. 2011;5:584. Published 2011 Dec 20. doi:10.1186/1752-1947-5-584 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3284562/
- Clinical differences between pulmonary and extrapulmonary tuberculosis: a 5-year retrospective study. Antony SJ, Harrell V, Christie JD, Adams HG, Rumley RL. J Natl Med Assoc. 1995 Mar; 87(3):187-92.
- Braun-Falco O, Plewig G, Wolff HH. Dermatology and venereology [in German] 3. Berlin, Germany: Springer-Verlag; 1984
- Extrapulmonary tuberculosis. Sharma SK, Mohan A. Indian J Med Res. 2004 Oct; 120(4):316-53.
- Boren E, Gershwin ME. Inflamm-aging: autoimmunity, and the immune-risk phenotype. Autoimmun Rev. 2004;3(5):401–406. doi: 10.1016/j.autrev.2004.03.004.
- Yan J, Greer JM, Hull R, O’Sullivan JD, Henderson RD, Read SJ, McCombe PA. The effect of ageing on human lymphocyte subsets: comparison of males and females. Immun Ageing. 2010;7:4. doi: 10.1186/1742-4933-7-4.
- Rozing J, Brons NHC, Benner R. Effects of splenectomy on the humoral immune system, A study in neonatally and adult splenectomized mice. Immunology. 1978;34(5):909–917
- Maglione PJ, Chan J. How B cells shape the immune response against Mycobacterium tuberculosis. Eur J Immunol. 2009;39(3):676–686. doi: 10.1002/eji.200839148.
- Roles of cytotoxic delayed-type hypersensitivity and macrophage-activating cell-mediated immunity in the pathogenesis of tuberculosis. Dannenberg AM Jr. Immunobiology. 1994 Oct; 191(4-5):461-73.
- Treatment for TB Disease. https://www.cdc.gov/tb/topic/treatment/tbdisease.htm