Sialadenitis
Sialadenitis refers to the inflammation or bacterial infection of a salivary gland, usually due to an obstructing stone or salivary gland hyposecretion. Symptoms are swelling, pain, redness, and tenderness. Sialadenitis is most common among elderly adults with salivary gland stones, calcified structures that can form inside a salivary gland and block the flow of saliva into the mouth and mostly affects the parotid and submandibular glands. Sialadenitis can also occur in other age groups, including infants during the first few weeks of life. Sialadenitis affects men and women of all races equally.
Sialadenitis often happens in people who are sick or recovering from surgery, or people who are dehydrated, malnourished, or immunosuppressed (when your body can’t fight disease).
Sialadenitis diagnosis is clinical. CT, ultrasonography, and MRI may help identify the cause. Treatment is with antibiotics.
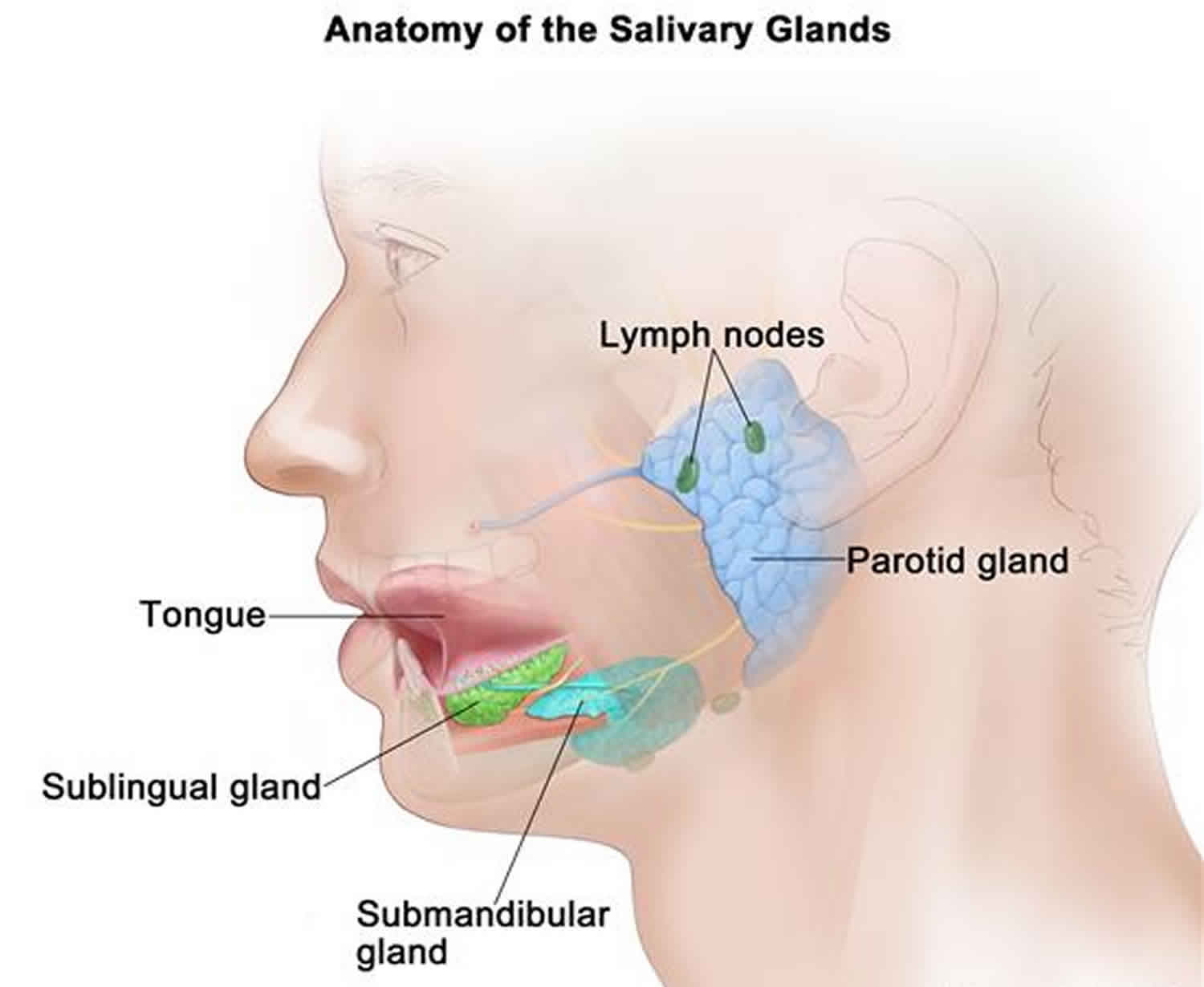
Salivary glands are the glands that make saliva, which helps with swallowing and digestion and protects your teeth from bacteria. There are three main salivary glands:
- Parotid glands in front of the ear in the cheeks
- Submandibular glands under the chin
- Sublingual glands under the tongue
Sialadenitis mostly affects the parotid and submandibular glands.
Sialadenitis can be an acute (sudden), chronic (long term), or recurrent condition. Sialadenitis is a rare condition.
Figure 1. Sialadenitis
Acute suppurative sialadenitis
Acute sialadenitis is a bacterial inflammation of the salivary gland. Acute sialadenitis typically affects one major salivary gland, most commonly the parotid 1 and is common in medically debilitated, hospitalized, or postoperative patients. Retrograde bacterial contamination from the oral cavity is thought to be the inciting cause 2. Stasis of salivary flow secondary to dehydration or decreased oral intake allows bacterial migration into the gland parenchyma.
Predisposing factors for acute sialadenitis include diabetes mellitus, hypothyroidism, renal failure, and Sjögren syndrome. The use of certain medications, especially those with anticholinergic properties, can also reduce salivary flow. Sialolithiasis and duct strictures can impair salivary flow and predispose the patient to acute infection, but more commonly cause chronic or recurrent infections. The most common bacterial cause of acute sialadenitis is Staphylococcus aureus, which has been cultured in 50% to 90% of cases 3. Streptococcal species and Haemophilus influenzae are also common causes 4.
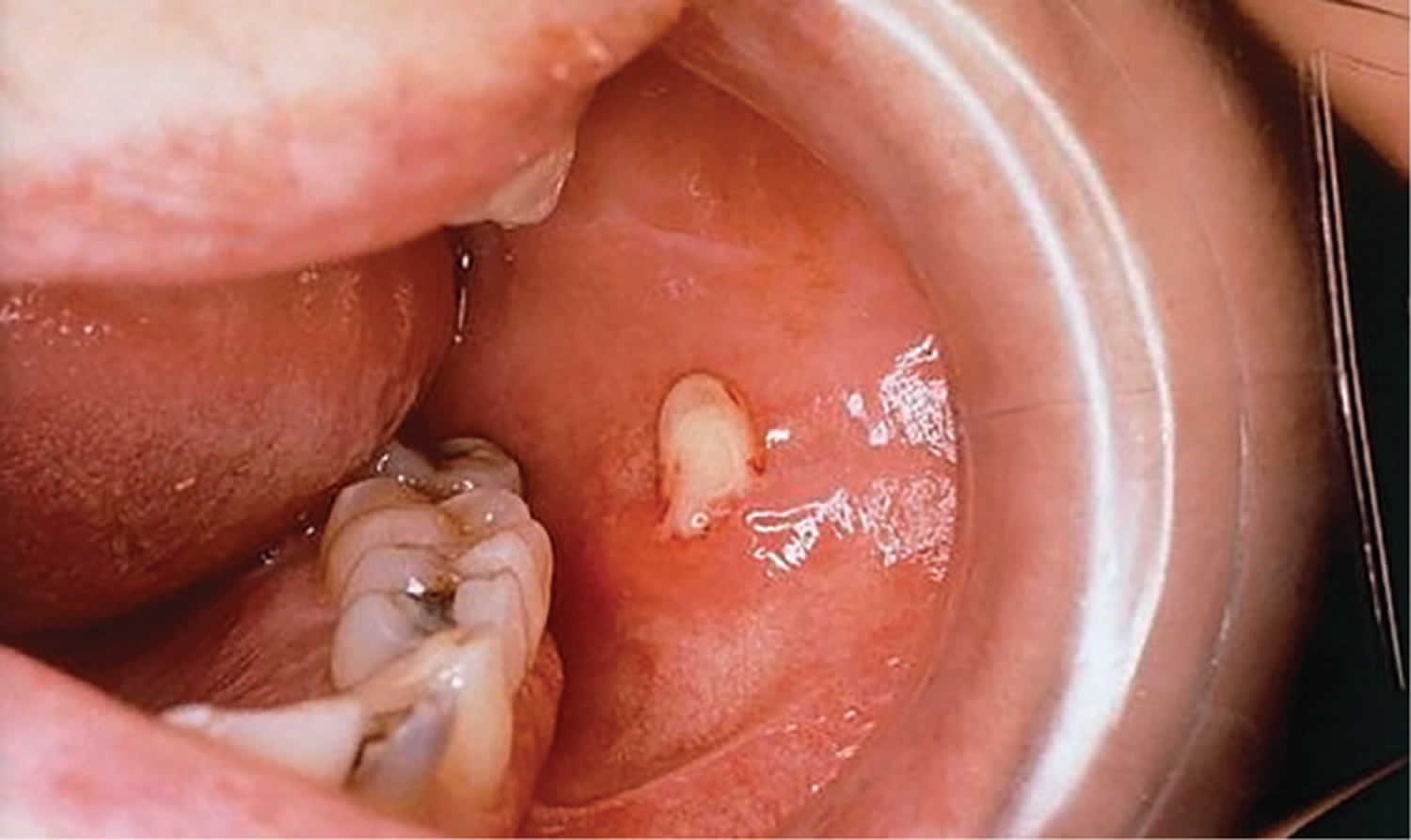
Patients with acute sialadenitis typically present with acute onset of pain and swelling of the affected gland. Physical examination may reveal induration, edema, and extreme localized tenderness. Massage of the gland may express pus from the respective intraoral orifice (Figure 2). This should be cultured to direct antibiotic therapy.
Management involves treating the infection and reversing the underlying medical condition and predisposing factors. This includes stimulation of salivary flow by application of warm compresses, administration of sialagogues (agents that promote the secretion of saliva) such as lemon drops or vitamin C lozenges 5, hydration, salivary gland massage, and oral hygiene. Empiric antimicrobial therapy is initially directed at gram-positive and anaerobic organisms, which are often penicillin-resistant, so augmented penicillin that contains beta-lactamase inhibitors (e.g., amoxicillin-clavulanate [Augmentin]) are recommended 6. Culture-directed therapy is administered, if possible. Rarely, acute suppurative sialadenitis can lead to abscess formation; surgical drainage is indicated in these cases.
Figure 2. Acute sialadenitis
Footnote: Intraoral view of purulence emanating from the parotid duct orifice in a patient with acute suppurative parotitis.
[Source 6 ]Chronic sialadenitis
Chronic sialadenitis is characterized by repeated episodes of pain and inflammation caused by decreased salivary flow and salivary stasis 6. Chronic sialadenitis most often affects the parotid gland 7. The initial inciting factor is thought to be salivary duct obstruction from stones, strictures, scarring, foreign bodies, or extrinsic compression by a tumor 8. Recurrent inflammatory reactions result in progressive acinar destruction with fibrous replacement and sialectasis.
Patients with chronic sialadenitis should be evaluated with a history, physical examination, and possibly imaging, and the underlying pathology should be treated 9. Patients typically present with recurrent or low-grade swelling and tenderness of the affected gland, especially when eating. Physical examination may reveal enlargement of the gland early on, but this may reverse in later stages of the disease. Massaging the gland toward the orifice often does not produce visible saliva. Workup should focus on identifying a predisposing factor, such as a calculus or stricture. If no cause is found, treatment is conservative and should consist of sialagogues, massage, hydration, and anti-inflammatory medications. In severe cases, excision of the gland is safe and effective 10, with a low incidence of xerostomia.
Recurrent parotitis of childhood
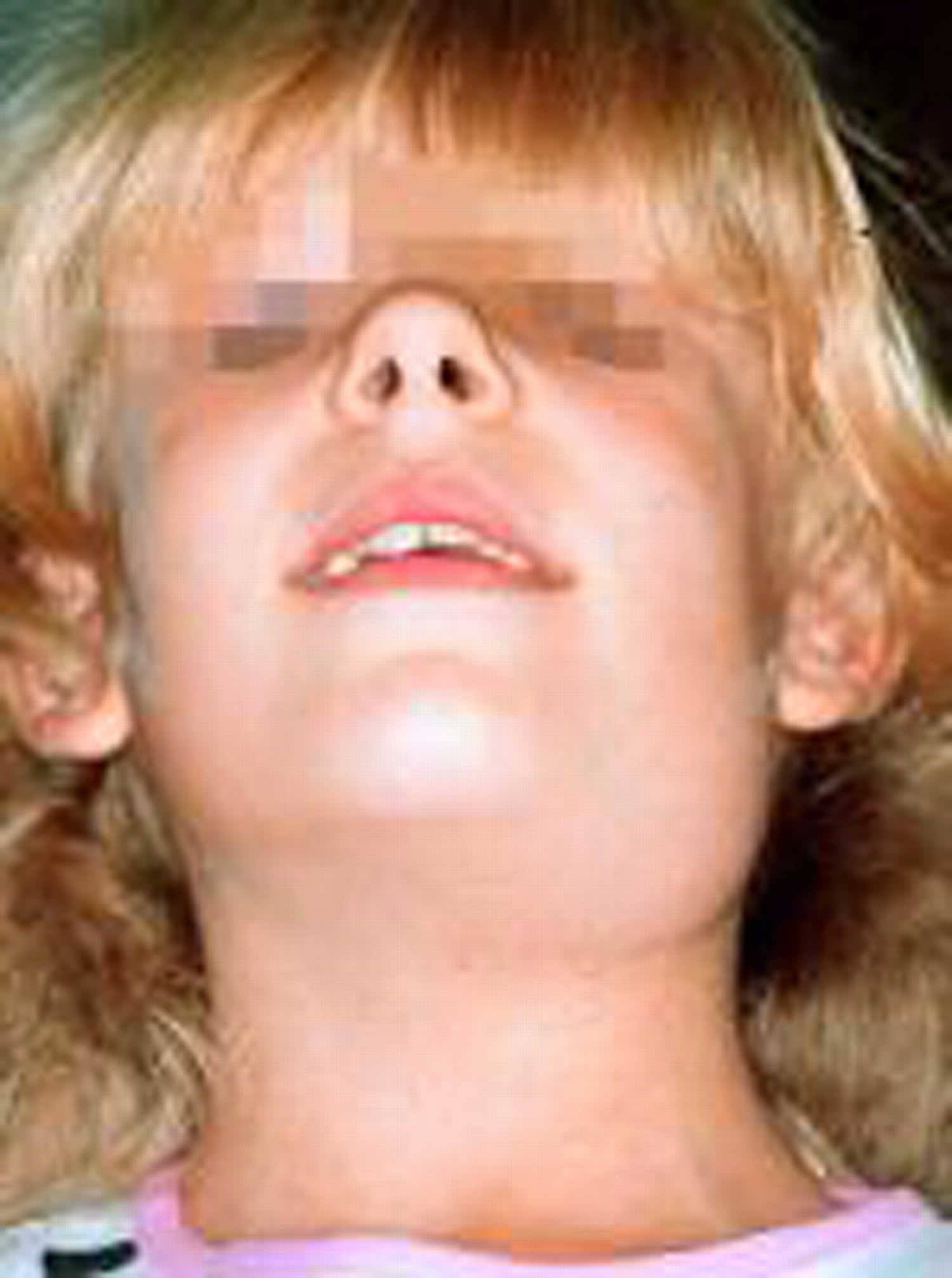
Recurrent parotitis of childhood is an inflammatory condition of the parotid gland characterized by recurrent episodes of swelling and pain 6. The cause of this disorder is not known. Children typically present with recurrent episodes of acute or subacute parotid gland swelling with fever, malaise, and pain (Figure 3). The disorder is usually unilateral, but can affect both sides. Episodes may last days to weeks and occur every few months. Treatment consists of supportive care with adequate hydration, gland massage, warm compresses, sialagogues, and antibiotics. Sialendoscopy has been shown to decrease the frequency and severity of episodes 11. Recurrent parotitis of childhood usually resolves spontaneously with puberty, and surgery is rarely required.
Figure 3. Recurrent parotitis of childhood
Sialadenitis causes
Sialadenitis usually occurs after salivary gland hyposecretion or salivary duct obstruction but may develop without an obvious cause. Poor oral hygiene can contribute to getting sialadenitis.
The major salivary glands are the parotid, submandibular, and sublingual glands. Sialadenitis is most common in the parotid gland and typically occurs in:
- Patients in their 50s and 60s
- Chronically ill patients with xerostomia
- Patients with Sjögren syndrome
- Adolescents and young adults with anorexia
The most common causative organism is Staphylococcus aureus; others include streptococci, coliforms, and various anaerobic bacteria.
Inflammation of the parotid gland can also develop in patients who have had radiation therapy to the oral cavity or radioactive iodine therapy for thyroid cancer 12. Although sometimes described as sialoadenitis, this inflammation is rarely a bacterial infection, particularly in the absence of fever.
Sialadenitis symptoms
Symptoms of sialadenitis include:
- Enlargement, tenderness, and redness of one or more salivary glands
- Fever (when the inflammation leads to infection)
- Decreased saliva (a symptom of both acute and chronic sialadenitis)
- Pain while eating
- Dry mouth (xerostomia)
- Reddened skin
- Swelling in the cheek and neck region
If you notice any of these symptoms you should seek medical advice from your doctor. He or she may refer you to an otolaryngologist.
Sialadenitis diagnosis
Sialadenitis is usually diagnosed though a physical examination and a history of your symptoms. CT, ultrasonography, and MRI may help identify the cause. Sometimes, the salivary glands may need to be examined with a scope.
Sialadenitis treatment
Sialadenitis is usually first treated with an antibiotic. You will also be advised of other treatments to help with the pain and increased saliva flow. These include drinking lemon juice or sucking hard candy, using warm compresses, and gland massages.
If your sialadenitis has created an abscess, that will need to be drained also.
In rare cases, surgery may also be needed.
Sialadenitis prognosis
Without proper treatment, sialadenitis can develop into a severe infection, especially in elderly or sick people. It is important to see a doctor right away if you have any of the symptoms.
References- McQuone SJ. Acute viral and bacterial infections of the salivary glands. Otolaryngol Clin North Am. 1999;32(5):793–811.
- Berndt AL, Buck R, von Buxton RL. The pathogenesis of acute suppurative parotitis: an experimental study. Am J Med Sci. 1931;182(5):639–649.
- Brook I, Frazier EH, Thompson DH. Aerobic and anaerobic microbiology of acute suppurative parotitis. Laryngoscope. 1991;101(2):170–172.
- Brook I. Diagnosis and management of parotitis. Arch Otolaryngol Head Neck Surg. 1992;118(5):469–471.
- Bozzato A, Hertel V, Bumm K, Iro H, Zenk J. Salivary simulation with ascorbic acid enhances sonographic diagnosis of obstructive sialadenitis. J Clin Ultrasound. 2009;37(6):329–332.
- Salivary Gland Disorders. Am Fam Physician. 2014 Jun 1;89(11):882-888. https://www.aafp.org/afp/2014/0601/p882.html
- Saunders JR Jr, Hirata RM, Jaques DA. Salivary glands. Surg Clin North Am. 1986;66(1):59–81.
- Zou ZJ, Wang SL, Zhu JR, Wu QG, Yu SF. Chronic obstructive parotitis. Report of ninety-two cases. Oral Surg Oral Med Oral Pathol. 1992;73(4):434–440.
- Rogers J, McCaffrey TV. Inflammatory disorders of the salivary glands. In: Flint PW, Haughey BH, Lund VJ, et al., eds. Cummings Otolaryngology Head and Neck Surgery. 5th ed. Philadelphia, Pa.: Mosby Elsevier; 2010: 1151–1161.
- O’Brien CJ, Murrant NJ. Surgical management of chronic parotitis. Head Neck. 1993;15(5):445–449.
- Quenin S, Plouin-Gaudon I, Marchal F, Froehlich P, Disant F, Faure F. Juvenile recurrent parotitis: sialendoscopic approach. Arch Otolaryngol Head Neck Surg. 2008;134(7):715–719.
- Erkul E, Gillespie MB: Sialendoscopy for non-stone disorders: the current evidence. Laryngoscope Investig Otolaryngol 1(5):140-145, 2016. doi: 10.1002/lio2.33