Sialocele
Sialocele is a localized accumulation of saliva in the soft tissue surrounding a salivary gland that typically occurs 1 – 2 weeks after injury to the excretory duct or gland, most frequently in association with sharp force trauma or following parotid surgery 1. Parotid sialocele is defined as an accumulation of saliva in the subcutaneous tissue around the salivary gland or duct 2. This occurs because of blunt or penetrating trauma to the parotid gland or duct or as a complication of surgery 3. Untreated sialocele may result in persistent painful facial swelling and cutaneous fistula formation 4.
Sialocele clinical presentation includes that of a painless swelling around the parotid gland or duct and may be complicated by fistula formation and infection 3. The typical age at presentation was between 32 and 88 years of age (mean age of presentation 52 years). Though parotid sialoceles and fistulas are two different clinical entities, a parotid sialocele may progress to a parotid fistula. Hence, early appropriate treatment of a sialocele is recommended. The incidence of sialocele/fistula development has been reported to be between 2 and 6.4% in patients undergoing partial superficial parotidectomy 3.
At present, definitive evidence‐based treatment guidelines for sialocele and fistula management do not exist. In the management of parotid sialocele or fistula, various conservative and surgical methods have been described 5. Some studies have described the use of Botulinum toxin A (Botox A) for the management of parotid sialocele and fistula. This is a less invasive and potentially equally effective option. Botox A is a neurotoxin which inhibits presynaptic acetylcholine release and hence saliva production from parotid glandular tissue 3. Its uses for facial cosmesis are widely documented 6. It has minimal side effects when injected locally. Few studies have described the use of Botox for the management of parotid sialocele. There is therefore a need to further explore the use, benefit, method of administration and optimal therapeutic dose of Botox A in the management of parotid sialoceles 7.
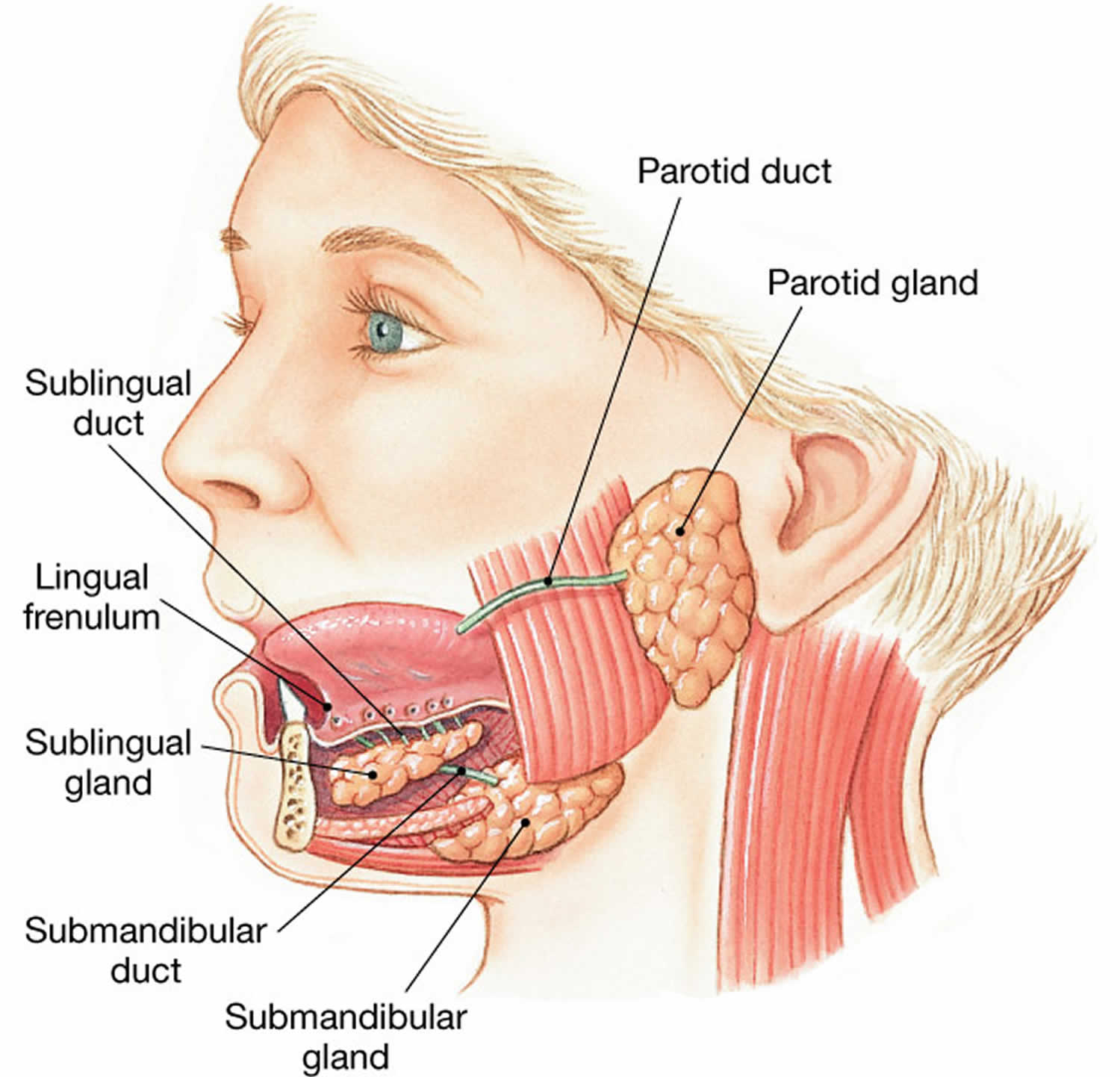
Figure 1. Parotid gland and duct
Sialocele causes
Sialocele can be caused due to trauma, surgery or infection. The majority of sialoceles and fistulas presented as a complication of surgery (77%) with the remaining cases occurring as a result of trauma 5. Surgery performed included parotidectomy for tumor excision and Mohs micrographic surgery. Surgery was performed for diagnosis of squamous cell carcinoma in most cases.
Sialocele symptoms
A sialocele presents as a swelling in the preauricular region which typically develops 8 to 14 days after the injury 8. In postoperative period it is frequently misdiagnosed as hematoma. On palpation the lesion is soft and mobile. No erythema of the skin, no fever, no supuration are observed 8. The patient can complaint of pressure sensation in the area 4.
Sialocele diagnosis
The diagnosis of sialocele usually is not difficult if the history of possible parotid duct injury is taken into account. The most common diagnostic test is the salivary amylase level, which is elevated. This is obtained either via aspiration of the sialocele, or by collection of clear fluid draining from the fistula. CT scan and ultrasound is also helpful in some cases to confirm the diagnosis.
The amylase identification in the liquid obtained via needle aspiration shows levels that exceed 10000 u/l 9. CT shows a single or multiloculated cystic lesion with smooth margins and internal density lower than that of surrounding tissues. The differential CT diagnosis includes retention cyst, sialodochitis, branchial cleft cyst and lymphoepitelial cyst 4. If sialocele is left untreated the swelling increases progressively and cutaneous fistula formation may occur.
Sialocele treatment for humans
There is no consensus regarding the management of sialocele. The management of salivary duct injury and resultant sialocele remains controversial. Various conservative and surgical approaches have been described such as multiple percutaneous needle aspirations, application of pressure dressings, antisialogogue therapy or botulinum toxin injection 10. The skin incision and drainage are often unsuccessful because of the recurrence of accumulation of fluid 11. If these techniques don’t resolve the problem then radiotherapy of salivary gland and surgical treatment have been proposed. Surgical options include ligation of parotid duct, primary repair of the duct, different drainage systems and even superficial or total parotidectomy/submaxilectomy. The repair of duct in cases of sialocele is considered to be challenging due to the presence of a fibrous scar over the area of injury and interposition of flap tissue.
The method of intraoral fistula surgical creation was re-ported by Morestin in 1917 for the management of parotid fistula after facial wounds. This method has been recently described for treatment of post-traumatic sialocele 12. There was no consensus about either the type of catheter to use [pigtail, silastic drains, Jackson Pratt, venous catheter] or the time to maintain it in the oral mucosa [four weeks, two months].
In general the management of the salivary duct injury depends on the age of injury, site of injury and mechanism of injury. Three methods generally employed are based on primary repair of the duct, creation of oral fistula and suppression of parotid gland function 9. It is considered that parotid duct injuries are best repaired early at the time of injury 9. In case of oral cancer patients the whole distal end of Stensen’s duct is resected in block with tumor at the time of surgery, thus no direct repair is possible. The technique of diversion of the Stensen’s duct into the mouth could be useful at the time of resection of oral mucosa if the iatrogenic injury to its distal end has been anticipated at the time of surgical planning 10. Another technique applied intraoperatively is the creation of oral fistula.
References- Giant post-traumatic parotid gland sialocele and fistula: A case report and review of the literature. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology Volume 27, Issue 1, January 2015, Pages 135-139 https://doi.org/10.1016/j.ajoms.2013.11.002
- Lovato A, Restivo DA, Ottaviiano G, Marchese‐Ragona R. Botulinum toxin therapy: functioning silencing of salivary disorders. Acta Otorhinolaryngol Ital. 2017;32:168‐177.
- Lee YC, Park GC, Lee J‐W, Eun YG, Kim SW. Prevalence and risk factors of sialocele formation after partial superficial parotidectomy: a multi‐institutional analysis of 357 consecutive patients. Head Neck. 2016;38(suppl 1):E941‐E944. 10.1002/hed.24130
- Canosa A, Cohen M, Dent M. Post-traumatic parotid sialocele: re-port of two cases. J Oral Maxillofac Surg. 1999;57:742-5.
- Maharaj S, Mungul S, Laher A. Botulinum toxin A is an effective therapeutic tool for the management of parotid sialocele and fistula: A systematic review. Laryngoscope Investig Otolaryngol. 2020;5(1):37-45. Published 2020 Jan 23. doi:10.1002/lio2.350 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7042652
- Nagi R, Kantharaj YBR, Nagaraju R, Reddy SJ. Sialocele of parotid duct: report of a case with review of the literature. J Diagn Res. 2016;10(2):04‐05.
- Marchese‐Ragona R, Blotta P, Pastore A, Tugnoli V, Eleopra R, De Grandis D. Management of parotid sialocele with botulinum toxin. Laryngoscope. 1999;109:1344‐1346.
- Kulyapina, Alena & Lopez-de-Atalaya, Javier & Ochandiano-Caicoya, Santiago & Navarro-Cuellar, Carlos & Navarro-Vila, Carlos. (2014). Iatrogenic salivary duct injury in head and neck cancer patients: Report of four cases and review of the literature. Journal of clinical and experimental dentistry. 6. e291-4. 10.4317/jced.51438
- Steinberg MJ, Herrera AF. Management of parotid duct injuries. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:136-41.
- Bomeli SR, Shaun CD, Johnson JT, Walvekar RR. Management of salivary flow in head and neck cancer patients: a systematic re-view. Oral Oncology. 2008;44:1000-8.
- Capaccio P, Cuccarini V, Benicchio V, Minorati D, Spadari F, Ottaviani F. Treatment of iatrogenic submandibular sialocele with botulinium toxin Case report. Br J Oral and Maxillofac Surg. 2007;45:415-7.
- Gahir D, Clifford N, Yousefpour A., Avery C. A novel method of managing persistent parotid sialocele. Br J Oral Maxillofac Surg. 2001;49:491-2.