Smooth tongue
Smooth tongue also known as atrophic glossitis or atrophic papillae, is glossy smooth appearance of the entire tongue surface with a red or pink background. Smooth tongue is a condition in which the normal rough surface (papillae) of the tongue shrinks or disappears, making the tongue look bald or shiny and thin. Smooth tongue is due to reduction in number and/or size of the filiform papillae. Smooth tongue always occurs when there is a loss of 50% of fungiform and filiform papillae on the dorsum of the tongue 1. Without this rough surface, the tongue may be tender and sensitive to spicy foods.
Smooth tongue is primarily a manifestation of underlying conditions and is a classic sign of nutritional deficiencies related to lack of iron, folic acid, vitamin B12, riboflavin, and niacin in the diet over a long period of time and warrants thorough diagnostic evaluation 2. Other causes include systemic infection (e.g., syphilis), localized infection (e.g., oral candidiasis), amyloidosis, celiac disease, protein-calorie malnutrition, AIDS, diabetes, heart failure, chemical irritation, drug reaction, pernicious anemia and xerostomia triggered by some medications and Sjögren syndrome, with high prevalence inpatients hospitalized 3, 4, 5, 6. Smooth tongue caused by nutritional deficiency often causes a painful sensation in the tongue. Often, smooth tongue and mucosal pallor may appear in the patient’s mouth while its main systemic disease remains asymptomatic 7. The pale mucous membranes occur when the hemoglobin concentration is below 9–10 g/dL. On the other hand, there is no record of studies correlating levels of hemoglobin and the appearance of smooth tongue. Elderly and debilitated patients are more affected by smooth tongue. A study by Bohmer 8 demonstrated that the prevalence in the elderly inpatients was 32%. On the other hand, the prevalence is 9.2% in the elderly living in their households. Treatment includes replacement of the missing nutrient or treatment of the underlying condition 9.
Another condition that affects the tongue and produces lingual papillae loss is geographic tongue or benign atrophic glossitis. A geographic tongue has localized areas of smoothening, but not sufficient to warrant use of the term smooth tongue. Geographic tongue occurs when patches of the rough surface (papillae) of the tongue disappear (sometimes rapidly) with irregular margins and elevated keratotic edges similarto maps in the back of the tongue. The absence of papillae makes those parts of the tongue appear to look like a map, with smooth, bright red areas. Another striking feature of geographic tongue is that the lesions migrate 10. The cause of geographic tongue is not known that affects 2% of the population, although it could be linked with allergies. In some cases geographic tongue causes soreness and burning. There is no specific treatment, although home treatment measures may relieve the soreness of geographic tongue. It may take a month for the tongue to regain its normal texture.
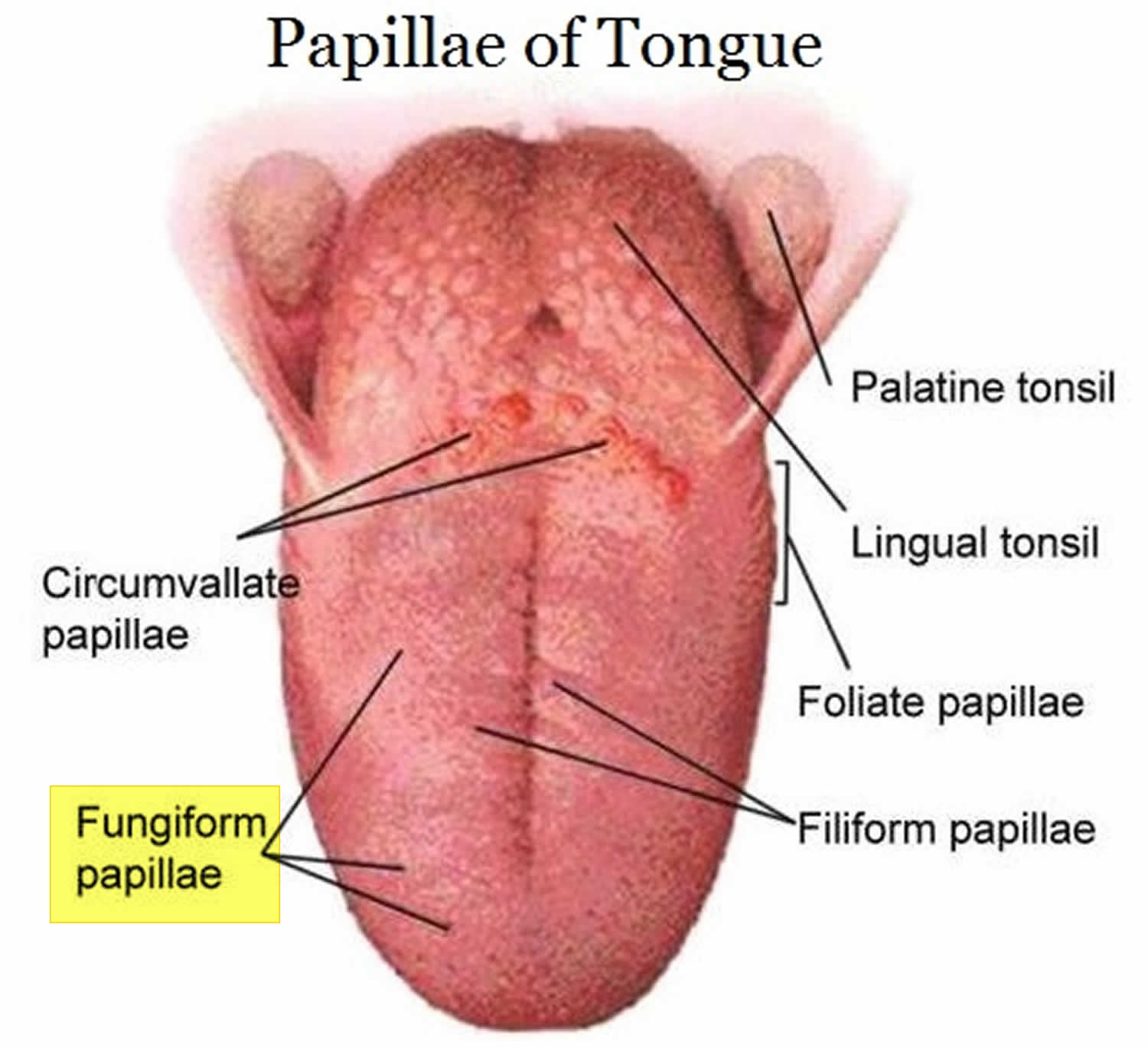
Figure 1. Tongue papillae
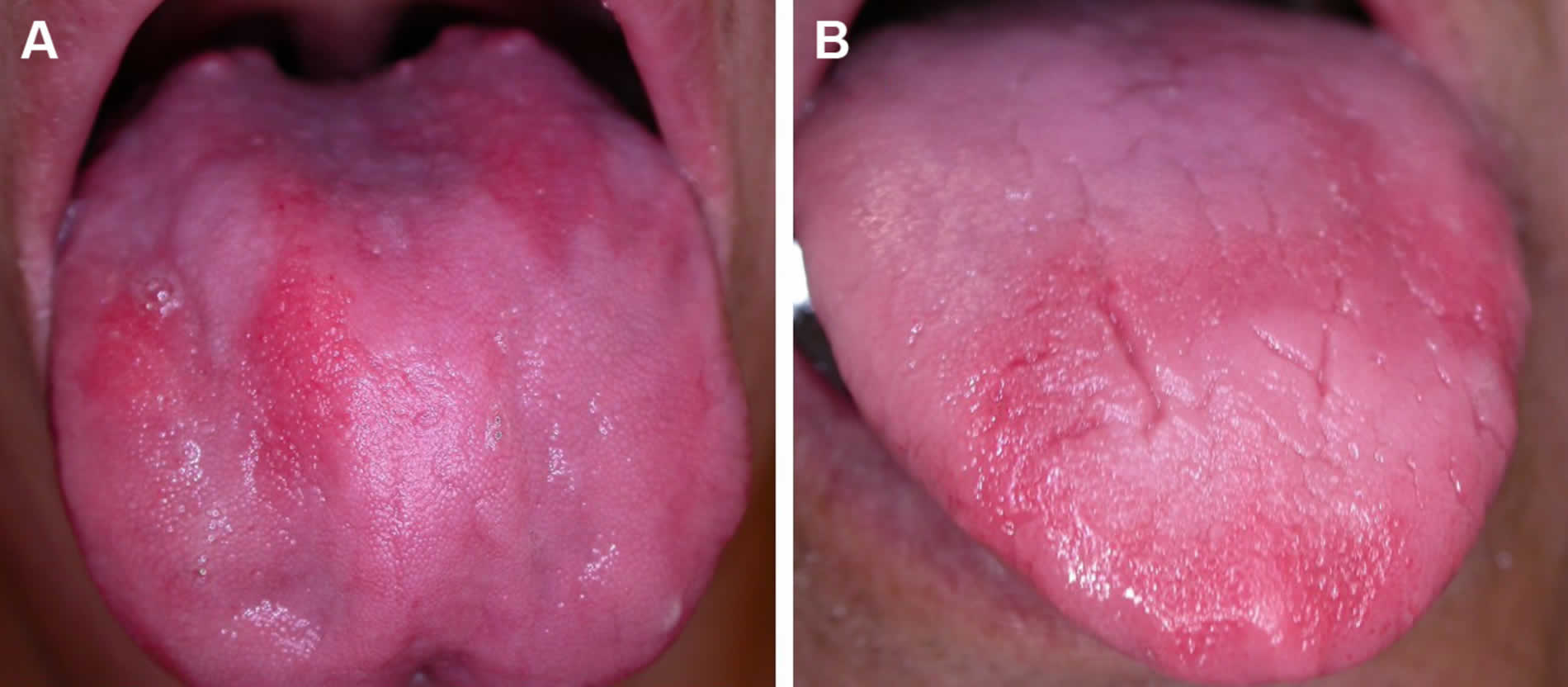
Figure 2. Smooth tongue in a HIV positive patient with severe anemia
Figure 3. Smooth tongue in patient with cancer-related severe anemia
Figure 4. A classic smooth, beefy red tongue from vitamin B12 deficiency
Footnote: (A and B) Linear or band-like “beefy red” patches on the lingual dorsum in B12 deficiency
Smooth tongue causes
The most common cause of a smooth tongue is the use of dentures. Nutritional deficiencies include iron, folate and vitamin B12 deficiency. Vitamin B12 deficiency will also make the tongue sore and beefy-red in color. Glossitis, by causing swelling of the tongue, may also cause the tongue to appear smooth. Among women, low-estrogen states may cause a “menopausal glossitis”.
Conditions associated with smooth tongue 11, 12, 13:
- AIDS (acquired immune deficiency syndrome)
- Amyloidosis
- Celiac disease
- Chemical irritants
- Diabetes
- Drug reactions
- Heart failure
- Local infections (oral candidiasis)
- Nutritional deficiencies (e.g., iron, folic acid, vitamin B12, riboflavin, niacin)
- Pernicious anemia
- Protein-calorie malnutrition
- Sarcoidosis
- Sjögren syndrome
- Systemic infections (e.g., syphilis)
- Xerostomia triggered by some medications
- Vesiculoerosive diseases (e.g., pemphigoid, pemphigus vulgaris, erythema multiforme, Stevens-Johnson syndrome).
Smooth tongue symptoms
The most common symptoms of glossitis include pain in the tongue, redness, swelling of the tongue and smooth surface of the tongue.
Smooth tongue diagnosis
When evaluating a patient with smooth tongue (atrophic glossitis), a thorough history is an absolute necessity. Specifics include an overall nutritional status and any dietary restrictions, tobacco, and alcohol use, and any fluctuation of symptoms with food or environmental exposure. A thorough past medical history should include concurrent immunosuppressive conditions, cancer history, as well as any autoimmune or endocrine conditions.
The diagnosis of smooth tongue (atrophic glossitis) is based on the oral mucosal, especially the tongue. A careful evaluation by a physician is required for correct diagnosis because it can be a manifestation of a systemic condition 14. To confirm the diagnosis of a systemic condition, your doctor should request some additional blood tests.
Physical exam
The examination of the tongue is an essential part of the physical examination and is a component of the overall oral cavity examination. The examiner should note the appearance of the tongue surface (dorsal and ventral), as well as the character of the mucosa (wet, dry, erythematous, leukoplakia, etc.). Any lesions visible on the tongue should be noted, as well as the overall dental health. Chronic friction from jagged teeth can lead to mucosal changes and even ulcerations of the tongue that the examiner must distinguish from primary tongue pathology. The language and floor of mouth should be palpated to assess for tenderness or palpable lesions. A thorough head and neck exam are also necessary to note any lymphadenopathy.
Blood tests used to diagnose some common types of anemia may include:
- Blood levels of iron, vitamin B12, folic acid, and other vitamins and minerals
- Complete blood count
- Reticulocyte count
Other tests may be done to find medical problems that can cause anemia.
Anemia due to iron deficiency is the most common type of anemia with women being more frequently affected than men 15. Hematological changes are common complications of HIV infection. Several factors play roles in thedevelopment of anemia in these patients include chronic diseases, opportunistic infections, nutritional deficiency andtoxicity produced by some drugs 16.
Smooth tongue treatment
Smooth tongue treatment includes replacement of the missing nutrient or treatment of the underlying pathological condition 2. The primary aim is of course to find the cause of the anemia and correct it if possible. As anemia is a major cause of atrophic glossitis, treatment of this condition is important to repair the loss of tongue papillae.
References- Cunha SFC, Melo DA, Braga CBM, Vannucchi H, Cunha DF.Papillary atrophy of the tongue and nutritional status ofhospitalized alcoholics. An Bras Dermatol 2012;87(1):84–89.
- Common Tongue Conditions in Primary Care. Am Fam Physician. 2010 Mar 1;81(5):627-634. https://www.aafp.org/afp/2010/0301/p627.html
- Byrd JA, Bruce AJ, Rogers RS III. Glossitis and other tongue disorders. Dermatol Clin. 2003;21(1):123–134.
- Mirowski GW, Mark LA. Oral disease and oral-cutaneous manifestations of gastrointestinal and liver disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 8th ed. Philiadephia, Pa.: Saunders; 2006: 443–459.
- Pastore L, Carroccio A, Compilato D, Panzarella V, Serpico R, Lo Muzio L. Oral manifestations of celiac disease. J Clin Gastroenterol. 2008;42(3):224–232.
- Terai H, Shimahara M. Atrophic tongue associated with Candida. J Oral Pathol Med. 2005;34(7):397–400.
- Pontes HAR, Conte Neto N, Fereira JB, Fonseca FP, VallinotoGM, Pontes FSR, Pinto Jr DS. Oral manifestations of vitamin B12deficiency: case report. J Can Dent Assoc 2009;75(7):533–537.
- Bohmer T, Mowé M. The association between atrophic glossitis and protein-calorie malnutrition in old age. Age Ageing 2000;29:47–50.
- Lee HJ, Jo DY. Images in clinical medicine. A smooth, shiny tongue. N Engl J Med. 2009;360(6):e8.
- Kumar D, Das A, Gharami RC. Benign migratory glossitis. Indian Pediatr 2013;50(12):1178
- Shulman JD, Beach MM, Rivera-Hidalgo F. The prevalence of oral mucosal lesions in U.S. adults: data from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Dent Assoc. 2004;135(9):1279–1286.
- Wright BA, Fenwick F. Candidiasis and atrophic tongue lesions. Oral Surg Oral Med Oral Pathol. 1981;51(1):55–61.
- Segal LM, Stephenson R, Dawes M, Feldman P. Prevalence, diagnosis, and treatment of ankyloglossia: methodologic review. Can Fam Physician. 2007;53(6):1027–1033.
- Byrd JA, Bruce AJ, Rogers RS. Glossitis and other tonguedisorders. Dermatol Clin 2003;21:123–134.
- Wu YC, Wang YP, Chang YF, Cheng SJ, Chen HM, Sun A. Oral manifestations and blood profile in patients with irondeficiency anemia. J Formos Med Assoc 2014;113–122.
- Enawgaw B, Alem M, Addis Z, Melku M. Determination of hematological and immunological parameters among HIVpositive patients taking highly active antiretroviral treatment and treatment naïve in the antiretroviral therapyclinic of Gondar University Hospital, Gondar, NorthwestEthiopia: a comparative cross-sectional study. BMC Hematol 2014;14:8.