What is soy lecithin
Soy lecithin is a by-product from the processing of soybean oil. Soy lecithin is widely used in the food industry as an emulsifier and stabilizing agent in the production of foods such as margarine, mayonnaise, chocolate and baked goods 1. Lecithin is the common name for a series of related compounds called phosphatidylcholines. Lecithins are mixtures or fractions of phosphatides obtained by physical procedures from animal or vegetable foodstuffs found mainly in egg yolks, soy (soybeans), organ and lean meats, fish and coleseeds. The total phospholipids contained in 100 g of egg yolk and soybeans are 31.8 g and 20.8 g, respectively 2, and the normal dietary intake of phospholipids is estimated as 2–8 g per day 3. Crude lecithin is a mixture of mainly phospholipids (up to approximately 75 % for de-oiled lecithin), i.e., phosphatidylcholine, phosphatidylethanolamine and phosphatidylinositol and a smaller fraction of glycolipids, neutral lipids, and carbohydrates, that can be extracted from plant or animal food substances 4. Dietary crude lecithin is a source of active compounds as it is digested into fatty acids, lysophospholipids, phosphatidic acid, glycerol, monoglycerides, and other compounds, including choline and ethanolamine. Lecithin has low solubility in water, but is a very good emulsifier and is also a source of active compounds, such as choline, that can be released from phosphatidylcholine. Lecithin is a choline-containing phospholipid and is the major dietary source of choline. It has been shown to increase serum choline levels more effectively than orally administered choline 5. Wurtman et al. 5 found that oral lecithin is considerably more effective in raising human serum-choline levels than an equivalent quantity of choline chloride. 30 minutes after ingestion of choline chloride (2·3 g free base), serum-choline levels rose by 86% and returned to normal values within 4 hours; 1 hour after lecithin ingestion, these levels rose by 265% and remained significantly raised for 12 hours. Lecithin may therefore be the method of choice for accelerating acetylcholine synthesis by increasing the availability of choline, its precursor in the blood.
There are three forms of lecithins (i) regular liquid lecithins, derived from soybean, rapeseed and sunflower; (ii) hydrolysed liquid lecithins, derived from soybean and sunflower; (iii) de‐oiled lecithins powder derived from soybean and sunflower.
Soy lecithin allergy
Soybean allergy is one of the most common food allergies especially among children. Approximately 0.4% of children are allergic to soy but about half of them spontaneously recover by the age of 7 years 6. Allergic reactions to soy lecithin have been previously reported in the literature: occupational asthma in bakers 7, chronic diarrhea in a child 8, and anaphylactic reaction in a 40-year-old woman treated with an inhalatory drug 9. In general, soy allergy is not as common as cow’s milk allergy, even in atopic children. Bruno et al. 10 found a prevalence of 1.2% in a cohort of 505 children suffering from allergic diseases and 0.4% in 243 children who had been fed soy protein formula in the first 6 months of life for supposed prevention of allergic diseases. Patients with soy allergy show a wide range of immunoglobulin E (IgE) and non IgE-mediated clinical symptoms 11. For these reasons, the Food Allergen Labeling and Consumer Protection Act in the US, from January 1, 2006, mandates labeling of all ingredients derived from commonly allergenic foods, including soybeans, with the exception of highly refined oils 12. The Food Allergen Labeling and Consumer Protection Act also requires the labeling of soy lecithin because it is derived from soybeans and may contain a number of IgE-binding proteins, possibly representing a source of hidden allergens 13. Soy lecithin is not only used in the food industry, as an antioxidant, but it is widely used in topical skin care products, in various drugs administered either topically, orally, intravenously or by inhalation, as an emulsifier 14.
In 2014, the European Food Safety Authority Panel on Dietetic Products, Nutrition and Allergies 15 prepared a scientific opinion on the evaluation of allergenic foods and food ingredients for labeling purposes where the allergenicity of egg and soya lecithins were considered. The possibility of residual allergenicity in food products manufactured using egg lecithin has been reported in a double‐blind placebo‐controlled food challenge. Heat denaturation and other food‐processing treatments do not reliably reduce the allergenicity of egg. Minimum eliciting doses (MEDs) of ingested egg proteins reported to trigger objective reactions in clinical studies range from few micrograms to milligrams.
The prevalence of clinically confirmed soya allergy in unselected populations in Europe appears to be low, although available studies are scarce. The sodium dodecyl sulfate polyacrylamide gel electrophoresis protein pattern of the standard soya lecithin is very similar to that of soya flour. The lowest minimum eliciting dose reported in soya‐allergic patients undergoing double‐blind placebo‐controlled food challenge was 0.2 mg of soya protein, although the majority of patients only reacted to higher doses 15.
Soybeans and eggs and products thereof (including lecithins) are listed as substances or products causing allergies or intolerances which indication as allergens is mandatory food information.
Table 1. Presentation of soy allergy (and cow’s milk allergy)
| IgE-mediated | |
|---|---|
| Cutaneous | Urticaria Angioedema |
| Gastrointestinal | Oral itching and abdominal pain Nausea and vomiting Diarrhea |
| Respiratory | Rhinoconjunctivitis Wheeze and asthma exacerbation Laryngeal edema |
| Systemic | Anaphylaxis |
| Mixed IgE- and non-IgE mediated | |
| Cutaneous | Atopic dermatitis |
| Gastrointestinal | Eosinophilic esophagitis and gastroenteritis |
| Non-IgE mediated | |
| Gastrointestinal | Dietary protein enterocolitis/proctitis/proctocolitis Protein-losing enteropathy Gastroesophageal reflux* Colic* Constipation* |
| Respiratory | Pulmonary hemosiderosis (i.e. Heiner syndrome) (mostly caused by milk allergy) |
Allergic reactions to soy are typically mild, but all reactions can be unpredictable. Although rare, severe and potentially life-threatening reactions can also occur. If you have a soy allergy, keep an epinephrine auto-injector (such as an EpiPen®, Auvi-Q™ or Adrenaclick®) with you at all times. Epinephrine is the first-line treatment for anaphylaxis.
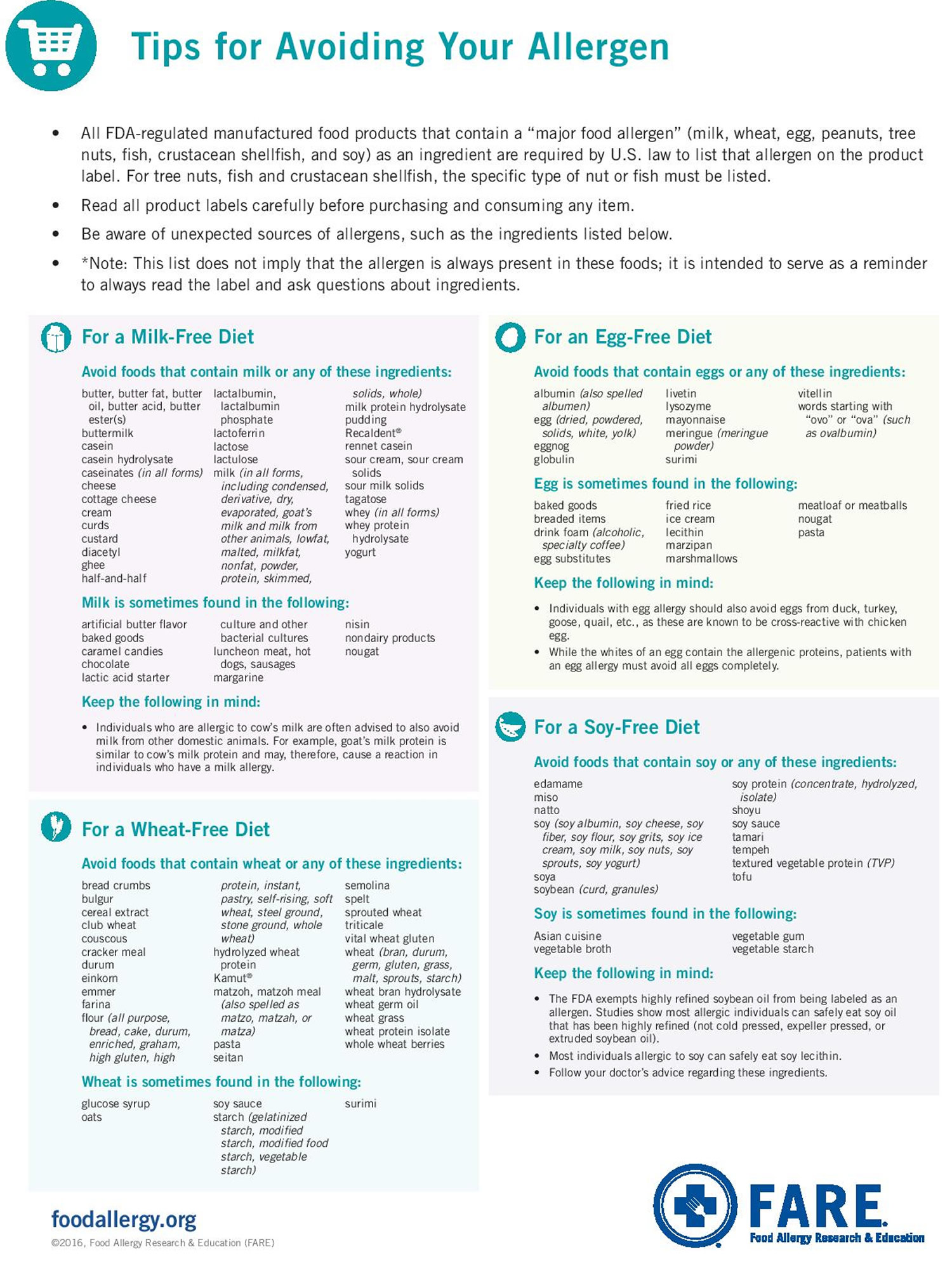
Avoiding Soy
The close resemblance and resultant cross-reactivity between proteins from soy and other related plants like peanut, and the lack of predictive values for clinical reactivity, often make the diagnosis of soy allergy far more challenging. Furthermore, diagnostic tests for non-IgE-mediated manifestations are lacking. Avoidance of the culprit food protein is the mainstay of therapy, although there is a growing body of evidence on the efficacy of investigational new therapies such as oral or sublingual immunotherapy.
To prevent a reaction, it is very important that you avoid soy and soy products. Always read food labels and ask questions about ingredients before eating a food that you have not prepared yourself.
Soybeans alone are not a common food in American diets. Instead, they are widely used in processed food products. Eliminating all those foods can result in an unbalanced diet. A dietitian can help you plan for proper nutrition.
Soy is one of the eight major allergens that must be listed on packaged foods sold in the U.S., as required by federal law.
Avoid foods that contain soy or any of these ingredients:
- Cold-pressed, expelled or extruded soy oil*
- Edamame
- Miso
- Natto
- Shoyu
- Soy (soy albumin, soy cheese, soy fiber, soy flour, soy grits, soy ice cream, soy milk, soy nuts, soy sprouts, soy yogurt)
- Soya
- Soybean (curd, granules)
- Soy protein (concentrate, hydrolyzed, isolate)
- Soy sauce
- Tamari
- Tempeh
- Textured vegetable protein
- Tofu
*Highly refined soy oil is not required to be labeled as an allergen. Studies show that most people with soy allergy can safely eat highly refined soy oil as well as soy lecithin. If you are allergic to soy, ask your doctor whether you need to avoid soy oil or soy lecithin.
But avoid cold-pressed, expelled or extruded soy oil—sometimes called gourmet oils. These ingredients are different and are not safe to eat if you have a soy allergy.
Soy is sometimes found in the following:
- Asian cuisine (including Chinese, Indian, Indonesian, Thai and Vietnamese)—even if you order a soy-free item, there is high risk of cross-contact
- Vegetable gum
- Vegetable starch
- Vegetable broth
Cross-contact occurs when an allergen is inadvertently transferred from a food containing an allergen to a food that does not contain the allergen. Cooking does not reduce or eliminate the chances of a person with a food allergy having a reaction to the food eaten.
Examples of cross-contact and how to avoid it:
Say a knife that has been used to spread peanut butter is only wiped off before being used to spread jelly. There could be enough peanut protein remaining on the knife to cause a reaction in a person who has a peanut allergy. All equipment and utensils must be cleaned with hot, soapy water before being used to prepare allergen-free food.
Even a trace of food on a spoon or spatula that is invisible to you can cause an allergic reaction.
Some Unexpected Sources of Soybeans and Soy Products:
- Baked goods
- Canned broths and soups
- Canned tuna and meat
- Cereals
- Cookies
- Crackers
- High-protein energy bars and snacks
- Infant formulas
- Low-fat peanut butter
- Pet food
- Processed meats
- Sauces
- Soaps and moisturizers
Allergens are not always present in these foods and products, but soy can appear in surprising places. Again, read food labels and ask questions if you’re ever unsure about an item’s ingredients.
Figure 1. Tips for Avoiding Food Allergens
 [Source 17
[Source 17
Will children outgrow a soy allergy?
About 0.4 percent of children are allergic to soy. Studies show an allergy to soy usually occurs early in childhood and often is outgrown by age three. The majority of children with soy allergy will outgrow the allergy by age 10 18.
With soy allergy, most people become tolerant over time, although as with cow’s milk allergy, it may take longer than previously thought. Savage et al. 18 retrospectively described the natural history of 133 patients allergic to soy (88% with concomitant peanut allergy) with a variety of clinical reactions and found that approximately 50% of the children outgrew their allergy by age 7 years and 69% by 10 years. By age 6 years, peak soy-specific IgE level less than 10 kUA/L was predictive of >50% chance of outgrowing allergy, but peak level more than 50 kUA/L suggested <20% chance of tolerance development. Although soy allergy is commonly considered to have an early onset, the study identified a subset of patients with late onset soy allergy whose symptoms started after tolerating soy on a regular basis in their diet. Savage et al. 18 suggested that such late-onset soy allergy may be related to either birch pollen cross-reactivity or persistent peanut allergy, as indicated by a very high peanut-specific IgE levels at their last follow-up. Notably, the prevalence of soy sensitization progressively increased with age from 2% at age 2 years to 7% at 10 years in the German Multi-Center Allergy Study, which followed 1314 children from birth to age 13 19.
Food protein-induced enterocolitis responds well to dietary elimination of the offending food, with tolerance usually developing within 3 years of life 20, although rate of tolerance development varies between studies and populations. Occasionally food protein-induced enterocolitis may persist into the teenage years. Earlier reports suggested that within 2 years, 60% of milk and 20% of soy-induced food protein-induced enterocolitis resolves 21. Preliminary data on 76 subjects with food protein-induced enterocolitis shows that the majority of patients with milk food protein-induced enterocolitis become tolerant by 3 to 4 years, but the natural history was not as favorable for soy 22. However, a recent study by Korean investigators on 23 infants with milk food protein-induced enterocolitis reported that 64% tolerated milk at 10 months, and 92% tolerated soy at 10 months 23.
What is food protein-induced enterocolitis?
Food protein-induced enterocolitis is when dietary protein-induced syndromes of enteropathy and enterocolitis are not IgE-mediated, and typically present with profuse vomiting and diarrhea within 2–3 hours after ingestion of the offending allergen, causing profound dehydration and lethargy 24. Three quarters of infants with FPIES appear acutely ill, and about 15% have hypotension requiring hospitalization 20. Mehr et al. 25 reported that one quarter of acute food protein-induced enterocolitis syndrome episodes in young infants manifested with hypothermia less than 36°C. The diarrhea may have occult blood, and fecal smears reveal leukocytes and eosinophils. Chronic exposure to the offending allergen results in a less acute clinical presentation of failure to thrive and hypoalbuminemia 26. Sicherer et al reported that food protein-induced enterocolitis syndrome was elicited most often by cow milk and soy protein, with 7 of 16 patients having sensitivity to both 21. Similarly, Burks et al. 27 reported that 6 of 10 patients with food protein-induced enterocolitis syndrome reacted to both milk and soy. Preliminary data on 76 patients with food protein-induced enterocolitis syndrome showed cow milk was the trigger in 58% and soy in 47% of patients 22. Among children with milk-food protein-induced enterocolitis syndrome, 45% had soy-food protein-induced enterocolitis syndrome and among children with soy-food protein-induced enterocolitis syndrome, 56% had milk-food protein-induced enterocolitis syndrome.
Protein-induced allergic enterocolitis/proctitis/proctocolitis usually presents by 6 months of life in an otherwise well-appearing breastfed or formula-fed infant with blood-streaked, mucousy, loose stools and occasionally diarrhea 24. Cow milk and soy are the major causative foods. The majority of breastfed infants with allergic proctocolitis respond to maternal elimination of cow milk proteins, although some require the additional elimination of soy 28 or conversion to extensively hydrolyzed formula. Other causes, such as viruses, may have a similar presentation 29. Despite concerns regarding co-sensitization or allergy to soy in cow milk allergic subjects, soy-based formulas continue to be a management option for cow’s milk allergic infants with IgE-mediated reactions, especially above 6 months of age.
Lecithin in food
Lecithin is found in many animal and vegetable sources including beef liver, steak, eggs, peanuts, cauliflower, and oranges 30. Commercial sources for lecithin can come from soybeans, egg yolk, or brain tissue 31. Some commercial lecithin and lecithin supplements contain between 10% and 35% phosphatidylcholine 30.
Is soy lecithin bad for you?
According to the 2017 re-evaluation of lecithins as a food additive by the European Food Safety Authority 32, the European Food Safety Authority Panel concluded that there was no need for a numerical acceptable daily intake (ADI) for lecithins (E 322) and that there was no safety concern for the general population from more than 1 year of age at the refined exposure assessment for the reported uses of lecithins (E 322) as a food additive. The European Food Safety Authority Panel further concluded that there is no safety concern for the exposure to the choline from lecithins (E 322) as a food additive at use and use levels reported by industry 32. For infants (from 12 weeks up to 11 months of age), the European Food Safety Authority Panel concluded that there was no safety concern at the refined exposure assessment for the reported uses of lecithins (E 322) as a food additive and for the choline from lecithins (E 322) as a food additive at use and use levels reported by industry 32. For infants and young children consuming foods for special medical purposes, the European Food Safety Authority Panel concluded that there was no safety concern with respect to the refined exposure assessment for the reported uses of lecithins (E 322) as a food additive and for exposure to choline resulting from these uses of lecithins (E 322) 32. The present opinion deals with the re‐evaluation of lecithins (E 322) when used as a food additive and does not include lecithin supplement.
Lecithins (E 322) is an authorized food additive as emulsifying agents in the European Union 33 and in the U.S. Food and Drug Administration (FDA) has determined lecithin to be generally recognized as safe (GRAS) for addition to food 34. Lecithin has been widely used in foods (e.g., infant formula and chocolate) as a natural emulsifier to improve physical stability 35. In humans, dietary lecithins are hydrolysed by phospholipases to liberate choline which is rapidly absorbed and appears in plasma predominantly as free choline. The European Food Safety Authority Panel considered that dietary intakes of lecithins (E 322) from the regular diet could be estimated in average ranging from 4 to 71 mg/kg body weight per day across all population age groups 32.
The European Food Safety Authority Panel concluded that there was no need for a numerical acceptable daily intake (ADI) for lecithins (E 322) and that there was no safety concern for the general population from more than 1 year of age at the refined exposure assessment for the reported uses of lecithins (E 322) as a food additive.
Taking into consideration that:
- hydrolysed lecithins and choline are produced in the gut as a result of normal digestion of lecithins. Choline is rapidly absorbed and appears in plasma predominantly as free choline,
- choline is a precursor of the neurotransmitter acetylcholine,
- the content of choline, that can theoretically be released from phosphatidylcholine containing two linoleate groups, is up to 13.2%, and the measured content of choline from commercial lecithins (E 322) up to 3.4%,
- 13.2% release would result in exposure up to 23 mg choline/kg bw per day at the 95th percentile intake of lecithins in toddlers (brand loyal scenario),
total choline intake considering regular diet (estimated in average ranging from 4 to 18 mg/kg bw per day) across all population age groups and choline intake resulting from lecithins (E 322) used as a food additive are below the upper intake level (UL) for choline defined by the Institute of Medicine 36,
The European Food Safety Authority Panel concluded that there is no safety concern for the exposure to the choline from lecithins (E 322) as a food additive at use and use levels reported by industry 32.
However, the European Food Safety Authority Panel noted that, the use levels of lecithins (E 322) in food for infants under the age of 12 weeks and because these uses would require a specific risk assessment; therefore, the existing evaluation of lecithins (E 322) as a food additive is not considered to be applicable for infants under the age of 12 weeks 32. The European Food Safety Authority Panel noted that it is prudent to keep the number of additives used in foods for infants and young children to the minimum necessary.
The acute toxicity of lecithins (E 322) in mice, rats and rabbits is low. Subchronic toxicity studies in rats and dogs did not report any adverse effect, even at the highest doses tested (3,750 mg essential phospholipid/kg body weight per day, 1,000 mg soya phosphatidylinositol or essential phospholipid/kg body weight per day in rats and dogs, respectively, and 5,460 mg lecithins/kg body weight per day in rats). The European Food Safety Authority Panel considered the available genotoxicity data on lecithins (E 322) to be sufficient to conclude that there is no concern with respect to genotoxicity 32. Chronic toxicity studies in rats did not report any adverse effects, even at the highest dose tested (3,750 mg essential phospholipid/kg body weight per day). No carcinogenic effects were reported in rats, even at the highest dose tested (1,470 and 2,280 mg soya lecithin/kg body weight per day in males and females, respectively) for 2 years 32. Several neurodevelopmental toxicity studies were conducted with lecithin. The European Food Safety Authority Panel concluded that the relevance of the studies is limited but, at concentrations of 5% soya lecithin and higher in the diet during the gestation, lactation and the post‐weaning period, there were indications for alterations in the development of the brain 32.
What is lecithin good for?
Soy lecithin is widely used in the food industry as an emulsifier and stabilizing agent in the production of foods such as margarine, mayonnaise, chocolate and baked goods. Lecithin is also used as an emulsifying and stabilizing agent in pharmaceutical, and cosmetic (eg, creams, lipsticks, conditioners) industries. Lecithin is also consumed because of its purported health benefits. A review 37 reported numerous data supporting the effect of lecithin in lowering the blood cholesterol level in hyperlipidemic animals and humans.
Lecithin is also sold as an herbal supplement. There are no regulated manufacturing standards in place for many herbal compounds and some marketed supplements have been found to be contaminated with toxic metals or other drugs. Herbal/health supplements should be purchased from a reliable source to minimize the risk of contamination.
Lecithin has been used in alternative medicine as a possibly effective aid in treating liver disease.
Lecithin has also been used to treat gallbladder disease, dementia related to Alzheimer’s disease, age related loss of memory, and head injuries. However, research has shown that lecithin may not be effective in treating these conditions.
Other uses not proven with clinical research have included high cholesterol, manic-depressive disorder, dermatitis, improvement of athletic performance, Parkinson’s disease, stress, insomnia, and other conditions.
It is not certain whether lecithin is effective in treating any medical condition. Medicinal use of this product has not been approved by the FDA. Lecithin should not be used in place of medication prescribed for you by your doctor.
Soy lecithin on cholesterol
Lecithin is one of the nature elements that have dispersing properties. That is why it can emulsify fat, avoiding its absorption. Lecithin is capable of reducing LDL “bad” cholesterol. It also promotes the HDL “good” cholesterol synthesis 38. In addition to be used to help reduce cholesterol and triglycerides and protect the liver in the prevention of kidney stone formation, it is used as a tonic for the nervous system and brain activities. The Food and Drug Administration-(FDA) USA, and the World Federation of Cardiology recommended the use of 25 grams per day of soy protein, which corresponds to approximately 60 g of soybeans for cardiovascular disease prevention. However, it is not yet clear which components of soy are responsible for their antiatherogenic purposes.
Recent studies suggest that a lecithin-rich diet can modify the cholesterol homeostasis and lipoprotein metabolism in liver. Lecithin diet modifies the cholesterol homeostasis in the liver, increasing the HMG-CoA reductase and alpha 7 hydroxylase cholesterol activities and decreasing the microsomal ACAT activity. The LDL concentration and size are also significantly reduced and the bile acid pool and bile lipid secretion are increased 39.
In this study 40, soy lecithin effect on the serum cholesterol concentration involving thirty volunteers (58–70 years old) was evaluated with one soy lecithin capsule 500 mg [22% phospholipid (phosphatidiletanolamine), 10% triacylglycerol, and 68% phosphatidylcholine] administrated daily for 2 months. The results showed a decrease of 40.65% and 42.60% in total cholesterol and 42.65% and 56.11% in LDL “bad” cholesterol, one and two months after administration, respectively. However, further works with a large number of patients should be carried out towards finding the ideal dose-response.
Lecithin-rich diets can stimulate the fatty acid secretion with high levels of cholesterol and phospholipids when compared with diets without lecithin, considering the lecithin performance as phytotherapic, with a large spectrum of activity. The results showed significant reduction in the concentration of total cholesterol and LDL-cholesterol during the first month, suggesting that the daily administration of lecithin capsule could be used as an adjuvant treatment in hypercholesterolemia, possibly by reducing the intestinal absorption or by the increased secretion of bile acids with high levels of cholesterol and phospholipids 40.
Soybean presents a number of advantages compared with other sources of vegetable protein 41. It has high-protein content (38%–42%) of low cost and high quality as well as isoflavones that help in reducing blood cholesterol. The daily intake of 25 grams of soy protein dramatically reduced the total cholesterol over a period of approximately three weeks, that is, one month after treatment beginning. It was also shown that this effect was not dependent on time, since there was no increase two months after the treatment end. The daily intake of soy protein may reduce the LDL concentration by 30%, while occurs a stimulus for the HDL “good” cholesterol production 42.
Soybean protein increases the cholesterol-lowering effects of plant sterols on rats fed cholesterol; the combination of plant sterols and soy protein increases fecal neutral sterols and bile acid excretion compared with the sterol and soy protein alone; therefore, the combination of sterol and soy protein shows a more ostensible decrease in plasma lipids than the isolated ingredients 38.
A decrease in the cholesterol intestinal absorption and an increase in the bile acid excretion have been suggested as possible mechanisms for the effects in the reduction of lipids by soy protein 43.
Jiang et al. 44 demonstrated the inhibition of cholesterol absorption in diets rich in phosphatidylcholine. This study suggests that the high degree of saturation of acyl groups of the soybean phosphatidylcholine decreases the cholesterol intestinal absorption.
Neurologic disorders
Lecithin is a good source of choline for treatment in dementias 45. Phosphatidylcholine is thought to be a precursor for acetylcholine (Ach) synthesis 46. Choline increases the accumulation of Ach within the brain. Ach is important for many brain functions including memory, so increasing concentration of this neurotransmitter can result in improved memory 30.
Positive effect on long-term memory has been demonstrated after administration of 35 g lecithin for 4 to 6 weeks 46. However, another report shows no improvement from lecithin in memory disorders when taken in 30 mg/day dosages 47.
Lecithin supplementation has also been studied in Alzheimer disease, starting with memory difficulties. Three of 7 Alzheimer patients receiving 25 g lecithin showed improvement in learning ability (coinciding with peak choline levels) 48. Combination tacrine and lecithin therapy conducted in a 32-patient double-blinded trial yielded poor results 49. In a multicenter study, this combination did not improve mental status in 67 Alzheimer patients 50.
Acetylcholine deficiencies are also associated with other neurological disorders including tardive dyskinesia, Huntington chorea, Friedreich ataxia, myasthenia gravis, and other brain atrophies. In 2 patients with tardive dyskinesia, lecithin administration reduced abnormal movements. Ten cases of Friedreich ataxia were also improved by lecithin supplementation 51. One study failed to show any beneficial response in 12 patients with Friedreich ataxia taking 25 g lecithin daily 52.
Liver disease
In Germany, a product called Essentiale (phosphatidylcholine) is marketed for liver disorders including acute and chronic hepatitis, cirrhosis, diabetic fatty liver, and toxic liver damage. However, there are no clinical data regarding the use of lecithin for liver disease.
Other uses
Lecithin has also been used for immune modulation, activating specific and nonspecific defense systems in 20 patients receiving 1 teaspoonful 3 times daily for 30 days 53. Another report discusses gallstone dissolution in 2 of 7 patients treated with lecithin and oral cholic acid. One patient experienced stone size reduction 54.
Lecithin dosage
Most previous studies 55, 56, 57 have used the dosage of 1 to 3 g per day of oral supplementation of lecithin, exhibiting its effects for inflammatory diseases, hyperlipidemia, cardiovascular diseases, cognitive impairment, and fatiguing illnesses. Oral administration of lecithins has been shown to be generally safe 55. For example, in phase I and II clinical trials in patients with cardiovascular diseases, over 5 g of soy lecithins were administered with no apparent toxicity 58. Referring to older studies, a daily dosage of as much as 54 g has been administered without any apparent adverse effects 59. Regarding the duration of the treatment, most of the previous studies investigating the effects of dietary lipid replacement therapy supplement on fatigue examined for 8 weeks, meanwhile some examined for 1 or 12 weeks 55.
Lecithin side effects
Although not all side effects are known, lecithin is thought to be likely safe for most people.
Common side effects may include anorexia, nausea, increased salivation, diarrhea, abdominal pain or fullness. However, there have been reports of hepatitis.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
References- Akit H, Collins C, Fahri F, et al. Dietary Lecithin Decreases Skeletal Muscle COL1A1 and COL3A1 Gene Expression in Finisher Gilts. McGlone JJ, ed. Animals : an Open Access Journal from MDPI. 2016;6(6):38. doi:10.3390/ani6060038. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4929418/
- Dietary phospholipids and intestinal cholesterol absorption. Cohn JS, Kamili A, Wat E, Chung RW, Tandy S. Nutrients. 2010 Feb; 2(2):116-27.
- Dietary phospholipids, hepatic lipid metabolism and cardiovascular disease. Cohn JS, Wat E, Kamili A, Tandy S. Curr Opin Lipidol. 2008 Jun; 19(3):257-62.
- Van Wijk N, Balvers M, Cansev M, Maher TJ, Sijben JWC, Broersen LM. Dietary Crude Lecithin Increases Systemic Availability of Dietary Docosahexaenoic Acid with Combined Intake in Rats. Lipids. 2016;51:833-846. doi:10.1007/s11745-016-4139-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4903106/
- Wurtman RJ, Hirsch MJ, Growdon JH. Lecithin consumption raises serum-free-choline levels. Lancet 1977;2:68-69. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(77)90067-8/fulltext
- The natural history of soy allergy. Savage JH, Kaeding AJ, Matsui EC, Wood RA. J Allergy Clin Immunol. 2010 Mar; 125(3):683-6. https://www.ncbi.nlm.nih.gov/pubmed/20226303/
- Perdu LF, Prevost A, Vallerand H, Cossart C, Passemard F. Baker’s asthma related to soybean lecithin exposure. Allergy. 1994;49:159–62. doi: 10.1111/j.1398-9995.1994.tb00819.x
- Renaud C, Cardiet C, Dupond C. Allergy to soy lecithin in a child. J Pediatr Gastroenterol Nutr. 1996;22:328–9. doi: 10.1097/00005176-199604000-00019
- Fine SR. Possible reactions to soya lecithin in aerosols. J Allergy Clin. Immunol. 1991;87:600. doi: 10.1016/0091-6749(91)90025-J
- Soy allergy is not common in atopic children: a multicenter study. Bruno G, Giampietro PG, Del Guercio MJ, Gallia P, Giovannini L, Lovati C, Paolucci P, Quaglio L, Zoratto E, Businco L. Pediatr Allergy Immunol. 1997 Nov; 8(4):190-3. https://www.ncbi.nlm.nih.gov/pubmed/9553984/
- Kattan JD, Cocco RR, Järvinen KM. Milk and Soy Allergy. Pediatr Clin North Am. 2011;58(2):407–426. doi: 10.1016/j.pcl.2011.02.005 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3070118/
- Food Allergy Research & Education. https://www.foodallergy.org/common-allergens/soy
- Gu X, Beardslee T, Zeece T, Sarath G, Markwell J. Identification of IgE-binding proteins in soy lecithin. Int Arch Allergy Immunol. 2001;126:218–25. doi: 10.1159/000049517
- Gultekin F, Doguc DK. Allergic and Immunologic Reactions to Food Additives. Clinic Rev Allerg Immunol. 2013;45:6–29. doi: 10.1007/s12016-012-8300-8
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2014. Scientific Opinion on the evaluation of allergenic foods and food ingredients for labelling purposes. EFSA Journal 2014;12(11):3894, 286 pp. doi:10.2903/j.efsa.2014.3894
- Kattan JD, Cocco RR, Järvinen KM. Milk and Soy Allergy. Pediatric clinics of North America. 2011;58(2):407-426. doi:10.1016/j.pcl.2011.02.005. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3070118/
- Tips for Avoiding Your Allergen. https://www.foodallergy.org/sites/default/files/migrated-files/file/tips-avoid-allergen.pdf
- The natural history of soy allergy. Savage JH, Kaeding AJ, Matsui EC, Wood RA. J Allergy Clin Immunol. 2010 Mar; 125(3):683-6. https://www.jacionline.org/article/S0091-6749(10)00007-2/fulltext
- Matricardi PM, Bockelbrink A, Beyer K, et al. Primary versus secondary immunoglobulin E sensitization to soy and wheat in the Multi-Centre Allergy Study cohort. Clin Exp Allergy. 2008;38(3):493–500.
- Nowak-Wegrzyn A, Muraro A. Food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol. 2009;9(4):371–7.
- Sicherer SH, Eigenmann PA, Sampson HA. Clinical features of food protein-induced enterocolitis syndrome. J Pediatr. 1998;133(2):214–9.
- Jarvinen KM, Sickles L, Nowak-Wegrzyn A. Clinical Characteristics of Children with Food Protein-Induced Enterocolitis (FPIES) Journal of Allergy and Clinical Immunology. 2010;125(2):AB85.
- Hwang JB, Sohn SM, Kim AS. Prospective follow-up oral food challenge in food protein-induced enterocolitis syndrome. Arch Dis Child. 2009;94(6):425–8.
- Maloney J, Nowak-Wegrzyn A. Educational clinical case series for pediatric allergy and immunology: allergic proctocolitis, food protein-induced enterocolitis syndrome and allergic eosinophilic gastroenteritis with protein-losing gastroenteropathy as manifestations of non-IgE-mediated cow’s milk allergy. Pediatr Allergy Immunol. 2007;18(4):360–7
- Mehr SS, Kakakios AM, Kemp AS. Rice: a common and severe cause of food protein-induced enterocolitis syndrome. Arch Dis Child. 2009;94(3):220–3.
- Maloney J, Nowak-Wegrzyn A. Educational clinical case series for pediatric allergy and immunology: allergic proctocolitis, food protein-induced enterocolitis syndrome and allergic eosinophilic gastroenteritis with protein-losing gastroenteropathy as manifestations of non-IgE-mediated cow’s milk allergy. Pediatr Allergy Immunol. 2007;18(4):360–7.
- Burks AW, Casteel HB, Fiedorek SC, et al. Prospective oral food challenge study of two soybean protein isolates in patients with possible milk or soy protein enterocolitis. Pediatr Allergy Immunol. 1994;5(1):40–5.
- Anveden-Hertzberg L, Finkel Y, Sandstedt B, et al. Proctocolitis in exclusively breast-fed infants. Eur J Pediatr. 1996;155(6):464–7.
- Arvola T, Ruuska T, Keranen J, et al. Rectal bleeding in infancy: clinical, allergological, and microbiological examination. Pediatrics. 2006;117(4):e760–8.
- Murray M. Encyclopedia of Nutritional Supplements . Rocklin, CA: Prima Publishing, 1996.
- Venturella US. Natural Products. Gennaro AR, ed. Remington: The Science and Practice of Pharmacy , ed. 19. Easton, PA: Mack Publishing Co., 1995.
- Re‐evaluation of lecithins (E 322) as a food additive. EFSA Journal 7 April 2017. https://doi.org/10.2903/j.efsa.2017.4742
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 1974a. 299. Lecithin. WHO Food Additives Series 5. 2 pp.
- GRAS Notices. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/scripts/fdcc/?set=GRASNotices&sort=GRN_No&order=DESC&startrow=1&type=basic&search=lecithin
- Van Nieuwenhuyzen W. 1981. The industrial uses of special lecithins: a review. J Am Oil Chem Soc 58:886–888. doi:10.1007/BF02659651
- IOM (Institute of Medicine), 1998. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Food and Nutrition Board. National Academy Press, Washington, DC.
- Soy constituents: modes of action in low-density lipoprotein management. van Ee JH. Nutr Rev. 2009 Apr; 67(4):222-34. https://www.ncbi.nlm.nih.gov/pubmed/19335716/
- Lin Y, Meijer GW, Vermeer MA, Trautwein EA. Soy protein enhances the cholesterol-lowering effect of plant sterol esters in cholesterol-fed hamsters. Journal of Nutrition. 2004;134(1):143–148.
- LeBlanc M-J, Brunet S, Bouchard G, et al. Effects of dietary soybean lecithin on plasma lipid transport and hepatic cholesterol metabolism in rats. Journal of Nutritional Biochemistry. 2003;14(1):40–48.
- Mourad AM, de Carvalho Pincinato E, Mazzola PG, Sabha M, Moriel P. Influence of Soy Lecithin Administration on Hypercholesterolemia. Cholesterol. 2010;2010:824813. doi:10.1155/2010/824813. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065734/
- Clifton PM, Keogh J. Metabolic effects of high-protein diets. Current Atherosclerosis Reports. 2007;9(6):472–478.
- Torres N, Torre-Villalvazo I, Tovar AR. Regulation of lipid metabolism by soy protein and its implication in diseases mediated by lipid disorders. Journal of Nutritional Biochemistry. 2006;17(6):365–373.
- Sugano M, Yamada Y, Yoshida K, Hashimoto Y, Matsuo T, Kimoto M. The hypocholesterolemic action of the undigested fraction of soybean protein in rats. Atherosclerosis. 1988;72(2-3):115–122.
- Jiang Y, Noh SK, Koo SI. Egg phosphatidylcholine decreases the lymphatic absorption of cholesterol in rats. Journal of Nutrition. 2001;131(9):2358–2363.
- Reynolds J, ed. Martindale, The Extra Pharmacopoeia , ed. 31. London, Eng.: Royal Pharm. Society, 1996.
- DerMarderosian A, et al. Natural Product Medicine , Philadelphia, PA: George F. Stickley Co., 1988;121-22,140,313-15.
- Caine E. NEJM . 1980 Sep 4;303:585-86.
- Etienne P, et al. Lancet . 1978 Dec 2;2:1206.
- Maltby N, et al. BMJ . 1994 Apr 2;308:879-83.
- Chatellier G, et al. BMJ . 1990 Feb 24;300:495-99.
- Barbeau A, et al. NEJM . 1978 Jul 27;299:200-1.
- Pentland B, et al. BMJ . 1981 Apr 11;282:1197-98.
- Pawlik A, et al. Herba Polonica . 1996;42(1):42-46.
- Toouli J, et al. Lancet . 1975 Dec 6;2:1124-26.
- Nicolson GL, Ash ME. Lipid replacement therapy: a natural medicine approach to replacing damaged lipids in cellular membranes and organelles and restoring function. Biochim Biophys Acta. 1838;2014:1657–1679.
- Küllenberg D, Taylor LA, Schneider M, Massing U. Health effects of dietary phospholipids. Lipids Health Dis. 2012;11:3. doi: 10.1186/1476-511X-11-3
- Cohn JS, Wat E, Kamili A, Tandy S. Dietary phospholipids, hepatic lipid metabolism and cardiovascular disease. Curr Opin Lipidol. 2008;19:257–262. doi: 10.1097/MOL.0b013e3282ffaf96
- Pandey NR, Sparks DL. Phospholipids as cardiovascular therapeutics. Curr Opin Investig Drugs. 2008;9:281–285.
- Knuiman JT, Beynen AC, Katan MB. Lecithin intake and serum cholesterol. Am J Clin Nutr. 1989;49:266–268. https://www.ncbi.nlm.nih.gov/pubmed/2916447