What is Stickler syndrome
Stickler syndrome is a group of hereditary multisystem connective tissue disorder characterized by a distinctive facial appearance, eye abnormalities, hearing loss, skeleton and joint problems 1. These signs and symptoms vary widely among affected individuals. Stickler syndrome signs and symptoms can include ocular findings of myopia, cataract, and retinal detachment; hearing loss that is both conductive and sensorineural; midfacial underdevelopment and cleft palate (either alone or as part of the Robin sequence); and mild spondyloepiphyseal dysplasia and/or precocious arthritis.
Stickler syndrome received its name from Dr. Gunnar B. Stickler, who first studied and documented the syndrome at Mayo Clinic in 1965. A syndrome is a collection of specific symptoms, all with one cause.
A characteristic feature of Stickler syndrome is a somewhat flattened facial appearance. This appearance results from underdeveloped bones in the middle of the face, including the cheekbones and the bridge of the nose. A particular group of physical features called Pierre Robin sequence is also common in people with Stickler syndrome. Pierre Robin sequence includes an opening in the roof of the mouth (a cleft palate), a tongue that is placed further back than normal (glossoptosis), and a small lower jaw (micrognathia). This combination of features can lead to feeding problems and difficulty breathing. 30-40% of patients with Pierre Robin sequence have Stickler syndrome.
Many people with Stickler syndrome have severe nearsightedness (high myopia). In some cases, the clear gel that fills the eyeball (the vitreous) has an abnormal appearance, which is noticeable during an eye examination. Other eye problems are also common, including increased pressure within the eye (glaucoma), clouding of the lens of the eyes (cataracts), and tearing of the lining of the eye (retinal detachment). These eye abnormalities cause impaired vision or blindness in some cases.
In people with Stickler syndrome, hearing loss varies in degree and may become more severe over time. The hearing loss may be sensorineural, meaning that it results from changes in the inner ear, or conductive, meaning that it is caused by abnormalities of the middle ear.
Most people with Stickler syndrome have skeletal abnormalities that affect the joints. The joints of affected children and young adults may be loose and very flexible (hypermobile), though joints become less flexible with age. Arthritis often appears early in life and may cause joint pain or stiffness. Problems with the bones of the spine (vertebrae) can also occur, including abnormal curvature of the spine (scoliosis or kyphosis) and flattened vertebrae (platyspondyly). These spinal abnormalities may cause back pain.
Researchers have described several types of Stickler syndrome, which are distinguished by their genetic causes and their patterns of signs and symptoms. In particular, the eye abnormalities and severity of hearing loss differ among the types. Type I has the highest risk of retinal detachment. Type II also includes eye abnormalities, but type III does not (and is often called non-ocular Stickler syndrome). Types II and III are more likely than type I to have significant hearing loss. Types IV, V, and VI are very rare and have each been diagnosed in only a few individuals. Stickler syndrome affects an estimated 1 in 7,500 to 9,000 newborns.
Stickler syndrome type I (mutations in the dominant genes COL2A1) is the most common form of the condition. Stickler syndrome type 1 – COL2A1 is responsible for Stickler syndrome in about 75% of people diagnosed with the condition. Most will have ‘full’ Stickler syndrome affecting the sight, joints, hearing and any mid-line clefting. Findings show those with this anomaly have an increased incidence of cleft abnormalities.
Stickler syndrome type II – COL112A again causes ‘full’ stickler syndrome, and patients with this anomaly have more incidence of deafness. There is also a recessive variety of type II which has been identified in 3 people with very, severe deafness.
Stickler syndrome type III -COL112A causes a non-ocular Stickler-like syndrome, which affects only the joints and hearing with no eye problems.
Stickler syndrome signs and symptoms
Eyes
- Short-sight (myopia)
- Abnormal appearance of the vitreous gel.
- High risk of retinal detachments (tearing of the lining of the eye), which may affect both eyes.
- Cataracts
- Glaucoma
Bones and Joints
- Hyper-mobile (over flexible) joints and/or stiff joints.
- Early joint disease leading to osteoarthritis and joint replacements at a younger age
Facial Features
- A full cleft, submucous or high arched palate and/or bifid uvula
- Micrognathia – where the lower jaw is shorter than the other resulting in poor contact between the chewing surfaces of the upper and lower teeth. These symptoms are similar to those found in Pierre Robin sequence. It is reported that 30-40% of children diagnosed with Pierre Robin sequence are later re-diagnosed as having Stickler syndrome.
- Other facial characteristics include a flat face with a small nose and little or no nasal bridge. Appearance tends to improve with age
Hearing
- Hearing loss ( sensorineural and or conductive. The degree varies in affected individuals and may become more severe over time.
- Glue ear in childhood caused by cleft palate.
Other symptoms
These may include curvature of the spine (scoliosis), and because of sight and hearing problems, some learning difficulties may be experienced. Many people within the support group, especially children, complain of chronic fatigue.
A condition similar to Stickler syndrome, called Marshall syndrome, is characterized by a distinctive facial appearance, eye abnormalities, hearing loss, and early-onset arthritis. Marshall syndrome can also include short stature. Some researchers have classified Marshall syndrome as a variant of Stickler syndrome, while others consider it to be a separate disorder.
No studies to determine the prevalence of Stickler syndrome have been undertaken 1. However, an approximate incidence of Stickler syndrome among newborns can be estimated from data regarding the incidence of Robin sequence in newborns (1:10,000-1:14,000) and the percent of these newborns who subsequently develop signs or symptoms of Stickler syndrome (35%). These data suggest that the incidence of Stickler syndrome among neonates is approximately 1:7,500-1:9,000 2.
Stickler is believed to be the most common syndrome in the United States and Europe, but one of the rarest to be diagnosed. Most sufferers have such minor symptoms that they do not seek a diagnoses. Those who become patients are generally not correctly diagnosed. One study found a 53% error in original diagnosis of patients found in retrospect to have Stickler. A lot of patients are only diagnosed with one symptom and called, for example, arthritic or near-sighted.
Figure 1. Stickler syndrome
Footnote: Physical appearance of the patients. (a, b) Case 1, age 1.5 years. Mild depression of the nasal bridge and micrognathia. (c) Case 2, age 1 month. Buphthalmic eyes, hypertelorism, bilateral epicanthus, flat face, depressed nasal bridge, short stubby nose, and micro-retrognathia. (d, e) Case 4, age 8.5 years. Proptotic eyes, flat face with mild frontal bossing, depressed nasal bridge, and short nose. (f, g) Case 3, age 9 months. Buphthalmic eyes, flat face with frontal bossing, midfacial hypoplasia, depressed nasal bridge, short nose with anteverted nares, long philtrum, and micro-retrognathia. (h–j) Case 3, age 9 years. (h, i) High-frontal area, big proptotic eyes, long palpebral fissures, depressed nasal bridge, short nose, long philtrum, irregular teeth order, micrognathia, and dry rough hairs. (j) Small hands with brachydactyly.
Stickler syndrome types
Stickler syndrome type 1
Stickler syndrome type 1 (STL1) is responsible for approximately 70% of reported cases and presents with a wide variety of symptoms affecting the eye, ear, facial appearance, palate and musculoskeletal system and occurs due to mutations over the entire COL2A1 gene on chromosome 12q13.11. These mutations cause loss of function of the COL2A1 gene. The majority of these mutations are associated with normal stature and early onset osteoarthritis. Only a few non-glycine missense mutations have been reported and among these, the arginine to cysteine substitutions predominate and these mutations cause some unusual disorders which may be described as Stickler-like but have short stature and brachydactyly. The inheritance pattern for Stickler syndrome type 1 is autosomal dominant.
Stickler syndrome type 2
Stickler syndrome type 2 (STL2) occurs due to mutations of the COL11A1 gene on chromosome 1p21. Patients with another condition, called Marshall syndrome, can have mutations of COL11A1 also, but patients with Stickler syndrome type 2 have a milder phenotype with less prominent facial dysmorphism than patients with Marshall syndrome. Patients with Stickler syndrome type 2 have less pronounced midfacial flattening and the nasal bridge better developed than seen in patients with Marshall syndrome. Myopia and retinal degeneration are not always present. Cataracts and more severe early onset hearing loss are more common in Stickler type 2 than in patients with Stickler type 1. The inheritance pattern is autosomal dominant.
Stickler syndrome type 3
Stickler syndrome type 3 (STL3) has been described as the non-ocular form of Stickler syndrome, affecting the joints and hearing without involving the eyes. Stickler syndrome type 3 is caused by mutations of the COL11A2 gene on chromosome 6p21.3. The inheritance pattern is autosomal dominant. This form is now considered the same disorder as heterozygous oto-spondylo-megaepiphyseal dysplasia (OSMED).
Stickler syndrome type 4
A mutation in a fourth gene, COL9A1, located on chromosome 6q13, has been identified in three reported intermarried families in Turkey and Morocco with Stickler syndrome type 4 or STL4.The inheritance pattern is autosomal recessive.
Stickler syndrome type 5
Stickler syndrome type 5 (STL5) is thought to be caused by COL9A2, located on chromosome 1p33. This has been described in one intermarried family in India. The inheritance pattern is autosomal recessive.
Stickler syndrome type 6
Mutations of COL9A3 have recently been reported in three brothers in an intermarried Moroccan family with features of Stickler syndrome and intellectual disability.
Stickler syndrome has also been subdivided based on the vitreous phenotype resulting from mutations in the various loci. However, it has been reported that it is difficult for most ophthalmologists to classify the type of vitreous anomalies in the patients with Stickler syndrome.
Stickler syndrome life expectancy
Because the symptoms of Stickler syndrome are variable, it can be difficult to predict what the long-term outlook is for people who have Stickler syndrome. There is an increased risk for eye problems associated with Stickler syndrome including retinal detachment and cataracts. These symptoms can lead to vision loss. People with Stickler syndrome may also experience arthritis before 40-years-old. In general, people with Stickler syndrome have typical intelligence and can function well in society. Some people do not know they have Stickler syndrome until another family member is diagnosed because the symptoms can be relatively mild 1.
Stickler syndrome causes
Mutations in several genes cause the different types of Stickler syndrome. Between 80 and 90 percent of all cases are classified as type I and are caused by mutations in the COL2A1 gene. Another 10 to 20 percent of cases are classified as type II and result from mutations in the COL11A1 gene. Marshall syndrome, which may be a variant of Stickler syndrome, is also caused by COL11A1 gene mutations. Stickler syndrome types III through VI result from mutations in other, related genes.
All of the genes associated with Stickler syndrome provide instructions for making components of collagens, which are complex molecules that give structure and strength to the connective tissues that support the body’s joints and organs. Mutations in any of these genes impair the production, processing, or assembly of collagen molecules. Defective collagen molecules or reduced amounts of collagen impair the development of connective tissues in many different parts of the body, leading to the varied features of Stickler syndrome.
Not all individuals with Stickler syndrome have mutations in one of the known genes. Researchers believe that mutations in other genes may also cause this condition, but those genes have not been identified.
Stickler syndrome inheritance pattern
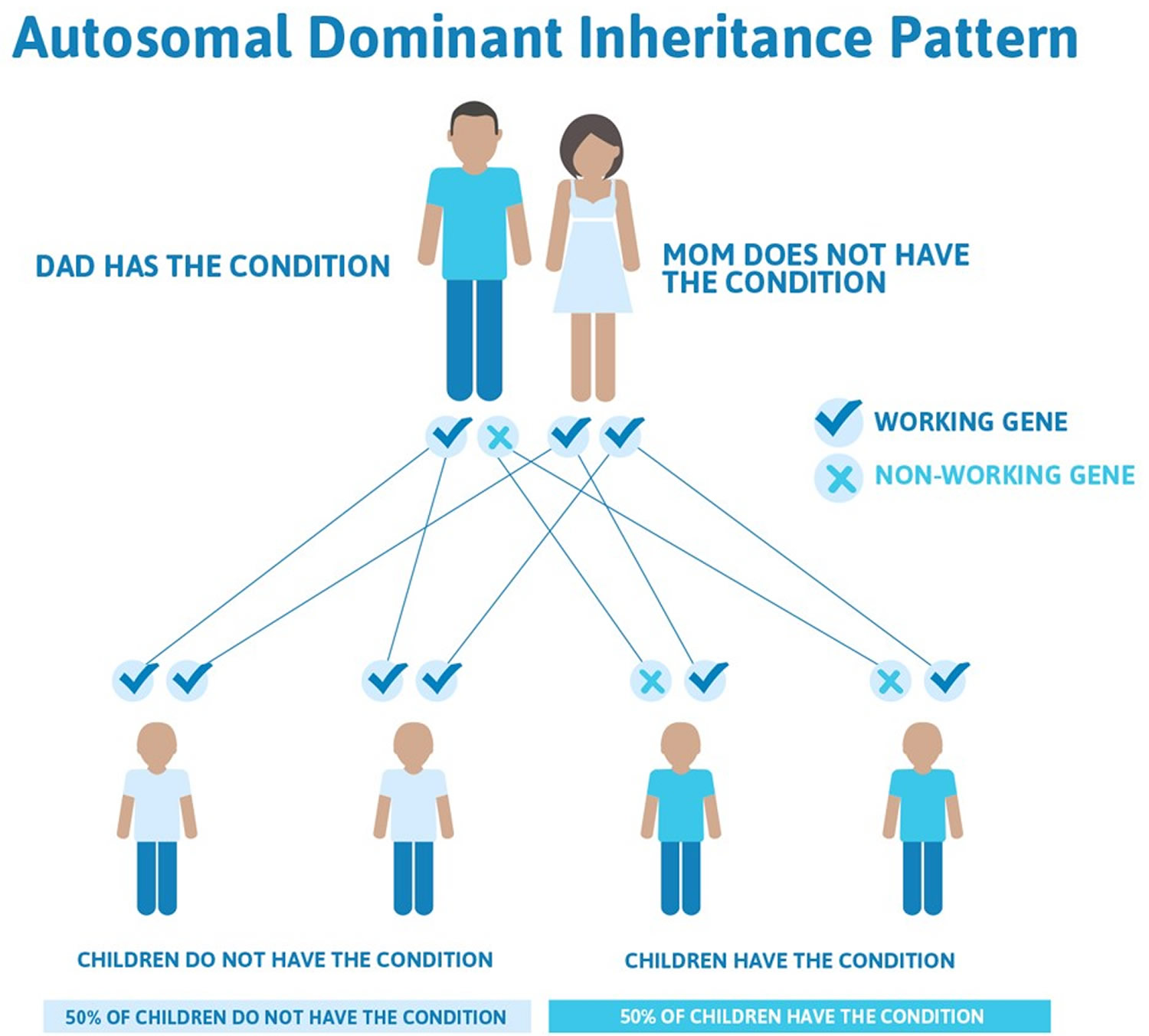
Stickler syndrome types I, II, and III are inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. In some cases, an affected person inherits a gene mutation from one affected parent. Other cases result from new mutations. These cases occur in people with no history of Stickler syndrome in their family. Marshall syndrome also typically has an autosomal dominant pattern of inheritance.
This means that only one copy of one of the genes causing Stickler syndrome types I, II, and III has a pathogenic variant. You inherit one copy of every gene from your mother and the other from your father. When a person who has Stickler syndrome types I, II, and III has children, for each child there is a:
- 50% chance that the child will inherit the gene with a pathogenic variant, meaning he or she will have Stickler syndrome
- 50% chance that the child will inherit the working copy of the gene, meaning he or she will not have Stickler syndrome
In some cases, people who have an autosomal dominant form of Stickler syndrome are the first people to be diagnosed in the family. This may be because they inherited the genetic change from a parent, but the parent has mild symptoms of the syndrome and was never diagnosed. Most people who have an autosomal dominant form of Stickler syndrome inherited the genetic change from a parent 1. In other cases, the genetic change may be new in the person who was diagnosed with Stickler syndrome. Genetic changes that are new in a person are called de novo 1.
Figure 2. Stickler syndrome types I, II, and III are inherited in an autosomal dominant inheritance pattern
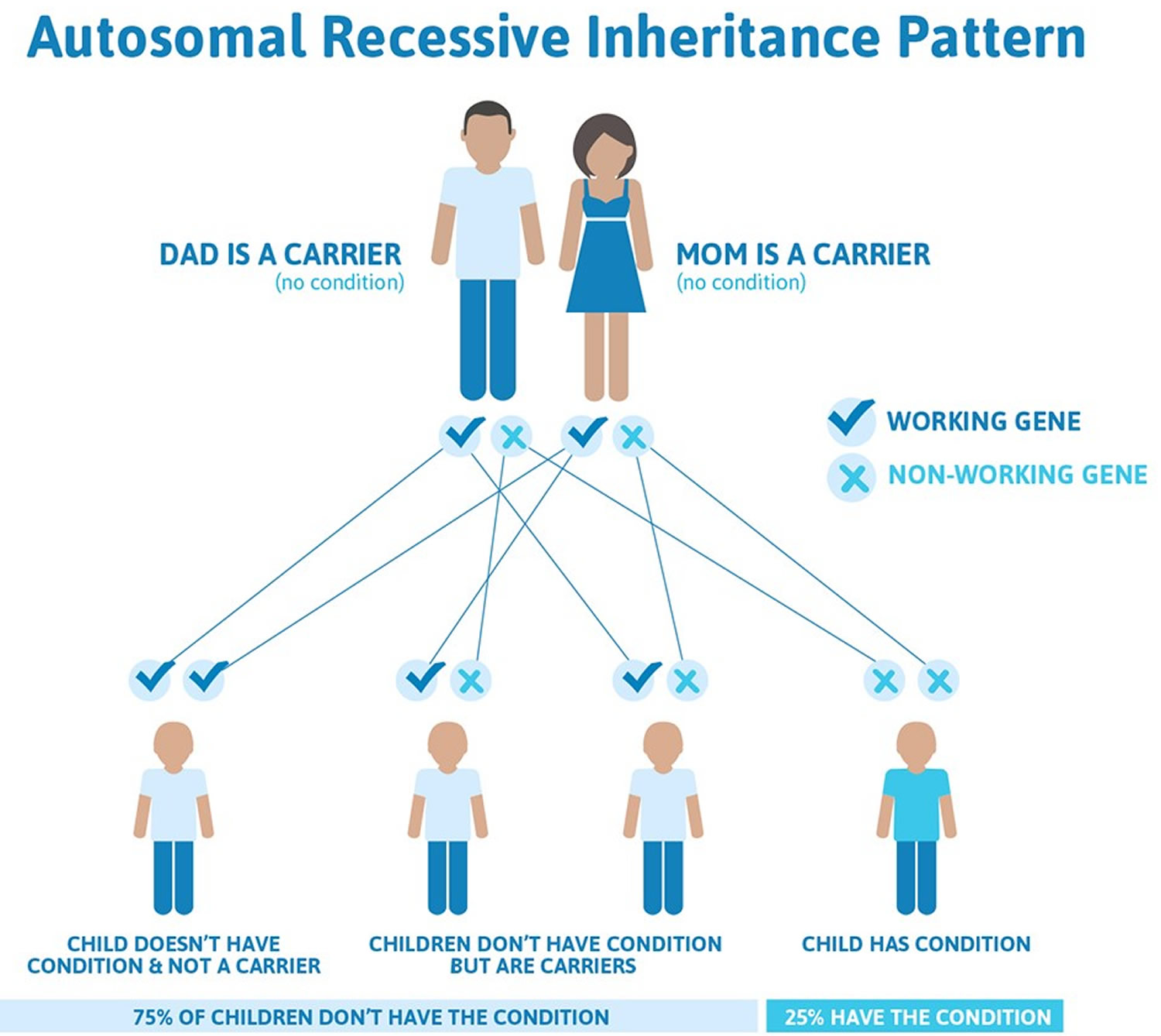
Stickler syndrome types IV, V, and VI are inherited in an autosomal recessive pattern. Autosomal recessive inheritance means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
This means that both copies of one of these genes must have a pathogenic variant for a person to have signs of Stickler syndrome types IV, V, and VI. People who only have one changed copy of a gene that causes an autosomal recessive form of Stickler syndrome are known as carriers. Carriers do not have signs or symptoms of the syndrome. When two carriers of Stickler syndrome have children together, for each child there is a:
- 25% chance that the child will inherit both changed copies of the gene, so he or she has Stickler syndrome
- 50% chance that the child will inherit only one changed copy of the gene, so he or she is a carrier of the syndrome like each of the parents
- 25% chance that the child will inherit both working copies of the gene, so he or she does not have Stickler syndrome and is not a carrier of the syndrome
Stickler syndrome shows a characteristic known as variable expressivity. This means that people with Stickler syndrome types IV, V, and VI can have different signs and symptoms of the syndrome, even among members of the same family. However, anyone with a pathogenic variant that causes Stickler syndrome is expected to have some symptoms of the syndrome. This is called full penetrance 1.
Figure 3. Stickler syndrome types IV, V, and VI are inherited in an autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Stickler syndrome symptoms
Stickler syndrome is a multisystem connective tissue disorder that can affect the craniofacies, eyes, inner ear, skeleton, and joints.
Craniofacial findings
Craniofacial findings include a flattened facial profile or an appearance that is often referred to as a “scooped out” face. This profile is caused by underdevelopment of the maxilla and nasal bridge, which can cause telecanthus and epicanthal folds. Midface retrusion is most pronounced in infants and young children, but these features usually become less distinctive as affected children grow older; older individuals may have a normal facial profile. Often the nasal tip is small and upturned, making the philtrum appear long. Certain facial features such as cleft palate can cause feeding or breathing difficulties in some children.
Micrognathia is common and may be associated with cleft palate as part of the Pierre Robin sequence (micrognathia, cleft palate, glossoptosis), an assortment of abnormalities that may occur as a distinct syndrome or as part of another underlying disorder. The degree of micrognathia may compromise the upper airway, necessitating tracheostomy. Pierre-Robin sequence is characterized by an unusually small jaw (micrognathia), downward displacement or retraction of the tongue (glossoptosis), and incomplete closure of the roof of the mouth (cleft palate, sub-mucous cleft palate or bifid uvula). Often babies with Pierre-Robin sequence and glossoptosis obstruct their airway when placed on their backs, and it may be recommended that they sleep prone due to this risk. Patients with very small jaws might be recommended to have surgery to extend their jaw forward.
Cleft palate may be seen in the absence of micrognathia.
Dental anomalies such as failure of the upper and lower teeth to meet when biting down (malocclusion) may also occur.
Stickler syndrome eye
Stickler syndrome eye findings include high myopia (>−3 diopters) that is non-progressive and detectable in the newborn period 3 and vitreous abnormalities.
Affected individuals may also develop degeneration of the thick, jelly-like fluid (vitreous) that fills the center of the eyes and the thin layer of nerve cells (retina) that lines the back of the eye (vitreoretinal degeneration). The retina senses light and converts it into nerve signals, which are then relayed to brain through the optic nerve. Vitreoretinal degeneration may cause tiny specks (floaters) that seem to float around obstructing a person’s field of vision. Vitreoretinal degeneration also places individuals with Stickler syndrome at risk for retinal detachment, which can affect one or both eyes.
Retinal detachment occurs when the retina pulls away or is separated (detaches) from the underlying tissue. In some cases, small tears may occur in the retina as well. Symptoms of retinal detachment include an increase in the number of floaters in the eye, increased blurriness of vision, sudden flashes of light and a sudden decrease in vision as if a curtain or veil is pulled over a portion of a person’s field of vision. Retinal detachment can cause significant loss of vision or blindness if left untreated. Retinal detachment can occur at any age.
Additional eye abnormalities associated with Stickler syndrome include clouding (opacity) of the lenses of the eyes (cataracts), crossed eyes (strabismus), and abnormal curvature to the cornea (the clear portion of the eye through which light passes) or lens of the eye (astigmatism), which can contribute to blurred vision. A small percentage of individuals with Stickler syndrome, approximately 5-10 percent, may develop glaucoma, a condition in which increased pressure within the eye causes characteristic damage to the optic nerve, which relays signals from the retina to the brain.
Two types of vitreous abnormalities are observed:
- Type 1 (“membranous”), which is much more common, is characterized by a persistence of vestigial vitreous gel in the retrolental space that is bordered by a folded membrane.
- Type 2 (“beaded”), much less common, is characterized by sparse and irregularly thickened bundles throughout the vitreous cavity.
The Stickler syndrome eye findings run true within families 3.
Posterior chorioretinal atrophy was described by Vu et al 4 in a family with vitreoretinal dystrophy, a novel pathogenic variant in COL2A1, and systemic features of Stickler syndrome, suggesting that individuals with Stickler syndrome may have posterior pole chorioretinal changes in addition to the vitreous abnormalities.
Hearing impairment
Hearing impairment is common. The degree of hearing loss is variable and may be progressive. The degree of hearing loss may vary greatly from one individual to another and can range from mild to significant. Hearing loss can occur due to failure of sound waves to be conducted through the middle ear (conductive hearing loss) or the impaired ability of the auditory nerves to transmit sensory input to the brain (sensorineural hearing loss) or from both (mixed hearing loss). Hearing loss is usually less severe and minimally progressive in Stickler syndrome type I as opposed to type II. Chronic (recurrent) infection of the middle ear (otitis media) may occur and can contribute to conductive hearing loss. Some individuals may develop the accumulation of thick, sticky fluid behind the eardrum (glue ear). People with Stickler syndrome can have hypermobility of the middle ear bones.
Some degree of sensorineural hearing impairment (typically high-tone, often subtle) is found in 40% of individuals 3. The exact mechanism is unclear, although it is related to the expression of type II and IX collagen in the inner ear 5. Overall sensorineural hearing loss in type I Stickler syndrome is typically mild and not significantly progressive; it is less severe than that reported for types II and III Stickler syndrome.
Conductive hearing loss can also be seen. This may be secondary to recurrent ear infections that are often associated with cleft palate and/or may be secondary to a defect of the ossicles of the middle ear.
Skeletal manifestations
Skeletal malformations are a common finding in individuals with Stickler syndrome. Affected individuals may have abnormally flexible or lax (hypermobile) joints (double jointedness) that may make them prone to joint dislocation. As affected individuals age, such flexibility becomes reduced. Joint pain and stiffness upon rest are frequent findings, and many individuals develop inflammation of the joints during the third or fourth decade of life (early-onset osteoarthritis).
Skeletal manifestations are early-onset arthritis, short stature relative to unaffected siblings, and radiographic findings consistent with mild spondyloepiphyseal dysplasia. Some individuals have a slender body habitus, but without tall stature.
Joint laxity, sometimes seen in young individuals, becomes less prominent (or resolves completely) with age 3.
Early-onset arthritis is common and may be severe, leading to the need for surgical joint replacement even as early as the third or fourth decade. More commonly, the arthropathy is mild, and affected individuals often do not complain of joint pain unless specifically asked. However, nonspecific complaints of joint stiffness can be elicited even from young children.
Chest deformities such as pectus excavatum (depression of the chest bone) and carinatum (prominent chest bone) can occur. Spinal abnormalities are also common in individuals with Stickler syndrome including abnormal sideways curvature of the spine (scoliosis), front-to-back curvature of the spine (kyphosis), endplate abnormalitiesand forward displacement of one vertebra over another, usually the 4th lumbar vertebra over the 5th or the 5th over the sacrum (spondylolisthesis) 6. Spinal abnormalities associated with Stickler may become progressively worse and may be associated with back pain.
Additional findings may occur in some cases including diminished muscle tone (hypotonia), abnormally long, slender fingers (arachnodactyly), flat feet (pes planus), and osteochondritis deformans of the hips (Legg-Calve-Perthes disease), a degenerative hip disorder with childhood onset.
Other features of Stickler syndrome
Intelligence is unaffected in children with Stickler syndrome, but some children may develop learning disabilities because of hearing and vision abnormalities.
Mitral valve prolapse has been reported in nearly 50% of individuals with Stickler syndrome in one series 7; diagnosis of Stickler syndrome was made on clinical features prior to the identification of the involved genes. A later study 8 reported mitral valve prolapse on echocardiogram in only one of 25 individuals with Stickler syndrome and a COL2A1 pathogenic variant. Ahmad et al 9 screened a group of 75 individuals with molecularly confirmed Stickler syndrome and found no individuals with clinical or echocardiographic evidence of significant mitral valve or other valve abnormality. It was suggested that among those with Stickler syndrome, the prevalence of mitral valve prolapse may be similar to that in the general population. No additional studies reviewing cardiac findings in Stickler syndrome have been reported.
The mitral valve is located between the left upper and left lower chambers (left atrium and left ventricle) of the heart. Mitral valve prolapse occurs when one or both of the flaps (cusps) of the mitral valve bulge or collapse backward (prolapse) into the left upper chamber (atrium) of the heart. In some cases, this may allow leakage or the backward flow of blood from the left lower chamber of the heart (ventricle) back into the left atrium (mitral regurgitation). In some cases, no associated symptoms are apparent (asymptomatic). However, in other cases, mitral valve prolapse can result in chest pain, abnormal heart rhythms (arrhythmias), fatigue, and dizziness.
Stickler syndrome diagnosis
Stickler syndrome can sometimes be diagnosed based on your child’s medical history and a physical exam, additional tests are needed to determine the severity of the symptoms and help direct treatment decisions.
Stickler syndrome should be suspected in individuals with a combination of the following findings:
- Cleft palate (open cleft, submucous cleft, or bifid uvula)
- Characteristic facial features including malar hypoplasia, broad or flat nasal bridge, and micro/retrognathia
- Vitreous changes or retinal abnormalities (lattice degeneration, retinal hole, retinal detachment or retinal tear)
- High-frequency sensorineural hearing loss
- Skeletal findings including:
- Slipped epiphysis or Legg-Perthes-like disease
- Scoliosis, spondylolisthesis, or Scheuermann-like kyphotic deformity
- Osteoarthritis before age 40
- An independently affected first-degree relative
Establishing the Diagnosis
The diagnosis of Stickler syndrome is established in a index case who meets the proposed clinical diagnostic criteria and/or has a heterozygous pathogenic variant in COL2A1, COL11A1, or COL11A2 or biallelic pathogenic variants in COL9A1, COL9A2, or COL9A3.
Clinical Diagnostic Criteria
Clinical diagnostic criteria have been proposed for type 1 Stickler syndrome (in which individuals have the membranous type of vitreous abnormality; see Clinical Description) but not validated [Rose et al 2005]. The proposed criteria are based on assigning points for clinical features, family history data, and molecular data.
Stickler syndrome should be considered in individuals with ≥5 points and absence of features suggestive of an alternative diagnosis. At least one finding should be a major (2-point) manifestation (denoted by *).
Abnormalities (2-pt maximum per category)
- Orofacial
- Cleft palate* (open cleft, submucous cleft, or bifid uvula): 2 points
- Characteristic facial features (malar hypoplasia, broad or flat nasal bridge, and micro/retrognathia): 1 point
- Ocular. Characteristic vitreous changes or retinal abnormalities* (lattice degeneration, retinal hole, retinal detachment or retinal tear): 2 points
- Auditory
- High-frequency sensorineural hearing loss*: 2 points
- Age <20 years: threshold ≥20 dB at 4-8 Hz
- Age 20-40 years: threshold ≥30 dB at 4-8 Hz
- Age >40 years: threshold ≥40 dB at 4-8 Hz
- Hypermobile tympanic membranes: 1 point
- Skeletal
- Femoral head failure (slipped epiphysis or Legg-Perthes-like disease): 1 point
- Radiographically demonstrated osteoarthritis before age 40: 1 point
- Scoliosis, spondylolisthesis, or Scheuermann-like kyphotic deformity: 1 point
Family history/molecular data
Independently affected first-degree relative in a pattern consistent with autosomal dominant inheritance or presence of a COL2A1, COL11A1, or COL11A2 pathogenic variant associated with Stickler syndrome**: 1 point
* Denotes major manifestation
** Does not account for families with autosomal recessive Stickler syndrome
Molecular genetic testing approaches can include serial single-gene testing, use of a multigene panel, and more comprehensive genomic testing:
- Serial single-gene testing can be considered based on the individual’s clinical findings and family history; however, findings should not be used to exclude specific testing:
- COL2A1 may be tested first in individuals with ocular findings including type 1 “membranous” congenital vitreous anomaly and milder hearing loss.
- COL11A1 may be tested first in individuals with typical ocular findings including type 2 “beaded” congenital vitreous anomaly and significant hearing loss.
- COL11A2 may be tested for in individuals with craniofacial and joint manifestations and hearing loss but without ocular findings.
- COL9A1, COL9A2, and COL9A3 may be tested for in individuals with possible autosomal recessive inheritance.
Sequence analysis of the gene of interest is performed first, followed by gene-targeted deletion/duplication analysis if no pathogenic variant is found.
- A multigene panel that includes COL2A1, COL11A1, COL11A2, COL9A1, COL9A2, COL9A3 and other genes of interest may be considered. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene varies by laboratory and over time. (2) Some multigene panels may include genes not associated with the condition discussed; thus, clinicians need to determine which multigene panel is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.
- More comprehensive genomic testing (when available) including exome sequencing and genome sequencing may be considered. Such testing may provide or suggest a diagnosis not previously considered (e.g., mutation of a different gene or genes that results in a similar clinical presentation).
Stickler syndrome treatment
There’s no cure for Stickler syndrome. Treatment addresses the signs and symptoms of the disorder.
To establish the extent of disease and needs in an individual diagnosed with Stickler syndrome, the following evaluations are recommended:
- Evaluation of palate by a craniofacial specialist
- Baseline ophthalmologic examination
- Baseline audiogram
- Directed history to elicit complaints suggestive of mitral valve prolapse, such as episodic tachycardia and chest pain. If symptoms are present, referral to a cardiologist should be made.
- Consultation with a clinical geneticist and/or genetic counselor
Craniofacial
Infants with Robin sequence need immediate attention from specialists in otolaryngology and pediatric critical care, as they may require tracheostomy to ensure a competent airway. It is recommended that evaluation and management occur in a comprehensive craniofacial clinic that provides all the necessary services, including otolaryngology, plastic surgery, oral and maxillofacial surgery, pediatric dentistry, orthodontics, and medical genetics.
In most individuals, micrognathia tends to become less prominent over time, allowing for removal of the tracheostomy. However, in some individuals, significant micrognathia persists, causing orthodontic problems. In these individuals, a mandibular advancement procedure is often required to correct the malocclusion.
Stickler syndrome eye
Refractive errors should be corrected with spectacles.
Individuals with Stickler syndrome should be advised of the symptoms associated with retinal detachment and the need for immediate evaluation and treatment when such symptoms occur.
Audiologic
Otitis media may be a recurrent problem secondary to palatal abnormalities. Myringotomy tubes are often required.
The ultimate goal in the evaluation and treatment of a child with hereditary hearing loss and deafness is mainstream schooling. Research shows that diagnosis by age three months and habilitation by six months makes this goal possible for children with mild-moderate hearing loss.
Your child may need speech therapy if hearing loss interferes with his or her ability to learn how to pronounce certain sounds.
If your child has problems hearing, you may find that his or her quality of life is improved by wearing a hearing aid. Cochlear implantation in children with severe-to-profound deafness who are part of mainstream education leads to social functioning and educational attainment that is indistinguishable from normal-hearing peers 10.
Special education
Hearing or vision problems may cause learning difficulty in school, so special education services may be helpful.
Joints
Treatment of arthropathy is symptomatic and includes using over-the-counter anti-inflammatory medications before and after physical activity.
In some cases, physical therapy may help with mobility problems associated with joint pain and stiffness. Equipment such as braces, canes and arch supports also may help.
Surgery
- Tracheostomy. Newborns with very small jaws and displaced tongues may need a tracheostomy to create a hole in the throat so that they can breathe. The operation is reversed once the baby has grown large enough that his or her airway is no longer blocked.
- Jaw surgery. Surgeons can lengthen the lower jaw by breaking the jawbone and implanting a device that will gradually stretch the bone as it heals.
- Cleft palate repair. Babies born with a hole in the roof of the mouth (cleft palate) typically undergo surgery in which tissue from the roof of the mouth may be stretched to cover the cleft palate.
- Ear tubes. The surgical placement of a short plastic tube in the eardrum can help reduce the frequency and severity of ear infections, which are especially common in children who have Stickler syndrome.
- Eye surgeries. Surgeries to remove cataracts or procedures to reattach the lining of the back of the eye (retina) may be necessary to preserve vision.
- Joint replacement. Early-onset arthritis, particularly in the hips and knees, may necessitate joint replacement surgeries at a much younger age than is typical for the general population.
- Spinal bracing or fusion surgeries. Children who develop abnormal curves in their spines, such as those seen in scoliosis and kyphosis, may require corrective surgery. Milder curves often can be treated with a brace.
Home remedies
- Pain relievers. Over-the-counter drugs such as ibuprofen (Advil, Motrin IB) and naproxen sodium (Aleve) may help relieve joint swelling, stiffness and pain.
- Avoid contact sports. Strenuous physical activity may stress the joints, and contact sports, such as football, may increase the risk of retinal detachment.
- Seek educational help. Your child may have difficulty in school due to problems hearing or seeing. Your child’s teachers need to be aware of his or her special needs.
- Robin NH, Moran RT, Ala-Kokko L. Stickler Syndrome. 2000 Jun 9 [Updated 2017 Mar 16]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1302/
- Printzlau A, Andersen M. Pierre Robin sequence in Denmark: a retrospective population-based epidemiological study. Cleft Palate Craniofac J. 2004;41:47–52. https://www.ncbi.nlm.nih.gov/pubmed/14697070
- Snead M, Yates J. Clinical and molecular genetics of Stickler syndrome. Journal of Medical Genetics. 1999;36(5):353-359. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1734362/pdf/v036p00353.pdf
- Vu CD, Brown J Jr, Korkko J, Ritter R 3rd, Edwards AO. Posterior chorioretinal atrophy and vitreous phenotype in a family with Stickler syndrome from a mutation in the COL2A1 gene. Ophthalmology. 2003;110:70–7. https://www.ncbi.nlm.nih.gov/pubmed/12511349
- Admiraal RJ, Brunner HG, Dijkstra TL, Huygen PL, Cremers CW. Hearing loss in the nonocular Stickler syndrome caused by a COL11A2 mutation. Laryngoscope. 2000;110:457–61. https://www.ncbi.nlm.nih.gov/pubmed/10718438
- Rose PS, Ahn NU, Levy HP, Ahn UM, Davis J, Liberfarb RM, Nallamshetty L, Sponseller PD, Francomano CA. Thoracolumbar spinal abnormalities in Stickler syndrome. Spine. 2001;26:403–9. https://www.ncbi.nlm.nih.gov/pubmed/11224888
- Liberfarb RM, Goldblatt A. Prevalence of mitral-valve prolapse in the Stickler syndrome. Am J Med Genet. 1986;24:387–92. https://www.ncbi.nlm.nih.gov/pubmed/3728560
- Liberfarb RM, Levy HP, Rose PS, Wilkin DJ, Davis J, Balog JZ, Griffith AJ, Szymko-Bennett YM, Johnston JJ, Francomano CA, Tsilou E, Rubin BI. The Stickler syndrome: genotype/phenotype correlation in 10 families with Stickler syndrome resulting from seven mutations in the type II collagen gene locus COL2A1. Genet Med. 2003;5:21–7. https://www.ncbi.nlm.nih.gov/pubmed/12544472
- Ahmad N, Richards AJ, Murfett HC, Shapiro L, Scott JD, Yates JR, Norton J, Snead MP. Prevalence of mitral valve prolapse in Stickler syndrome. Am J Med Genet. 2003;116A:234–7. https://www.ncbi.nlm.nih.gov/pubmed/12503098
- Langereis M, Vermeulen A. School performance and wellbeing of children with CI in different communicative–educational environments. Int J Pediatr Otorhinolaryngol. 2015;79:834–9. https://www.ncbi.nlm.nih.gov/pubmed/25840945