What is syringoma
Syringoma is a harmless eccrine sweat duct tumor which occur predominantly in young women in early adulthood 1. Syringoma is a non-cancerous (benign) bump, usually found on the upper cheeks and lower eyelids of young adults. Syringomas are completely harmless and are caused by the overgrowth of cells from sweat glands (eccrine glands) and are characterized by firm yellowish, translucent, or skin colored benign lump 1-3 mm in diameter, that are often found on the face, particularly around the eyes, but may also appear elsewhere on the face, in the armpits, umbilicus, upper chest, and genitalia and usually asymptomatic 2. Syringomas are most often found in clusters on the eyelids but they may also arise elsewhere on the face, in the armpits, umbilicus, upper chest and vulva. Syringomas arise from the sweat ducts and may occur suddenly in crops or multiples 3. There are 4 types of syringoma: a localized form, a form associated with Down syndrome, a generalized form that encompasses multiple and eruptive syringomas, and a familial form. Distribution of the generalized syringoma was mainly in the chest and neck followed by the forearms whereas localized syringoma was mostly confined to the face, armpits and genitalia 1. Syringomas are usually asymptomatic; however, rarely, individuals can experience extreme itching (pruritus), especially while sweating 4. Syringomas are found more commonly in Asians, and in females at puberty or near middle-age 5.
Any new skin growth should be examined by your doctor in order to obtain a correct diagnosis.
Syringoma may be confused with xanthelasma (cholesterol deposits on the eyelids), trichoepitheliomas or basal cell skin cancer.
The skin biopsy appearance under a microscope is characteristic. There are small ducts with comma-like tails, looking like tadpoles in the skin.
Syringomas may be treated surgically using different methods such as high frequency electric current (electrosurgery) or laser 2.
Syringoma causes
Syringomas are benign tumours of the sweat ducts (eccrine glands). These tumors lie in the mid to deep (dermal) layers of the skin. The majority of syringomas are spontaneous. Inherited (genetic) factors play a role in some cases, more than 10 cases of familial syringomas have been reported in the English literature. Inherited syringomas tend to occur in in pre-adolescence or adolescence, most commonly affect the face, and are usually inherited as an autosomal dominant trait 6. Eruptive syringomas have been reported in Down syndrome. Syringomas have also been associated with other rare genetic conditions such as Brooke-Spiegler syndrome. Eruptive syringomas are more common in African Americans and Asians than in other ethnic groups. One patient presented with extensive eruptive syringomas following liver transplantation, suggesting a potential role for immunosuppression in pathogenesis 7.
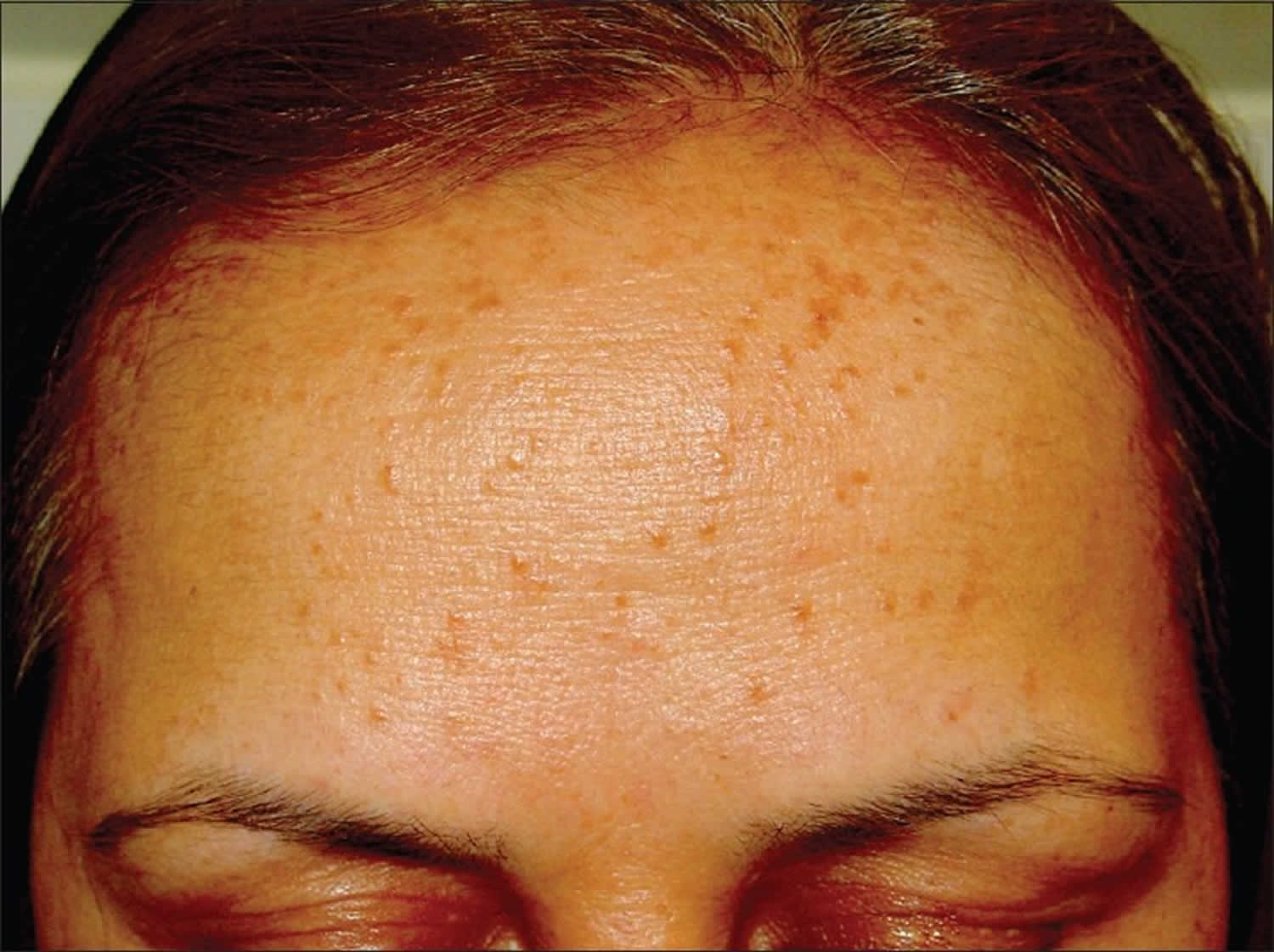
What do syringoma look like?
A syringoma is a skin colored or yellowish firm rounded bump, one to three millimeters in diameter. In people with skin of color (pigmented or dark skin), syringomas may appear as yellowish or pale bumps.
They start to appear in adolescence and are more common in women than men and most frequently appear during or after adolescence. There is sometimes another affected member of the family.
The most common location is around the eye area. Eruptive syringomas appear abruptly in adult life, as a crop of multiple lesions typically on the chest or lower abdomen. Most patients with eruptive syringomas are Asian and people with darker skin types.
The majority of syringomas are not associated with symptoms. Some people may experience itching with sweating.
Figure 1. Syringoma on the neck
Figure 2. Syringoma eyelid
Syringoma signs and Symptoms
The most common locations for syringomas include:
- Upper cheeks
- Lower eyelids
- Armpits
- Chest
- Abdomen
- Forehead
- Genitalia (penis or vulva)
Syringomas typically appear as small (1–3 mm) flesh-colored-to-yellowish bumps. They usually occur in clusters on both sides of the body and in an evenly distributed (symmetrical) fashion.
Eruptive syringomas appear as multiple lesions that all develop at the same time, usually on the chest and abdomen.
Syringomas do not itch or cause pain.
How is syringoma diagnosed?
Most cases are diagnosed by their appearance. A biopsy may be needed to exclude other similar kinds of tumours such as trichoepitheliomas, trichodiscomas, fibrofolliculomas as well as milia and basal cell cancers. Biopsies of syringomas show comma-shaped sweat ducts in the dermal (deep) layers of the skin.
If the diagnosis of syringoma is suspected, the doctor may want to perform a skin biopsy.
The procedure involves:
- Numbing the skin with an injectable anesthetic.
- Sampling a small piece of skin by using a flexible razor blade, a scalpel, or a tiny cookie cutter (called a “punch biopsy”). If a punch biopsy is taken, a stitch (suture) or two may be placed and will need to be removed 6–14 days later.
- Having the skin sample examined under the microscope by a specially trained physician (dermatopathologist).
Syringoma treatment
Syringomas are benign so they do not require treatment. However, they may be treated if they are disfiguring. Syringomas are often treated by electrosurgery (diathermy) or laser. This may or may not prove successful and can result in small scars. If they recur, they can be treated again the same way.
Though there is a risk of scarring, destruction of syringomas is fairly simple and may include:
- Burning (cauterization) with an electric needle
- Cutting out (excision) with a scalpel, scissors, or flexible razor blade
- Carbon dioxide laser treatment
- Procedure to rub out the lesion (dermabrasion)
- Freezing (cryosurgery) with liquid nitrogen
The aim of treatment is to reduce the visibility of the tumor rather than eliminate it completely. This reduces the risk of scarring. In order to achieve this, the upper portion of the syringoma is treated reducing its size. If complete ablation or tissue removal is carried out too deeply, scarring may result. More recently fractional ablative lasers have been introduced allowing treatment of the deeper component of the syringoma with much reduced risk of scarring.
People with darker skin types are at greater risk of scarring. It is wise to treat a small test area first. If this is successful, without complications or unacceptable scarring, then a larger area can be treated.
Syringomas can recur after all forms of treatment as they penetrate into the deep dermis or deeper layers of the skin.
Specific treatments
Syringoma laser treatment
Fully ablative or fractional ablative devices including CO2 and erbium laser are most commonly used. For darker skin types, the erbium laser may be preferred. Dermatologists may combine fully ablative with fractional laser treatment in the same session allowing treatment to the deeper component of the syringoma.
Healing times range from 5 to 14 days. In darker skin types, temporary hyper or hypo-pigmentation may occur which can last several months.
If fractional laser treatment is used on its own, without combined fully ablative laser, several treatments will be required for the best results. Fractional laser is sometimes used over the entire area around the eye to blend the fully ablated areas with the background skin if the treated areas are too pale.
Electrosurgery or diathermy can be successful for very small lesions or those containing milia. A needle point hyfrecator set at the lowest effective level is preferable to hot wire diathermy.
Syringoma removal
For syringomas localized to a small area, excision (surgical removal) of the area may be an excellent method of treatment. In fair-skinned individuals, scissor excision can be effective for protuberant lesions. However, excision is not recommended in darker skin types as pigment changes may occur and may take months to resolve.
Complications
Recurrence, hypertrophic (thick) or atrophic (depressed) scarring and excessive dyspigmentation (a too dark or too pale appearance) are uncommon complications.
What is the post treatment prognosis?
Treatment is usually successful. However, syringomas are likely to recur and maintenance treatment may be necessary. Recurring syringomas can be safely treated again.
References- Ghanadan A, Khosravi M. Cutaneous syringoma: a clinicopathologic study of 34 new cases and review of the literature. Indian J Dermatol. 2013;58(4):326. doi:10.4103/0019-5154.113956 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3726900
- Syringoma. https://www.dermnetnz.org/topics/syringoma/
- Guldbakke KK. Woman with translucent to yellow papules. J Am Acad Dermatol. 2006 Jul
- Syringoma. https://emedicine.medscape.com/article/1059871-overview
- Lee KK, Mehrany K, Swanson NA. Recognition and treatment of skin lesions. In: Cummings. Otolaryngology: Head & Neck Surgery, 4th ed. Philadelphia, PA: Mosby, Inc; 2005
- Marzano AV, Fiorani R, Girgenti V, Crosti C, Alessi E. Familial syringoma: report of two cases with a published work review and the unique association with steatocystoma multiplex. J Dermatol. 2009 Mar. 36(3):154-8
- Maeda T, Natsuga K, Nishie W, Yamashita K, Shimizu H. Extensive Eruptive Syringoma After Liver Transplantation. Acta Derm Venereol. 2018 Jan 12. 98 (1):119-120.