Tarlov cyst
Tarlov cysts also known as meningeal or perineural cysts or sacral nerve root cysts, are cerebrospinal fluid-filled sacs that most commonly are found at the base of the spine (the sacrum). Tarlov cysts affect the nerve roots in the sacrum, whereas the spinal nerve roots are embedded within the cyst wall or within the cyst cavity 1. Tarlov cysts were first described in 1938 by neurosurgeon, Isadore Tarlov. Tarlov cysts were an incidental finding during autopsy and were initially thought to be asymptomatic 2. A person can have one Tarlov cyst or multiple cysts, and symptoms may or may not be present, depending on the size and location of the cyst(s) 3. In general, the larger the cyst is, the more likely it is to cause symptoms 1. In some cases, a Tarlov cyst begins to cause symptoms following trauma or in response to a buildup of cerebrospinal fluid (CSF) 4. Examples of symptoms caused by a Tarlov cyst include pain especially in the buttocks or lower back when moving or changing position, sciatica (shock-like or burning pain in the lower back, buttocks, and down one leg to below the knee), muscle weakness, impaired reflexes, numbness or other sensation abnormalities, urinary incontinence, headaches (due to changes in cerebrospinal fluid pressure), loss of bowel control, constipation, sexual dysfunction (impotence), and some loss of feeling or control of movement in the leg and/or foot or other neurologic problems 1. Pressure on the nerves next to the cysts can also cause pain and deterioration of surrounding bone. Symptoms generally occur in the area of the body served by the involved nerves 3. Tarlov cysts may become symptomatic following shock, trauma, or exertion that causes the buildup of cerebrospinal fluid. Women are at much higher risk of developing these cysts than are men.
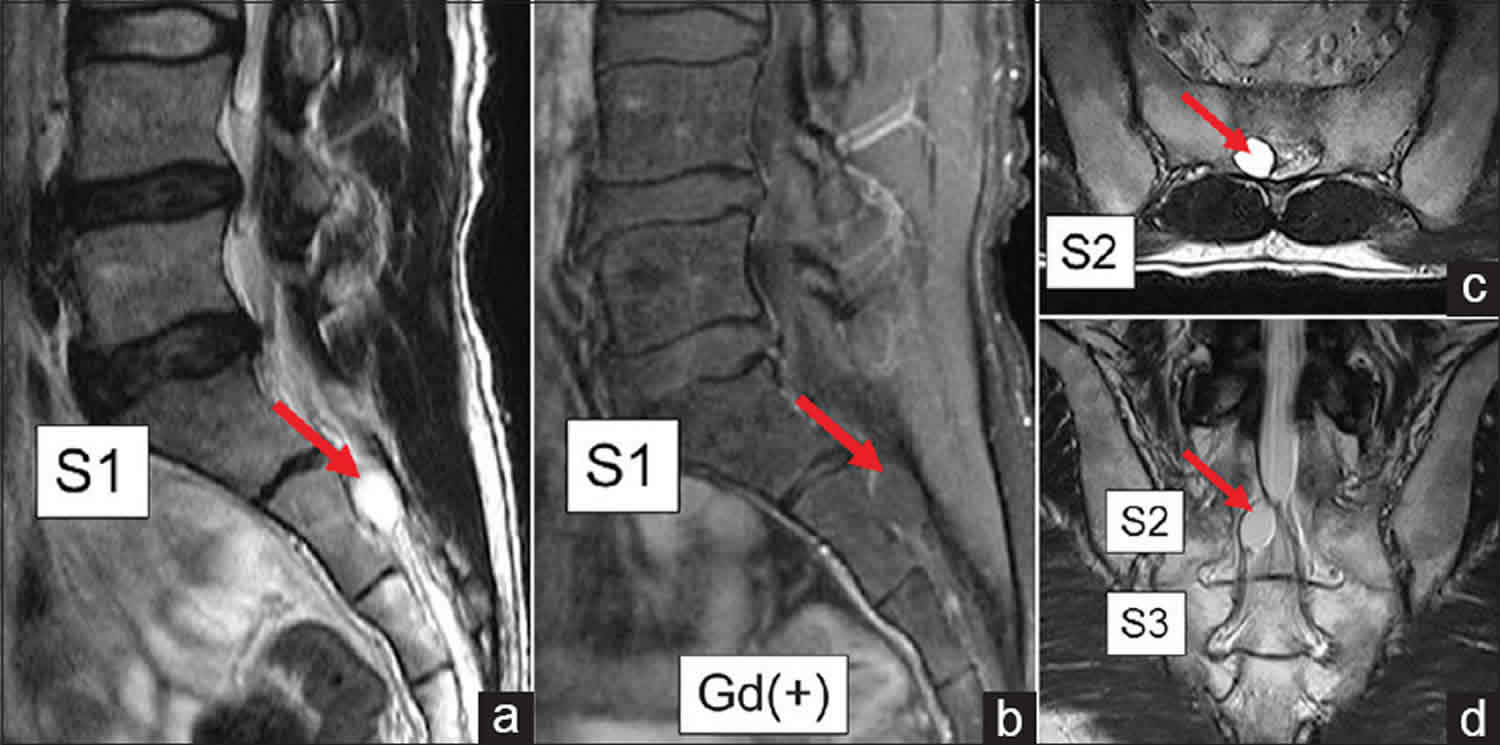
Diagnosing a Tarlov cyst can take a long time because there is limited awareness among primary care physicians and symptoms are similar to those of many other disorders or health problems. In some cases, a person may be misdiagnosed as having herniated discs, arachnoiditis, or gynecological conditions (in females). The diagnosis may ultimately be made following an magnetic resonance imaging (MRI) and/or CT myelogram due to pain, or sometimes following tests performed by a urologist due to bladder problems. However, it is estimated that the majority of Tarlov cysts observed by MRI cause no symptoms.
The exact cause of Tarlov cysts is not currently known. Tarlov cysts have been estimated to affect between 4.6 and 9% of the adult population 5. Tarlov cysts are most commonly found in Caucasian women 5. A study carried out in 2013 6 found that there was a significantly higher incidence of Tarlov cysts in women than in men, and referred to another paper by Landown et al 7 where 70% of cases were woman. An additional study published in 2013 called ‘Tarlov cysts: clinical evaluation of an Italian cohort of patients’ had a sample population of 157 patients with symptomatic Tarlov cysts; 88% were woman 8. Another paper published in 2016 documented the treatment of 213 patients with symptomatic Tarlov cysts by CT-guided injection of fibrin sealant. 89.9% of this patient cohort were woman 9.
In a recent Tarlov cyst survey, an estimated 86.6 percent of respondents were female and 13.4 percent were male. The largest majority of respondents were ages 31 to 60, with a combined total of 80.4 percent in that age demographic. An estimated 33 percent of respondents had a cyst(s) present in other parts of the body, most commonly the abdomen or hand and wrists 1.
An estimated 3 percent of respondents had no pain; 4.2 percent categorized their pain as very mild; 7.6 percent as mild; 31.5 percent as moderate; 38.6 percent as severe; and 15.1 percent as very severe 1.
Treatment depends on the symptoms and size of the Tarlov cyst(s). Many methods have been described with variable results 10. Non-surgical treatment options may include pain management, lumbar drainage of cerebrospinal fluid-filled (CSF), CT scan-guided cyst aspiration, and removing the CSF from inside the cyst and injecting the space with a fibrin sealant. However, these options do not prevent symptoms from returning. Surgical options may include opening and draining the cyst before filling it with fibrin sealant, laminectomy, removing the cyst or nerve roots, and other neurosurgical techniques 1.
Tarlov cyst long-term outlook (prognosis) varies from person to person depending on the severity of symptoms and effectiveness of treatment. Following surgery, some people have considerable relief of pain, while others have no change in symptoms. In some cases, surgery causes different symptoms or worsens existing symptoms 1. Residual symptoms following treatment may require continued pain management and changes in lifestyle. If left untreated, nerve root compression can cause permanent neurological damage 4.
Tarlov cyst causes
The exact cause of Tarlov cysts is unknown. Several theories exist including that the cysts result from an inflammatory process within the nerve root sheath or that trauma injures the nerve root sheath and causes leaking of cerebrospinal fluid (CSF) into the area where a cyst forms. Some researchers believe that an abnormal congenital connection (communication) exists between the subarachnoid space, which contains cerebrospinal fluid, and the area surrounding the affected nerves (perineural region). The connection may remain or eventually close, after allowing cerebrospinal fluid to leak out and cause a cyst. Because Tarlov cysts contain cerebrospinal fluid, researchers have speculated that normal fluctuations in CSF pressure may lead to an increase in cyst size and a greater likelihood of developing symptoms.
In many cases, individuals with asymptomatic Tarlov cysts developed symptoms following trauma or activities that raise cerebrospinal fluid pressure such as heavy lifting. Some reports suggest that individuals with connective tissue disorders are at a greater risk of developing Tarlov cysts than the general population.
More research is necessary to understand the underlying mechanisms that ultimately cause the development of Tarlov cysts or the onset of their symptoms.
Tarlov cyst symptoms
Many cases of Tarlov cysts are not associated with symptoms (asymptomatic). However, Tarlov cysts can grow in size eventually compressing or damaging adjacent nerve roots or nerves contained within the cyst (radiculopathy). The specific symptoms and their severity vary from one individual to another and with location along the spinal column.
Any of the following may be present in patients that have symptomatic Tarlov cysts:
- Pain in the area of the nerves affected by the cysts, especially the buttocks
- Pain in lower back (particularly below the waist) and in buttocks, legs, and feet
- Weakness of muscles and/or cramping in legs and feet / arms and hands
- Paresthesias (abnormal sensations) in legs and feet or arms and hands, dependent on cyst locations
- Difficulty sitting for prolonged periods
- Pain sitting or standing for even short periods of time
- Pain when sneezing or coughing
- Loss of sensation on the skin
- Loss of reflexes
- Bowel or bladder changes, including incontinence
- Changes in bowel function, such as constipation
- Changes in bladder function, including increased frequency or incontinence
- Inability to empty the bladder or in extreme cases to urinate at all requiring catheterization
- Changes in sexual function
- Pain in the chest, upper back, neck, arms and hands
- Swelling over the sacral (or cervical, thoracic, or lumbar) area of the spine
- Soreness, a feeling of pressure and tenderness over the sacrum and coccyx (tailbone), extending across the hip and into the thigh with cysts in the sacrum. Same feelings in upper sections of the spine dependent on cyst locations
- Headaches (due to the changes in the CSF pressure) and sometimes accompanied by blurred vision, double vision, pressure behind the eyes and optic nerve pressure causing papilledema (optic nerve swelling)
- Other sensory system symptoms: Tinnitus/Ear noises (ringing, buzzing, snapping,popping, cricket sounds,etc.)
- Dizziness and feeling of loss of balance or equilibrium, especially with change of position
- The feeling of sitting on a rock
- Pulling and burning sensation in coccyx (tailbone) area, especially when bending
- Sciatica
- Vaginal, rectal, pelvic and/or abdominal pain
- Restless leg Syndrome
- PGAD (Persistent Genital Arousal Disorder)
- Sexual dysfunction and painful intercourse
Chronic pain is a common with symptomatic Tarlov cysts. Pain from lumbo-sacral cysts may affect the lower back, especially below the waist, and spread to the buttocks and legs. Pain may be worsened by walking (neurogenic claudication). Symptoms may become progressively worse. In some individuals sitting or standing may worsen pain; recumbency may relieve pain. In some cases, pain can also affect the upper back, neck, arms and hands if the cysts are located in the upper spine. Pain may worsen when coughing or sneezing. Affected individuals have also reported vulvar, testicular, rectal, pelvic and abdominal pain.
Because Tarlov cysts can affect the nerves, symptoms relating to loss of neurological function can also develop including leg weakness, diminished reflexes, loss of sensation on the skin, and changes in bowel or bladder function such as incontinence or painful urination (dysuria). Some individuals may have difficulty empting the bladder and constipation has also been reported. Changes in sexual function such as impotence can also occur.
Affected individuals may also develop abnormal burning or prickling sensations (paresthesias) or numbness and decreased sensitivity (dysesthesia), especially in the legs or feet. Tenderness or soreness may be present around the involved area of the spine.
Additional symptoms have been reported in the medical literature including chronic headaches, blurred vision, pressure behind the eyes, dizziness, and dragging of the foot when walking due to weakness of the muscles in the ankles and feet (foot drop). Some individuals demonstrate progressive thinning (erosion) of the spinal bone overlying the cyst.
Tarlov cyst diagnosis
Tarlov cyst is difficult to diagnose because of the limited knowledge about the condition and because many of the symptoms can mimic other disorders. Most primary care physicians would not consider the possibility of Tarlov cyst. It is best to consult a neurosurgeon with experience in treating this condition.
Tarlov cysts may be discovered when patients with low back pain or sciatica have a magnetic resonance imaging (MRI) performed. Follow-up radiological studies, in particular, computed tomographic (CT) myelography are usually recommended.
If a patient has bladder problems and seeks medical help from an urologist, there are tests that can help diagnose Tarlov cyst. The standard urological tests for Tarlov cyst help determine if the patient has a neurogenic (malfunctioning) bladder. In urodynamics, the bladder is filled with water through a catheter and the responses are noted. Cystoscopy involves inserting a tube with a miniature video camera into the bladder via the urethra. A neurogenic bladder shows excessive muscularity. A third possible test is a kidney ultrasound to see if urine is backing up into the kidneys.
Tarlov cyst treatment
Tarlov cysts that do not cause symptoms should be monitored periodically to see whether cysts increase in size or whether symptoms develop. There is no specific, accepted therapy for individuals with symptomatic Tarlov cysts. Treatment is directed toward the specific symptoms that are apparent in each individual and may include drugs, surgery and other techniques. The response to various therapeutic options is highly individualized; what works for one person may be ineffective for another.
Non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed to treat nerve irritation and inflammation. A procedure known as transcutaneous electrical nerve stimulation or TENS may also be used to relieve nerve pain. During this procedure, electrical impulses are sent through the skin to help control pain.
Transcutaneous electrical nerve stimulation (TENS) has been proven useful for some in pain management. TENS devices deliver electrical impulses through the skin to the nerves to control pain. Unlike medications and topical ointments, TENS does not have any known side effects, other than skin irritation from the electrodes in some patients 11.
Tarlov cysts have been treated by procedures in which cerebrospinal fluid is drained from the cyst (aspiration). Results from such procedures vary and, in most cases, the cysts eventually fill up with cerebrospinal fluid again. In some cases, symptoms can return within hours.
Several different procedures, both surgical and nonsurgical, have been used that involve draining a Tarlov cyst and then filling the cyst with another substance such as fibrin glue, fat, or muscle. This prevents cerebrospinal fluid from refilling the cysts and reduces pressure on the surrounding nerves.
A nonsurgical procedure used to treat individuals with symptomatic Tarlov cysts uses a combination of substances that mimic blood clotting (fibrin glue). Fibrin glue injection is a minimally invasive procedure that has benefited some individuals with symptomatic Tarlov cysts. After the cysts are drained, fibrin glue is used to seal or “glue” the cyst closed preventing the cysts from filling up again. Some individuals have experienced immediate relief after this procedure; others reported delayed benefit. This procedure has led to short-term and long-term relief of symptoms in some cases. Complications have been reported in cases where the cyst communicates readily with the spinal fluid containing space.
Surgery
Surgical removal of Tarlov cysts may be used to treat symptomatic individuals who do not respond to other forms of therapy. Debate exists in the medical literature as to the most appropriate surgical technique to treat individuals with symptomatic Tarlov cysts. Various techniques have been used with different success rates and side effects. Surgical intervention depends upon numerous factors such as the progression of the Tarlov cysts; the degree of nerve root compression; the size of the connection between the subarachnoid space and the cyst; an individual’s age and general health; and/or other factors. Decisions concerning the use of particular interventions should be made by physicians and other members of the health care team in careful consultation with the patient, based upon the specifics of his or her case. A thorough discussion of the potential benefits and risks, patient preference and other appropriate factors is needed.
Very large cysts may require direct surgical intervention to drain and then obliterate the cyst. One surgical technique that has been used to treat symptomatic Tarlov cysts is an operation that exposes the region of the spine where the cyst is located by removal of overlying vertebral bone. The cyst is then sliced open with one or more thin cuts (fenestrations) and drained of fluid. The cyst wall is collapsed, circumferentially reinforced and sutured closed or the cavity is packed full of another substance such as fat or tissue adhesive to prevent it from refilling with cerebrospinal fluid.
In another procedure, after surgery to expose and drain the cysts, a flap of nearby muscle tissue is used to fill the cyst in order to prevent recurrence. A muscle flap is a portion of muscle that can be transferred along with its blood supply to an adjacent part of the body. The muscle flap is use to fill the decompressed cyst and to prevent it from refilling with cerebrospinal fluid. Results of treatment may be disappointing if irreversible nerve damage has already occurred.
A recent review analyzed the different surgical options, including the following 12:
- Sacral laminectomy with microsurgical cyst fenestration and cyst imbrication
- Sacral laminectomy with resection of the sacral cyst
- Microsurgical excision of the cyst along with duraplasty or plication of the cyst
- Release of the valve and imbrication of the sacral cysts with laminectomies
- Total or partial cyst wall removal, arranging the remaining nerve sheath, and repairing the local defect with muscle, gelfoam and fibrin glue
- Removing of the cyst and closure of defect by fibrin glue
- Microscopic cyst resection and closure of defect by fibrin glue
- Microsurgical fenestration from the cyst to the thecal sac
- Fenestration of the cyst and closure of the opening by stitches and glue
- Cyst remodeling around the root using titanium clips
- Cyst excision and occlusion of its neck.
The authors of this review concluded that the best results are obtained with the complete removal of the cyst and closure of the defect by fibrin glue, microscopic cyst resection and closure of the defect by fibrin glue, or cyst removal with closure of its neck 12.
Tarlov cyst prognosis
Postoperative CSF leak is the most common complication, but in some cases, these leaks may self-heal. Patients may be advised to stay in bed with the foot of the bed raised and to wear a corset to control swelling. Although it is low, there is a risk of developing bacterial meningitis. Although some patients have noted a considerable decrease in pain, the most common negative outcome is the failure of the surgery to eliminate the symptoms. In some cases, the surgery may cause an existing symptom to worsen or it may cause a new one.
When all treatment options have been exhausted, it is very important for the patient to make any necessary lifestyle changes and to undertake a pain management strategy with his or her physician. Supervised pain management, as well as support groups, can help a patient cope and improve his or her quality of life.
References- Tarlov Cyst. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Tarlov-Cyst
- Tarlov IM. Perineurial cysts of the spinal nerve roots. Arch Neurol Psychiatry 1938;40:1067–74. 10.1001/archneurpsyc.1938.02270120017001
- Tarlov Cysts. https://rarediseases.org/rare-diseases/tarlov-cysts
- Tarlov Cysts Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Tarlov-Cysts-Information-Page
- Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts). AJNR Am J Neuroradiol 1994;15:293–7.
- Burdan F, Mocarska A, Janczarek M, et al. Incidence of spinal perineurial (Tarlov) cysts among East-European patients. PLoS One 2013;8:e71514 10.1371/journal.pone.0071514
- Langdown AJ, Grundy JR, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech 2005;18:29–33. 10.1097/01.bsd.0000133495.78245.71
- Marino D, Carluccio MA, Di Donato I, et al. Tarlov cysts: clinical evaluation of an italian cohort of patients. Neurological Sciences 2013;34:1679–82. 10.1007/s10072-013-1321-0
- Murphy K, Oaklander AL, Elias G, et al. Treatment of 213 Patients with Symptomatic Tarlov Cysts by CT-Guided Percutaneous Injection of Fibrin Sealant. AJNR Am J Neuroradiol 2016;37:373–9. 10.3174/ajnr.A4517
- Elsawaf A, Awad TE & Fesal SS. Surgical excision of symptomatic sacral perineurial Tarlov cyst: case series and review of the literature. Eur Spine J. May 6, 2016; https://www.ncbi.nlm.nih.gov/pubmed/27154168
- Tarlov Cyst Information. https://www.tarlovcystfoundation.org/info/
- Elsawaf A, Awad TE, Fesal SS. Surgical excision of symptomatic sacral perineurial Tarlov cyst: case series and review of the literature. Eur Spine J. 2016;25(11):3385–3392. doi:10.1007/s00586-016-4584-3