Thoracic aorta
Thoracic aorta is a continuation of the descending aorta. The thoracic aorta is contained in the posterior mediastinal cavity. Thoracic aorta begins at the lower border of the fourth thoracic vertebra. The thoracic aorta descends on the bodies of the thoracic vertebrae (T5–T12) just to the left of the midline and ends in front of the lower border of the twelfth thoracic vertebra, at the aortic hiatus in the diaphragm where it becomes the abdominal aorta. At its commencement, it is situated on the left of the vertebral column; it approaches the median line as it descends; and, at its termination, lies directly in front of the vertebral column. Along the way, the thoracic aorta gives off multiple vessels before exiting the thoracic cavity, including arteries to supply the pericardium, bronchi, mediastinum, and esophagus; it also gives off the superior phrenic arteries, posterior intercostal arteries, and subcostal arteries.
The thoracic aorta passes through the diaphragm at the level of vertebra T12 and enters the abdominal cavity as the abdominal aorta, which lies on the lumbar vertebral bodies in the midline. The abdominal aorta ends at the level of vertebra L4, where it divides into the right and left common iliac arteries, which supply the pelvis and lower limbs.
Thoracic aorta branches
The thoracic aorta gives off several paired branches as it descends in the thorax. These includes the
- Bronchial arteries. The bronchial arteries supply systemic (oxygenated) blood to the lung structures. Usually, two bronchial arteries serve the left lung, and one serves the right lung; in some people they arise from posterior intercostal arteries instead of the aorta. Bronchial arteries enter the lung’s medial surface along with the large pulmonary vessels.
- Esophageal arteries. The thoracic aorta also sends several small branches to the esophagus directly anterior to it, as well as to the posterior part of the mediastinum and pericardium.
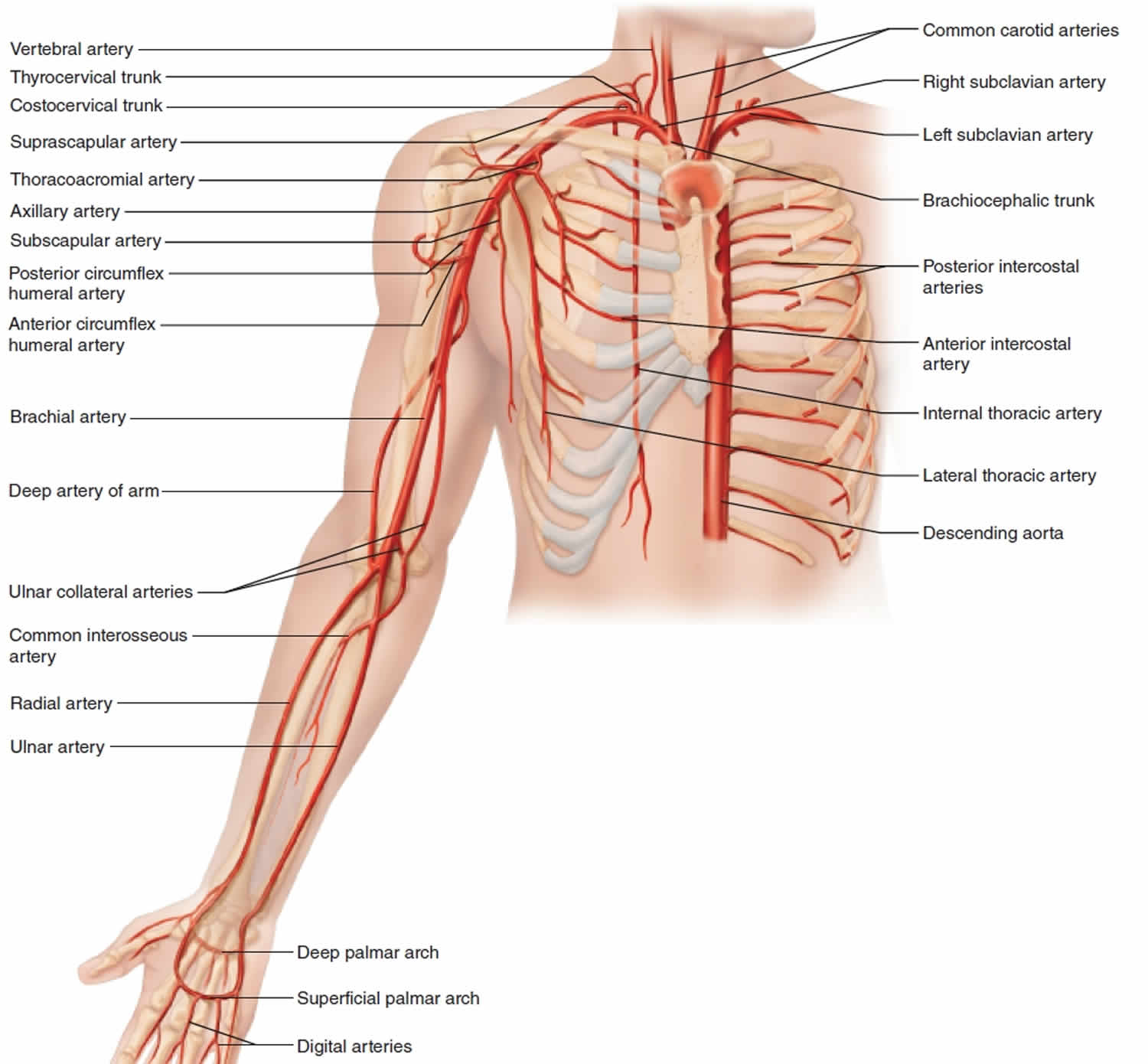
- Posterior intercostal arteries
The posterior thoracic wall receives its blood from the posterior intercostal arteries. The superior two pairs arise from the costocervical trunk, whereas the inferior nine pairs issue from the thoracic aorta. All of the posterior intercostal arteries run anteriorly in the costal grooves of their respective ribs. In the lateral thoracic wall, they form anastomoses with the anterior intercostal arteries. Inferior to the twelfth rib, one pair of subcostal arteries branches from the thoracic aorta. Finally, a pair of superior phrenic arteries leaves the most inferior part of the thoracic aorta to supply the posterior, superior part of the diaphragm.
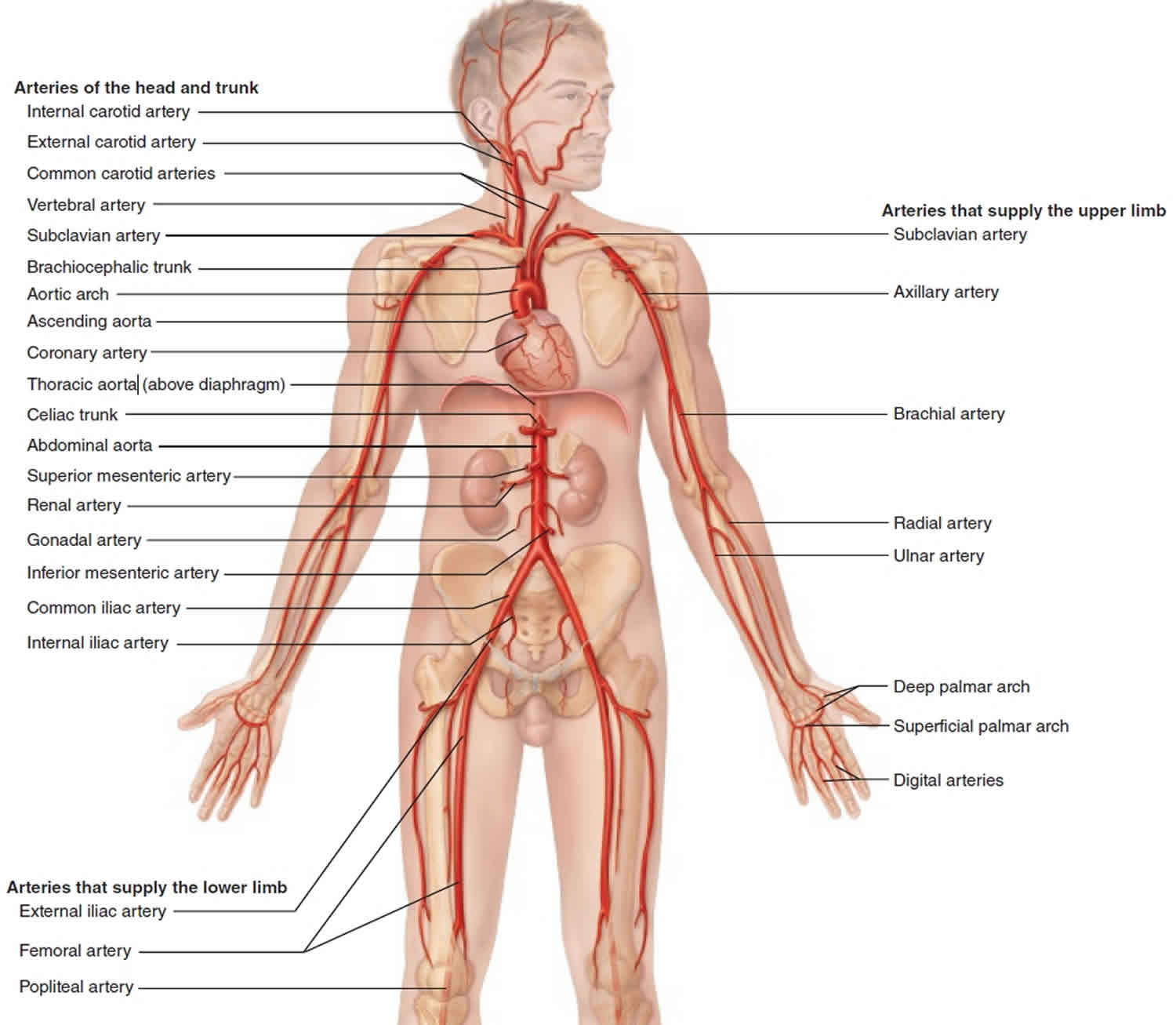
Figure 1. Thoracic aorta branches
Thoracic aorta function
The thoracic aorta gives off multiple vessels before exiting the thoracic cavity, including arteries to supply the pericardium, bronchi, mediastinum, and esophagus; it also gives off the superior phrenic arteries, posterior intercostal arteries, and subcostal arteries.
Enlarged thoracic aorta
A thoracic aortic aneurysm refers to a dilatation of the proximal ascending aorta; this is most often the result of chronic hypertension when seen in adults 1. In young adults, the most common underlying factor is a connective tissue disorder such as Marfan syndrome or Ehler-Danlos syndrome. An aortic aneurysm is of concern because dilation of the aorta results in weakening of the aortic wall, increasing risk of aortic rupture or dissection. For this reason, elective repair is often the recommendation once an aneurysm has reached a diameter of 5.5cm or greater 2. Elective repair can reduce the risk of rupture and survival to near normal.
References- Shahoud JS, Bolla SR. Anatomy, Thorax, Heart Aorta. [Updated 2019 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538140
- Coady MA, Rizzo JA, Hammond GL, Kopf GS, Elefteriades JA. Surgical intervention criteria for thoracic aortic aneurysms: a study of growth rates and complications. Ann. Thorac. Surg. 1999 Jun;67(6):1922-6; discussion 1953-8.