What is tonometry
Tonometry is a test to measure the pressure inside your eyes. Tonometry test is used to screen for glaucoma. Tonometry is also used to measure how well glaucoma treatment is working. Tonometry test may also be done before and after eye surgery.
Your eyes constantly make a fluid called aqueous humor. As new aqueous flows into your eye, the same amount should drain out through a tiny drainage area. This process keeps pressure in your eye (called intraocular pressure or IOP) stable. But if the drain is not working properly, fluid builds up. Pressure inside the eye rises, damaging the optic nerve. This is often how glaucoma develops.
Each person’s eye pressure is different, and there is no single correct pressure for everyone. Generally, the range for normal pressure is between 10 and 21 mmHg (“mmHg” means “millimeters of mercury,” a scale used to record eye pressure).
Most people who have glaucoma will have an eye pressure higher than 21 mmHg. However, some people with pressures between 10 and 21 mmHg may have glaucoma.
People over age 40 years, particularly African Americans, have the highest risk for developing glaucoma. Regular eye exams can help detect glaucoma early. If it is detected early, glaucoma can be treated before too much damage is done.
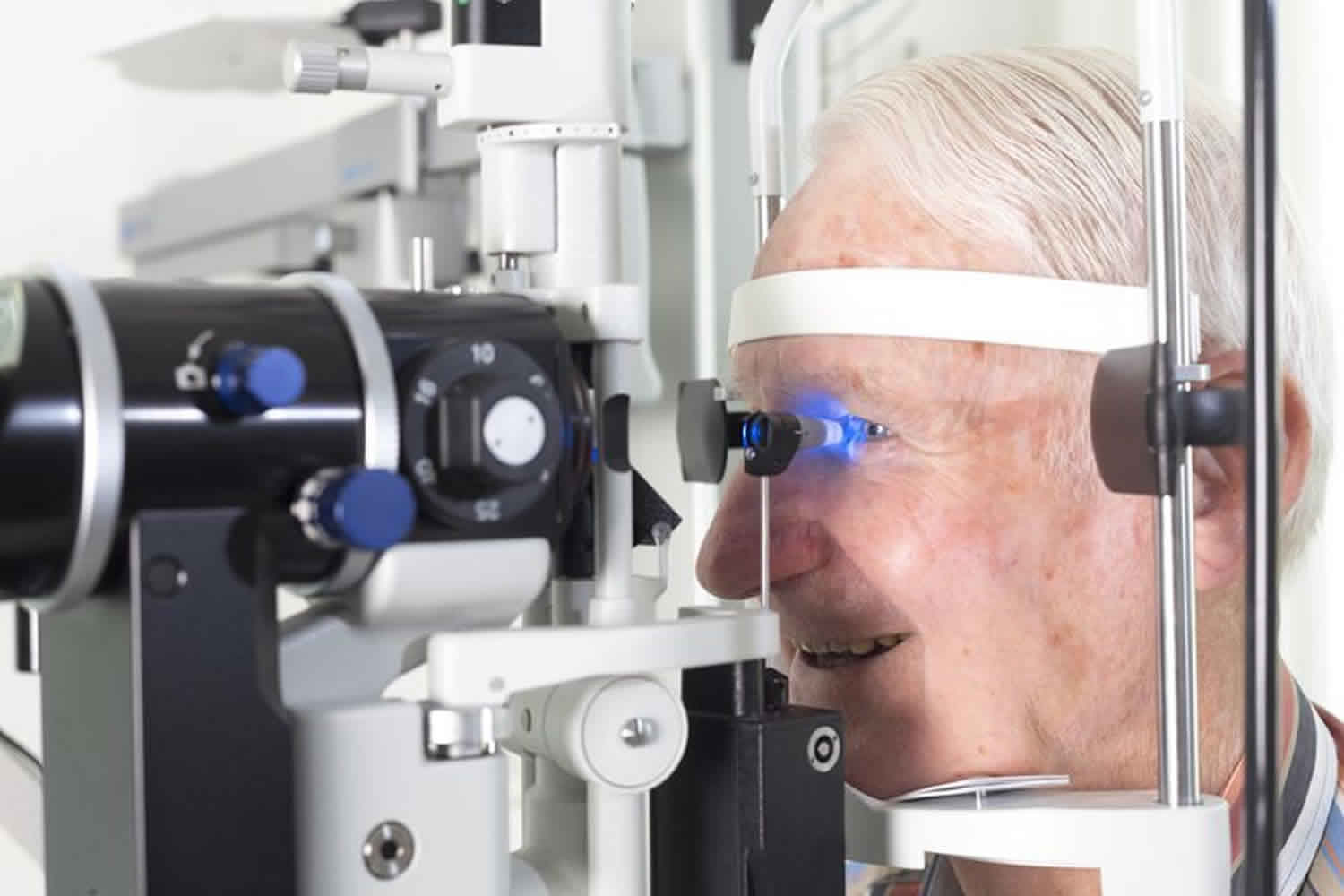
As part of a complete eye exam, your ophthalmologist or an assistant will measure your eye pressure. This pressure check is called tonometry.
Your ophthalmologist will determine the eye pressure range that is healthy specifically for you.
In the past, you may have had an eye pressure test using a puff of air. Now most ophthalmologists use a more accurate device that measures pressure by direct contact with the eye.
Tonometry test
Applanation Tonometry
Goldmann applanation tonometry
Goldmann applanation tonometry is considered the standard method for measuring intraocular pressure and is most frequently used by ophthalmologists in the clinical setting. It utilizes applanation, which is the measurement of the force required to compress the cornea over a given area. The higher the intraocular pressure, the greater the force needed to compress the cornea 1. Eye clinicians use Goldmann tonometry as a standard component of a slit-lamp eye exam 2. To perform Goldmann applanation tonometry, topical anesthetic drops and a fluorescein dye are first applied to the eyes. Filtered cobalt blue light is then used to visualize the fluorescein dye while the tonometer tip compresses the center of the cornea. The blue light and dye highlight the circular border of the tear film created by the applanator tip pressed against the cornea. A prism in the tip splits this circular film of fluorescein into two green semicircles when visualized from the slit lamp oculars. The clinician then alters the tonometer force against the cornea until the two semicircles overlap slightly (Figure 1). This slight overlap of the two semicircles indicates the cornea has been flattened by a calibrated amount to give an accurate intraocular pressure reading, measured in millimeters of mercury, that is read on the dial of the tonometer 3. Disadvantages of the Goldmann method include a high level of skill to operate, inability to measure in supine patients, need for topical anesthesia, and decreased accuracy on an irregular or scarred cornea 2.
Figure 1. Goldmann applanation tonometry

Perkins Applanation Tonometer
This hand-held tonometer uses the same mechanism of applanation as the Goldmann. However, due to its portability, it can be useful in settings where a slit lamp exam is not feasible, such as an emergency department or operating room. It can also be used in the upright or supine patient. Disadvantages of the Perkins method include a high level of skill to operate, decrease in stability with a handheld instrument, need for topical anesthesia, and decreased accuracy on an irregular or scarred cornea 2.
Non-contact Tonometers
Non-contact tonometers are also known as “air-puff” tonometers. They use a small puff of air directed at the cornea. The returning air from the surface of the cornea is measured by a membrane that records the force, which is converted to intraocular pressure. Advantages of this method include no requirement for topical anesthesia and its usefulness in screening, especially in children and adults who are unable to tolerate contact methods 1. However, it is considered a less accurate method than GAT or pneumotonometer, although it has been shown to have comparable readings to GAT in some studies [4]. Non-contact tonometers are available in table-top and portable devices 2.
Ocular-Response Analyzer
This is a recently developed type of non-contact tonometer that utilizes a column of air as the applanating force to deform the cornea. Based on the force of airflow and the rate of recovery from deformation, the optical sensors can evaluate the elasticity of the cornea to provide a corrected intraocular pressure and corneal hysteresis value 2. Corneal hysteresis is the ability of the cornea to absorb and dissipate applied forces based on its viscoelastic properties. ORA is designed to improve IOP accuracy as it allows clinicians to account for the variability in corneal biomechanical properties seen among patients 2. Corneal hysteresis has been demonstrated to contribute to glaucoma progression risk with lower values imparting a greater risk of glaucoma progression 4. Ocular-Response Analyzer cannot be used on supine patients.
Indentation Tonometry
Tono-Pen Indentation tonometry
The Tono-pen is an electronic hand-held device that uses a small plunger to record the force needed to applanate the cornea. The Tono-pen averages multiple readings of this small force that is converted to intraocular pressure 2. It requires daily recalibration, topical anesthesia, and uses disposable covers. It can prove useful in portable screenings, emergency rooms, or operating rooms to measure intraocular pressure. Advantages of this method include the ability measure over soft contact lens, on an irregular corneal surface, averaging of multiple readings, and potential to measure at peripheral cornea if a central corneal scar or ulcer exists. It can also measure intraocular pressure independent of patient position 2.
Pneumatonometer
A pneumatonometer uses a stream of air to indent the cornea with a 5 mm diameter silicone tip. The force of air that indents the cornea is recorded and converted to intraocular pressure. This method correlates well with Goldmann tonometry in normal pressure ranges 2. Similar to the Tono-pen, it has the advantages of measuring irregular cornea surfaces, over soft contact lens, at the peripheral cornea, and accuracy is independent of patient position, although it requires topical anesthesia 2. The pneumatonometer is accessible in a hand-held probe attached to a table-mounted device. The device is also used for pneumatonography, which uses changes in intraocular pressure to measure the outflow resistance of aqueous humor from the anterior chamber. If increased outflow resistance is found, it can cause increased intraocular pressure and contribute to glaucoma. Algorithms are used to correlate the pneumatonography values to a Shiotz-based tonograph, but with shorter potential measurement times.
Schiotz tonometry
This portable tonometer employs a rarely used, older technique. It consists of a weighted plunger attached to a footplate positioned on the cornea. Weights are stacked onto the probe to cause depression of the cornea. The number of weights stacked onto the probe correlates to a calibrated intraocular pressure, using a conversion chart provided with the device 2. The patient must be supine during measurement, and topical corneal anesthetic is required 1.
Rebound Tonometry
I-Care tonometry
This is a portable and simple-to-use hand-held device that uses a small probe that bounces of the cornea in the horizontal plane. The deceleration of the probe produces a level of voltage that is converted to intraocular pressure. The faster the rate of deceleration against the cornea, the higher the pressure. The slower the rate of deceleration, the lower the pressure 2. Advantages of this method include no requirement for topical anesthetics and its usefulness in children and dementia patients who are not tolerant of a slit-lamp exam or more involved contact methods 2. It cannot be used on supine patients, and accuracy decreases in the setting of corneal edema, making it less useful with acute intraocular pressure elevation associated with acute angle closure with corneal edema.
Dynamic Contour Tonometry (DCT)
Pascale dynamic contour tonometry
This device utilizes a contour-matched, piezoelectric sensor to measure minuscule dynamic pulsations in intraocular pressure at the cornea 2. This method allows measurement of intraocular pressure without deforming the cornea and therefore its readings are independent of corneal thickness, unlike other methods 2. It is considered a more accurate method on regularly shaped corneas, but it’s more difficult to use properly. It also requires topical anesthesia and is less accurate on irregular corneas 4.
How the tonometry test is performed
There are three main methods of measuring eye pressure.
The most accurate method measures the force needed to flatten an area of the cornea.
- The surface of the eye is numbed with eye drops. A fine strip of paper stained with orange dye is held to the side of the eye. The dye stains the front of the eye to help with the exam. Sometimes the dye is in the numbing drops.
- You will rest your chin and forehead on the support of a slit lamp so that your head is steady. You will be asked to keep your eyes open and to look straight ahead. The lamp is moved forward until the tip of the tonometer just touches the cornea.
- Blue light is used so that the orange dye will glow green. The health care provider looks through the eyepiece on the slit-lamp and adjusts a dial on the machine to give the pressure reading.
- There is no discomfort with the test.
A second method uses a handheld device shaped like a pencil. You are given numbing eye drops to prevent any discomfort. The device touches the surface of the cornea and instantly records eye pressure.
The last method is the noncontact method (air puff). In this method, your chin rests on a device similar to a slit lamp.
- You stare straight into the examining device. When you are at the correct distance from the device, a tiny beam of light reflects off of your cornea onto a detector.
- When the test is performed, a puff of air will slightly flatten the cornea; how much it flattens depends on the eye pressure.
- This causes the tiny beam of light to move to a different spot on the detector. The instrument calculates eye pressure by looking at how far the beam of light moved.
Tonometry contraindications
Tonometry contraindications include:
- Ruptured globe: Avoid tonometry in the setting of a ruptured globe or suspicion of one. Additional pressure on the globe with tonometry methods can further damage the globe and cause extrusion of aqueous and vitreous humor. A ruptured globe is often apparent in an acute situation with the examination of the anterior ocular anatomy.
- Infection (relative): When an infection such as keratoconjunctivitis is suspected in one eye, thoroughly disinfect or use a new cover before measuring the contralateral eye and between patients to prevent disease transmission 1.
- Unhealed corneal abrasions or ulcers: Manipulation with tonometry can further aggravate the lesion 3. Methods such as the Tono-Pen and pneumatonometer provide the ability to measure intraocular pressure at the peripheral cornea if the corneal lesion is located centrally.
- Inability to administer topical anesthesia can be a contraindication depending on the method, as most methods of tonometry require topical anesthesia before measurement of intraocular pressure. Methods that do not require topical anesthesia include rebound (I-Care) and non-contact “air puff” tonometry.
Tonometry results
Normal Results
A normal result means your eye pressure is within the normal range. The normal eye pressure range is 10 to 21 mm Hg.
The thickness of your cornea can affect measurements. Normal eyes with thick corneas have higher readings, and normal eyes with thin corneas have lower readings. A thin cornea with a high reading may be very abnormal (the actual eye pressure will be higher than shown on the tonometer).
A corneal thickness measurement (pachymetry) is needed to get a correct pressure measurement.
Talk to your doctor about the meaning of your specific test results.
What Abnormal Results Mean
Abnormal results may be due to:
- Glaucoma
- Hyphema (blood in the front chamber of the eye)
- Inflammation in the eye
- Injury to the eye or head
Tonometry risks
Corneal abrasion, aggravation of globe rupture, transmission of infection, and reaction to ocular drugs are potential complications of tonometry. If the applanation tonometry method is used, there is a small chance the cornea may be scratched (corneal abrasion). The scratch will normally heal within a few days. Risk of these complications is considerably low (less than 1%) 5.
References- Alguire PC. Tonometry. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Butterworths; Boston: 1990.
- Aziz K, Friedman DS. Tonometers-which one should I use? Eye (Lond). 2018 May;32(5):931-937
- Stevens S, Gilbert C, Astbury N. How to measure intraocular pressure: applanation tonometry. Community Eye Health. 2007 Dec;20(64):74-5
- Alguire PC. Tonometry. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Butterworths; Boston: 1990
- Bader J, Havens SJ. Tonometry. [Updated 2018 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493225