What is tracheoesophageal fistula
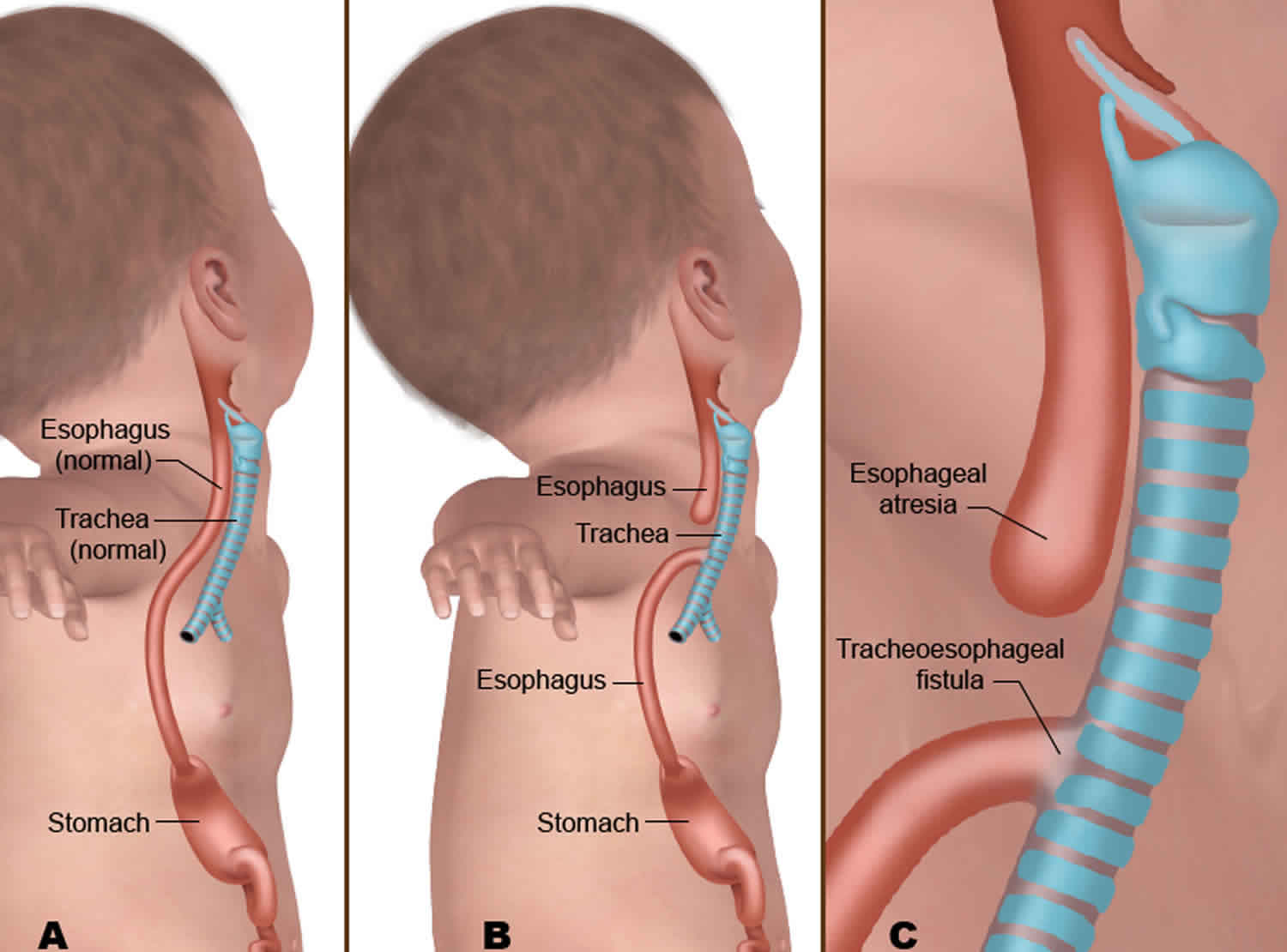
Tracheoesophageal fistula, also known as TE fistula or TEF, is an abnormal connection (fistula) in one or more places between the trachea (windpipe) and the esophagus (tube from the mouth to the stomach) that results from these two structures not forming separately. Your baby may also have esophageal atresia, meaning the esophagus does not develop all the way to the stomach but ends as a pouch in the upper chest. Infants with tracheoesophageal fistulas tend to have rounded abdomens and bowel sounds, while those with esophageal atresia without a fistula tend to have scaphoid abdomens and absent bowel sounds. Ask your doctor to draw on this picture, to show you your baby’s condition.
Esophageal atresia (EA) and tracheoesophageal fistula (TEF) are rare conditions that develop before birth. They often occur together and affect the development of the esophagus, trachea or both. These conditions can be life-threatening and must be treated shortly after birth.
During normal prenatal development, the trachea (which connects the throat to the lungs) and esophagus (which connects the back of the mouth to the stomach) start out as a single tube. While babies are developing in the womb, a wall usually forms in the tube — dividing it into two separate tubes that have no connections. The trachea is for air, the esophagus is for food.
If the esophagus and trachea form abnormally or don’t divide completely, an esophageal atresia and/or tracheoesophageal fistula can occur.
Tracheoesophageal fistula in newborns is slightly different, in that babies with tracheoesophageal fistula can swallow breast or bottle milk. However, the liquid often leaks through the fistula between the esophagus and trachea and travels to the lungs. This can cause infections or pneumonia.
Neonates with tracheoesophageal fistula should be nursed preoperatively prone or in lateral position at an incline of 30° to decrease the risk of pulmonary aspiration. A suction catheter may be placed in the esophageal pouch preoperatively to decrease the accumulation of saliva and reduce the risk of aspiration. It is not uncommon for the neonate to undergo staged repairs of the lesions. A gastrostomy tube to vent the stomach and a central line for total parenteral nutrition may be placed under sedation with local anesthesia or general anesthesia. Thus, allowing the infant to receive long-term nutrition and continue to grow so that the esophageal anastomosis can be performed when the infant is older. When the infant is older, the distance between the esophageal pouch and stomach is decreased.
Associated conditions
In particular, esophageal atresia or tracheoesophageal fistula has been linked to:
- VACTERL syndrome, a complex condition that includes a group of birth defects often seen together that affect the vertebrae, anus, heart (cardiac), trachea, esophagus, kidney (renal), and limbs
- Digestive tract problems such as congenital diaphragmatic hernia, duodenal atresia, or imperforate anus
- Heart problems such as ventricular septal defect, tetralogy of Fallot, or patent ductus arteriosus
- Kidney and urinary tract problems such as horseshoe or polycystic kidney, absent kidney, or hypospadias
- Muscular or skeletal problems
- Trisomy 13, Trisomy 18 and Trisomy 21 (Down syndrome)
If your esophageal atresia and tracheoesophageal fistula baby has no other associated problems, the outlook is excellent. Most children grow up to live normal lives. The outlook for children with esophageal atresia and tracheoesophageal fistula who have other difficulties, such as extreme prematurity and heart conditions will vary depending on how severe these other problems are.
There are a few problems which may happen after surgery that you should know about. They happen most often in the first few years after the operation and improve as your child grows older.
Figure 1. Tracheoesophageal fistula
Footnote: (A) Normal anatomy of baby’s esophagus and trachea. (B) During prenatal development, a baby’s upper digestive tract may form abnormal gaps and connections. (C) These birth defects are known as esophageal atresia and tracheoesophageal fistula.
What is VACTERL Association?
Tracheoesophageal fistula and esophageal atresia is one of several birth defects that often occur together. Doctors have grouped these conditions under the acronym VACTERL. Up to half of babies with tracheoesophageal fistula/esophageal atresia have one or more of these additional conditions.
- Vertebral (spinal) defects
- Anorectal atresia (malformation of the anus)
- Cardiac (heart) defects
- Tracheoesophageal fistula/esophageal atresia
- Renal (kidney) anomalies
- Limb (usually arm) defects
How is tracheoesophageal fistula or esophageal atresia managed before birth?
The prenatal management of babies with tracheoesophageal fistula or esophageal atresia starts with acquiring as much information about the condition—and possible co-existing VACTERL conditions—as early as possible. To gather that information, we use several different techniques, including high-resolution fetal ultrasonography, fetal echocardiography and fetal magnetic resonance imaging (MRI).
How is tracheoesophageal fistula/esophageal atresia treated after birth?
Infants with tracheoesophageal fistula and esophageal atresia can be delivered vaginally. The goal will be to have your baby’s birth occur as near to your due date as possible. Your baby will be born at a specialized birth center located within the hospital complex. This means that your baby will be born just a few feet down the hall from our newborn intensive care unit (NICU). Also, many of the physicians you have already met will be present during or immediately after your baby’s birth to help care for your baby right away.
Most babies with tracheoesophageal fistula or esophageal atresia are comfortable breathing on their own after birth. But your baby will be unable to nurse or take a bottle and will be fed intravenously instead. In addition, a small suction tube will be inserted into your baby’s esophageal “pouch” to keep the saliva your baby swallows from entering the trachea and overflowing into the lungs.
Our goal will be to make a definitive diagnosis of tracheoesophageal fistula or esophageal atresia as quickly as possible. The diagnosis can be made with a simple x-ray, done soon after birth. Other tests, including an ultrasound scan and an echocardiogram, will also be conducted to identify any co-existing VACTERL conditions.
When will my baby have an operation?
Tracheoesophageal fistula and esophageal atresia repair requires an operation to close the fistula and repair the esophagus and trachea. Surgery for esophageal atresia is not considered an emergency, and is typically done when the baby is two or three days old.
In most cases of tracheoesophageal fistula and esophageal atresia repair, the surgeon cuts through the abnormal connection (fistula) between the windpipe and esophagus and then sews together the two ends of the esophagus. The windpipe is also repaired. But the exact nature of your baby’s surgery will depend on the specific defects in your baby’s digestive tract.
The surgery is done under general anesthesia. After the procedure, your baby will be returned in the NICU. For several days, your baby may need a machine (ventilator) to help with breathing.
Care of your tracheoesophageal fistula baby
Caring for your baby does not begin when you take your baby home. You can share in your baby’s care while still in hospital. Don’t be afraid to ask questions, even the same question over and over again. It is often hard to fully understand things when you are worried or anxious. People caring for babies and children in hospital understand that all parents are worried and anxious when their child is not well and needing medical attention. Confused feelings are normal at this early time.
Many parents speak of their deep disappointment that they were unable to take their baby home from the maternity hospital in the usual way. Sometimes people can feel confused and angry. Most parents feel frightened to see their baby connected up to tubes and machines. Some parents may not want to see their baby until they are well on the road to recovery and free of equipment. If that is the way you feel, remember that these feelings are perfectly normal. The sooner parents are involved with their baby the better. The more you know your child and care for them in hospital, the easier it will be when you take your baby home.
Parents are the real experts in the care of their child. Every tracheoesophageal fistula child, like every other child, is different. Though you need the help of other experts for a time, you are the most important people in the team caring for your child. A multidisciplinary team of experts will help you look after your baby by monitoring their progress during regular clinic visits.
Problems your child may have in the early years
It is important to know that your child may experience problems in the early years. Problems include swallowing difficulties and a higher number of childhood coughs and colds. It is important to keep in close touch with your baby’s doctor about anything that you are worried about. The following gives you an idea of problems that can occur:
Swallowing problems
Many children with esophageal atresia or tracheoesophageal fistula experience some form of feeding difficulty, however the amount of difficulty varies between children. Feeding will improve as your child gets older.
When you take your baby home you will be given a feeding program suitable for your baby and their specific needs. You should start feeding orally as soon as your child is allowed. Many children can breastfeed. As many children with esophageal atresia or tracheoesophageal fistula suffer from gastroesophageal reflux (GER), they often cope better with smaller more regular feeds.
Solids should be introduced around 6 months, as they would with any other baby, unless you are told otherwise by your doctor.
As your baby grows you will add solids and increased varieties of foods. Often children with esophageal atresia or tracheoesophageal fistula have difficulty progressing with their food textures from very smooth runny purees to more solid or lumpy foods.
Esophageal atresia or tracheoesophageal fistula children may take longer than usual with the introduction of solids into their diet. In order to give your baby a good start to feeding, your child needs to stay on smooth purees and “mushy foods” for a longer period of time to reduce the risk of choking. Feeding should be done under close supervision to reduce the risk of choking.
A blender or small mincer is really helpful when preparing “mushy” food.
Experts recommend that you give your baby a wide range of food. Frequent and early exposure to a wide range of tastes has been shown to play a major role in what food children will eat.
Common problem foods for children with esophageal atresia or tracheoesophageal fistula include:
- meat (unless pureed or minced)
- bread/doughy foods
- hard raw vegetables (carrots, apples)
- foods with skins (grapes, tomatoes).
When you introduce new foods, always blend, mince or chop them finely. When your child gets used to eating the new food, gradually make the sizes bigger. Also let your child watch you cut it up. Give them a nibble while you are doing it. As they grow, they won’t be afraid to eat new things if you have been introducing them to food gradually.
Some children complain of problems with swallowing and need to have a drink with all food. This is often caused by the esophagus not being coordinated.
Try to make sure that meal times are quiet and peaceful (this is not always easy with a young, energetic family). When children are in a hurry or excited, swallowing problems are more likely to occur. During social occasions keep an eye on your child. Things like nuts and potato crisps left at the child’s level can be a significant problem.
The Speech Pathologist and Dietician can give more individualized advice on feeding. They can help you with advice on weaning and suggest the types of foods that are most suitable for your child as they grow older. The Speech Pathologist can help with problems with swallowing including troubles with textures and also help with exercises to help with chewing and swallowing at meal times. The Dietician can help with ensuring your child’s intake is meeting their nutritional needs and recommend higher energy options or additions if there are concerns with growth.
Stricture
Sometimes the esophagus becomes narrow at the site of the join (anastomosis) – this is called a stricture. Babies with a stricture have problems swallowing and may have increased vomiting or may choke or gag with feeds. Stricture is treated with dilation (stretching the narrowed food pipe). This procedure is done under a general anesthetic either in the radiology department or with the help of an endoscope in the operating theater. The purpose is to widen the narrowed esophagus to help with feeding.
Reflux
Children with esophageal atresia or tracheoesophageal fistula often develop a problem with gastro-esophageal reflux disease (GERD). This is where the contents of the stomach flow back up the esophagus causing pain and irritation. This may cause a baby to vomit, but not always. As acid reflux can irritate the oesophagus and increase the chances of stricture, your child will be started on an anti-reflux medication after the initial operation to reduce the risk of this developing. Your child will need regular surveillance endoscopies to monitor their gastro-esophageal reflux.
Tracheomalacia
In addition to a possible abnormal connection (fistula) between your baby’s windpipe (trachea) and food pipe (oesophagus), the windpipe in children with esophageal atresia or tracheoesophageal fistula is unduly floppy due to a lack of properly developed cartilage to support its walls. This is known as “tracheomalacia” (or soft trachea) and may cause noisy breathing at rest or with activity, a loud “barking” cough, reduced ability to bring up phlegm/sputum and breathing difficulties.
Many, but not all children with esophageal atresia or tracheoesophageal fistula suffer from what has become known as the “tracheoesophageal fistula” cough. This is a harsh, brassy, “barking” cough, which sounds as if the child is very sick. Remember, this does not mean that your child is sick and often family and friends need to be reassured that your child is fine.
Sometimes due to their floppy windpipe, your child might experience a sudden breath-holding episode or “blue spell”. This usually happens during eating, if a piece of food becomes stuck in the food pipe. The lump of food puts pressure on the windpipe significantly narrowing it so that air cannot move in and out. As a result, breathing becomes extremely difficult and your child may change color, becoming a dusky red or even blue. Please contact your doctor immediately if this happens.
Respiratory problems
Children with esophageal atresia or tracheoesophageal fistula are more likely to experience prolonged colds and even pneumonia in the first few years of life. This is because they cannot clear their secretions effectively due to their floppy windpipe. Although this is likely to improve by the early school years, chest physiotherapy and measures to increase mucus clearance can help. Physiotherapy exercises can be taught at the hospital by a trained physiotherapist. These can be done at home quite easily and help when your baby has a cold. We would recommend that your child also have the Influenza Vaccine every year to prevent serious pneumonia.
In time most respiratory symptoms improve. It is important though that your child be regularly reviewed throughout childhood so that any ongoing problems can be identified and managed so that your child’s wellbeing is maintained.
Tracheoesophageal fistula causes
Tracheoesophageal fistula or esophageal atresia is a congenital condition, which means it develops before birth. The cause of esophageal atresia or tracheoesophageal fistula is not known. Research suggests a genetic component because around half of the babies born with esophageal atresia or tracheoesophageal fistula also have other birth defects. Scientists do know that one of the contributing factors may be hereditary but this is not certain. It is highly unlikely to happen in following pregnancies or in your grandchildren. An important point to keep in mind is that you have not done anything wrong. The good news is that the majority of OA/TOF children grow up to be normal, active young people if they are born with no other major problems.
What scientists do know is that the usual development does not occur at the normal time, very early in the pregnancy – sometime during the first three to six weeks. Boys and girls are equally affected. It is believed that it is caused by a number of factors acting together, but just what they are scientists have yet to learn.
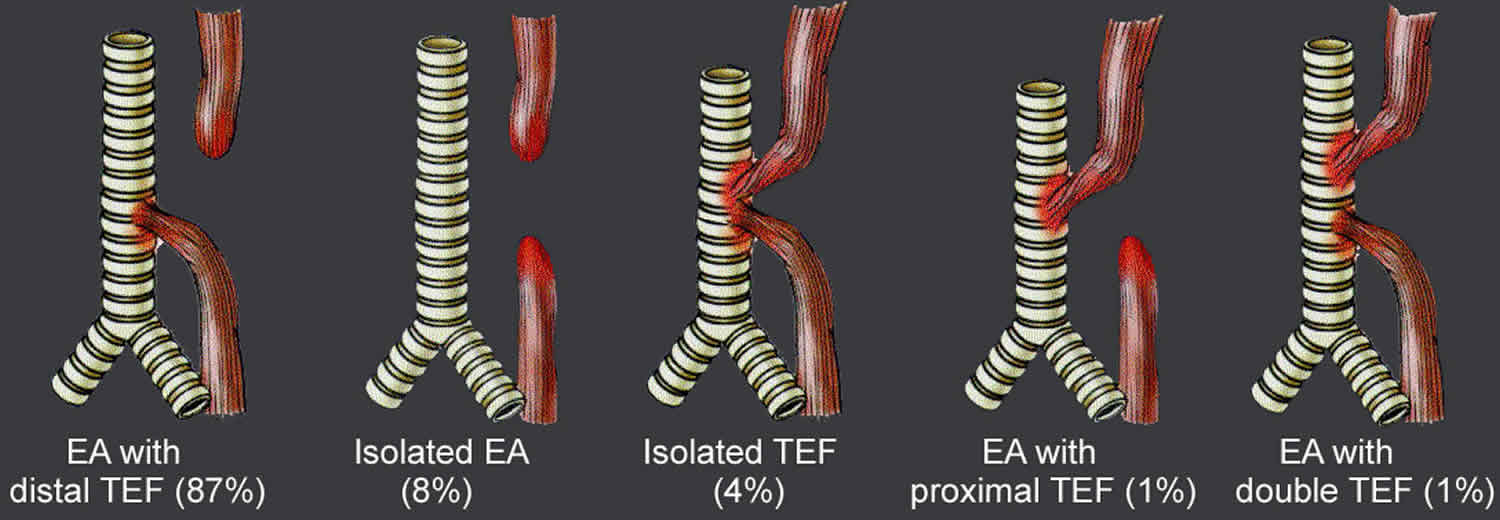
Congenital tracheoesophageal fistulas result from failure of the esophageal lumen to develop completely separate from the trachea. Embryonically, the trachea and upper gastrointestinal tract have a common origin at the caudal end (rear end) of the embryonic pharynx. In normal development during the second month of gestation, the esophagus assumes a back position, while the trachea lies at the front. Failure of this complete separation leads to the development of tracheoesophageal fistulas. Below images (Figures 1 to 3) depicting the different type of congenital tracheoesophageal fistulas and their frequency of occurrence.
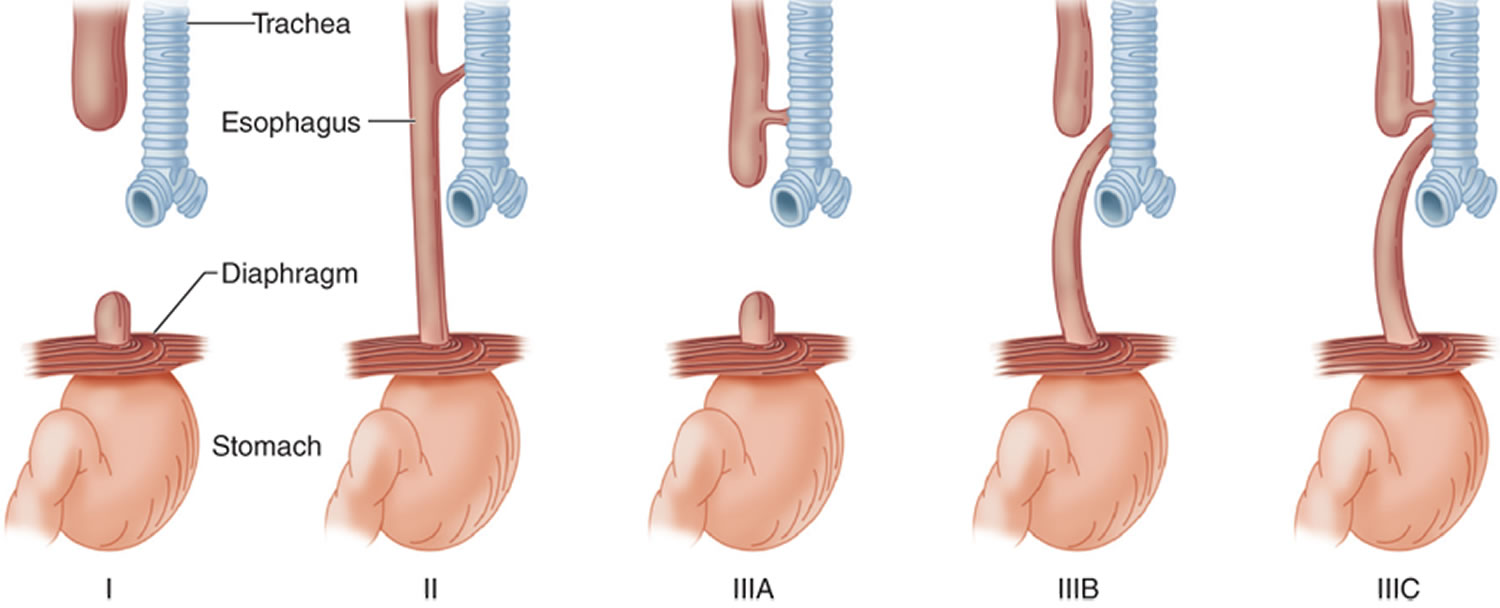
Tracheoesophageal fistula types
Most babies with esophageal atresia will also be born with an abnormal connection or “fistula” between the food pipe (oesophagus) and the windpipe (trachea) [tracheoesophageal fistula] (see Figures 2 and 3). This causes air to pass from the windpipe to the stomach and stomach juices to reflux from the stomach to the lungs both which cause breathing difficulties and dusky episodes soon after birth.
There are 5 types of esophageal atresia or tracheoesophageal fistula. Most babies born with tracheoesophageal fistula are of the common type, often referred to as Type C. This is where there is a connection between the distal part of the esophagus and the trachea. Check with your baby’s doctor which type of tracheoesophageal fistula your baby has.
Figure 2. Tracheoesophageal fistula types
[Source 1 ]Esophageal atresia with tracheoesophageal fistula
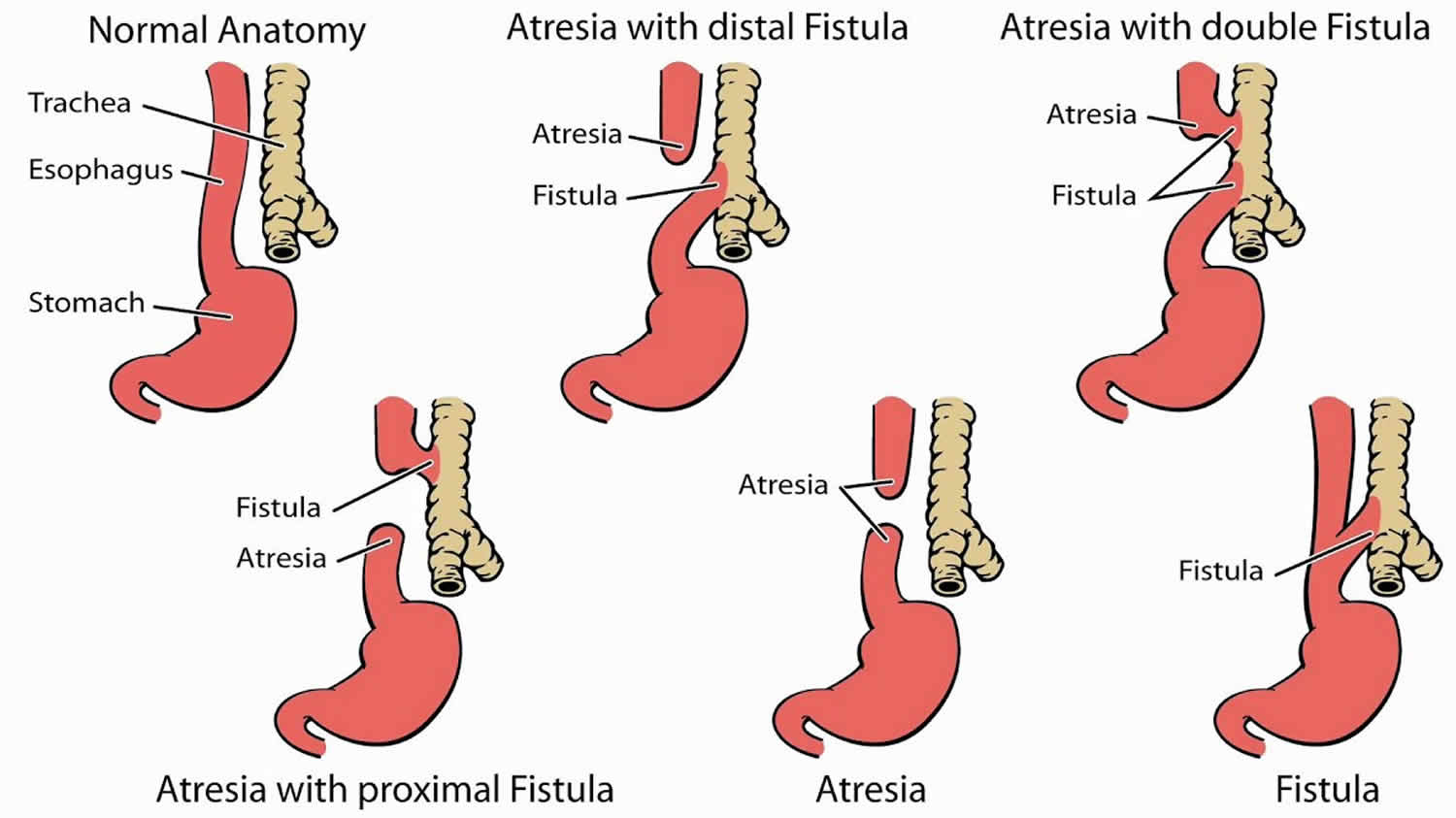
An esophageal atresia occurs when the esophagus is formed in two segments, and the baby is born with their esophagus not attached to their stomach. The upper part connects the mouth/throat to a blind pouch (proximal end), and the lower part connects the stomach to a blind pouch (distal end). While esophageal atresia can appear alone, most forms of esophageal atresia also include tracheoesophageal fistula.
In infants with esophageal atresia, the two ends of the esophagus do not meet. Food and saliva cannot get from the mouth to the stomach. Esophageal atresia is a common cause of polyhydramnios in utero. At birth, the infant may have difficulty handling secretions and may have respiratory distress at first feeding. Attempts to pass a nasogastric tube are usually unsuccessful.
Babies with esophageal atresia cannot swallow breastmilk, bottled milk or even their own saliva, and food cannot get to the stomach to be digested.
Esophageal atresia and tracheoesophageal fistula are often association with other anomalies. The most common congenital abnormality is the VACTERL association (vertebral defects, imperforate anus, cardiac defects, tracheoesophageal fistula, radial aplasia, limb anomalies). A thorough evaluation for these additional defects, especially cardiac, should be undertaken in these infants. The severity of illness can be mild (e.g., feeding difficulties in a full-term neonate with no respiratory distress), but some patients are critically ill. Severe respiratory failure can result from continuous aspiration of gastric contents via the distal tracheoesophageal fistula, exacerbated by respiratory distress syndrome as well as massive abdominal distention from filling of the stomach with gas from the tracheoesophageal fistula.
Figure 3. Esophageal atresia with tracheoesophageal fistula
Abbreviations: EA = esophageal atresia; TEF = tracheoesophageal fistula
Tracheoesophageal fistula symptoms
Tracheoesophageal fistula in newborns is slightly different, in that babies with tracheoesophageal fistula can swallow breast or bottle milk. However, the liquid often leaks through the fistula between the esophagus and trachea and travels to the lungs. This can cause infections or pneumonia.
Babies with a tracheoesophageal fistula — but not esophageal atresia — may take several weeks to diagnose because tracheoesophageal fistula symptoms generally only appear as mild coughing or respiratory problems.
Other tracheoesophageal fistula symptoms and/or esophageal atresia symptoms can include:
- Frothy, white bubbles from the mouth
- Vomiting
- Very round, full belly (from gas being trapped there)
- Bluish color to the skin, especially when the baby is feeding
- Nurses unable to pass a tube from your baby’s mouth into their stomach
For babies born with both esophageal atresia and tracheoesophageal fistula, symptoms are obvious almost immediately after birth.
The most common esophageal atresia and tracheoesophageal fistula symptoms include:
- Difficulty breathing
- Coughing or choking when swallowing or attempting to feed
Signs of esophageal atresia and tracheoesophageal fistula are:
- Large amounts of saliva.
- Trouble swallowing saliva .
- Choking or coughing when being fed.
How is tracheoesophageal fistula and esophageal atresia diagnosis made?
Tracheoesophageal fistula and esophageal atresia diagnosis can sometimes be made by ultrasound during pregnancy. The ultrasound might show that the baby has an abnormally small stomach. Or it might show that there is an excessive amount of amniotic fluid in the womb. Both are potential tracheoesophageal fistula/esophageal atresia symptoms. If these signs are present, a more detailed ultrasound may be done to see if the condition can be confirmed. Usually, however, a diagnosis cannot be made with certainty until after the baby is born.
Most babies with esophageal atresia and tracheoesophageal fistula are diagnosed shortly after birth when symptoms first appear. In these cases, clinicians perform a physical examination of the baby, get a medical history, then perform tests to determine how your child’s trachea and esophagus are affected.
Tests may include:
- Rigid bronchoscopy: A surgeon uses a telescope and camera to peer into the baby’s windpipe (trachea). This is the test most often used to establish the presence and type of tracheoesophageal fistula.
- X-rays, with a nasogastric tube: A clinician will insert an nasogastric tube into your baby’s nose, down the esophagus and try to get it to the stomach. If the nasogastric tube hits a blocked end of the esophagus — which happens if your child has esophageal atresia – doctors can see the blockage and where it is using an X-ray. X-rays can also show if there is gas in your baby’s stomach, a sign of tracheoesophageal fistula caused by air traveling through the abnormal opening (fistula) between the esophagus and the trachea.
- Barium swallow test: If clinicians suspect your baby has a tracheoesophageal fistula without esophageal atresia, they may have your baby swallow a chalky liquid called barium, then X-ray your child’s digestive tract to detect any abnormalities. This test is rarely used.
As prenatal imaging has improved, some babies with esophageal atresia or tracheoesophageal fistula are now being diagnosed before birth with high-resolution fetal ultrasound.
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of the baby within the womb. We will use ultrasonography to follow the development of your baby’s internal organs throughout your pregnancy so that an accurate diagnosis of tracheoesophageal fistula and esophageal atresia can be made as soon as possible. It will also help us identify other VACTERL birth defects that might be present.
What is fetal echocardiogram?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non- invasive, high-resolution ultrasound procedure looks specifically at how the baby’s heart is structured and functioning while in the womb. This test is important because babies with tracheoesophageal fistula or esophageal atresia sometimes have a heart-related birth defect as well.
What is fetal MRI?
Fetal MRI is another non-invasive test. It uses a large magnet, pulses of radio waves and a computer to create detailed images of your baby’s organs and other structures while in the womb. This procedure involves both mom and baby being scanned while partially inside our MRI machine. The test is a bit loud, but it takes only a few minutes and is not uncomfortable.
Tracheoesophageal fistula treatment
If your baby has tracheoesophageal fistula and/or esophageal atresia, they will need surgery. The type of surgery will depend on the internal structure of your child’s trachea and esophagus, how the anomaly is affecting your child’s breathing or feeding, and the overall health of your baby. In some cases, multiple procedures may be needed.
The surgery may not be done right away. The surgeons will need to evaluate the best way to correct the problem. Some babies need to grow before surgery.
Before surgery, your baby will be cared for in the neonatal intensive care unit (NICU) or infant care center. Sometimes a ventilator (breathing machine) may be used to help your baby breathe and a suction tube may be needed in the esophagus to keep secretions from going down the trachea.
Your baby will have an intravenous (IV) line to provide fluids and nutrition. IV antibiotics may be needed to prevent infection. Some babies need a gastrostomy tube (tube into the stomach) for feedings.
Tests for a possible VACTERL association will be done at your baby’s bedside. Blood will also be drawn to determine type, electrolyte levels, and any signs of infection. If an infection is found, your baby may be given antibiotics.
Until your baby has the operation to repair the tracheoesophageal fistula and/or esophageal atresia, a tube called a “replogle tube” is passed through the nose into the food pipe (esophagus). This will drain off any saliva which is in the esophagus, so that your baby does not choke. Your child will be nursed in the intensive care unit during this period, depending on their general condition.
For most tracheoesophageal fistula babies it is possible to repair the food pipe immediately with surgery. During the operation the connection between the windpipe and the food pipe (fistula) is closed off (ligated) and the two ends of the food pipe (esophagus) are joined together. The join is called anastomosis.
There are two ways of carrying out the operation: using thoracoscopic (keyhole) or open (thoracotomy) surgery. The surgeon will discuss the most appropriate method with you. The method used to repair the esophageal atresia depends on the distance between the ends of the esophagus. In most cases, the surgeons will be able to join the two ends of the esophagus together to form a continuous passage from the mouth to the stomach.
In rare cases (around 5%) called “Long Gap esophageal atresia” where the distance between the two ends of the esophagus is too large for the surgeon to be able to join them straightaway, a different treatment is needed. One of the ways in which “Long Gap esophageal atresia” is repaired is by a technique called the “Foker Technique”. The principle behind this technique is the fact that in a fetus inside the uterus, the normal esophagus develops because of the tension placed on it by the growing tissues of the baby. This tension has to be created for children with esophageal atresia to help lengthen the esophagus. After birth, traction sutures are attached to the tiny esophageal ends and the tension on these sutures is increased, bit by bit. These traction sutures stimulate the upper and lower ends of the esophagus to grow. At least two operations are needed in the “Foker Technique”. The first operation attaches traction sutures to both ends of the esophagus. This tension is then increased on the sutures over the following days or weeks (depending on length of the gap), by your surgeon. Another operation then removes the sutures and joins the oesophageal ends together. In some cases while waiting for the two ends of the esophagus to approximate, a special feeding tube or button (gastrostomy tube) is placed in the stomach of your child so milk can be given directly into the stomach. A small operation is needed when the gastrostomy tube is first put in place.
Another way to repair a “Long Gap esophageal atresia” involves nursing your baby in hospital until the esophagus (food pipe) grows enough to make it possible to be joined together. During this time a replogle tube is used. Also a special feeding tube (gastrostomy tube) is placed in the stomach so milk can be given directly into the stomach. A small operation is needed when the gastrostomy tube is first put in place.
For some children with “Long Gap esophageal atresia”, the upper part of the food pipe (esophagus) is brought out into an opening at the side of the neck. This is called an “esophagostomy”. This opening is left for 1-2 years before another operation is done to join the food pipe together. The opening in the neck allows saliva to drain out onto a small pad so your baby does not choke. It is important to feed your baby with milk into the mouth so that they remember how to suck when the feeding tube is repaired/joined. This is called “sham” feeding. The milk will flow out the opening in the neck so your baby does not choke. A special feeding gastrostomy tube or button is also placed in the stomach so milk can be given directly into the stomach.
Once you are confident with the special care your baby needs, you can be discharged to go home until the next operation.
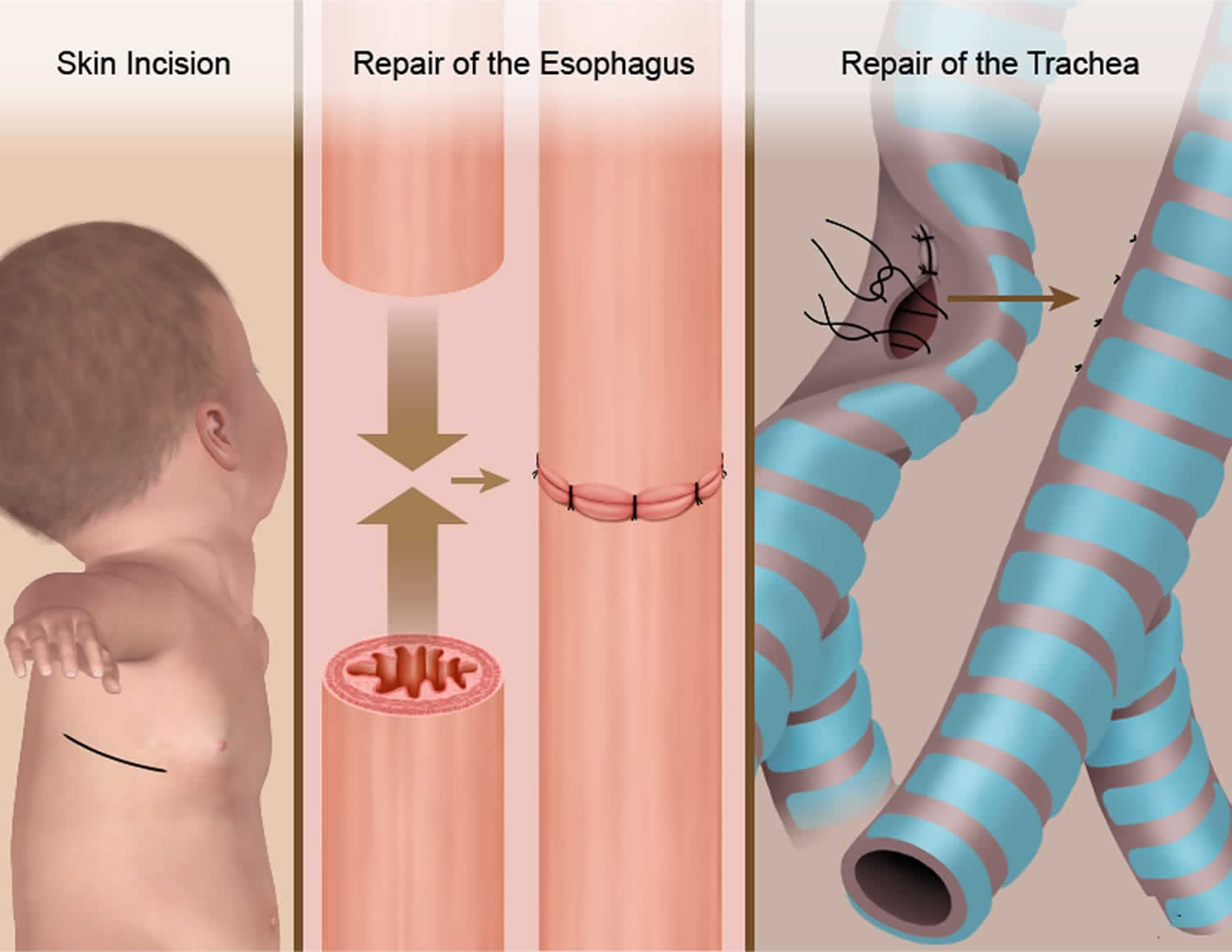
Figure 4. Esophageal atresia and tracheoesophageal fistula repair
What to expect during surgery for esophageal atresia or tracheoesophageal fistula
To prepare for esophageal atresia or tracheoesophageal fistula surgery, your baby will be given a breathing tube — if they don’t already have one — to help maintain their airway during surgery. A doctor will then administer an anesthetic to your baby for the operation.
Surgery for esophageal atresia and tracheoesophageal fistula is performed through an opening on the side of your baby’s chest. Depending on the type of surgery your child needs, this will either be one long opening or several small openings.
The first step in esophageal atresia repair — whether your baby has esophageal atresia or tracheoesophageal fistula or esophageal atresia alone — is a bronchoscopy. In a bronchoscopy, a small camera is inserted into the windpipe to look for fistulas that are small, hidden, or not obvious from prior tests.
If your child has tracheoesophageal fistula and esophageal atresia, the surgeon may decide to place a gastrostomy tube that can be used to feed your child and “burb” the stomach of excess air. For children with esophageal atresia alone, a gastrostomy tube will definitely be placed because it will be the only way your child can get food and nutrients into their stomach.
For babies with tracheoesophageal fistula and esophageal atresia, the next part of surgery is to divide the esophagus from the windpipe at the abnormal connection (fistula) and close the hole left in the windpipe. If the two ends of the esophagus are long enough, the surgeon will stitch the two ends of the esophagus together to create a functioning esophagus between the back of the throat and the stomach.
If the two ends of the esophagus aren’t long enough to be connected, we will wait a few weeks to allow your baby to grow before attempting to connect them again in a second surgery. In the meantime, your baby can be fed through the gastrostomy tube that was placed.
For babies with esophageal atresia — and not tracheoesophageal fistula — surgery includes connecting the two ends of the esophagus to form a functioning channel between the back of the throat and the stomach. If the ends of the esophagus are not long enough to be connected at this time, we will wait until your baby grows and try again in a few weeks. While waiting for esophageal atresia surgery, your baby can be fed through a gastrostomy tube.
If the two ends of the esophagus are successfully sewn together, a chest tube may be placed during surgery to drain saliva that may leak from the new connection.
What can I expect after surgery?
After surgery for esophageal atresia or tracheoesophageal fistula, your baby will return to the NICU. Depending on your child’s condition and which procedures were performed, your baby may have an IV for pain medications, a gastrostomy tube to carry food to the stomach, and a chest tube to drain fluid away from their reconnected esophagus. Your baby may also need a ventilator to help them breathe for a short time after surgery. Once your child can breathe on their own, the ventilator will be removed.
After surgery, many babies are on the ventilator and get their fluids, pain medicine, and nutrition by IV. Most babies will have a chest tube (a tube inserted through the skin into the baby’s chest wall) to help keep the lungs open and free of fluids that might collect after surgery.
Your doctors and nurses will watch for these complications:
- Trouble breathing.
- Infection.
- Problems with the chest tube.
- Leaking or narrowing where the trachea or esophagus are sewn.
- Unstable temperature.
Your baby will stay in the NICU until stable.
Nurses will suction your baby’s mouth frequently until they get used to swallowing their own saliva. Additionally, clinicians may gently tap on your baby’s chest to keep their lungs expanded and clear.
The chest tube (drain) will stay in place until approximately a week after surgery when special X-rays are done and show there isn’t a leak where the two ends of the esophagus were sewn together (anastomosis). If a leak is found, the drain will stay in place until the leak stops.
Your baby may not be able to eat for the first week after surgery. Most babies begin to receive nutrients through the gastrostomy tube initially as they practice eating smaller volume feedings by mouth. It can take a while for babies with esophageal atresia or tracheoesophageal fistula to work up to eating everything by mouth.
Surgery risks
All surgery carries a small risk of bleeding during or after the operation. Even if the gap between the ends of the esophagus is quite small, it can still be difficult to join together. After the operation, the join may leak or it may narrow over time, but these can both be treated. Your child will be reviewed regularly for a long time after the operation.
Every anesthetic carries a risk of complications, but this is very small. Your child’s anesthetist is a very experienced doctor who is trained to deal with any complications.
Anesthesia and risk in infants
Modern anesthesia and surgery is very safe for children and infants. With new technology and new drugs, the risks of cardiac arrest, allergic reactions, kidney and liver failure are now extremely low.
Recently, the chance that anesthesia (and other sedative drugs) may cause long term effects on brain development has been raised. In December 2016, the FDA (Food and Drug Administration, USA) made an announcement that the development of a child’s brain may be affected by repeated or lengthy use of anesthetics. This announcement has been carefully considered by your surgeon and anesthetist before planning your child’s surgery.
Several large studies have looked at anesthesia in early life and its effect on brain development. These studies have measured learning disabilities, school results, intelligence quotients (IQ), autism and individual behaviors in children who have had anesthesia in infancy. The majority of these studies have shown that single, short anesthetics in infancy, do not lead to reduced scores in currently available developmental measures.
Remember:
- Your surgeon is recommending surgery and anesthesia for your child for a good reason.
- There are risks associated with the use of anesthesia, however your surgeon will explain the benefits for your child, which are based on clinical evidence.
- Overall the risk of reduced academic and developmental outcomes from anesthesia is small.
Are there any alternative forms of anesthesia/ sedation that may be safer?
There are no known alternatives to current general anesthetic drugs. No particular anesthetic drugs or techniques have been proven to be safer than those used in current practice.
My child may need several general anesthetics when still very young (under 3 years). Could these have long term effects?
Having multiple procedures that need anesthesia early in life, is associated with a small increase in risk of a learning disability and/or a developmental and behavioral disorder, in later life.
It is not possible to work out whether the small increase in risk is related to the anesthesia drugs or the effect of the underlying illness that made surgery necessary. It is possible that the illness, the surgery itself or repeated hospitalizations and absence from school may be more important factors than the anesthesia drugs. It is also possible that children who need repeated surgery may already be at risk of poorer developmental outcomes.
Please note that the risk of a reduced academic or developmental score is generally low and the size of any reduction is small. These reductions, if any, may be related to the surgery, anesthesia drugs or the underlying illness.
Your surgeon will discuss the factors that must be taken into account when deciding the timing of surgery. These decisions always involve a balance of risks.
My child is likely to need repeated general anesthetics. What should I be doing?
There is no good reason to treat your child any differently. All children develop best when nurtured in a safe, secure and loving environment. Give your child good nutrition, clean air, regular exercise and sleep to keep them safe and healthy. Brain development is likely to be improved when children are provided with an enriched learning environment in early life. If you have concerns about your child’s development, ask to see your pediatrician.
Surgery complications
Complications are possible for babies after treatment for esophageal atresia and tracheoesophageal fistula.
The most common complications include:
- A leak of saliva where the two ends of the esophagus were connected. If a leak occurs, it will generally heal in a week or two. Additional surgery is not usually necessary.
- Difficulty eating by mouth. Because babies haven’t eaten by mouth since birth, it often takes time and practice to learn this skill. Speech therapy can help your child build these skills
- Gastroesophageal reflux (GER) is very common after esophageal atresia or tracheoesophageal fistula surgery. It is treated with medications (or, rarely, with an operation called fundoplication) prescribed by the surgical/medical team.
- The newly connected esophagus may not function perfectly at first. The passage of liquid and food may be delayed compared to a baby who was born with normal anatomy. As your baby grows and starts to eat table food, your doctors will tell you which foods your baby may have difficulty swallowing.
- Scar tissue at the surgical site may cause the esophagus to narrow, making it more difficult for your baby to swallow food. This is treated by a procedure to widen or dilate the esophagus.
- Tracheomalacia, a softening of the cartilage of the windpipe, can occur where the fistula was repaired during surgery. This causes a partial collapse of the windpipe with increased airflow. Because of this, your baby’s cry or cough may sound like a “barking” sound similar to a seal or a sea lion.
Follow-up care for esophageal atresia/tracheoesophageal fistula
When your baby can return home after surgery depends on many things, including:
- Whether your baby was premature
- If your baby’s esophagus could be connected right away
- Your baby’s respiratory status
- Whether other medical problems were identified in your baby
If your baby was premature, they will likely need to remain in the Hospital for several weeks to months after surgery. If your baby was close to full term, the esophagus could be connected right away and there wasn’t a leak, your baby may only need to be hospitalized for a few weeks.
Before your child is discharged from the hospital, you will be taught how to:
- Feed your baby if they have a feeding tube
- Give your baby medications, if needed
- Mix formula or breast milk if your baby needs increased calories
- Take care of your baby’s incision and dressing, if applicable
You’ll also be taught to spot signs of possible infection or narrowing of the esophagus, and when to call the pediatrician or surgeon with concerns or problems.
A few weeks after your baby leaves the Hospital, they will need to return for a follow-up visit. Your child’s surgeon will ensure the incision is healing, and your baby is recovering and growing as expected. Support staff will help your family coordinate additional services, such as home nursing visits, early intervention services, speech therapy, physical therapy and occupational therapy, as needed.
Esophageal atresia and tracheoesophageal fistula prognosis
Long-term outcomes for children with esophageal atresia and tracheoesophageal fistula are generally good. While most children can eat normally, some may need to chew their food more, eat slower or take smaller bites to help ease food down the esophagus. About half of all children who had esophageal atresia will have life-long problems with gastroesophageal reflux. In most cases, gastroesophageal reflux can be treated with medication.
Most babies born with esophageal atresia or tracheoesophageal fistula thrive. Their outcome depends mostly on associated conditions more than on the problems with the esophagus itself.
References