Trigeminal trophic syndrome
Trigeminal trophic syndrome a rare cause of facial ulceration and cutaneous dysesthesia (unpleasant and abnormal sensation in the skin) that most often presents with ulceration of the ala nasi (nares or wing of tissue at the end of the nose above the nostril) caused by damage to the trigeminal nerve or its central sensory connections 1. It results in sores affecting the skin supplied by the sensory component of the trigeminal nerve. Trigeminal trophic syndrome is characterized by the triad of dysesthesias, anesthesia, and ulceration. Trigeminal trophic syndrome most often arises in women and the elderly and occurs at an average age of 57 2.
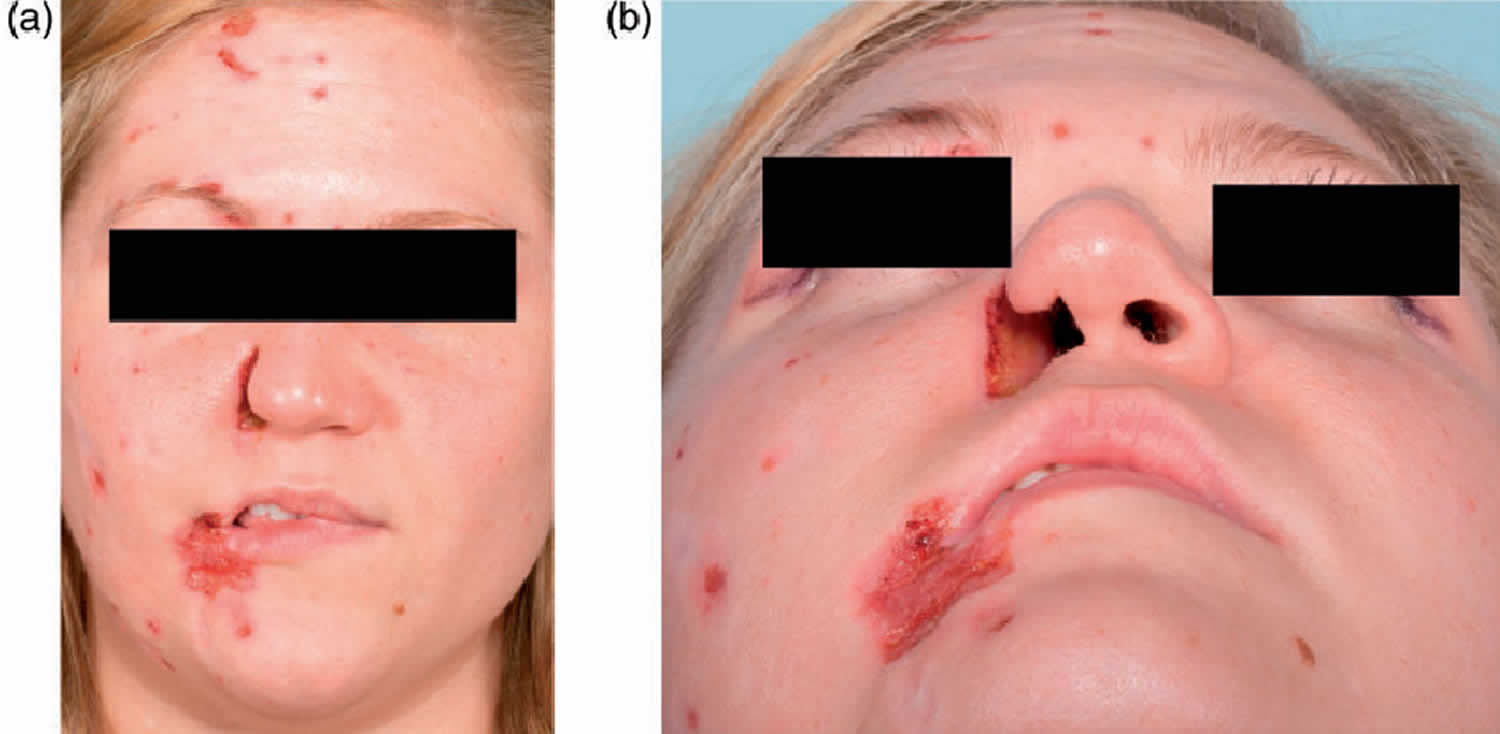
The first sign is a small crust that leads to a crescent-shaped ulcer on the side of the nose. The characteristic shape helps in distinguishing it from other possible causes. The ulcer may extend to the cheek and lips. Healing leads to fibrosis (scarring), and the lip may be drawn up into a characteristic sneer.
Similar lesions may also occur in the corners of the eyes, scalp or inside the mouth. The tip of the nose is characteristically spared because it derives sensation from a different nerve, the medial branch of the anterior ethmoidal nerve.
Patients complain of picking, rubbing, or scratching sensations in the affected areas; these sensations are attributed to hyperesthesia (an abnormal increase in sensitivity to stimuli), paraesthesia (abnormal sensation, typically tingling or pricking also called ‘pins and needles’), or pain following damage of the sensory trigeminal fibers or nuclei.
Trigeminal trophic syndrome differs from dermatitis artefacta or compulsive skin picking as there is an identifiable neurological abnormality. The patient is aware of the problem and readily admits to manipulation of the area. Even so, it can be commoner in individuals with psychological disorders.
The diagnosis of trigeminal trophic syndrome should be suspected when there is unilateral facial ulceration, especially involving the ala nasi associated with sensory impairment.
The management of trigeminal trophic syndrome is often difficult 3. Application of occlusive dressings can reduce trauma of the affected area. Hydrocolloid dressings help the ulcers heal. Transcutaneous electrical nerve stimulation was reported to be of use in some cases. Treatment regimens involving amitriptyline and diazepam in addition to chlorpromazine and pimozide have met with some success. Carbamazepine is an effective therapy in trigeminal neuralgia and atypical facial pain because these agents may influence both the paresthesias and behavioral factors in trigeminal trophic syndrome 1.
Figure 1. Trigeminal trophic syndrome
[Source 4 ]Figure 2. Trigeminal trophic syndrome scalp (zoster-associated trigeminal trophic syndrome)
Footnote: Development of zoster-associated trigeminal trophic syndrome. A 21-year-old woman was irradiated after resection of a pituitary adenoma. A few weeks later, she developed right ophthalmic-distribution zoster and right abducens palsy. Zoster rash resolved, but persistent dysesthesias led to constant rubbing and scratching, ultimately leading to ulceration. Skin biopsy was negative for malignancy and chronic infection. Despite antibiotic, antiviral, triamcinolone, and hyperbaric oxygen treatment, the ulceration expanded.
[Source 5 ]Trigeminal trophic syndrome causes
Any lesion in the central or peripheral nervous system which impairs the function of the trigeminal nerve can lead to the trigeminal trophic syndrome. Trigeminal trophic syndrome commonest causes are injuries or neurosurgical procedures such as trigeminal rhizotomy or injection of alcohol to the Gasserian ganglion in 70 percent of cases.
The average period from the time of trigeminal nerve injury to the onset of the ulcer varies from several weeks to many years, with an average of 2 years 6.
Other associations include Wallenberg syndrome (6 %), and following a cerebral vascular accident (7 %). Exceptionally, Trigeminal trophic syndrome also occurs following encephalitis, resection of acoustic neuroma, pontine infarction, meningioma, syringobulbia, craniotomy, amyloid deposits in the brain, during syphilis, herpes zoster, herpes simplex, and neurological complications from birth trauma or it can be idiopathic 7.
Trigeminal trophic syndrome differential diagnosis
Other causes of facial ulceration include infections, autoimmune disorders and malignancies (cancer) 8.
Infections that need exclusion may include:
- Viruses: herpes zoster, herpes simplex
- Molds and fungi: sporotrichosis, zygomycosis
- Bacteria: neuralgic leprosy, cutaneous tuberculosis, syphilis, yaws, anthrax
- Parasites: leishmaniasis
Autoimmune disorders causing facial ulceration include:
- Cutaneous lupus erythematosus
- Granulomatosis with polyangiitis
- Sarcoidosis
- Cutaneous vasculitis
The most common skin cancers causing ulceration are:
- Basal cell carcinoma
- Squamous cell carcinoma
Trigeminal trophic syndrome signs and symptoms
Signs of trigeminal trophic syndrome begin weeks to decades after the injury to the trigeminal nerve – generally around a year later (average of 2 years) 6.
The damaged area feels numb (anesthesia) or tingly-prickly (paresthesia). This provokes rubbing, scratching, picking and eventually ulceration.
Some people with trigeminal trophic syndrome complain of a blocked nose or a foreign body in a nostril purely because of the loss of sensation which impairs the ability to perceive air flowing through the nostril.
There may be a delay in recognizing the association of a unilateral ulcer on the trigeminal area (first and second branch of trigeminal nerve), with the underlying nerve damage. These chronic ulcerating lesions can typically be observed in the nasal ala and paranasal areas but may be seen to involve any of the ophthalmic (V1) maxillary (V2) or mandibular (V3) nerve distributions 9. Often, the ala nasi is involved with a characteristic painless, sickle-shaped lesion. The margins are free, and the ulcer base has scant crust. Other areas may be involved with these ulcers, including the frontal scalp (resulting in triangular frontoparietal alopecia), ear, cheek, temple, and cornea 10. Once the ulcers appear, they are extremely persistent. Rare cases of self-healing in the trigeminal dermatome are reported 11.
Trigeminal trophic syndrome diagnosis
The diagnosis is clinical and is suggested when loss of sensation occurs in association with unilateral facial ulceration, especially involving the ala nasi. Neurological examination revealed decreased sensation of pain and thermal perception over the trigeminal area 10. This sign is very important for making the diagnosis.
Laboratory tests are often necessary to differentiate other causes of facial ulceration such as infections, autoimmune disorders and malignancies (cancer). There are no distinguishing blood tests or characteristic skin biopsy features in trigeminal trophic syndrome.
X-rays and other imaging studies may be performed to attempt to locate the site of trigeminal injury, but they may prove unhelpful. Neurophysiological studies can be helpful in evaluating function of the trigeminal nerve.
Trigeminal trophic syndrome treatment
The treatment options for the trigeminal trophic syndrome are varied. Unfortunately, they are often ineffective.
Often a multi-disciplinary team (dermatologists, neurologists, psychiatrist and occasionally surgeons) is required to successfully treat trigeminal trophic syndrome.
Patient education about the cause of the ulceration is of paramount importance may help patients reverse destructive scratching habits 12. Covering the area to prevent self-manipulation until the wound heals may be useful.
If chronic herpes simplex virus is responsible, symptoms may respond to antiviral therapy, such as longterm oral aciclovir.
Medications such as olanzapine, gabapentin, carbamazepine, amitriptyline, chlorpromazine have been used to reduce paraesthesia with questionable benefit 13.
Transcutaneous electrical stimulation, stellate ganglionectomy and ionising radiation (radiotherapy) have also been used as a treatment in resistant cases.
Surgical grafts or a rotation flap taking tissue from the innervated unaffected side to cover the ulcer has proved successful in a few cases.
Treatment remains challenging and a number of therapies, including electrical stimulation, negative pressure therapy and autologous epidermal cell transplant have been investigated with varying degrees of success 14.
References- Bhushan M, Parry EJ, Telfer NR. Trigeminal trophic syndrome: successful treatment with carbamazepine. Br J Dermatol. 1999 Oct;141(4):758-9. doi: 10.1046/j.1365-2133.1999.03133.x
- Weintraub E, Soltani K, Hekmatpanah J, Lorincz AL. Trigeminal trophic syndrome. A case and review. J Am Acad Dermatol. 1982 Jan;6(1):52-7. doi: 10.1016/s0190-9622(82)80200-4
- Kumar P, Thomas J. Trigeminal trophic syndrome. Indian J Dermatol 2014;59:75-6
- Golden E, Robertson CE, Moossy JJ, Sandroni P, Garza I. Trigeminal trophic syndrome: A rare cause of chronic facial pain and skin ulcers. Cephalalgia. 2015 Jun;35(7):636. doi: 10.1177/0333102414547140. Epub 2014 Aug 21.
- The trigeminal trophic syndrome. Maria A. Nagel, Don Gilden. Neurology Oct 2011, 77 (15) 1499; DOI: 10.1212/WNL.0b013e318232ac46
- Miko K, Bauer K, Schopf RE. Neurotrophisches Ulkus als Spätfolge einer Trigeminusexhärese [Neurotrophic ulcer as late sequela of trigeminal nerve excision]. Hautarzt. 2001 Nov;52(11):1043-4. German. doi: 10.1007/s001050170041
- Mishra SN, Nayak CS, Deshpande DJ, Pereira RR. Trigeminal trophic syndrome: A rare entity. Indian J Dermatol Venereol Leprol 2011;77:729.
- Trigeminal trophic syndrome. https://dermnetnz.org/topics/trigeminal-trophic-syndrome
- Kurien AM, Damian DL, Moloney FJ. Trigeminal trophic syndrome treated with thermoplastic occlusion. Australas J Dermatol 2011; 52: e1–4.
- Chavingyn J-k, Hery B, Litoux P. Trigeminal neurotrophic ulcerations Nouv. Dermatol. 1997; 16 : 48-9.
- Ziccardi VB, Rosenthal MS, Ochs MW. Trigeminal trophic syndrome: a case of maxillofacial self-mutilation. J Oral Maxillofac Surg. 1996 Mar;54(3):347-50. doi: 10.1016/s0278-2391(96)90758-2
- Bewley A, Taylor RE, Reichenberg JS, Magrid M. Practical Psychodermatology. West Sussex, UK: Wiley Blackwall, 2014.
- Fruhauf J, Schaider H, Massone C, Kerl H, Mullegger RR. Carbamazepine as the only effective treatment in a 52-year-old man with trigeminal trophic syndrome. Mayo Clin Proc 2008; 83: 502–504.
- Atypical Trigeminal Trophic Syndrome: An Unusual Cause of Facial Ulceration. Acta Derm Venereol 2017; 97: 971–972. doi: 10.2340/00015555-2675