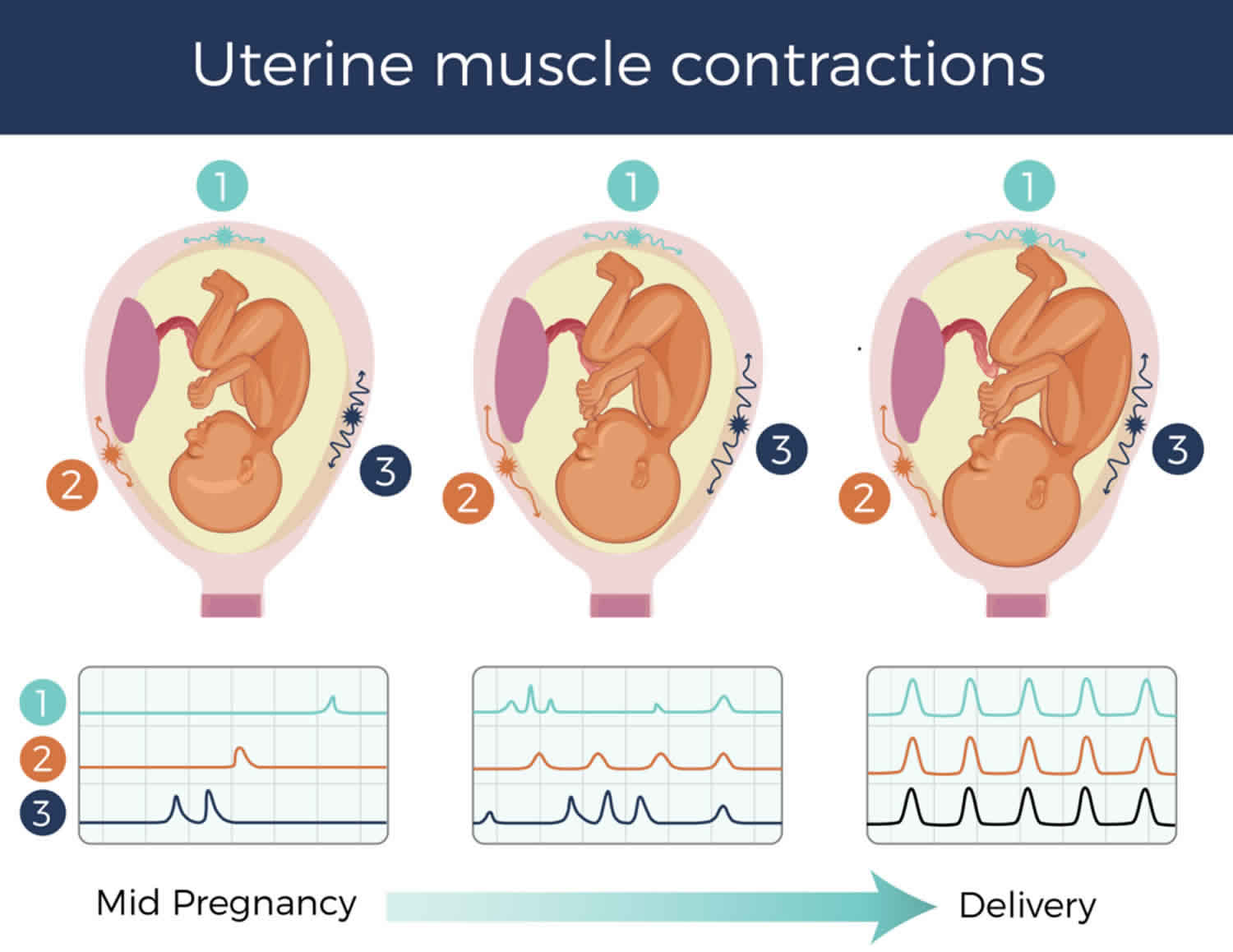
Uterine contractions
Uterine contractions are the tightening and shortening of the uterine muscles. During labor, uterine contractions accomplish two things: they cause the cervix to thin and dilate (open) and they help the baby to descend into the birth canal. Uterine contractions also occur during your monthly menstrual cycle and are recognized as menstrual cramps. The uterus is a hollow organ of the female reproductive system that three main layers: a well-differentiated lining layer (endometrium), a thick smooth muscle (myometrium) and an outer serosal layer 1. The myometrium (thick smooth muscle middle layer) is the main layer responsible for uterine contractions. Uterine contractions are very important for multiple reproductive functions, such as the menstrual cycle, the transport of sperms and embryo, pregnancy, and parturition 2. Uterine contractions play an important role in many and varied reproductive functions including sperm and embryo transport, implantation, menstruation, gestation and parturition 3. Abnormal uterine contractions can cause common pathological disorders of the female reproductive system, such as preterm labor, infertility, implantation failure, irregular menstrual cycle (dysmenorrhea), endometriosis, spontaneous miscarriage or preterm birth 4. Moreover, a coordinated activity of uterine muscle contractions is required for initiation and flow of a successful labor course 5. On the other hand, if uterine contractions is impaired, it significantly affects the progression of normal labor 1.
The uterus frequently contracts throughout the entire menstrual cycle, and these contractions have been termed endometrial waves or contractile waves 3. In the early follicular phase following menstruation, contractile waves occur once or twice per minute and last 10–15 seconds with low-amplitude (usually <30 mmHg) 3. As ovulation approaches, the frequency increases to 3–4 per minute. During the luteal phase, the frequency and amplitude decrease perhaps to facilitate implantation. In the absence of implantation of a blastocyst, the contraction frequency remains low but the amplitude increases dramatically (50–200 mmHg) producing labor-like contractions at the time of menstruation. The most fascinating aspect of endometrial waves is the integrated directionality of the uterine smooth muscle activity and the changes that occur through the reproductive cycle. These have been classified and are described in greater detail by others 6.
However, although the importance of abnormal uterine contractions is well acknowledged, there has been rather insufficient research focusing on the role of the uterine myometrium in common disorders of the female reproductive system 4. A better understanding of human myometrium physiology and contractility is essential to designing and testing interventions that can prevent or treat the important clinical problems noted above. More research is necessary to understand the mechanisms that generate the frequency, amplitude, duration and direction of propagation of uterine contractile activity 3. On the basis of current knowledge of the molecular control of uterine myocyte function, there are opportunities for systematic testing of the efficacy of a variety of available potential pharmacological agents and for the development of new agents. Taking advantage of these opportunities could result in an overall improvement in female reproductive health 3.
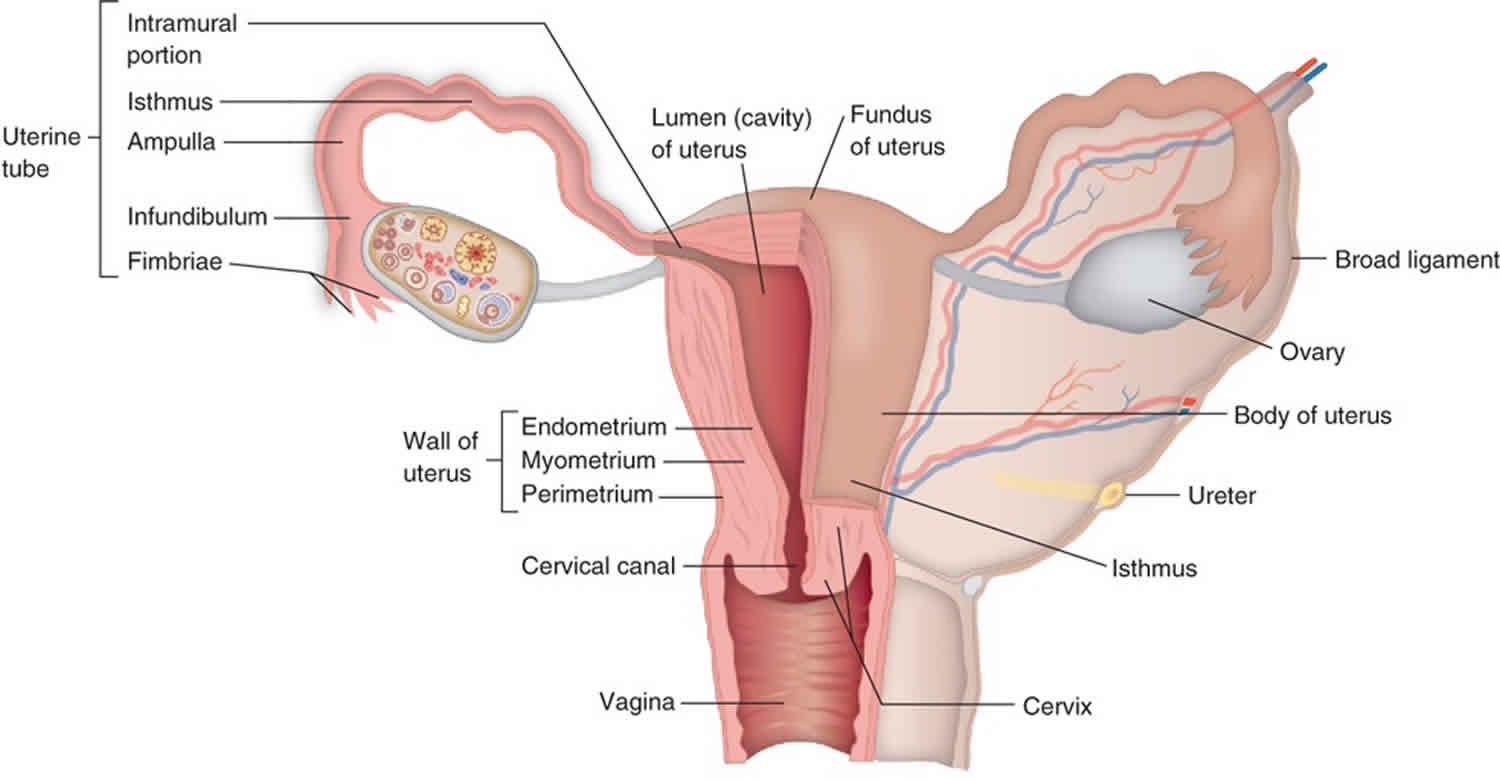
Figure 1. Uterus anatomy
Uterine contractions physiology
Uterine contractions occur throughout the menstrual cycle in the non-pregnant state and throughout pregnancy 3. There are four important parameters that change under various physiological or pathophysiological conditions: frequency, amplitude, duration and direction of propagation. Over the past two decades, considerable information regarding myometrial function in non-pregnant women has been obtained from the use of open-tipped pressure catheter recordings or from three-dimensional ultrasound or magnetic resonance imaging (MRI). Several reviews have described these changes and their potential clinical significance 7. Contractile activity in the non-pregnant uterus appears to be fundamentally different than in the pregnant organ. The contractions observed during the menstrual cycle have been termed ‘endometrial waves’ 8. Using a variety of imaging techniques, these contractions appear to involve only the sub-endometrial layer of the myometrium. These observations have led to a new concept of uterine anatomy that encompasses two distinct zones of the myometrium (see Figure 2 below).
In non-primate species, the myometrium consists of two distinct layers—an outer longitudinal layer and an inner circular layer. However, in the human, the myometrial substructure is not so well defined 9. The outer longitudinal layer is much less distinct and the major thickness of the myometrium is composed of intertwined muscle bundles that frequently surround abundant vascular channels. This histological arrangement may be of vital hemostatic importance following delivery of the hemochorial placenta that is characteristic of primates. Perhaps of particular interest to the physiology of the myometrium in the non-pregnant state, the inner (sub-endometrial) portion of the myometrium has been the focus of compelling research over the past three decades 10.
In 1983, Hricak 11 used MRI to demonstrate a distinct tissue layer occupying the inner one-third of the myometrium, which appeared as a low intensity signal area that blended into the endometrial stroma. During the reproductive years, this ‘junctional’ or ‘sub-endometrial’ layer appears anatomically distinct from the outer, denser myometrium but this distinctiveness is blurred in pre-pubertal and post-menopausal years. Noe et al. 12 have proposed and provided some evidence to support the view that this junctional layer is also embryologically and functionally distinct from the outer myometrium. They suggest that the inner, junctional myometrium, which is composed of short muscle bundles arranged in a predominantly circular pattern, is derived from the paramesonephric (Mullerian) ducts of the female embryo but the outer, more predominant myometrium originates from non-Mullerian tissue. The junctional myometrium is rich in estrogen and progesterone receptors that are regulated throughout the menstrual cycle 12. In contrast, there appears to be no such cyclic changes in sex steroid receptor expression in the thick outer layer of the myometrium, which contains predominantly long muscle fibers arranged longitudinally and is the major contractile tissue during parturition and abortion. More recent and sophisticated MRI studies using diffusion tensor imaging to provide a three-dimensional view confirmed the overall presence of anisotropy, indicating a lack of organization of fibers, but also provided more evidence to support the presence of a distinct inner, sub-endometrial circular layer of fibers throughout the uterine corpus and tubes 13.
The proposed junctional zone rationalizes the types of contractile activity observed in the video images from ultrasound or MRI studies. These waves have been described by most investigators as having peristalsis-like character. This is reminiscent of small intestinal peristaltic motility, which is mediated by the actions of distinct inner circular and outer longitudinal muscle layers, although the exact mechanism of coordination for these impulses remains unclear. Interestingly, regarding gastro-intestinal motility, the phenomenon of reverse peristalsis is well described 14. Thus, the presence of a functional inner circular layer of muscle fibers could represent a mechanism for this peristaltic and anti-peristaltic activity that is well-documented through the menstrual cycle. The circular arrangement of the muscle fibers may underlie the ability of the contractile activity to travel from fundus to cervix or in the opposite direction, depending on the local hormonal milieu and, undoubtedly, many other factors.
Regardless of the presence or absence of physiologically distinct myometrial zones, uterine contractions are dependent on the individual contractile activity of the cellular elements, the uterine myocytes. The remainder of this review will describe the molecular mechanisms that are likely to be involved in this activity. Most myometrial research has focused on changes that occur during pregnancy and in particular, those that might be related to the occurrence of preterm labor 15. In addition, much of what scientists know about uterine smooth muscle contractility has been derived from studies of vascular uterine smooth muscle, from either human or animal sources, or from other uterine smooth muscle tissues such as rodent ileum or frog stomach. Because of the paucity of information regarding the uterine tissues from non-pregnant women, it is impossible to present a picture of uterine physiology specific to the non-pregnant state. Scientists have attempted to identify studies that have focused specifically on human uterine myocytes, but they have not exhaustively named the species and uterine smooth muscle types for findings that are highly likely to be applicable to the human uterine myocyte.
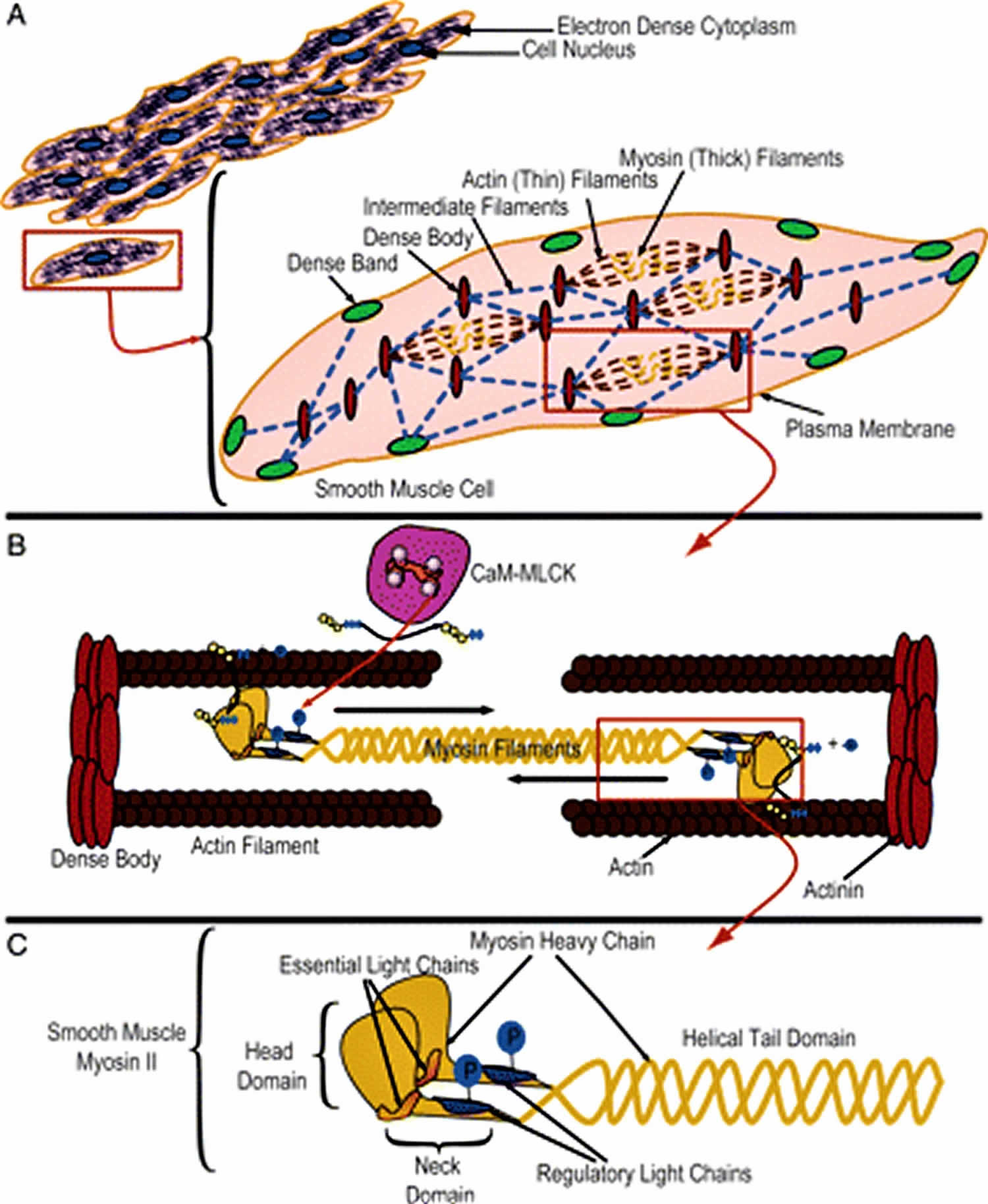
Uterine smooth muscle cells are relatively small and densely packed with myofilaments and associated dense bodies that occupy 80–90% of the cell volume and constitute the contractile machinery (see Figure 3A) 16. As in all muscle tissue, the predominant proteins expressed in uterine uterine smooth muscle are myosin and actin. In skeletal or striated muscle, there is ∼3-fold more myosin than actin. Conversely, uterine smooth muscle has more actin than myosin by a factor ranging from 2 to 10 17. In uterine uterine smooth muscle, there is ∼6-fold more actin than myosin 18.
The myofilaments are classified according to their diameter. Thin filaments (6–8 nm diameter) are polymers of globular monomeric actin. Thick filaments (15–18 nm diameter) are made up of myosin. In general, the actin and myosin filaments run in parallel and in the longitudinal dimension of the cell. In contrast, intermediate filaments (10 nm diameter) may be composed of a large number of proteins, although desmin and vimentin are the predominant constituents.
In addition to the constituents of the filamentous structures discussed above, other proteins accessory to the contractile machinery may play important roles in contractile regulation. These proteins are primarily associated with the thin filaments and include tropomyosin, calponin and caldesmon. Tropomyosin is an actin-associated protein that spans seven actin monomers and is laid out end to end over the entire length of the thin filaments. In striated muscle, tropomyosin serves to enhance actin–myosin interactions. However, it has an uncertain role in uterine smooth muscle. Calponin may be expressed at levels reaching stoichiometric equivalence with actin, and has been proposed to be a load-bearing protein. Caldesmon may be involved in tethering actin, myosin and tropomyosin, and in so doing may enhance the ability of uterine smooth muscle to maintain tension. In addition, caldesmon may be directly involved as a molecular switch for MII ATPase activity dependant on its phosphorylation state. All three of these proteins may have a role in inhibiting MII ATPase activity. For a more thorough discussion regarding these and other important regulatory proteins, the reader is referred to other reviews 19.
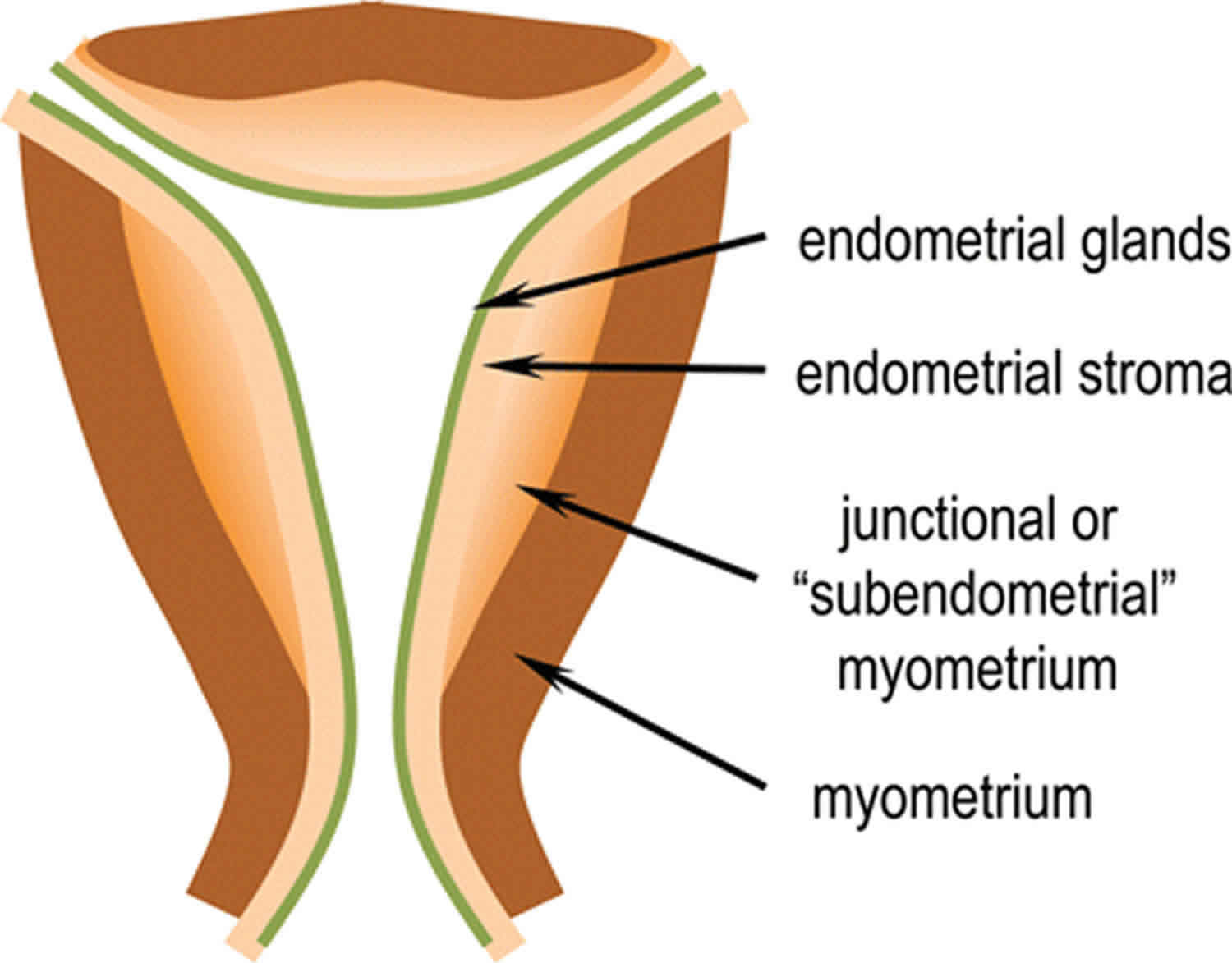
Figure 2. Uterine myometrium
Footnote: Concept of the sub-endometrial layer of myometrium. This thinner, innermost layer of muscle fibers, which are arranged predominantly in a circular configuration around the uterine cavity, is suggested to be of different embryological origin with physiological properties distinct from the more prominent outer layer. The circular sub-endometrial layer may facilitate the changing vectors of ‘endometrial waves’ that might play important roles in common reproductive disorders. The outer layer is likely to be more important in more intense uterine activity including abortion or parturition.
[Source 3 ]Figure 3. Uterine smooth muscle cells
Footnote: Smooth muscle (SM) contractile machinery. (A) The smooth muscle cell cytoplasm is densely packed with elements of the contractile machinery (thick and thin filaments), and other structural components (dense bodies, dense bands, intermediate filaments). The network formed by the combination of these elements results in force transduction along the longitudinal axis of the cell and cell shortening. (B) The contractile elements are composed of myosin thick filaments and actin thin filaments anchored to dense bodies. The movement of thin filaments caused by phosphorylation of myosin light chains and subsequent ATP hydrolysis by the myosin II ATPase decreases the distance between anchor points. (C) Myosin II is a hexamer composed of two heavy chains, two essential light chains and two regulatory light chains. Phosphorylation of the two regulatory light chains causes formation of a cross bridge between actin and myosin filaments and also creates a change in the angle of the neck region of myosin II, which causes motion of the actin thin filaments resulting in shortening of the cell.
[Source 3 ]Therapeutic approaches to regulation of uterine contractions
Perhaps the most common gynecological problem associated with uterine motility is primary dysmenorrhea. There is reasonable evidence to support the efficacy of the usual treatments including the contraceptive pill 20 or non-steroidal anti-inflammatory drugs (NSAIDs) 21. The mechanisms of these therapies appear to be directed towards limiting the contractile stimuli to the uterus (through steroid hormonal effects of suppression of inflammatory stimuli) rather than directly interfering with the contractions themselves. Hence, the duration of the effects (and side-effects) of treatment may actually be longer than the duration of the increased uterine contractility resulting in the painful contractions. Furthermore, in view of the intense increases in intrauterine pressure that usually accompany dysmenorrhea, it is likely that it is the outer, predominant zone of the myometrium that is mediating the contractions rather than then inner junctional zone that may be the site of pathophysiology in the other important disorders including abnormal sperm transport, fertilization, implantation, endometriosis and ectopic pregnancy.
The recently developed concept that contractile activity in the non-pregnant uterus results from a distinct zone of the inner myometrium emphasizes current lack of understanding of this organ even at the level of its anatomy and histology. Understanding its physiology and pharmacology lags even further behind. Much additional research is necessary before therapeutic agents can be designed or attempted, to increase the clarity of the recommendation on the basis of strong evidence. Even with the greater volume of research information concerning uterine contractility in late gestation, most attempts to prevent or inhibit uterine contractions have had little, if any, beneficial effect and have resulted in common and serious side-effects 22. However, there are some considerations with fair supportive evidence as to where research into therapeutic manipulation of endometrial wave activity in the non-pregnant state could be undertaken immediately.
The strongest evidence regarding regulation of the junctional zone of the myometrium concerns the effects of ovarian steroids 23. Perhaps the research strategy with the greatest potential for success would be a systematic assessment of the effects of estradiol and/or progesterone or their well-characterized antagonists on endometrial waves at different stages of the reproductive cycle. There is almost a complete void of research data in this potentially fruitful area 3. Endpoints would include parameters that have both physiological as well as clinical relevance: effects on frequency, amplitude, duration and direction of wave propagations as well as measures of clinical effectiveness. Vaginal suppositories of progesterone will diminish uterine activity at the time of embryo transfer following in vitro fertilization 24 but the effects on the rate of successful cycles has not been systematically evaluated.
An important pharmacological principle is to minimize potential toxicity by maximizing the specificity of the therapeutic agent for the target organ. Oxytocin is the most potent and specific contractile agonist and its receptor levels in non-pregnant rat uterine tissue are very high, similar to those at the time of parturition (Arthur et al., 2008). More studies are required to determine the expression of the oxytocin/oxytocin receptor system specifically in the human and particularly in the junctional myometrium through the reproductive cycle. However, vaginally administered OT increases basal uterine tone as well as the frequency and amplitude of cervical–fundal contractions 25, but despite obvious potential use to aid sperm transport in normal or donor insemination cycles, it has never been assessed for therapeutic efficacy in this regard 3. This is an obvious area for increased clinical research 3. In addition, the possibility that new, orally active anti-oxytocic agents will have a role to play in treating these conditions involving the junctional myometrium or in alleviating dysmenorrhea needs to be appropriately investigated. In a recent case report, the anti-cholinergic hyoscine bromide (another antagonist of the pro-contractile pathway) was used to decrease the frequency of uterine peristalsis and appeared to be of benefit in three women with repeated failures with in vitro fertilization 26.
At present, there are many well-characterized inhibitors and activators of many of the pathways described in this review. For example, Ca2+ channel blockers can effectively prevent the Ca2+ influx necessary to enable a contraction. Inhibitors of calmodulin (CaM) and smooth muscle MLCK enzyme (smMLCK) have been thoroughly studied in vitro and have demonstrated the expected reduction in phosphorylation of MLC20 levels. However, there currently are no antagonists of these proteins in use therapeutically. The energy supply could be disrupted using myosin ATPase inhibitors to reduce the rate of active cross bridge cycling. ‘Ca2+ sensitization’ mechanisms can be manipulated using well-studied agents that are activators or inhibitors of rhoA, Rho-associated kinase (ROK) or MLC20 phosphatase (MLCP). Stimulation of cAMP or cGMP can affect several key factors, particularly smMLCK and MYPT1, which can diminish uterine contractile activity. The concerns with all of these agents relate to their non-specificity and, as has been learned from their use in pregnancy, the resulting potential for significant side-effects. Considering the centrality of many of these protein targets in mediating uterine smooth muscle contractility in all muscle beds, it may be difficult to develop pharmacological tools with therapeutic efficacy for uterine disorders without significant advances in drug targeting technologies.
Uterine contractions period
The uterus frequently contracts throughout the entire menstrual cycle, and these contractions have been termed endometrial waves or contractile waves 3. These appear to involve only the sub-endometrial layer of the myometrium 3. In the early follicular phase, these contractions occur once or twice per minute and last 10–15 seconds with a low amplitude of usually 30 mmHg 3. The frequency increases to 3–4 per minute towards ovulation. During the luteal phase, the frequency and amplitude decrease, possibly to facilitate any implantation.
If implantation does not occur, the frequency remains low, but the amplitude increases dramatically to between 50 and 200 mmHg producing labor-like contractions at the time of menstruation 3. These contractions are sometimes termed menstrual cramps, although that term is often used for menstrual pain in general. These contractions may be uncomfortable or even painful, but they are generally significantly less painful than contractions during labor.
Uterine contractions during pregnancy
Braxton Hicks contractions
Braxton Hicks’ contractions, also known as false labor, “prodromal” or “latent” labor. Braxton Hicks contractions are sporadic uterine contractions that actually start at about 6 weeks, although you will not feel them that early. Most women start feeling them during the second or third trimester of pregnancy. Braxton Hicks’ contractions soften and thin the cervix to help your body get ready for labor and birth. You may feel them in the weeks right before your due date. Learning the differences between true labor contractions and false labor contractions can help you know when you’re really in labor.
Braxton Hicks’ contractions:
- Are typically short
- Are not painful
- DO NOT come at regular intervals
- Are not accompanied by bleeding, leaking fluid, or decreased fetal movement
- Are concentrated in your abdomen
- Make your belly feel tight
- May be uncomfortable at times
You may get these contractions when you’re tired, dehydrated, or on your feet too much. False labor will usually ease up if you change what you’re doing.
Braxton Hicks contractions is a tightening of the uterine muscles for one to two minutes and is thought to be an aid to yor body in its preparation for birth. Not all expectant mothers have Braxton Hicks contractions. They are thought to be part of the process of effacement, the thinning and dilation of the cervix.
It can be hard to tell the difference between true labor and false labor. When you first feel contractions, time them. Write down how much time it takes from the start of one contraction to the start of the next. Make a note of how strong the contractions feel. Keep a record of your contractions for 1 hour. Walk or move around to see if the contractions stop when you change positions.
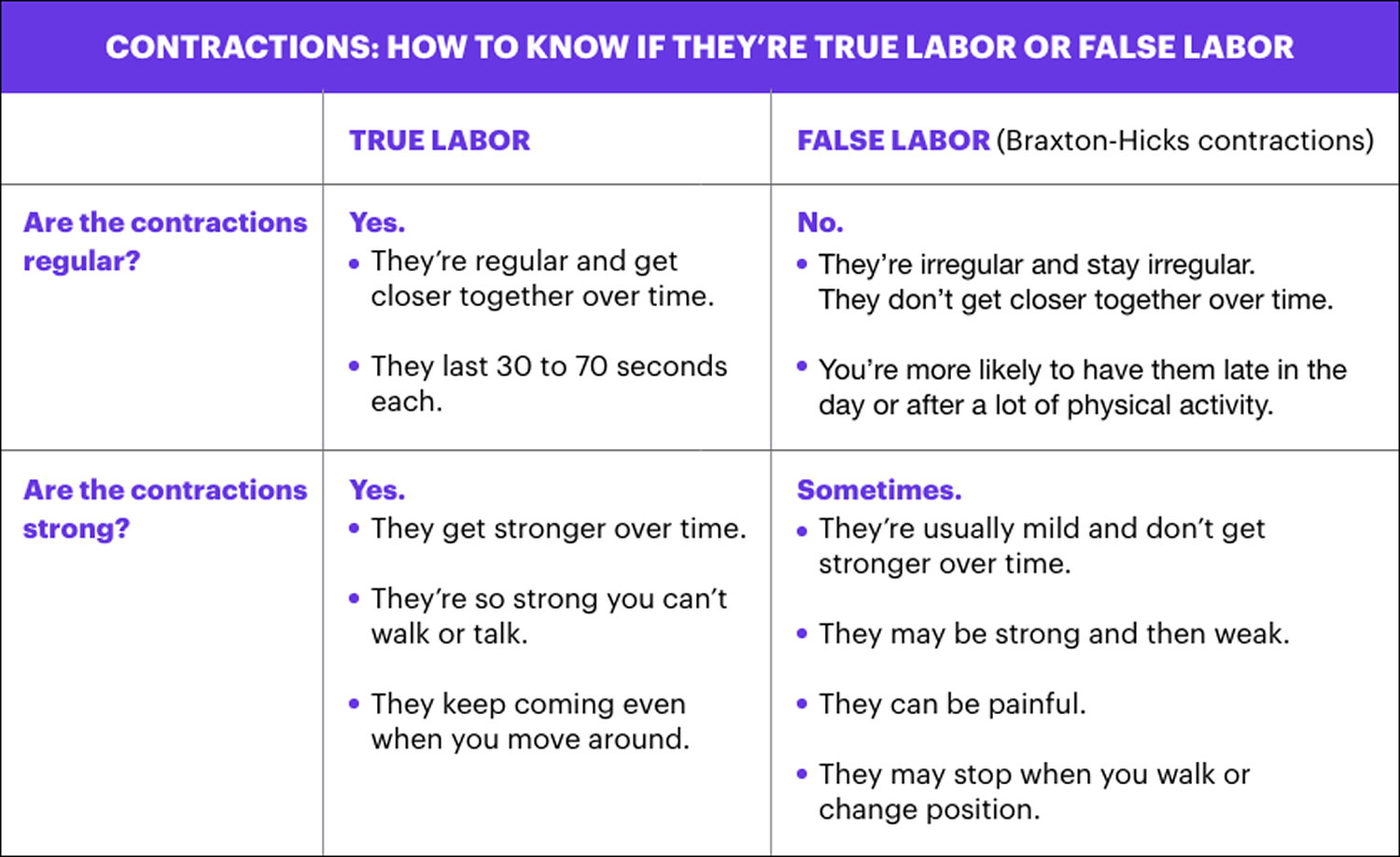
Table 1. Uterine contractions – true labor versus false labor
Methods for ceasing Braxton Hicks contractions include:
- changing position (like from standing to sitting);
- taking a warm bath or shower;
- drinking water;
- resting;
- changing activities, stop what you’re doing and rest (preferably on your left side).
If you’ve tried these things and you’re still having frequent Braxton-Hicks contractions, it’s a good idea to call your doctor to rule out preterm labor.
Preterm labor contractions
Preterm labor is labor that begins too early, before 37 weeks of pregnancy. Premature babies (born before 37 weeks of pregnancy) can have health problems at birth and later in life. If you’re not to 37 weeks of pregnancy and you have signs or symptoms of preterm labor, call your doctor. Getting help quickly is the best thing you can do. Preterm and premature mean the same thing — early.
Preterm labor can lead to premature birth. Premature birth is when your baby is born early, before 37 weeks of pregnancy. Your baby needs about 40 weeks in the womb to grow and develop before birth.
Babies born before 37 weeks of pregnancy are called premature. Premature babies can have serious health problems at birth and later in life. About 1 in 10 babies is born prematurely each year in the United States.
Signs and symptoms of preterm labor
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Learn the signs and symptoms of preterm labor so you can get help quickly if they happen to you.
If you have even one of these signs and symptoms of preterm labor, call your doctor right away:
- Change in your vaginal discharge (watery, mucus or bloody) or more vaginal discharge than usual
- Pressure in your pelvis or lower belly, like your baby is pushing down
- Constant low, dull backache
- Belly cramps with or without diarrhea
- Regular or frequent contractions that make your belly tighten like a fist. The contractions may or may not be painful.
- Your water breaks
When you see your provider, he may do a pelvic exam or a transvaginal ultrasound to see if your cervix has started to thin out and open for labor. Your cervix is the opening to the uterus (womb) that sits at the top of the vagina (birth canal). A transvaginal ultrasound is done in the vagina instead of on the outside of your belly. Like a regular ultrasound, it uses sound waves and a computer to make a picture of your baby. If you’re having contractions, your provider monitors them to see how strong and far apart they are. You may get other tests to help your provider find out if you really are in labor.
If you’re having preterm labor, your provider may give you treatment to help stop it. Or you may get treatment to help improve your baby’s health before birth. Talk to your provider about which treatments may be right for you.
Risk factors for preterm labor and premature birth
Experts don’t always know for sure what causes preterm labor and premature birth. Sometimes labor starts on its own without warning. Even if you do everything right during pregnancy, you can still give birth early.
Experts do know some things may make you more likely than others to have preterm labor and premature birth. These are called risk factors. Having a risk factor doesn’t mean for sure that you’ll have preterm labor or give birth early. But it may increase your chances. Talk to your health care provider about what you can do to help reduce your risk.
Because many premature babies are born with low birthweight, many risk factors for preterm labor and premature birth are the same as for having a low-birthweight baby. Low birthweight is when a baby is born weighing less than 5 pounds, 8 ounces.
These three risk factors make you most likely to have preterm labor and give birth early:
- You’ve had a premature baby in the past.
- You’re pregnant with multiples (twins, triplets or more).
- You have problems with your uterus or cervix now or you’ve had them in the past. Your uterus (also called the womb) is where your baby grows inside you.
Medical risk factors before pregnancy for preterm labor and premature birth:
- Being underweight or overweight before pregnancy. This can include having an eating disorder, like anorexia or bulimia.
- Having a family history of premature birth. This means someone in your family (like your mother, grandmother or sister) has had a premature baby. If you were born prematurely, you’re more likely than others to give birth early.
- Getting pregnant again too soon after having a baby. For most women it’s best to wait at least 18 months before getting pregnant again. Talk to your provider about the right amount of time for you.
Medical risk factors during pregnancy for preterm labor and premature birth
Having certain health conditions during pregnancy can increase your risk for preterm labor and premature birth, including:
- Connective tissue disorders, like Ehlers-Danlos syndromes (also called EDS) and vascular Ehlers-Danlos syndrome (also called vEDS). Connective tissue is tissue that surrounds and supports other tissues and organs. Ehlers-Danlos syndrome can cause joints to be loose and easy to dislocate; skin to be thin and easily stretched and bruised; and blood vessels to be fragile and small. It also can affect your uterus and intestines. Vascular Ehlers-Danlos syndrome is the most serious kind of Ehlers-Danlos syndrome because it can cause arteries and organs (like the uterus) to rupture (burst). Ehlers-Danlos syndrome and vascular Ehlers-Danlos syndrome are genetic conditions that can be passed from parent to child through genes.
- Diabetes. Diabetes is when your body has too much sugar (called glucose) in your blood.
- High blood pressure and preeclampsia. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. This can stress your heart and cause problems during pregnancy. Preeclampsia is a kind of high blood pressure some women during or right after pregnancy. If not treated, it can cause serious problems and even death.
- Infections, including sexually transmitted infections (also called STIs or STDs) and infections of the uterus, urinary tract or vagina
- Intrahepatic cholestasis of pregnancy. This is the most common liver condition that happens during pregnancy.
- Thrombophilias. These are conditions that increase your risk of making abnormal blood clots.
Other medical risk factors during pregnancy include:
- Getting late or no prenatal care. Prenatal care is medical care you get during pregnancy.
- Not gaining enough weight during pregnancy. This can include having an eating disorder, like anorexia or bulimia.
- Bleeding from the vagina in the second or third trimester
- Preterm premature rupture of the membranes also called PPROM. Premature rupture of membranes (also called PROM) is when the amniotic sac around your baby breaks (your water breaks) before labor starts. PPROM is when this happens before 37 weeks of pregnancy. If you have any fluid leaking from your vagina, call your provider and go to the hospital.
- Being pregnant after in vitro fertilization also called IVF. IVF is a fertility treatment used to help women get pregnant.
- Being pregnant with a baby who has certain birth defects, like heart defects or spina bifida. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works. Spina bifida is a birth defect of the spine.
Risk factors in your everyday life for preterm labor and premature birth:
- Smoking, drinking alcohol, using street drugs or abusing prescription drugs
- Having a lot of stress in your life.
- Low socioeconomic status. Socioeconomic status is a combination of things like your education, your job and your income (how much money you make).
- Domestic violence. This is when your partner hurts or abuses you. It includes physical, sexual and emotional abuse.
- Working long hours or having to stand a lot
- Exposure to air pollution, lead, radiation and chemicals in things like paint, plastics and secondhand smoke. Secondhand smoke is smoke from someone else’s cigarette, cigar or pipe.
Age and race as risk factors for preterm labor and premature birth:
- Being younger than 17 or older than 35 makes you more likely than other women to give birth early. In the United States, black women are more likely to give birth early. Almost 17 percent of black babies are born prematurely each year. Just more than 10 percent of American Indian/Alaska Native and Hispanic babies are born early, and less than 10 percent of white and Asian babies. We don’t know why race plays a role in premature birth; researchers are working to learn more about it.
Can I reduce your risk for preterm labor and premature birth?
Yes, you may be able to reduce your risk for early labor and birth. Some risk factors are things you can’t change, like having a premature birth in a previous pregnancy. Others are things you can do something about, like quitting smoking.
Here’s what you can do to reduce your risk for preterm labor and premature birth:
- Get to a healthy weight before pregnancy and gain the right amount of weight during pregnancy. Talk to your doctor about the right amount of weight for you before and during pregnancy.
- Don’t smoke, drink alcohol use street drugs or abuse prescription drugs. Ask your provider about programs that can help you quit.
- Go to your first prenatal care checkup as soon as you think you’re pregnant. During pregnancy, go to all your prenatal care checkups, even if you’re feeling fine. Prenatal care helps your provider make sure you and your baby are healthy.
- Get treated for chronic health conditions, like high blood pressure, diabetes, depression and thyroid problems. Depression is a medical condition in which strong feelings of sadness last for a long time and interfere with your daily life. It needs treatment to get better. The thyroid is a gland in your neck that makes hormones that help your body store and use energy from food.
- Protect yourself from infections. Talk to your doctor about vaccinations that can help protect you from certain infections. Wash your hands with soap and water after using the bathroom or blowing your nose. Don’t eat raw meat, fish or eggs. Have safe sex. Don’t touch cat poop.
- Reduce your stress. Eat healthy foods and do something active every day. Ask family and friends for help around the house or taking care of other children. Get help if your partner abuses you. Talk to your boss about how to lower your stress at work.
- Wait at least 18 months between giving birth and getting pregnant again. Use birth control until you’re ready to get pregnant again. If you’re older than 35 or you’ve had a miscarriage or stillbirth, talk to your provider about how long to wait between pregnancies. Miscarriage is the death of a baby in the womb before 20 weeks of pregnancy. Stillbirth is the death of a baby in the womb after 20 weeks of pregnancy.
What should I do if I think I’m having preterm labor?
If you have even one sign or symptom of preterm labor, call your health care provider right away. If you have preterm labor, getting help quickly is the best thing you can do.
When you see your doctor, he may do a pelvic exam or a transvaginal ultrasound to see if your cervix has started to thin out and open for labor. Your cervix is the opening to the uterus (womb) that sits at the top of the vagina (birth canal). A transvaginal ultrasound is done in the vagina instead of on the outside of your belly. Like a regular ultrasound, it uses sound waves and a computer to make a picture of your baby. If you’re having contractions, your provider monitors them to see how strong and far apart they are. You may get other tests to help your provider find out if you really are in labor.
If you’re having preterm labor, your provider may give you treatment to help stop it or to help improve your baby’s health before birth. Talk to your provider about which treatments may be right for you.
Uterine contractions and signs of labor
Labor also called childbirth, is the process of your baby leaving the uterus (womb). You’re in labor when you have regular contractions that cause your cervix to change. Contractions are when the muscles of your uterus get tight and then relax. Contractions help push your baby out of your uterus. Your cervix is the opening to the uterus that sits at the top of the vagina. When labor starts, your cervix dilates (opens up).
In real labor, your contractions will:
- Come regularly and get closer together
- Last from 30 to 70 seconds, and will get longer
- Not stop, no matter what you do
- Radiate (reach) into your lower back and upper belly
- Get stronger or become more intense as time goes on
- Make you unable to talk to other people or laugh at a joke
You know you’re in true labor when:
- You have strong and regular contractions. A contraction is when the muscles of your uterus tighten up like a fist and then relax. Contractions help push your baby out. When you’re in true labor, your contractions last about 30 to 70 seconds and come about 5 to 10 minutes apart. They’re so strong that you can’t walk or talk during them. They get stronger and closer together over time.
- You feel pain in your belly and lower back. This pain doesn’t go away when you move or change positions.
- You have a bloody (brownish or reddish) mucus discharge. This is called bloody show.
- Your water breaks. Your baby has been growing in amniotic fluid (the bag of waters) in your uterus. When the bag of waters breaks, you may feel a big rush of water. Or you may feel just a trickle.
If you think you’re in labor, call your health care provider, no matter what time of day or night. Your doctor or midwife can tell you if it’s time to head for the hospital. To see for sure that you’re in labor, your health care provider measures your cervix.
Signs that labor is near
You may be close to starting labor if:
Lightening. This happens when your baby’s head “drops” down into your pelvis. It means that your baby is getting ready to move into position for birth. It can happen a few weeks or even just a few hours before your labor begins.
- Your belly will look lower. It will be easier for you to breathe because the baby is not putting pressure on your lungs.
- You may need to urinate more often because the baby is pressing on your bladder.
- For first-time mothers, lightening often happens a few weeks before birth. For women who have had babies before, it may not happen until labor has begun.
Bloody show. You have an increase in vaginal discharge that’s clear, pink or slightly bloody. If you have bloody or brownish discharge from your vagina, it may mean your cervix has begun to dilate. The mucous plug that sealed your cervix for the last 9 months may be visible. This is a good sign. It can happen a few days before labor starts or at the beginning of labor. But active labor may still be days away.
Your baby moves less. If you feel less movement, call your health care provider, as sometimes decreased movement can mean that the baby is in trouble.
Your water breaks. When the amniotic sac (bag of fluid around the baby) breaks, you will feel fluid leak from your vagina. It may come out in a trickle or a gush.
- For most women, contractions come within 24 hours after the bag of water breaks.
- Even if contractions do not begin, let your provider know as soon as you think your water has broken.
Diarrhea. Some women have the urge to go to the bathroom often to empty their bowels. If this happens and your stools are looser than normal, you may be going into labor.
You have the nesting instinct. This is when you want to get things organized in your home to get ready for your baby. There is no science behind this theory, but plenty of women feel the sudden urge to “nest” right before labor starts. You may want to do things like cook meals or get the baby’s clothes and room ready. If you feel the need to vacuum the entire house at 3 a.m., or finish your work in the baby’s nursery, you may be getting ready for labor. Doing these things is fine as long as you’re careful not to overdo it. You need your energy for labor and birth.
At a prenatal checkup, your health care provider tells you that your cervix has begun to efface (thin) and dilate (open). Before labor, your cervix is about 3.5 to 4 centimeters long. When it’s fully dilated (open) for labor, it’s 10 centimeters. Once labor starts, contractions help open your cervix.
See your doctor or midwife right away if you have:
- Leaking amniotic fluid
- Decreased fetal movement
- Any vaginal bleeding other than light spotting
- Regular, painful contractions every 5 to 10 minutes for 60 minutes
See see your doctor for any other reason if you are unsure what to do.
- Blanks, A.M.; Shmygol, A.; Thornton, S. Preterm labour. Myometrial function in prematurity. Best Pract. Res. Clin. Obstet. Gynecol. 2007, 21, 807–819.
- Lyons, E.A.; Taylor, P.J.; Zheng, X.H.; Ballard, G.; Levi, C.S.; Kredentser, J.V. Characterization of subendometrial myometrial contractions throughout the menstrual cycle in normal fertile women. Fertil. Steril. 1991, 55, 771–774.
- Hector N. Aguilar, B.F. Mitchell, Physiological pathways and molecular mechanisms regulating uterine contractility, Human Reproduction Update, Volume 16, Issue 6, November-December 2010, Pages 725–744, https://doi.org/10.1093/humupd/dmq016
- Magnetically Bioprinted Human Myometrial 3D Cell Rings as A Model for Uterine Contractility. Int. J. Mol. Sci. 2017, 18(4), 683; https://doi.org/10.3390/ijms18040683
- Wray, S. Insights from physiology into myometrial function and dysfunction. Exp. Physiol. 2015, 100, 1468–1476.
- van Gestel I, MM IJ, Hoogland HJ, Evers JL. Endometrial wave-like activity in the non-pregnant uterus, Hum Reprod Update , 2003, vol. 2 pg. 131-138
- Bulletti C, de Ziegler D. Uterine contractility and embryo implantation, Curr Opin Obstet Gynecol , 2006, vol. 4 pg. 473-484.
- Ijland MM, Evers JL, Dunselman GA, van Katwijk C, Lo CR, Hoogland HJ. Endometrial wavelike movements during the menstrual cycle, Fertil Steril , 1996, vol. 4 pg. 746-749
- Huszar G, Naftolin F. The myometrium and uterine cervix in normal and preterm labor, N Engl J Med , 1984, vol. 9 pg. 571-581
- Brosens JJ, Barker FG, de Souza NM. Myometrial zonal differentiation and uterine junctional zone hyperplasia in the non-pregnant uterus, Hum Reprod Update , 1998, vol. 5 pg. 496-502
- Hricak H, Alpers C, Crooks LE, Sheldon PE. Magnetic resonance imaging of the female pelvis: initial experience, AJR Am J Roentgenol , 1983, vol. 6 pg. 1119-1128
- Noe M, Kunz G, Herbertz M, Mall G, Leyendecker G. The cyclic pattern of the immunocytochemical expression of oestrogen and progesterone receptors in human myometrial and endometrial layers: characterization of the endometrial-subendometrial unit, Hum Reprod , 1999, vol. 1 pg. 190-197
- Weiss S, Jaermann T, Schmid P, Staempfli P, Boesiger P, Niederer P, Caduff R, Bajka M. Three-dimensional fiber architecture of the nonpregnant human uterus determined ex vivo using magnetic resonance diffusion tensor imaging, Anat Rec A Discov Mol Cell Evol Biol , 2006, vol. 1 pg. 84-90
- Andrews J, Blackshaw LA. Feldman M, Friedman LS, Brandt LJ. Small intestinal motor and sensory function and dysfunction, Sleisenger and Fordtran’s Gastrointestinal and Liver Disease , 2006 Saunders pg. 2093-2111
- Mitchell BF, Taggart MJ. Are animal models relevant to key aspects of human parturition?, Am J Physiol Regul Integr Comp Physiol , 2009, vol. 3 pg. R525-R545
- Gunst SJ, Zhang W. Actin cytoskeletal dynamics in smooth muscle: a new paradigm for the regulation of smooth muscle contraction, Am J Physiol Cell Physiol , 2008, vol. 3 pg. C576-C587
- Gabella G. Structural apparatus for force transmission in smooth muscles, Physiol Rev , 1984, vol. 2 pg. 455-477
- Word RA, Stull JT, Casey ML, Kamm KE. Contractile elements and myosin light chain phosphorylation in myometrial tissue from nonpregnant and pregnant women, J Clin Invest , 1993, vol. 1 pg. 29-37
- Kordowska J, Huang R, Wang CL. Phosphorylation of caldesmon during smooth muscle contraction and cell migration or proliferation, J Biomed Sci , 2006, vol. 2 pg. 159-172
- Wong CL, Farquhar C, Roberts H, Proctor M. Oral contraceptive pill as treatment for primary dysmenorrhoea, Cochrane Database Syst Rev , 2009, vol. 2 pg. CD002120
- Marjoribanks J, Proctor ML, Farquhar C. Nonsteroidal anti-inflammatory drugs for primary dysmenorrhoea, Cochrane Database Syst Rev , 2003, vol. 4 pg. CD001751
- Mitchell BF, Olson DM. Prostaglandin endoperoxide H synthase inhibitors and other tocolytics in preterm labour, Prostaglandins Leukot Essent Fatty Acids , 2004, vol. 2 pg. 167-187
- Fanchin R, Ayoubi JM, Olivennes F, Righini C, de Ziegler D, Frydman R. Hormonal influence on the uterine contractility during ovarian stimulation, Hum Reprod , 2000, vol. 15(Suppl.1) pg. 90-100
- Fanchin R, Righini C, de Ziegler D, Olivennes F, Ledee N, Frydman R. Effects of vaginal progesterone administration on uterine contractility at the time of embryo transfer, Fertil Steril , 2001, vol. 6 pg. 1136-1140
- Kunz G, Noe M, Herbertz M, Leyendecker G. Uterine peristalsis during the follicular phase of the menstrual cycle: effects of oestrogen, antioestrogen and oxytocin, Hum Reprod Update , 1998, vol. 5 pg. 647-654
- Kido A, Togashi K, Hatayama H, Nakayama T, Yamamoto A, Kataoka M, Tulandi T. Uterine peristalsis in women with repeated IVF failures: possible therapeutic effect of hyoscine bromide, J Obstet Gynaecol Can , 2009, vol. 8 pg. 732-735