Ventricular flutter
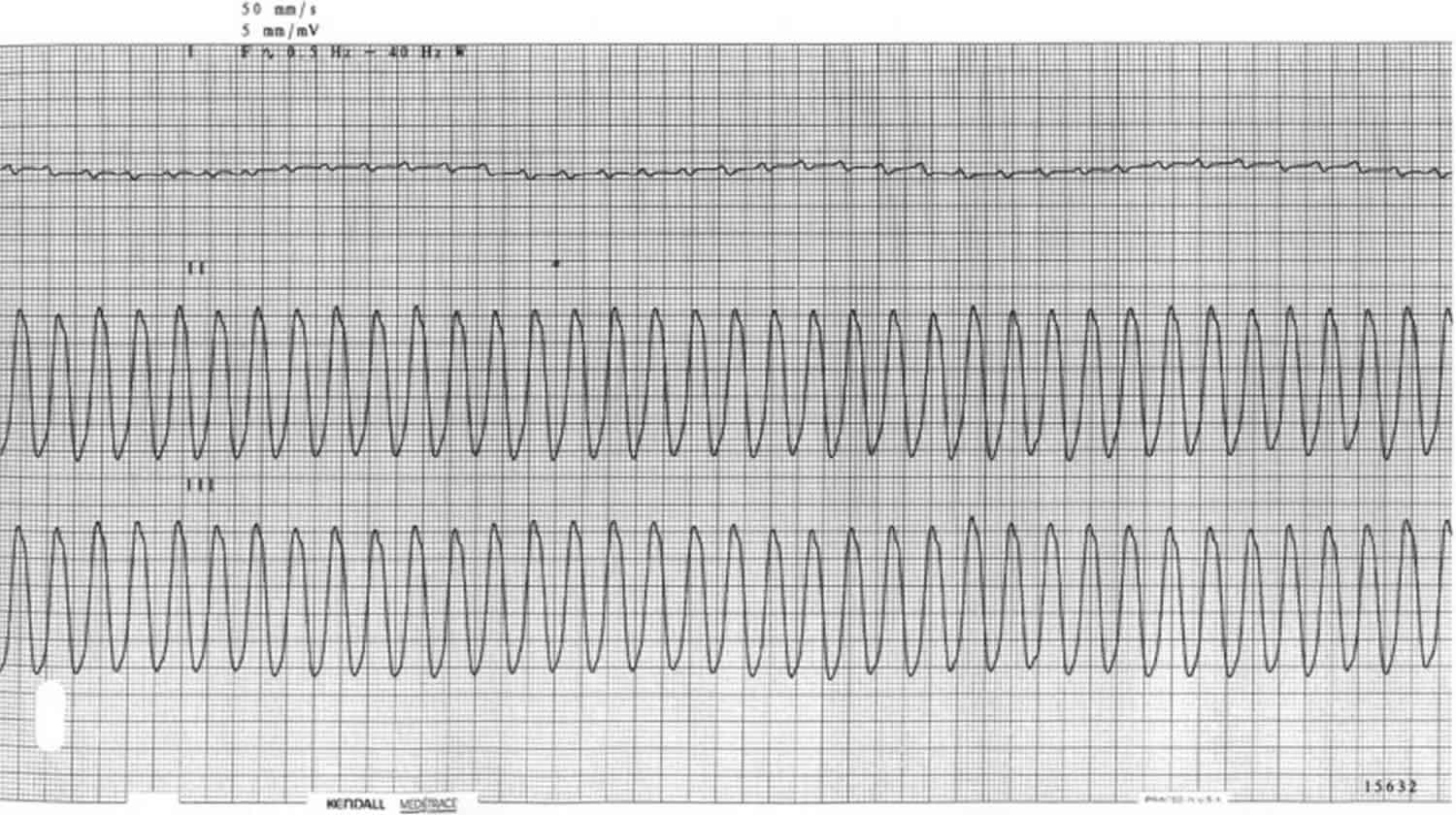
Ventricular flutter is a rapid ventricular tachycardia (250 to 350 beats/min), which is characterized by a sinusoidal QRS configuration on the electrocardiogram (ECG) that prevents identification of the QRS morphology (P waves, QRS complexes and T waves cannot be distinguished) 1. Ventricular flutter is closely related to ventricular fibrillation and can progress to ventricular fibrillation. In severe cardiac or systemic disease states, ventricular tachycardia can progress to ventricular flutter, then to ventricular fibrillation. Ventricular flutter clinical implications, causes, and consequences are very similar to ventricular fibrillation. The two arrhythmias are classified together 2. Ventricular flutter is a critically unstable arrhythmia that can result in sudden cardiac death. Ventricular flutter can occur in infancy, youth, or as an adult. It can be induced by programmed electrical stimulation.
Idiopathic ventricular flutter also called primary ventricular flutter occurs in patients with normal cardiac structure. Primary ventricular flutter has been estimated to account for 5% of cases of sudden cardiac death with the mean age 36 years, and the male to female ratio of 2.5:1 3.
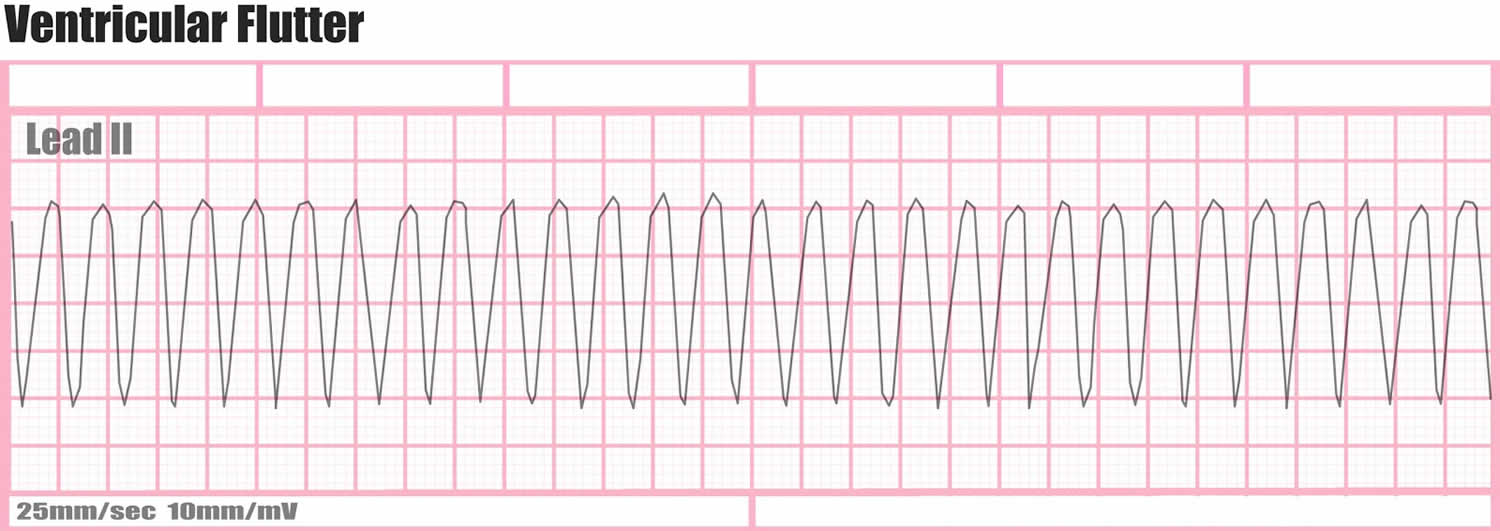
Figure 1. Ventricular flutter ECG
Ventricular flutter cause
The cause of ventricular flutter isn’t always known. The most common cause is a problem in the electrical impulses traveling through your heart after a first heart attack or problems resulting from a scar in your heart’s muscle tissue from a previous heart attack.
Some cases of ventricular flutter begin as a rapid heartbeat called ventricular tachycardia (VT). This rapid but regular beating of the heart is caused by abnormal electrical impulses that start in the ventricles.
Most ventricular tachycardia occurs in people with a heart-related problem, such as scars or damage from a heart attack. Sometimes ventricular tachycardia can last less than 30 seconds (nonsustained) and may not cause symptoms. But ventricular tachycardia may be a sign of more-serious heart problems.
If ventricular tachycardia lasts more than 30 seconds, it will usually lead to palpitations, dizziness or fainting. Untreated ventricular tachycardia will often lead to ventricular flutter.
Most cases of ventricular flutter are linked to some form of heart disease.
Risk factors for developing ventricular flutter
Factors that may increase your risk of ventricular flutter include:
- A previous episode of ventricular flutter
- A previous heart attack
- A heart defect you’re born with (congenital heart disease)
- Heart muscle disease (cardiomyopathy)
- Injuries that cause damage to the heart muscle, such as electrocution
- Use of illegal drugs, such as cocaine or methamphetamine
- Significant electrolyte abnormalities, such as with potassium or magnesium.
Ventricular flutter prevention
If you have one first-degree relative — a parent, sibling or child — with an inherited heart condition (congenital heart disease), talk with your doctor about genetic screening. Identifying an inherited heart problem early can guide preventive care and reduce your risk of complications.
Ventricular flutter symptoms
Loss of consciousness is the most common sign of ventricular flutter.
Early signs and symptoms
A condition in which the lower chambers of your heart beat too rapidly (ventricular tachycardia, or VT) can lead to ventricular flutter. Signs and symptoms of ventricular tachycardia include:
- Chest pain
- Rapid heartbeat (tachycardia)
- Dizziness
- Nausea
- Shortness of breath
- Loss of consciousness.
If you or someone else is having the above signs and symptoms, seek emergency medical help immediately. Follow these steps:
- Call the emergency number in your area.
- If the person is unconscious, check for a pulse.
- If no pulse, begin CPR to help maintain blood flow to the organs until an electrical shock (defibrillation) can be given. Push hard and fast on the person’s chest — about 100 compressions a minute. It’s not necessary to check the person’s airway or deliver rescue breaths unless you’ve been trained in CPR.
Portable automated external defibrillators, which can deliver an electrical shock that may restart heartbeats, are available in an increasing number of places, such as in airplanes, police cars and shopping malls. They can even be purchased for your home.
Portable defibrillators come with built-in instructions for their use. They’re programmed to deliver a shock only when it’s needed.
Ventricular flutter diagnosis
Ventricular flutter is always diagnosed in an emergency situation. Your doctors will know if you’re in ventricular flutter based on results from:
- Heart monitoring. A heart monitor that will read the electrical impulses that make your heart beat will show that your heart is beating erratically or not at all.
- Pulse check. In ventricular flutter, there will be no pulse.
Tests to diagnose the cause of ventricular flutter
To find out what caused your ventricular flutter, you’ll have additional tests, which can include:
- Electrocardiogram (ECG). This test records the electrical activity of your heart via electrodes attached to your skin. Impulses are recorded as waves displayed on a monitor or printed on paper. Because injured heart muscle doesn’t conduct electrical impulses normally, the ECG may show that a heart attack has occurred or is in progress.
- Blood tests. Emergency room doctors take samples of your blood to test for the presence of certain heart enzymes that leak into your blood if your heart has been damaged by a heart attack.
- Chest X-ray. An X-ray image of your chest allows your doctor to check the size and shape of your heart and its blood vessels.
- Echocardiogram. This test uses sound waves to produce an image of your heart. During an echocardiogram, sound waves are directed at your heart from a transducer, a wandlike device, held on your chest. Processed electronically, the sound waves provide video images of your heart.
- Coronary catheterization (angiogram). To determine if your coronary arteries are narrowed or blocked, a liquid dye is injected through a long, thin tube (catheter) that’s fed through an artery, usually in your leg, to the arteries in your heart. The dye makes your arteries become visible on X-ray, revealing areas of blockage.
- Cardiac computerized tomography (CT). In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest.
- Magnetic resonance imaging (MRI). For a cardiac MRI, you lie on a table inside a long tubelike machine that produces a magnetic field that aligns atomic particles in some of your cells. Radio waves aimed at these aligned particles produce signals that create images of your heart.
Ventricular flutter treatment
Emergency treatments for ventricular flutter focus on restoring blood flow through your body as quickly as possible to prevent damage to your brain and other organs. After blood flow is restored through your heart, if necessary, you’ll have treatment options to help prevent future episodes of ventricular flutter.
Emergency treatments
- Cardiopulmonary resuscitation (CPR). This treatment can help maintain blood flow through the body by mimicking the pumping motion your heart makes. CPR can be performed by anyone, including family members. In a medical emergency, first call for emergency medical help, then start CPR by pushing hard and fast on the person’s chest — about 100 to 120 compressions a minute. Allow the chest to rise completely between compressions. Unless you’re trained in CPR, don’t worry about breathing into the person’s mouth. Keep up chest compressions until a portable defibrillator is available or emergency personnel arrive.
- Direct current cardioversion. The delivery of an electrical shock through the chest wall to the heart momentarily stops the heart and the chaotic rhythm. This often allows the normal heart rhythm to resume.If a public-use automated external defibrillator is available, anyone can administer it. Most public-use automated external defibrillators voice instructions as you use them. Public-use automated external defibrillators are programmed to recognize ventricular flutter and send a shock only when needed.
Treatments to prevent future episodes
If your doctor finds that your ventricular flutter is caused by a change in the structure of your heart, such as scarred tissue from a heart attack, he or she may recommend that you take medications or have a medical procedure performed to reduce your risk of future ventricular flutter and cardiac arrest. Treatment options can include:
- Medications. Doctors use various anti-arrhythmic drugs for emergency or long-term treatment of ventricular flutter. A class of medications called beta blockers is commonly used in people at risk of ventricular flutter or sudden cardiac arrest.
- Implantable cardioverter-defibrillator (ICD). After your condition stabilizes, your doctor is likely to recommend implantation of an ICD. An implantable cardioverter-defibrillator is a battery-powered unit that’s implanted near your left collarbone. One or more flexible, insulated wires (leads) from the implantable cardioverter-defibrillator run through veins to your heart. The implantable cardioverter-defibrillator constantly monitors your heart rhythm. If it detects a rhythm that’s too slow, it sends an electrical signal that paces your heart as a pacemaker would. If it detects ventricular tachycardia or ventricular flutter, it sends out low- or high-energy shocks to reset your heart to a normal rhythm. An implantable cardioverter-defibrillator is more effective than drugs for preventing arrhythmia-induced cardiac arrest.
- Coronary angioplasty and stent placement. This procedure is for the treatment of severe coronary artery disease. It opens blocked coronary arteries, letting blood flow more freely to your heart. If your ventricular flutter was caused by a heart attack, this procedure may reduce your risk of future episodes of ventricular flutter. Doctors insert a long, thin tube (catheter) that’s passed through an artery, either in your leg or arm, to a blocked artery in your heart. This catheter is equipped with a special balloon tip that briefly inflates to open up a blocked coronary artery. At the same time, a metal mesh stent may be inserted into the artery to keep it open long term, restoring blood flow to your heart. Coronary angioplasty may be done at the same time as a coronary catheterization (angiogram), a procedure that doctors do first to locate narrowed arteries to the heart.
- Coronary bypass surgery. Another procedure to improve blood flow is coronary bypass surgery. Bypass surgery involves sewing veins or arteries in place at a site beyond a blocked or narrowed coronary artery (bypassing the narrowed section), restoring blood flow to your heart. This may improve the blood supply to your heart and reduce your risk of ventricular flutter.
Lifestyle and home remedies
Lifestyle changes that help keep your heart as healthy as possible include:
- Eat a healthy diet. Heart-healthy foods include fruits, vegetables and whole grains, as well as lean protein sources such as soy, beans, nuts, fish, skinless poultry and low-fat dairy products. Avoid extra salt (sodium), added sugars and solid fats.
- Exercise regularly. Aim for 150 minutes a week of moderate aerobic activity, 75 minutes a week of vigorous aerobic activity, or a combination of moderate and vigorous activity.
- Stop smoking. You’re more likely to quit successfully if you take advantage of strategies proved to help. Talk with your doctor about medications that can reduce your cravings and reduce symptoms of nicotine withdrawal.
- Keep your blood pressure and cholesterol levels in a healthy range. Take medications as prescribed to correct high blood pressure (hypertension) or high cholesterol, and maintain a healthy body weight.
- Limit alcohol intake. Too much alcohol can damage your heart. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger.
- Maintain follow-up care. Take your medications as prescribed and have regular follow-up appointments with your doctor. Tell your doctor if your symptoms worsen.
- Chapter 22 – Post-Infarction Sustained Monomorphic Ventricular Tachycardia. Clinical Arrhythmology and Electrophysiology: A Companion to Braunwald’s Heart Disease (Second Edition) 2012, Pages 512-561 https://doi.org/10.1016/B978-1-4557-1274-8.00022-1
- xPharm: The Comprehensive Pharmacology Reference Work 2008. ISBN 978-0-08-055232-3
- Viskins S, Lesch MD, Eldar M (1997) J Cardiovasc Electrophysiol 8:1115–1120