Vitamin B12 deficiency
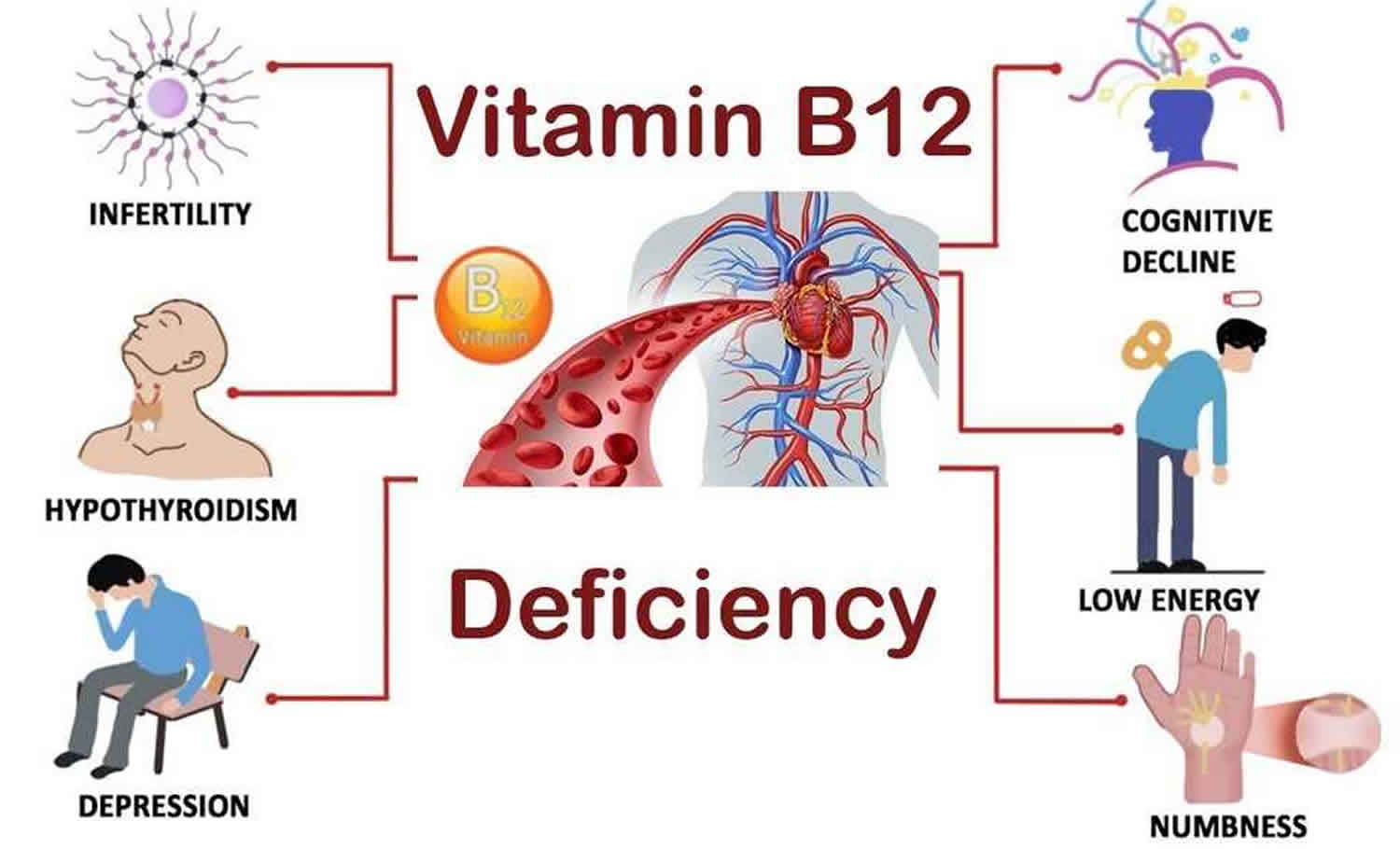
Vitamin B12 deficiency also known as cobalamin deficiency is characterized by megaloblastic anemia, fatigue, weakness, constipation, loss of appetite, and weight loss 1, 2, 3. Neurological changes, such as numbness and tingling in the hands and feet, can also occur 4, 5. Additional symptoms of vitamin B-12 deficiency include difficulty maintaining balance, depression, confusion, dementia, poor memory, and soreness of the mouth or tongue 6. The neurological symptoms of vitamin B12 deficiency can occur without anemia, so early diagnosis and intervention is important to avoid irreversible damage 7. During infancy, signs of a vitamin B12 deficiency include failure to thrive, movement disorders, developmental delays, and megaloblastic anemia 8. Many of these symptoms are general and can result from a variety of medical conditions other than vitamin B-12 deficiency.
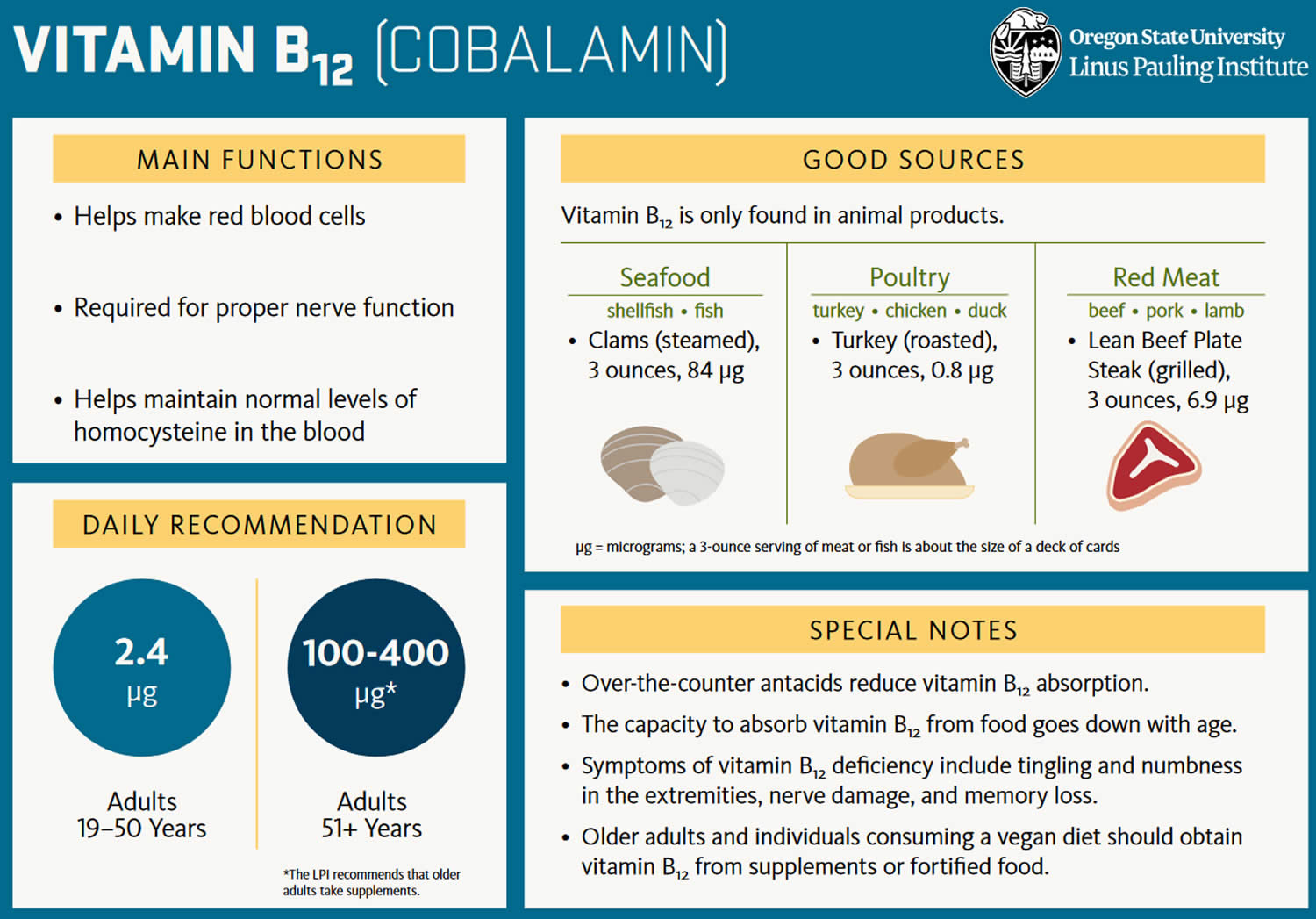
In healthy adults, vitamin B12 deficiency is uncommon, mainly because your body stores 1,000 to 2,000 times as much vitamin B12 (about 3 to 5 mg vitamin B12) as you’d typically eat in a day – total body stores can exceed 2,500 micrograms (2,500 μg), daily turnover is slow, and dietary intake of only 2.4 mcg/day (2.4 μg/day) is sufficient to maintain adequate vitamin B12 status (see Recommended Dietary Allowance [RDA]) 9. Therefore, when there is little or no vitamin B12 in your diet, vitamin B12 stores (about 3 to 5 mg) may last for up to 5–10 years before the signs and symptoms of vitamin B12 deficiency are seen clinically 9. In elderly individuals, vitamin B12 deficiency is more common mainly because of impaired intestinal absorption that can result in marginal to severe vitamin B12 deficiency in this population. The Recommended Dietary Allowance (RDA) for vitamin B12 is 2.4 micrograms per day (2.4 μg/day) for adolescents and adults. It is slightly higher for women who are pregnant (2.6 mcg/day) or breastfeeding (2.8 mcg/day). Currently, to maintain a healthy hematological status and serum vitamin B12 levels, average daily intakes of vitamin B12 from food of 5.94 mcg for men and 3.78 mcg for women aged 20 and older have been recommended 10. For children aged 2–19 years old, mean daily intakes of vitamin B12 from food range from 3.76 mcg to 4.55 mcg 11. The original estimates of dietary folate and vitamin B12 requirements and recommended dietary allowances (RDAs) were based on the amount needed to avoid manifest deficiency disorders (megaloblastic anemia, with sub-acute combined degeneration of the cord in the case of vitamin B12 deficiency) and on levels observed in populations. However, these levels do not essentially represent necessary requirements 10.
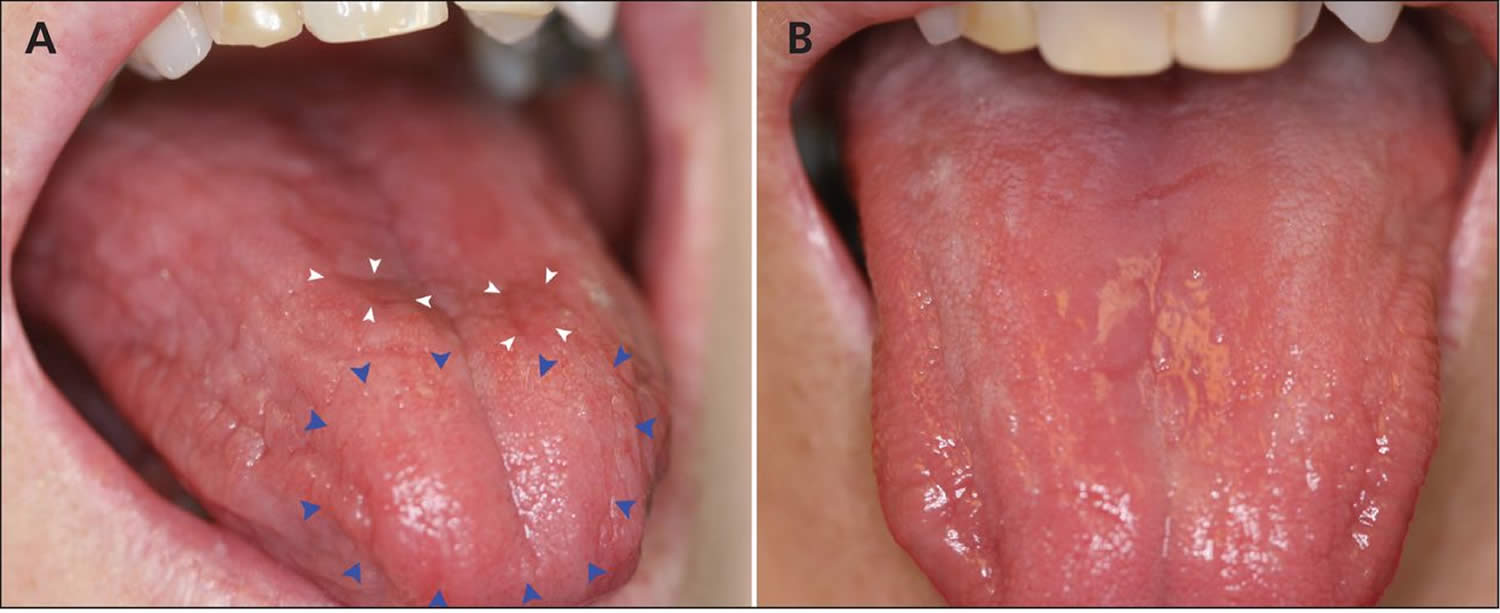
The signs and symptoms of vitamin B12 deficiency can take several years to appear 12, 13. The signs and symptoms of vitamin B12 deficiency can include the hallmark megaloblastic anemia (characterized by large, abnormally nucleated red blood cells) as well as low counts of white and red blood cells, platelets, or a combination; glossitis of the tongue (a condition in which your tongue becomes inflamed and swollen) (Figure 3); fatigue; palpitations; pale skin; dementia; weight loss; and infertility 14, 15, 13. Neurological changes, such as numbness and tingling in the hands and feet, can also occur 13. These neurological symptoms can occur without anemia, so early diagnosis and intervention is important to avoid irreversible damage 16. In addition, some studies have found associations between vitamin B12 deficiency or low vitamin B12 intakes and depression 17, 18, 19. In pregnant and breastfeeding women, vitamin B12 deficiency might cause neural tube defects, developmental delays, failure to thrive, and anemia in babies 13.
Vitamin B12 deficiency with the classic hematologic and neurologic signs and symptoms is uncommon 20. However, low or marginal vitamin B12 status (200–300 pg/mL [148–221 pmol/L]) without these symptoms is much more common, at up to 40% in Western populations, especially in those with low intakes of vitamin B12-rich foods 21, 20. The prevalence of vitamin B12 deficiency varies by cutoff level and biomarker used. For example, among adults aged 19 and older who participated in the National Health and Nutrition Examination Survey (NHANES) between 1999 and 2004, the rate of low vitamin B12 levels in serum was 3% with a cutoff of less than 200 pg/mL (148 pmol/L) and 26% with a cutoff of less than 350 pg/mL (258 pmol/L) 22. Approximately 21% of adults older than 60 had abnormal levels of at least one vitamin B12 biomarker 22.
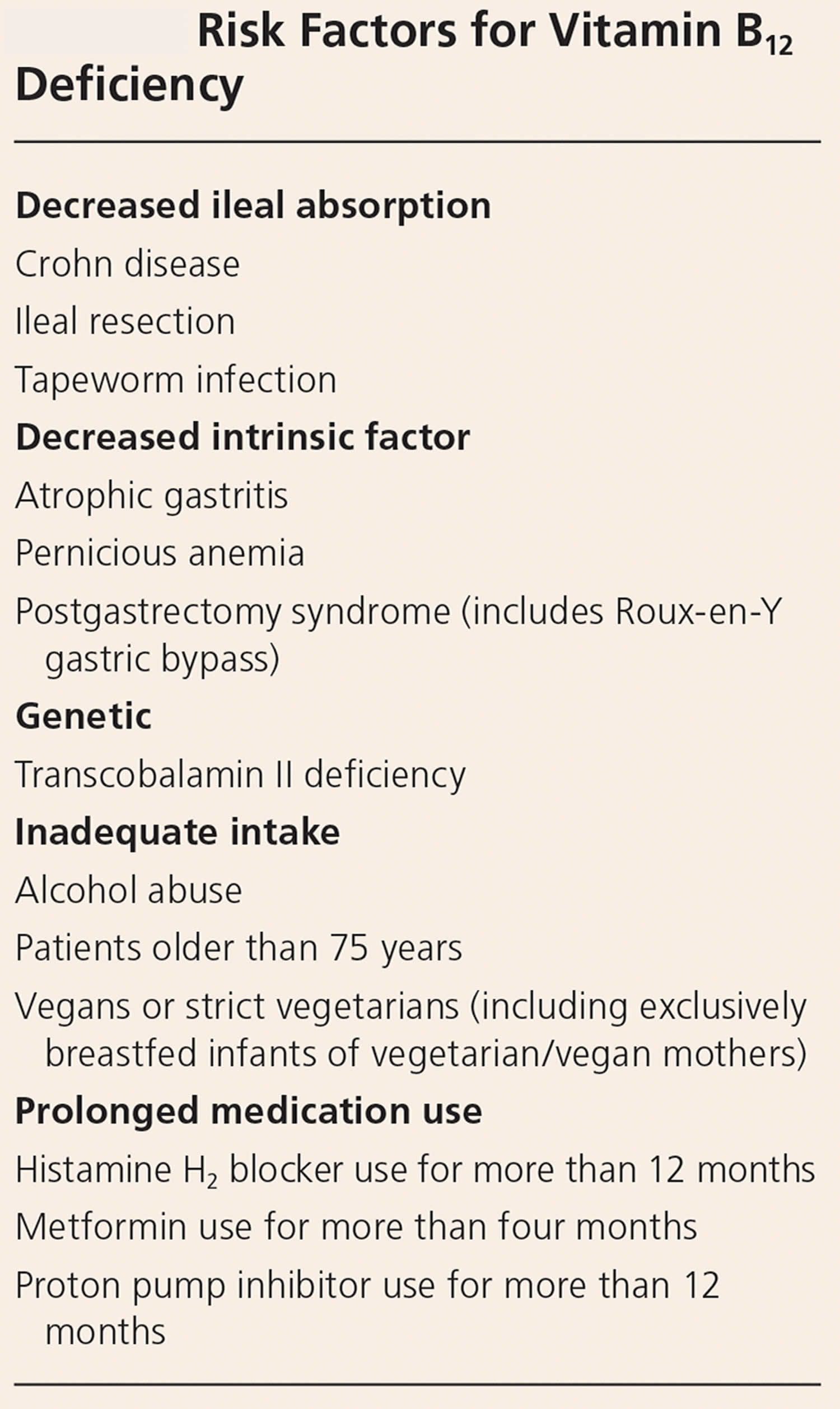
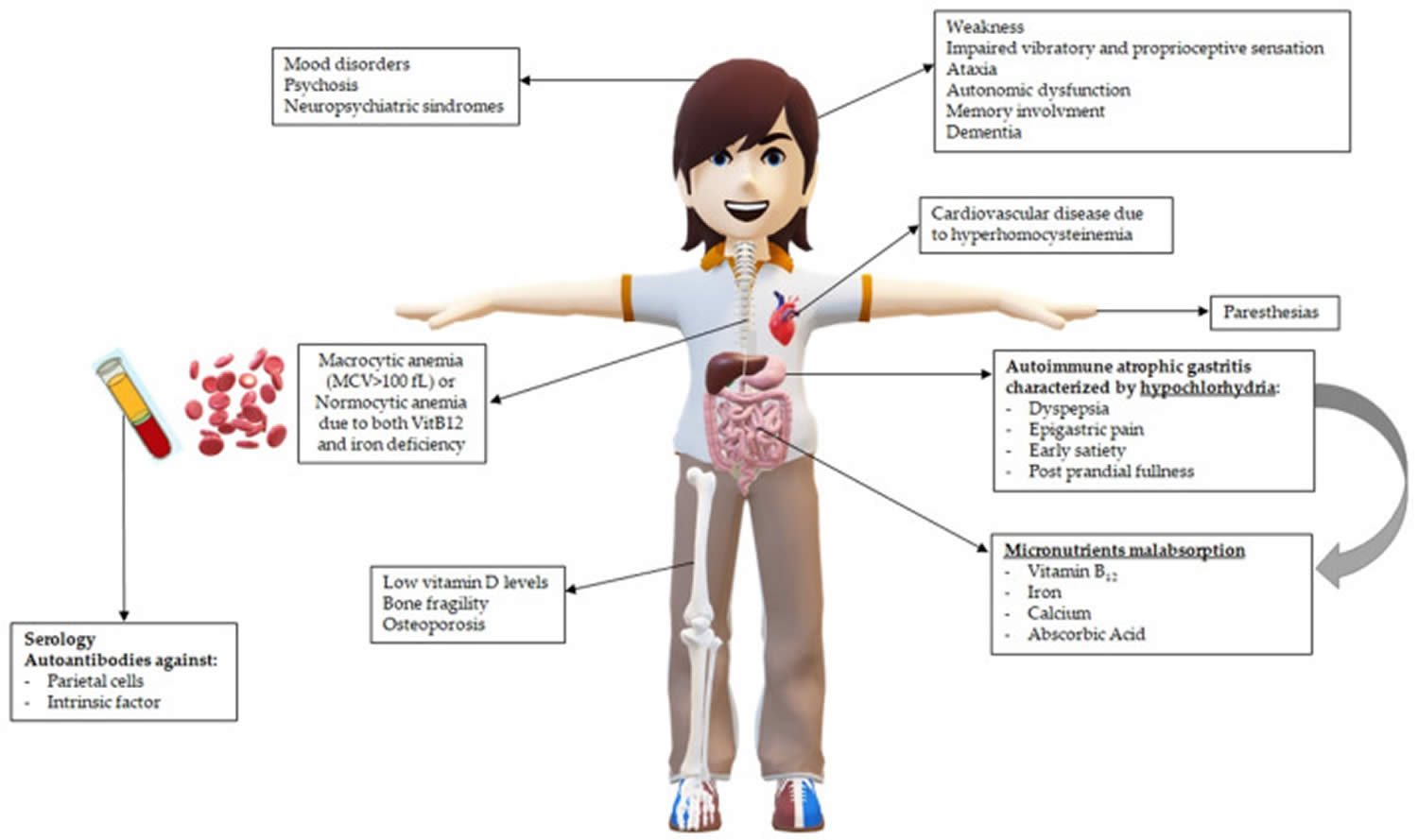
The most common cause of vitamin B12 deficiency is autoimmune pernicious anemia, a condition that carries an increased risk of gastric cancer. In pernicious anemia, absorption is impaired due to intrinsic factor deficiency arising from autoimmune destruction of parietal cells 23. Other common causes of vitamin B12 deficiency include gastrectomy, ileal resection, pancreatic insufficiency, and malabsorption syndromes including Crohn’s disease and celiac disease. Other less common causes of vitamin B12 deficiency include use of medications such as biguanides (metformin), antacids (proton pump inhibitors and H2 receptors antagonists), aminoglycoside, antibiotics and colchicines, and rarely, malabsorption due to gastrointestinal bacterial overgrowth, congenital defects (e.g. birth transcobalamin deficiency), and infestation 13. Pure nutritional deficiency is rare and usually occurs only in strict vegans 24. Because people who have difficulty absorbing vitamin B12 from food absorb free vitamin B12 normally, their vitamin B12 deficiency tends to be less severe than that of individuals with pernicious anemia, who cannot absorb either food-bound or free vitamin B12. It is recommended that vegetarians and vegans take vitamin B12 supplements to prevent vitamin B12 deficiency 25. Certain congenital conditions, such as hereditary intrinsic factor defects and congenital vitamin B12 malabsorption (Imerslund-Gräsbeck disease), can also cause severe vitamin B12 deficiency 15. In some cases, vitamin B12 deficiency can be a risk factor for cardiovascular disease 26.
In the United States and the United Kingdom, the prevalence of vitamin B12 deficiency is approximately 6% in persons younger than 60 years, and nearly 20% in those older than 60 years 27, 28. Latin American countries have a clinical or subclinical B12 deficiency rate of approximately 40% 12. The prevalence is 70% in Kenyan school children, 80% in East Indian preschool-aged children, and 70% in East Indian adults 12. Pawlak 29 examined the prevalence of vitamin B12 deficiency among individuals adhering to vegetarian diets. The reviewed studies show relatively high vitamin B12 deficiency prevalence among vegetarians. Vitamin B12 deficiency in infants is about 45%, among the children and adolescents ranging from 0% to 33.3%, and among pregnant women ranging from 17% to 39%, dependent on the trimester 29. Adults and elderly individuals had a deficiency range of 0 to 86.5% 29. Higher vitamin B12 deficiency prevalence was reported in vegans than in other vegetarians, while B12 deficiency prevalence of 0% was reported among vegans who consumed vitamin B12-fortified foods, highlighting that vitamin B12 supplements to ensure adequate vitamin B12 intake should be considered in these individuals 10.
Certain risk factors increase the prevalence of vitamin B12 deficiency (see Table 1) 30. Dietary insufficiency, pernicious anemia (i.e., an autoimmune process that reduces available intrinsic factor and subsequent absorption of vitamin B12) 12 and long-term use of metformin or stomach acid-suppressing medications have been implicated in B12 deficiency 31, 32. A multicenter randomized controlled trial of 390 patients with diabetes mellitus showed that those taking 850 mg of metformin three times per day had an increased risk of vitamin B12 deficiency (number needed to harm = 14 per 4.3 years) and low vitamin B12 levels (number needed to harm = 9 per 4.3 years) vs. placebo 31. This effect increased with duration of metformin therapy, and patients had an unclear prophylactic supplementation response 31. A case-control study that compared 25,956 patients who had vitamin B12 deficiency with 184,199 control patients found a significantly increased risk of vitamin B12 deficiency in patients who had taken proton pump inhibitors or histamine H2 blockers for at least two years 32. In light of these findings, long-term use of these medications should be periodically reassessed, particularly in patients with other risk factors for vitamin B12 deficiency 31, 32.
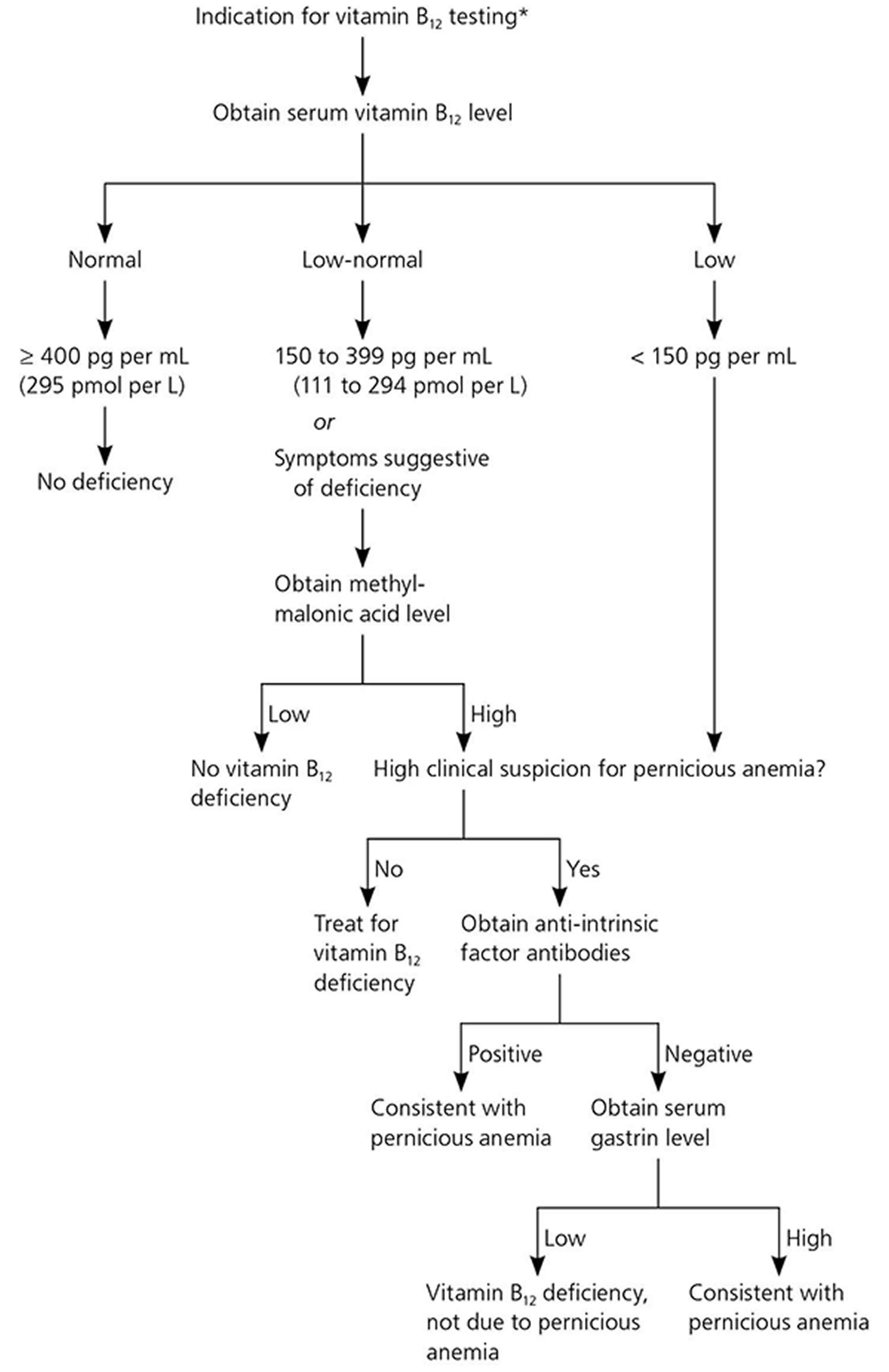
Screening persons at average risk of vitamin B12 deficiency is not recommended 13. Screening for vitamin B12 deficiency should be considered in patients with risk factors, and diagnostic testing for vitamin B12 deficiency should be considered in those with suspected clinical signs and symptoms of vitamin B12 deficiency 33, 12, 34.
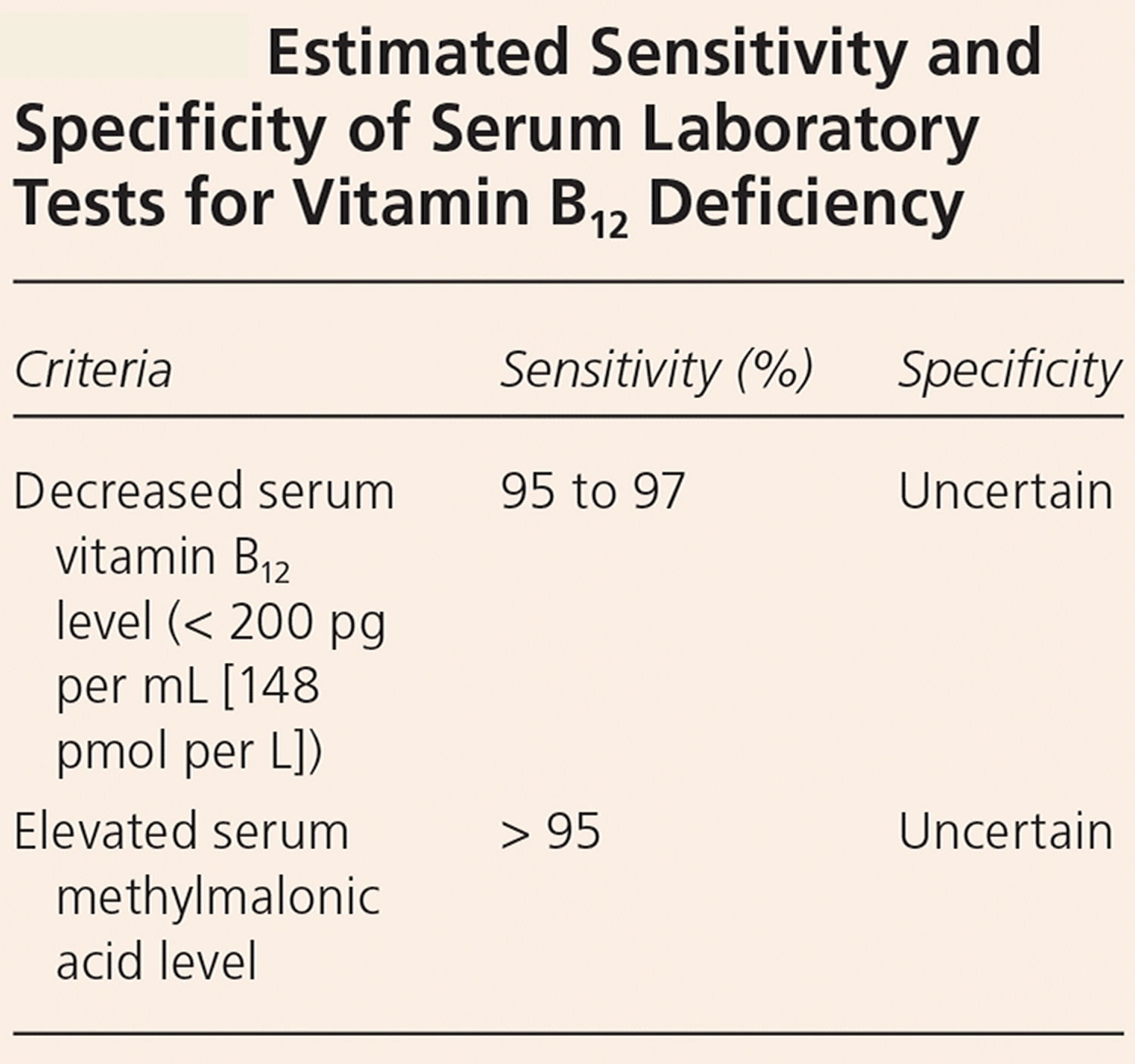
The recommended laboratory evaluation for patients with suspected vitamin B12 deficiency includes a complete blood count (CBC) and serum vitamin B12 level 33, 35. A level of less than 150 pg per mL (111 pmol per L) is diagnostic for deficiency 33, 12. Serum vitamin B12 levels may be artificially elevated in patients with alcoholism, liver disease, or cancer because of decreased liver clearance of transport proteins and resultant higher circulating levels of vitamin B12; physicians should use caution when interpreting laboratory results in these patients 36, 37. In patients with a normal or low-normal serum vitamin B12 level, complete blood count results demonstrating macrocytosis, or suspected clinical manifestations, a serum methylmalonic acid (MMA) level is an appropriate next step 38 and is a more direct measure of vitamin B12’s physiologic activity 33, 12. Although not clinically validated or available for widespread use, measurement of holotranscobalamin, the metabolically active form of vitamin B12, is an emerging method of detecting deficiency 13.
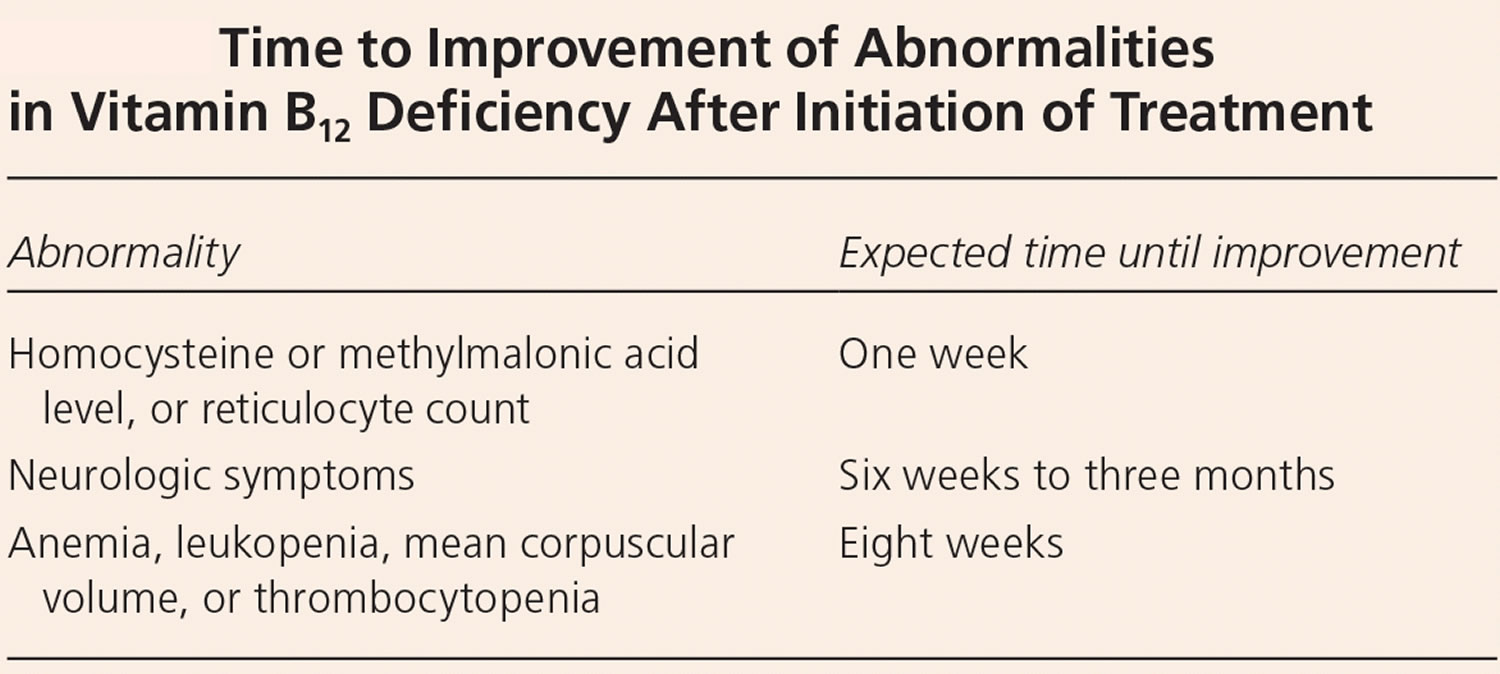
Typically, vitamin B12 deficiency is treated with intramuscular injections of cyanocobalamin or hydroxocobalamin, because this method bypasses any barriers to absorption. Hydroxocobalamin is usually the recommended option as it stays in the body for longer. Approximately 10% of the standard injectable dose of 1 mg is absorbed, which allows for rapid replacement in patients with severe deficiency or severe neurologic symptoms 15. Guidelines from the British Society for Haematology recommend injections three times per week for two weeks in patients without neurologic deficits 38. If neurologic deficits are present, injections should be given every other day for up to three weeks or until no further improvement is noted.
However, high doses of oral vitamin B12 might also be effective 39. A 2018 Cochrane review included three randomized controlled trials (RCTs) that compared very high doses (1,000–2,000 mcg) of oral with intramuscular vitamin B12 for vitamin B12 deficiency in a total of 153 participants 23. The evidence from these studies, although of low quality, showed that the ability of high oral doses of vitamin B12 supplements to normalize serum vitamin B12 was similar to that of intramuscular vitamin B12. The British Society for Haematology recommends intramuscular vitamin B12 for severe deficiency and malabsorption syndromes, whereas oral replacement may be considered for patients with asymptomatic, mild disease with no absorption or compliance concerns 38.
If vitamin B12 deficiency coexists with folate deficiency, vitamin B12 should be replaced first to prevent subacute combined degeneration of the spinal cord 12.
The British Society for Haematology does not recommend retesting vitamin B12 levels after treatment has been initiated, and no guidelines address the optimal interval for screening high-risk patients 38. In general, patients with an irreversible cause should be treated indefinitely, whereas those with a reversible cause should be treated until the deficiency is corrected and symptoms resolve 12.
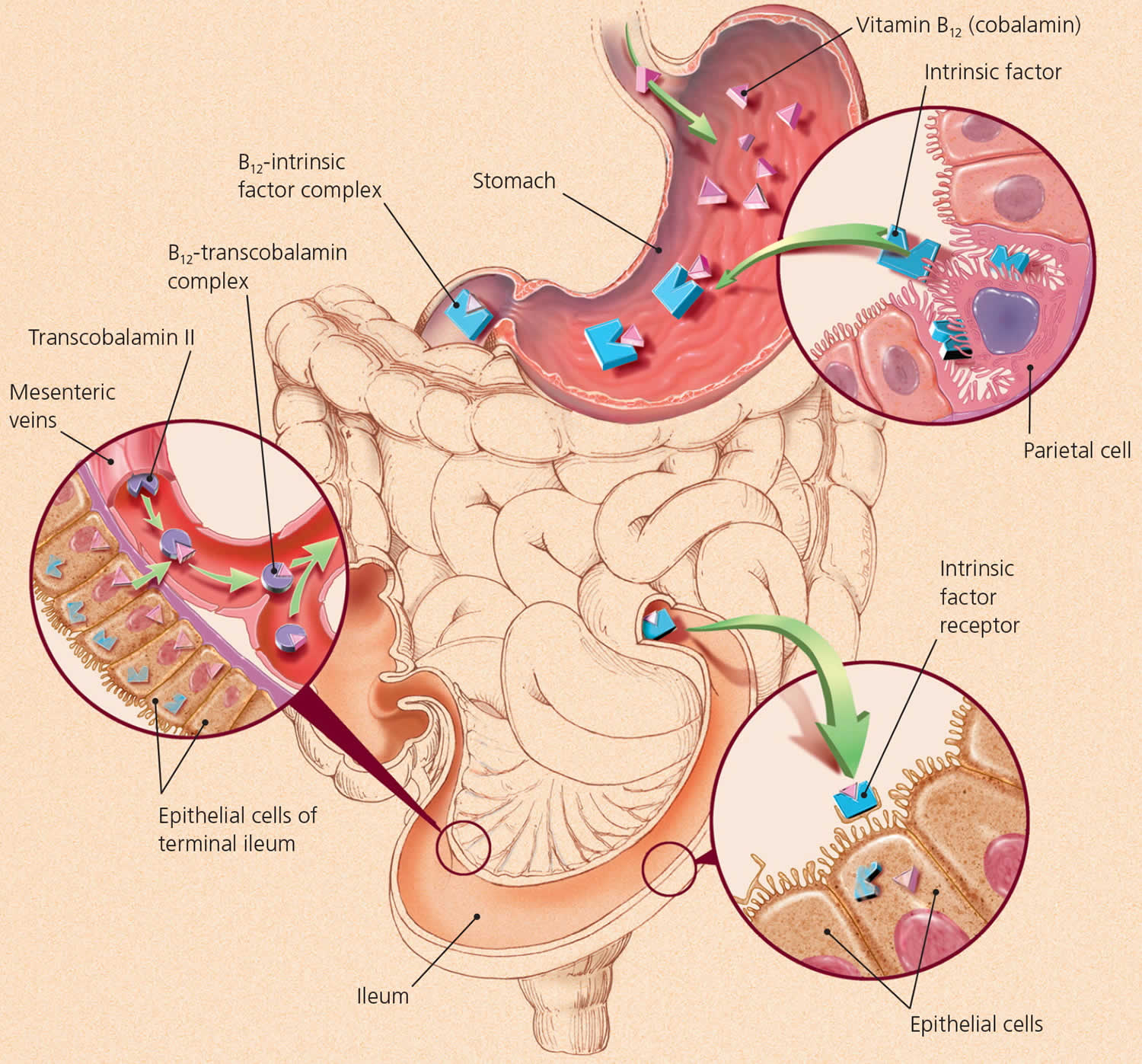
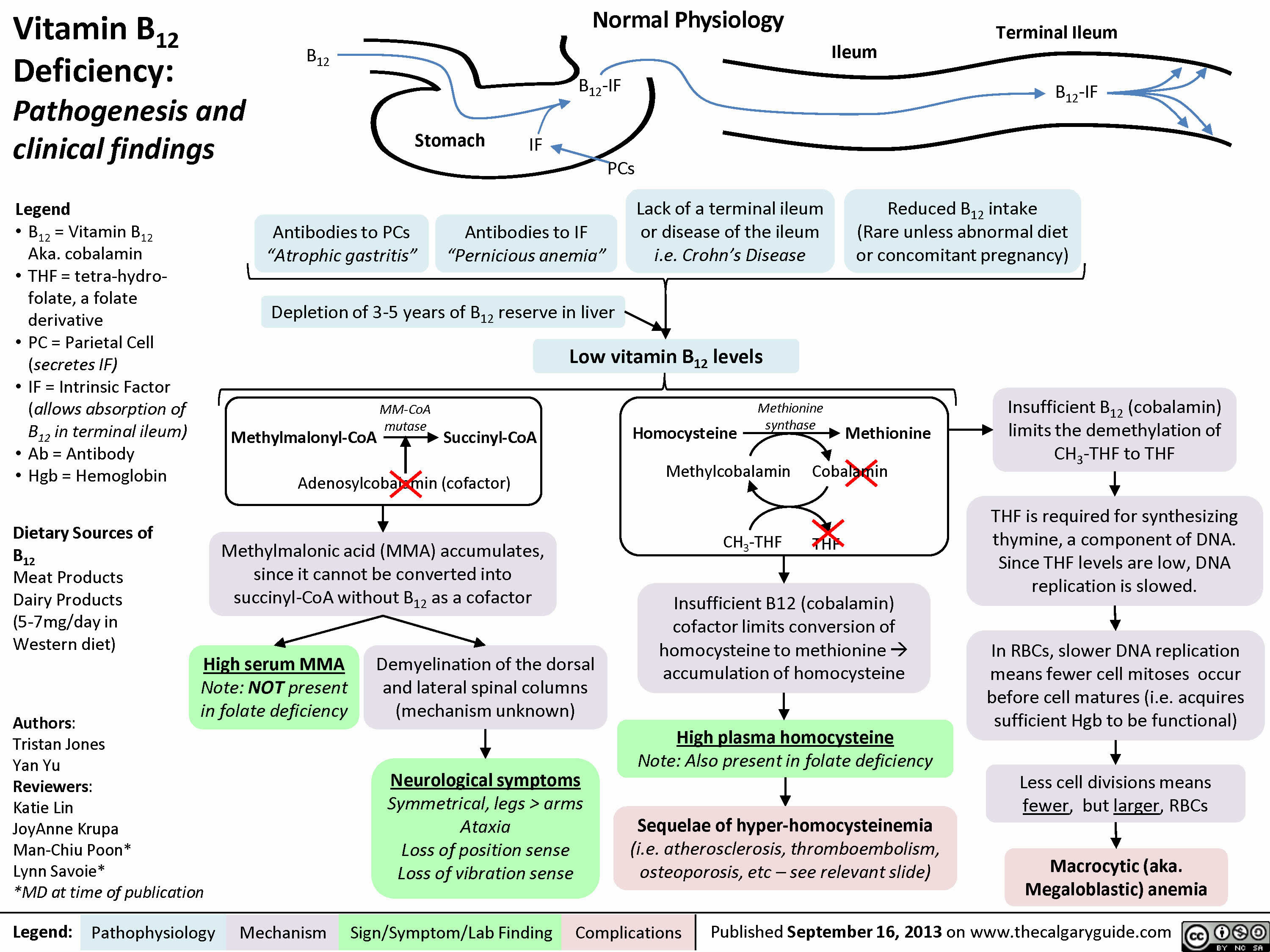
Figure 1. Vitamin B12 absorption and transport
Figure 2. Vitamin B12 deficiency pathophysiology
Figure 3. Glossitis secondary to vitamin B12 deficiency anemia
Footnotes: (A) Generalized dryness of the tongue of a 61-year-old woman with vitamin B12 deficiency, with atrophy (blue arrowheads) and erythematous plaques (white arrowheads). (B) Normal appearance of the tongue 3 days after the patient received a single injection of vitamin B12.
[Source 41 ]Table 1. Risk factors for vitamin B12 deficiency
[Source 13 ]Table 2. Clinical and laboratory findings in vitamin B12 deficiency
| General symptoms | Weight loss observed in most patients |
| Low-grade fever occurs in one third of newly diagnosed patients and promptly disappears with treatment | |
| Gastrointestinal symptoms | Smooth tongue (50% of patients) with loss of papillae. Changes in taste and loss of appetite |
| Patients may report either constipation or having several semi-solid bowel movements daily | |
| Anorexia, nausea, vomiting, heartburn, pyrosis, flatulence and a sense of fullness | |
| Brain | Altered mental status. Cognitive defects (“megaloblastic madness”): depression, mania, irritability, paranoia, delusions, lability |
| Sensory organs | Optic atrophy, anosmia, loss of taste, glossitis |
| Bone marrow | Hypercellular bone marrow |
| Increased erythroid precursors | |
| Open, immature nuclear chromatin | |
| Dyssynchrony between maturation of cytoplasm and nuclei | |
| Giant bands, metamyelocytes | |
| Karyorrhexis, dysplasia | |
| Abnormal results on flow cytometry and cytogenetic analysis | |
| Spinal cord | Myelopathy |
| Spongy degeneration | |
| Paresthesias | |
| Loss of proprioception: vibration, position, ataxic gait, limb weakness/spasticity (hyperreflexia) | |
| Positive Romberg sign | |
| Lhermitte’s sign | |
| Segmental cutaneous sensory level | |
| Autonomic nervous system | Postural hypotension |
| Incontinence | |
| Impotence | |
| Peripheral nervous system | Cutaneous sensory loss |
| Hyporeflexia symmetric weakness | |
| Paresthesias | |
| Genitourinary symptoms | Urinary retention and impaired micturition may occur because of spinal cord damage. This can predispose patients to urinary tract infections |
| Reproductive system | Infertility |
| Abnormalities in infants and children | Developmental delay or regression, permanent disability |
| The patient does not smile | |
| Feeding difficulties | |
| Hypotonia, lethargy, coma | |
| Hyperirritability, convulsions, tremors, myoclonus | |
| Microcephaly | |
| Choreoathetoid movements, peripheral blood | |
| Macrocytic red cells, macro-ovalocytes | |
| Anisocytosis, fragmented forms | |
| Hypersegmented neutrophils | |
| Leukopenia, possible immature white cells | |
| Thrombocytopenia | |
| Pancytopenia | |
| Elevated lactate dehydrogenase level (extremes possible) | |
| Elevated indirect bilirubin and aspartate aminotransferase levels | |
| Decreased haptoglobin level | |
| Elevated levels of methylmalonic acid, homocysteine, or both |
Folic Acid and Vitamin B12 Deficiency
Large amounts of folic acid can mask the damaging effects of Vitamin B-12 deficiency by correcting the megaloblastic anemia caused by Vitamin B-12 deficiency 2, 4 without correcting the neurological damage that also occurs 1, 43. Moreover, preliminary evidence suggests that high serum folate levels might not only mask Vitamin B-12 deficiency, but could also exacerbate the anemia and worsen the cognitive symptoms associated with Vitamin B-12 deficiency 44, 45. Permanent nerve damage can occur if Vitamin B-12 deficiency is not treated. For these reasons, folic acid intake from fortified food and supplements should not exceed 1,000 mcg daily in healthy adults 4.
What is vitamin B12?
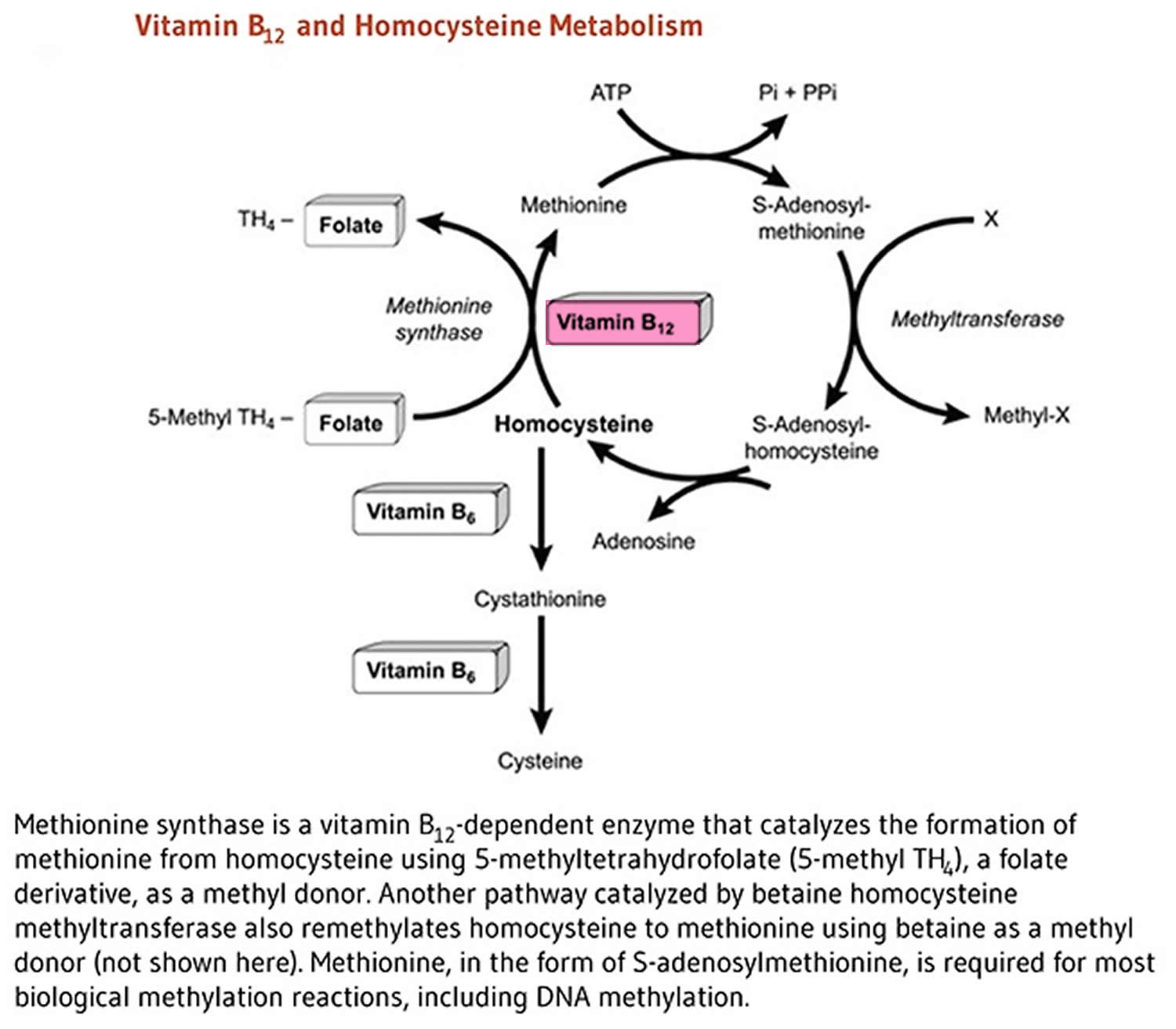
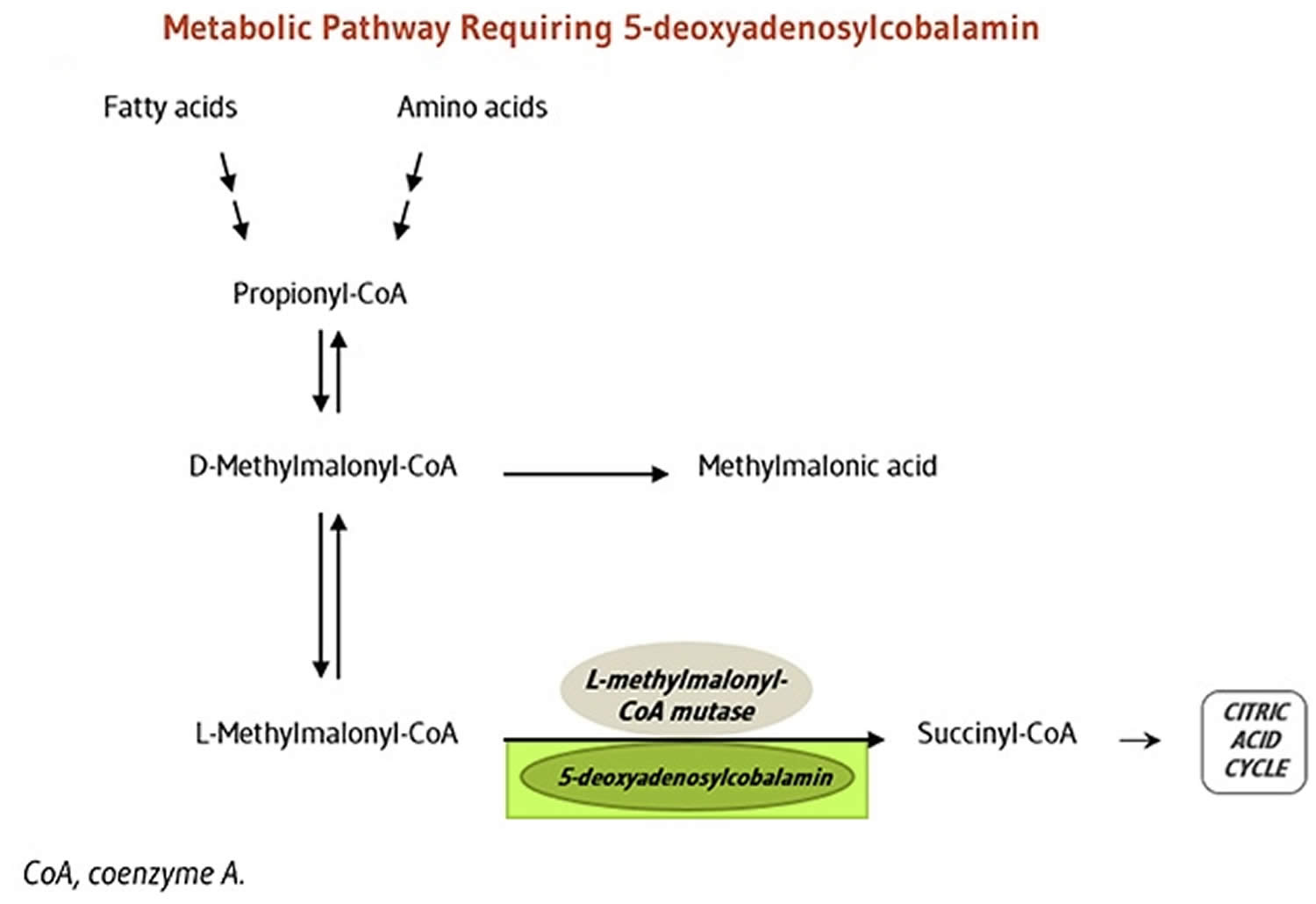
Vitamin B12 is also known as cobalamin or cyanocobalamin (man-made form of vitamin B12), is a nutrient that helps keep your body’s nerve and blood cells healthy and helps make DNA, the genetic material in all cells. Vitamin B-12 is a water-soluble vitamin that is naturally present in some foods, added to others, and available as a dietary supplement and a prescription medication. Vitamin B12 has the largest and most complex chemical structure of all the vitamins. Vitamin B12 is unique among vitamins in that it contains a metal ion, cobalt 46, 1, 47, 2, 48. For this reason cobalamin is the term used to refer to compounds having vitamin B12 activity 46. Methylcobalamin and adenosylcobalamin (5-deoxyadenosylcobalamin) are the two forms of “active” vitamin B12 used by your body 49, 50, 51. The form of cobalamin used in most nutritional supplements and fortified foods, cyanocobalamin (man-made form of vitamin B12), is readily converted to adenosylcobalamin (5-deoxyadenosylcobalamin) and methylcobalamin in your body. In mammals, vitamin B-12 is a cofactor for only two enzymes, methionine synthase and L-methylmalonyl-coenzyme A mutase 52, 53. Methionine synthase catalyzes the conversion of homocysteine to methionine 51, 7. Methionine is required for the formation of S-adenosylmethionine, a universal methyl donor for almost 100 different substrates, including DNA, RNA, hormones, proteins, and lipids. L-methylmalonyl-CoA mutase converts L-methylmalonyl-CoA to succinyl-CoA in the degradation of propionate 2, 51, 7, an essential biochemical reaction in fat and protein metabolism. Succinyl-CoA is also required for hemoglobin synthesis.
Vitamin B12 is required for the development, myelination, and function of the central nervous system; healthy red blood cell formation; and DNA synthesis 1, 47, 2, 48, 51.
Large amounts of Vitamin B-12 seem to be nontoxic but are not recommended for regular use (ie, as a general tonic). The Recommended Dietary Allowance (RDA) for vitamin B12 is 2.4 micrograms per day (μg/day) for adolescents and adults. It is slightly higher for women who are pregnant (2.6 mcg/day) or breastfeeding (2.8 mcg/day) 46. The Food and Nutrition Board at the National Academies of Sciences, Engineering, and Medicine did not establish a Tolerable Upper Intake Level (maximum daily intake unlikely to cause adverse health effects) for vitamin B12 because of its low potential for toxicity 51. Even at large doses, vitamin B12 is generally considered to be safe because your body does not store excess amounts 39.
Vitamin B-12 also helps prevent a type of anemia called megaloblastic anemia that makes people tired and weak. Your body cannot make vitamin B12. Vitamin B-12 is synthesized only by bacteria. While present in animal products, including meats, fish, shellfish, dairy products, and eggs, it is absent in plant-based foods. People most at risk for vitamin B12 deficiency are vegans, as diets devoid of animal products will result in B12 deficiency. However, vitamin B12 issues can be caused by taking some types of stomach acid blockers. Also, some people have an autoimmune or inflammatory condition of the stomach wall that degrade the proteins that aid vitamin B12 absorption.
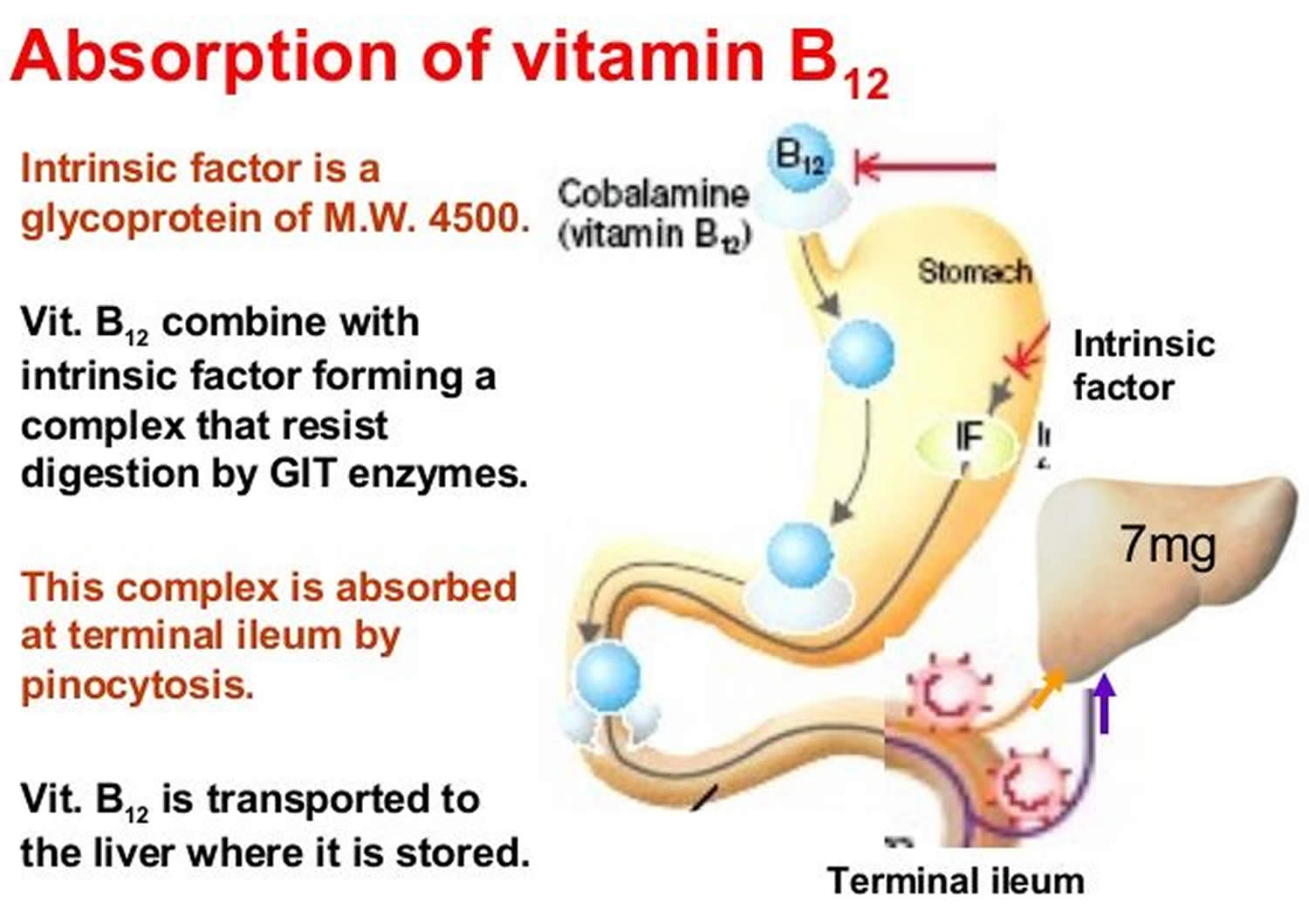
Two steps are required for your body to absorb Vitamin B-12 from food.
- First, food-bound Vitamin B-12 is released in the stomach’s acid environment (hydrochloric acid and and gastric protease in the stomach separate Vitamin B-12 from the protein to which Vitamin B-12 is attached in food) and is bound to R protein (haptocorrin) 51. Approximately 1.2% of vitamin B12 is absorbed passively without the help of intrinsic factor (IF) 54. When synthetic Vitamin B-12 is added to fortified foods and dietary supplements, it is already in free form and thus, does not require this separation step. If a patient receives the oral formulation of cobalamin at high doses, this passive absorption is sufficient to replenish vitamin B12 deficiency (a lack of vitamin B12). If intrinsic factor (IF) is present in an adequate amount, then oral cobalamin is absorbed with the help of intrinsic factor (IF). When administering cobalamin parenterally, it bypasses the intestinal barrier, absorbs quickly by diffusion, and enters into the systemic circulation 23.
- Second, pancreatic enzymes cleave this B12 complex (B12-R protein) in the small intestine. After cleavage, intrinsic factor (IF), a protein secreted by parietal cells situated in the mucosa of your stomach, binds with the free Vitamin B-12. Intrinsic factor is required for absorption of Vitamin B-12, which takes place in the terminal ileum 51, 55. Intrinsic factor (IF) binds to vitamin B12 and the complex is transported across the cell membrane bound to another glycoprotein called transcobalamin 23. Approximately 56% of a 1 mcg oral dose of Vitamin B-12 is absorbed, but absorption decreases drastically when the capacity of intrinsic factor is exceeded (at 1–2 mcg of Vitamin B-12) 9. Some people have pernicious anemia, a condition where they cannot make intrinsic factor (IF). As a result, they have trouble absorbing Vitamin B-12 from all foods and dietary supplements.
Pernicious anemia is an autoimmune disease that affects the gastric mucosa and results in gastric atrophy. This leads to the destruction of parietal cells, achlorhydria, and failure to produce intrinsic factor, resulting in Vitamin B-12 malabsorption 2, 51, 56, 57, 58. If pernicious anemia is left untreated, it causes vitamin B-12 deficiency (a lack of vitamin B12), leading to megaloblastic anemia and neurological disorders, even in the presence of adequate dietary intake of vitamin B-12. Pernicious anemia can cause fatigue, weakness, constipation, loss of appetite, and weight loss. Numbness and tingling in the hands and feet, depression, confusion, or poor memory can also occur. Symptoms of vitamin B12 deficiency can take decades to develop, and can usually only be diagnosed by a medical professional. For more details see below – Groups at Risk of Vitamin B12 deficiency.
In the blood plasma, Vitamin B-12 is bound to transcobalamins 1 and 2 59. Transcobalamin 2 is responsible for delivering Vitamin B-12 to tissues. The liver stores large amounts of Vitamin B-12. Enterohepatic reabsorption helps retain Vitamin B-12. Liver Vitamin B-12 stores can normally sustain physiologic needs for 3 to 5 years if B12 intake stops (eg, in people who become vegans) and for months to 1 year if enterohepatic reabsorption capacity is absent.
In healthy adults, vitamin B12 deficiency is uncommon, mainly because total body stores can exceed 2,500 mcg, daily turnover is slow, and dietary intake of only 2.4 mcg/day is sufficient to maintain adequate vitamin B12 status 9. In elderly individuals, vitamin B12 deficiency is more common mainly because of impaired intestinal absorption that can result in marginal to severe vitamin B12 deficiency in this population.
Vitamin B12 status is typically assessed by measurements of serum or plasma vitamin B12 levels 39. The cutoff between normal vitamin B12 levels and vitamin B12 deficiency varies by method and laboratory, but most laboratories define subnormal serum or plasma values as those lower than 200 or 250 pg/mL (148 or 185 pmol/L) 14. Levels of serum methylmalonic acid (MMA), a vitamin B12-associated metabolite, are the most sensitive markers of vitamin B12 status, and an methylmalonic acid (MMA) level greater than 0.271 micromol/L suggests vitamin B12 deficiency 60, 13, 61. However, MMA levels also rise with kidney failure and tend to be higher in older adults 60, 21, 62. Another marker is total plasma homocysteine levels, which rise quickly as vitamin B12 status declines; a serum homocysteine level higher than 15 micromol/L, for example, suggests vitamin B12 deficiency 20. However, this indicator has poor specificity because it is influenced by other factors, such as low folate levels and, especially, by declines in kidney function 60. Experts suggest that if a patient’s serum vitamin B12 level is less than 150 pg/ml (111 pmol/L), the patient’s serum methylmalonic acid (MMA) levels should be checked to confirm a diagnosis of vitamin B12 deficiency 13, 21.
Vitamin B12 key points
- Vitamin B12 or cobalamin plays essential roles in folate metabolism and in the synthesis of the citric acid cycle intermediate, succinyl-CoA.
- Vitamin B12 deficiency is commonly associated with chronic stomach inflammation, which may contribute to an autoimmune vitamin B12 malabsorption syndrome called pernicious anemia and to a food-bound vitamin B12 malabsorption syndrome. Impairment of vitamin B12 absorption can cause megaloblastic anemia and neurologic disorders in deficient subjects.
- Normal function of the digestive system required for food-bound vitamin B12 absorption is commonly impaired in individuals over 60 years of age, placing them at risk for vitamin B12 deficiency.
- Vitamin B12 and folate are important for homocysteine metabolism. Elevated homocysteine levels in blood are a risk factor for cardiovascular disease. Although B vitamin supplementation has been proven effective to control homocysteine levels, current data from intervention trials have not shown that lowering homocysteine levels decreases cardiovascular disease risk.
- The preservation of DNA integrity is dependent on folate and vitamin B12 availability. Poor vitamin B12 status has been linked to increased risk of breast cancer in some, but not all, observational studies. There is a need to evaluate whether supplemental vitamin B12, along with folic acid, could help reduce breast cancer incidence.
- Low maternal vitamin B12 status has been associated with an increased risk of neural tube defects, but it is not known whether vitamin B12 supplementation could help reduce the risk of neural tube defects.
- Vitamin B12 is essential for the preservation of the myelin sheath around neurons and for the synthesis of neurotransmitters. While hyperhomocysteinemia may increase the risk of cognitive impairment, it is not clear whether vitamin B12 deficiency contributes to the risk of dementia in the elderly. Although B-vitamin supplementation lowers homocysteine levels in older subjects, the long-term benefit is not yet known.
- Both depression and osteoporosis have been linked to diminished vitamin B12 status and high homocysteine levels.
- Products of animal origin constitute the primary source of vitamin B12. Older individuals and vegans are advised to use vitamin B12 fortified foods and supplements to meet their needs.
- The long-term use of certain medications, such as inhibitors of stomach acid secretion, can adversely affect vitamin B12 absorption.
What does vitamin B12 do?
Vitamin B12 is required for the development, myelination, and function of the central nervous system; healthy red blood cell formation; and helps make DNA, the genetic material in all cells 15, 63. Vitamin B12 functions as a cofactor for two enzymes, methionine synthase and L-methylmalonyl-CoA mutase (see more below) 15, 14, 64. Methionine synthase catalyzes the conversion of homocysteine to the essential amino acid methionine 65, 14. Methionine is required for the formation of S-adenosylmethionine, a universal methyl donor for almost 100 different substrates, including DNA, RNA, proteins, and lipids 15, 64. L-methylmalonyl-CoA mutase converts L-methylmalonyl-CoA to succinyl-CoA in the metabolism of propionate, a short-chain fatty acid 14.
Vitamin B12 functions as a cofactor for methionine synthase
Methylcobalamin is required for the function of the folate-dependent enzyme, methionine synthase. The methionine synthase enzyme is required for the synthesis of the amino acid, methionine, from homocysteine. Methionine in turn is required for the synthesis of S-adenosylmethionine (SAMe), a methyl group donor used in many biological methylation reactions, including the methylation of a number of sites within DNA, RNA, and proteins 66. Aberrant methylation of DNA and proteins, which causes alterations in chromatin structure and gene expression, are a common feature of cancer cells. Inadequate function of methionine synthase can lead to an accumulation of homocysteine, which has been associated with increased risk of cardiovascular disease (Figure 4).
Figure 4. Vitamin B12 functions as a cofactor for methionine synthase
[Source 46 ]Vitamin B12 functions as a cofactor for L-methylmalonyl-coenzyme A mutase
5-Deoxyadenosylcobalamin is required by the enzyme that catalyzes the conversion of L-methylmalonyl-coenzyme A to succinyl-coenzyme A (succinyl-CoA), which then enters the citric acid cycle (Figure 5). Succinyl-CoA plays an important role in the production of energy from lipids and proteins and is also required for the synthesis of hemoglobin, the oxygen-carrying pigment in red blood cells 66.
Figure 5. Vitamin B12 functions as a cofactor for L-methylmalonyl-coenzyme A mutase
[Source 46 ]How much Vitamin B-12 do you need?
The amount of Vitamin B-12 you need each day depends on your age. Average daily recommended amounts for different ages are listed below in micrograms (mcg). Table 3 lists the current Recommended Dietary Allowance (RDA) for Vitamin B-12 in micrograms (mcg). For infants aged 0 to 12 months, the Food and Nutrition Board established an adequate intake (AI) for vitamin B-12 that is equivalent to the mean intake of Vitamin B-12 in healthy, breastfed infants.
- Recommended Dietary Allowance (RDA): average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals.
- Adequate Intake (AI): established when evidence is insufficient to develop an RDA and is set at a level assumed to ensure nutritional adequacy.
Table 3. Vitamin B-12 Recommended Intake
| Life Stage | Recommended Amount |
|---|---|
| Birth to 6 months | 0.4 mcg |
| Infants 7–12 months | 0.5 mcg |
| Children 1–3 years | 0.9 mcg |
| Children 4–8 years | 1.2 mcg |
| Children 9–13 years | 1.8 mcg |
| Teens 14–18 years | 2.4 mcg |
| Adults | 2.4 mcg |
| Pregnant teens and women | 2.6 mcg |
| Breastfeeding teens and women | 2.8 mcg |
What are food sources of vitamin B12?
Vitamin B12 is found naturally in a wide variety of foods of animal origin (such as fish, meat, poultry, eggs, and dairy products) and manufacturers add it to some fortified foods (e.g., fortified breakfast cereals and fortified nutritional yeasts) 15. Plant foods have no vitamin B12 unless they are fortified 68. You can get recommended amounts of vitamin B12 by eating a variety of foods including the following:
- Fish, meat, poultry, eggs, milk, and other dairy products contain vitamin B12.
- Clams and beef liver are some of the best source of vitamin B12.
- Some breakfast cereals, nutritional yeasts, and other food products are fortified with vitamin B12.
The U.S. Department of Agriculture’s FoodData Central (https://fdc.nal.usda.gov) lists the nutrient content of many foods and provides a comprehensive list of foods containing vitamin B12 arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/VitaminB12-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/VitaminB12-Food.pdf).
The average vitamin B12 level in the breast milk of women with vitamin B12 intakes above the RDA is 0.44 mcg/L 69. The U.S. Food and Drug Administration (FDA) specifies that infant formulas sold in the United States must provide at least 0.15 mcg vitamin B12 per 100 kcal 70.
The estimated bioavailability of vitamin B12 from food varies by vitamin B12 dose because absorption decreases drastically when the capacity of intrinsic factor is exceeded (at 1–2 mcg of vitamin B12) 71. Bioavailability also varies by type of food source. For example, the bioavailability of vitamin B12 appears to be about three times higher in dairy products than in meat, fish, and poultry, and the bioavailability of vitamin B12 from dietary supplements is about 50% higher than that from food sources 72.
A variety of foods and their vitamin B12 levels per serving are listed in Table 4.
Table 4. Vitamin B12 Food Sources
| Food | Micrograms per serving | Percent DV* |
| Beef liver, cooked, pan-fried, 3 ounces | 70.7 | 2944 |
| Clams (without shells), cooked, 3 ounces | 17 | 708 |
| Tuna, bluefin, cooked, dry heat, 3 ounces | 9.3 | 385 |
| Nutritional yeast, fortified, from several brands (check label), about ¼ cup | 8.3 to 24 | 346 to 1,000 |
| Salmon, Atlantic, cooked, 3 ounces | 2.6 | 108 |
| Beef, ground, 85% lean meat/15% fat, pan-browned, 3 ounces | 2.4 | 100 |
| Milk, 2% milkfat, 1 cup | 1.3 | 54 |
| Yogurt, plain, fat free, 6-ounce container | 1 | 43 |
| Breakfast cereals, fortified with 25% of the DV for vitamin B12, 1 serving | 0.6 | 25 |
| Cheese, cheddar, 1½ ounces | 0.5 | 19 |
| Egg, whole, cooked, 1 large | 0.5 | 19 |
| Turkey, breast meat, roasted, 3 ounces | 0.3 | 14 |
| Tempeh, 1/2 cup | 0.1 | 3 |
| Banana, 1 medium | 0 | 0 |
| Bread, whole-wheat, 1 slice | 0 | 0 |
| Strawberries, raw, halved, 1/2 cup | 0 | 0 |
| Beans, kidney, boiled, 1/2 cup | 0 | 0 |
| Spinach, boiled, drained, 1/2 cup | 0 | 0 |
Footnote: *DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration (FDA) to help consumers determine the level of various nutrients in a standard serving of food in relation to their approximate requirement for it. The DV for Vitamin B-12 is 6.0 mcg. However, the FDA does not require food labels to list Vitamin B-12 content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 73 ]Who are at risk of vitamin B12 deficiency?
The following people are among those most likely to be vitamin B12 deficient.
Older adults
Depending on the definition used, between 3% and 43% of community-dwelling older adults, especially those with atrophic gastritis (chronic inflammation and thinning of your stomach), have vitamin B12 deficiency based on serum vitamin B12 levels 74, 75. The vitamin B12 deficiency rate at a cutoff of less than 211 mcg/L (156 pmol/L) at admission to a long-term care facility, according to one study, was 14%, and 38% of these older adults had levels lower than 407 pg/mL (300 pmol/L) 75.
Conditions associated with vitamin B12 deficiency include pernicious anemia, present in about 15% to 25% of older adults with vitamin B12 deficiency 42. Atrophic gastritis, an autoimmune condition affecting 2% of the general population but 8–9% of adults aged 65 and older, decreases production of intrinsic factor and secretion of hydrochloric acid in the stomach and thus decreases absorption of vitamin B12 42, 76. A third condition associated with vitamin B12 deficiency in older adults is Helicobacter pylori infection, possibly because this bacterium causes inflammation that leads to malabsorption of vitamin B12 from food 77.
Individuals with pernicious anemia
Pernicious anemia is an irreversible autoimmune disease that affects the gastric mucosa and results in gastric atrophy 78. This disease leads to attacks on parietal cells in the stomach, resulting in failure to produce intrinsic factor (IF) and malabsorption of dietary vitamin B12, recycled biliary vitamin B12, and free vitamin B12 79, 60. Therefore, without treatment, pernicious anemia causes vitamin B12 deficiency, even in the presence of adequate vitamin B12 intakes.
Pernicious anemia is the most common cause of clinically evident vitamin B12 deficiency around the world 79, 78. The incidence of pernicious anemia in the United States is an estimated 151 per 100,000, and this condition is more common in women and in people of European ancestry 78.
Individuals with gastrointestinal disorders
Individuals with stomach and small intestine disorders, such as celiac disease and Crohn’s disease, may be unable to absorb enough vitamin B12 from food to maintain healthy body stores 80. But although rates of vitamin B12 deficiency are higher in people with celiac disease than other people 81, the evidence for whether rates of vitamin B12 deficiency are higher in people with Crohn’s disease is mixed 82, 83. Vitamin B12 deficiency in people with Crohn’s disease is typically treated with intramuscular cobalamin injections, but high doses of oral cyanocobalamin therapy (e.g., 1,000 mcg/day) might be equally effective 84.
Individuals who have had gastrointestinal surgery
Surgical procedures in the gastrointestinal tract, such as for weight loss (bariatric surgery) or to remove all or part of the stomach (gastrectomy), can cause a complete or partial loss of cells that secrete hydrochloric acid and cells that secrete intrinsic factor (IF) 85, 86. Thus, these procedures reduce the amount of vitamin B12, particularly food-bound vitamin B12, that the body absorbs 85, 86. High doses (1,000 mcg/day) of oral methylcobalamin supplements appear to be as effective as hydroxycobalamin injections in normalizing vitamin B12 values in patients who have undergone Roux-en-Y gastric bypass surgery 87.
Vegetarians
Vegans who consume no animal products and vegetarians who consume some animal products (e.g., dairy products, eggs, or both) but not meat have a higher risk of developing vitamin B12 deficiency because natural food sources of vitamin B12 are limited to animal foods 88. Consumption of foods fortified with vitamin B12 (such as fortified nutritional yeasts) as well as vitamin B12 supplements can substantially reduce the risk of deficiency 88.
Infants of vegan women
Exclusively breastfed infants of women who consume no animal products might have very limited reserves of vitamin B12 and can develop vitamin B12 deficiency, sometimes very early in life 89. The infant’s vitamin B12 deficiency can be severe, especially if the mother’s vitamin B12 deficiency is severe or caused by pernicious anemia; sometimes, the mother’s own vitamin B12 deficiency is clinically mild and not recognized. Undetected and untreated vitamin B12 deficiency in infants can result in neurological damage, failure to thrive, developmental delays, and anemia 89, 90. The reasons include the small amounts of vitamin B12 in the breast milk of vegan mothers as well as the limited amounts of vitamin B12 crossing the placenta in these women during fetal development.
What is pernicious anemia?
Pernicious anemia is an irreversible auto-immune disease that affects the gastric mucosa (autoimmune gastritis) and results in gastric atrophy 78, 91, 92. People who have pernicious anemia can’t absorb enough vitamin B12 from food. This is because they lack intrinsic factor (IF), a protein made in your stomach. A lack of intrinsic factor (IF) leads to vitamin B12 deficiency. In pernicious anemia your own antibodies attack the parietal cells in your stomach, resulting in failure to produce intrinsic factor (IF) and malabsorption of dietary vitamin B12, recycled biliary vitamin B12, and free vitamin B12 93, 79, 60. Progressive destruction of the parietal cells that line your stomach cause decreased secretion of acid and enzymes required to release food bound vitamin B12. Antibodies to intrinsic factor (IFA) bind to IF preventing formation of the IF-B12 complex, further inhibiting vitamin B12 absorption. Without enough vitamin B12, your red blood cells don’t divide normally and are too large (megaloblasts). These changes occur because vitamin B12 is necessary for DNA synthesis 94. Pernicious anemia is one of two major types of “macrocystic” or “megaloblastic” anemia. These terms refer to anemia in which the red blood cells are larger than normal. The other major type of macrocystic anemia is caused by folic acid deficiency. In addition to megaloblasts, hypersegmented neutrophils are also present. The large red blood cells may have trouble getting out of the bone marrow—a sponge-like tissue inside the bones where blood cells are made. Megaloblastic anemia is characterized by large nucleated red blood cell precursors called megaloblasts in the bone marrow 94. Without enough red blood cells to carry oxygen to your body, you may feel tired and weak. Severe or long-lasting pernicious anemia can damage the heart, brain, and other organs in the body. Note that the causes of megaloblastic anemia other than vitamin B12 deficiency caused by impaired intrinsic factor (IF) production can include folic acid deficiency, altered pH in the small intestine, and lack of absorption of vitamin B12 complexes in the terminal ileum. Thus, pernicious anemia must be differentiated from other disorders that interfere with the absorption and metabolism of vitamin B12.
Pernicious anemia has often been confused with vitamin B12 deficiency 95. Pernicious anemia denotes only vitamin B12 deficiency due to gastric atrophy and/or intrinsic factor deficiency or autoimmune gastritis 95. Pernicious anemia is considered a late stage of autoimmune gastritis.
The pathogenesis of pernicious anemia has not been clarified, but it is likely linked to the autoimmune destruction of gastric glands due to autoreactive T lymphocytes in genetically predisposed individuals 95. The role of previous Helicobacter pylori (H. pylori) infection as a supposed but not yet definitely proven trigger of gastric autoimmunity cannot be excluded 95. Hershko et al. 96 have reported that H. pylori might serve as a trigger of autoimmune metaplastic atrophic gastritis and pernicious anemia, based on their observation that the prevalence of H. pylori infection was 87.5% in patients under 20 years of age. In addition, one theory regarding the initiating event of autoimmune metaplastic atrophic gastritis is molecular mimicry between H. pylori antigens and gastric H+/K+−ATPase 97.
In pernicious anemia, the underlying pathogenetic mechanism is autoimmune gastritis, an organ-specific immune-mediated disorder featuring the damage of the gastric parietal cells involved in the secretion of intrinsic factor (IF) and hydrochloric acid by the gastric proton pump 98. The presence of anti-parietal cell antibodies (PCAs) directed towards the gastric proton pump (gastric hydrogen potassium adenosine triphosphatase (H+/K+ ATPase)) as well as antibodies against intrinsic factor (IF) (although in a lower percentage) are commonly associated with gastric corpus atrophy and intrinsic factor deficiency 95, 99. Atrophic corpus gastritis is a chronic disease defined as a decrease in or loss of the original gastric glands, replaced by pseudo-pyloric or intestinal metaplasia or fibrosis 100. Gastric corpus atrophy is a necessary but insufficient condition for the onset of pernicious anemia, as gastric corpus atrophy may also take its course without pernicious anemia.
In rare cases, pernicious anemia is passed down through families (inherited disorder). This is called congenital pernicious anemia 95. Babies with congenital pernicious anemia do not make enough intrinsic factor (IF). Or they cannot properly absorb vitamin B12 in the small intestine. Congenital pernicious anemia is quite rare and distinguishable from the usual form of pernicious anemia due to the early age of onset and the absence of gastric corpus atrophy.
Pernicious anemia can also cause other problems, such as nerve damage, neurological problems (such as memory loss), and digestive tract problems. People who have pernicious anemia also may be at higher risk for weakened bone strength (osteoporosis) and stomach cancer. Pernicious anemia is frequently presenting with other autoimmune conditions such as autoimmune thyroid disease, type 1 diabetes, and vitiligo 101.
Without treatment, pernicious anemia causes vitamin B12 deficiency, even in the presence of adequate vitamin B12 intakes. Generally, it takes about 10–12 years to clinically develop symptomatic pernicious anemia, so pernicious anemia may onset with subclinical vitamin B12 deficiency 102.
Pernicious anemia is the most common cause of clinically evident vitamin B12 deficiency around the world 79, 78. Pernicious anemia accounts for 20%‐50% of the vitamin B12 deficiency in adults 103. The incidence of pernicious anemia in the United States is an estimated 151 per 100,000, and this condition is more common in women and in people of European ancestry (North Europeans and Caucasian Americans) 78. The prevalence of pernicious anemia in Japan is rare, 1 to 5 per 100,000 persons 104, compared with the West.
An important point is that pernicious anemia may lead to potentially serious long-term complications that may be related to micronutrient deficiencies and the development of gastric neoplasms, in particular, gastric cancer and type 1 gastric neuroendocrine tumors 95. When not recognized in a timely manner or when pernicious anemia is diagnosed with delay, these complications may be potentially life-threatening and sometimes irreversible.
Vitamin B12 therapy resolves the anemia of pernicious anemia, but does not cure the atrophic gastritis, which can progress to gastric cancer 105. The incidence of gastric adenocarcinoma is 2- to 3-fold greater in patients with pernicious anemia than in the general population of the same age 106. Presently, periodic gastroscopy and/or barium studies are not advocated in patients with treated pernicious anemia who are asymptomatic, because such screening has not been demonstrated to prolong lifespan 106.
A population-based, case-control study using the Surveillance, Epidemiology, and End Results (SEER)–Medicare database found that elderly persons with pernicious anemia were not only at significantly increased risk for noncardia gastric adenocarcinoma and gastric carcinoid tumors, they were also at increased risk for the following 105:
- Tonsillar cancer
- Hypopharyngeal cancer
- Esophageal squamous cell carcinoma
- Small intestinal cancer
- Liver cancer
- Myeloma
- Acute myeloid leukemia
- Myelodysplastic syndrome
In a longitudinal study of 199 intrinsic factor antibody (IFA)–positive and 168 IFA-negative Chinese patients, Chan et al 107 found that despite a good hematologic response to therapy, both groups had an unsatisfactory neurologic response, and newly diagnosed hypothyroidism was found during follow-up. In addition, newly diagnosed cancers were also found (24 in IFA-positive patients, seven in IFA-negative patients), of which 20% were stomach cancer 107.
For the intrinsic factor antibody (IFA)-positive patients with a cancer, mean survival was 64 months; for those without a cancer, it was 129 months. Mortality was 31% in this group, in which cancer-related deaths represented 37% of the total 107. For the intrinsic factor antibody (IFA)-negative patients with a cancer, mean survival was 36 months. For those without a cancer, it was 126 months. Mortality was 21% in this group, in which cancer-related deaths represented 14% of the total.
Chan et al 107 concluded that although Chinese patients treated for pernicious anemia demonstrated a good survival period, they remained at increased risk for gastric carcinoma, and IFA-positive patients had a higher risk of developing all types of cancers and cancer-related deaths than did IFA-negative patients.
Pernicious anemia has been estimated to be present in approximately 2% of individuals over 60 years of age 108. Although anemia is often a symptom, the condition is actually the end stage of an autoimmune inflammation of the stomach known as autoimmune atrophic gastritis, resulting in destruction of stomach cells by one’s own antibodies (autoantibodies). Progressive destruction of the cells that line the stomach causes decreased secretion of acid and enzymes required to release food-bound vitamin B12. Antibodies to intrinsic factor (IF) bind to IF preventing formation of the IF-B12 complex, further inhibiting vitamin B12 absorption. About 20% of the relatives of pernicious anemia patients also have the condition, suggesting a genetic predisposition. It is also thought that H. pylori infection could be involved in initiating the autoimmune response in a subset of individuals 109. Further, co-occurrence of autoimmune atrophic gastritis with other autoimmune conditions, especially autoimmune thyroiditis and type 1 diabetes mellitus, has been reported 110.
Pernicious anemia signs and symptoms are similar to other vitamin B12 deficiencies, but pernicious anemia is sometimes associated with other autoimmune diseases such as type 1 diabetes, autoimmune thyroiditis, and Addison’s disease.
When pernicious anemia is suspected, the first step is usually a full blood panel to test for anemia and/or macrocytosis, together with testing for cobalamin deficiency and increased levels of homocysteine and/or methylmalonic acid (MMA) 95. Next, the positivity of gastric autoantibodies towards parietal cells and/or intrinsic factor (IF) is commonly assessed 95. Sensitivity and specificity of the anti‐intrinsic factor antibody test were 50%‐70%, and greater than 95%, respectively 111. Sensitivity and specificity of the antigastric parietal cell antibody test were more than 90% and 50%, respectively 112. In any case, the hematological and/or serological suspicion of pernicious anemia always needs to be confirmed by histological assessment of gastric antral and corpus biopsies obtained during gastroscopy to ascertain the presence of autoimmune gastritis 95.
The treatment for pernicious anemia is lifelong administration of vitamin B12. Treatment of pernicious anemia generally requires injections of vitamin B12 to bypass intestinal absorption. High-dose oral supplementation is another treatment option, because consuming 1,000 mcg (1 mg)/day of vitamin B12 orally should result in the absorption of about 10 mcg/day (1% of dose) by passive diffusion. In fact, high-dose oral therapy is considered to be as effective as intramuscular injection 9.
Patients with pernicious anemia are at high risk of developing stomach cancer such as gastric adenocarcinoma and carcinoid tumors 113. Significant risk factors for the development of gastric carcinoma in autoimmune metaplastic atrophic gastritis include the presence of pernicious anemia, severity of mucosal atrophy, intestinal metaplasia, disease duration, and over 50 years of age 114. Periodic stomach examinations are recommended for patients with pernicious anemia.
Pernicious anemia causes
Pernicious anemia is an autoimmune disorder. Typically, pernicious anemia is associated with the presence of autoantibodies against intrinsic factor (anti-intrinsic factor antibody or IFA) and anti-parietal cell antibodies (PCA), thus supporting the autoimmune origin of this condition 115. Anti-parietal cell antibodies (PCA) are seen in up to 85% of patients with pernicious anemia 116. However, the anti-parietal cell antibody (PCA) is not specific for pernicious anemia and can be seen in 3 to 10% of normal healthy populations without any evidence of megaloblastic anemia 116. Antibodies against parietal cells (PCA) are class M, G, and A immunoglobulins directed towards the alpha and beta subunits of the gastric proton pump (hydrogen-potassium ATP-ase) 117. Anti-intrinsic factor antibodies (IFA) are seen in 40 to 60% of the patients with pernicious anemia and are highly specific for the disease 116. Antibodies against intrinsic factor (IFA) are class G immunoglobulins that target the binding site for cobalamin (type I) or the binding site for ileal epithelial mucosa (type II) 118. These autoantibodies are released from plasma cells activated by autoreactive CD4+ T cell lymphocytes in perigastric lymph nodes 119. These triggered CD4+ T cells target the proton pump ATPases, which leads to their immune destruction 116. Atrophic gastritis with loss of parietal cells and subsequent intrinsic factor (IF) deficiency develops. This leads to vitamin B12 deficiency and the onset of symptoms associated with pernicious anemia. Gastric dendritic cells are responsible for the activation of lymphocytes that lead to the production of these antibodies. The cause and mechanism of dendritic cell activation are not yet clarified 116. Some research studies suggest Helicobacter pylori (H. pylori) infection is a trigger in genetically susceptible individuals 120. The studies propose molecular mimicry and immune cross-reactivity between the proton pump ATPase and the H. pylori antigens as a triggering event 120. A 2017 review evaluating H. pylori antigenic mimicry stated that these antigens play an important role in the induction of humoral and cellular immune responses, which may predispose patients to pathological inflammatory responses 121.
These circulating anti-intrinsic factor antibodies (IFA) and anti-parietal cell antibodies (PCA) cause autoimmune chronic atrophic gastritis with parietal cell loss and eventual vitamin B12 deficiency 116. However, autoimmune gastritis-associated gastric corpus atrophy may progress without developing pernicious anemia 95.
Pernicious anemia can be associated with other autoimmune diseases and in patients with polyglandular autoimmune disorders. Autoimmune diseases associated with pernicious anemia include type 1 diabetes (3 to 4%), vitiligo (2 to 8%), and autoimmune thyroid disease (3 to 32%) 115. Type III polyglandular autoimmune syndrome is characterized by the presence of autoimmune thyroiditis, vitiligo, alopecia, type 1A diabetes mellitus, pernicious anemia, and chronic atrophic gastritis 122. HLA alleles are thought to play a role in the pathogenesis of these autoimmune disorders, but the mechanism is not entirely understood. HLA-DRB1/03 and HLA-DRB1/04 alleles may predispose to autoimmune gastritis and subsequent pernicious anemia 115.
There is an overlap in patients infected with Helicobacter pylori (H. pylori) and the development of chronic atrophic gastritis associated with pernicious anemia 123. Researchers propose H. pylori peptide-induced gastric T-cell proliferation as the cause of pernicious anemia in some patients 120. They were able to demonstrate the presence of activated T cells in the gastric mucosa of patients with autoimmune chronic atrophic gastritis and H. pylori infection. These T cells reacted to both hydrogen-potassium-ATPase and H. pylori 120. Recent experimental and clinical data suggest long-standing H. pylori infection plays a pivotal role in developing atrophic gastritis and subsequent pernicious anemia; however, convincing data to support H. pylori infection as a definite cause of pernicious anemia is still lacking 115. Molecular analyses have revealed hydrogen-potassium-ATPase epitopes that are similar to, or cross-reactive with, epitopes of H. pylori antigens. Thus suggesting that in genetically susceptible individuals, H. pylori infection can trigger gastric autoimmunity via molecular mimicry 120.
A heritable form of pernicious anemia called “childhood pernicious anemia” is seen in children with a genetic defect that leads to decreased IF production or abnormal IF formation 95. This condition is quite rare and distinguishable from the usual form of pernicious anemia due to the early age of onset and the absence of gastric corpus atrophy.
Risk factors for pernicious anemia
Pernicious anemia is more common in people of Northern European and African descent than in other ethnic groups.
Older people also are at higher risk for the condition. This is mainly due to a lack of stomach acid and intrinsic factor, which prevents the small intestine from absorbing vitamin B12. As people grow older, they tend to make less stomach acid.
Pernicious anemia also can occur in younger people and other populations. You’re at higher risk for pernicious anemia if you:
- Have a family history of the condition.
- Have had part or all of your stomach surgically removed. The stomach makes intrinsic factor. This protein helps your body absorb vitamin B12.
- Have an autoimmune disorder that involves the endocrine glands, such as Addison’s disease, type 1 diabetes, Graves’ disease, or vitiligo. Research suggests a link may exist between these autoimmune disorders and pernicious anemia that’s caused by an autoimmune response.
- Have had part or all of your small intestine surgically removed. The small intestine is where vitamin B12 is absorbed.
- Have certain intestinal diseases or other disorders that may prevent your body from properly absorbing vitamin B12. Examples include Crohn’s disease, intestinal infections, and HIV.
- Take medicines that prevent your body from properly absorbing vitamin B12. Examples of such medicines include antibiotics and certain seizure medicines.
- Are a strict vegetarian who doesn’t eat any animal or dairy products and doesn’t take a vitamin B12 supplement, or if you eat poorly overall.
Pernicious anemia prevention
Because an increased familial incidence of pernicious anemia exists, family members should be aware that they are at greater risk of developing this disease and should seek medical attention promptly if they develop anemia or mental and neurologic symptoms 124. Monitor siblings and children of patients with a hereditary abnormality of vitamin B12 deficiency for evidence of the specific defect in cobalamin transport or metabolism.
Determine whether vitamin B12 deficiency is the cause in patients who recently developed evidence of mental deterioration.
Prophylactically treat patients with vitamin B12 when they have undergone total gastrectomy, bypass procedures for weight reduction, ileectomy, pancreatectomy, or when they have atrophic gastritis or chronic inflammatory disease of the ileum 124.
Strict vegetarians should continue supplementary vitamin B12, particularly during pregnancy and while nursing a newborn infant 124.
Elderly people are at risk for developing pernicious anemia due to achlorhydria. Therefore, serum vitamin B-12 levels should be checked. If low or if cobalamin deficiency is suspected, they should be treated with vitamin B-12 supplementation.
Pernicious anemia signs and symptoms
The onset of pernicious anemia usually is insidious and vague. The main signs and symptoms of pernicious anemia are hematological and neurological consequences of vitamin B12 deficiency, and both require several years for their development. The classic presentation consists of a triad of jaundice, glossitis, and myeloneuropathy 125. However, with advances in clinical detection and often routine laboratory testing, this classic triad of jaundice, glossitis, and myeloneuropathy is now a rarity. Many pernicious anemia patients are incidentally noted to have macrocytic anemia and are ultimately diagnosed with this condition. Others may either present with symptoms attributable to anemia, such as lethargy and inability to concentrate, or with symptoms attributable to neuronal damage, such as paresthesias, imbalance, and spasticity 116.
Figure 6. Pernicious anemia signs and symptoms (related to hypochlorhydria and vitamin B12 deficiency)
[Source 95 ]General symptoms
Weight loss of 10-15 lb occurs in about 50% of patients and probably is due to anorexia, which is observed in most patients. Low-grade fever occurs in one third of newly diagnosed patients and promptly disappears with treatment.
Heart symptoms
Individuals with pernicious anemia often tolerate the anemia well, and many are ambulatory with hematocrit levels in the mid-teens. However, the cardiac output is usually increased when hematocrit levels fall below 20%, with associated accerations in heart rate. Congestive heart failure and coronary insufficiency can occur, most particularly in patients with preexisting heart disease.
Gastrointestinal symptoms
Approximately 50% of patients with pernicious anemia develop atrophic glossitis, presenting with a smooth tongue that may be painful and beefy red, with loss of papillae that is usually most marked along the edges of the tongue 126. These patients report burning or soreness, most particularly on the anterior third of the tongue, associated with changes in taste and loss of appetite 41.
Patients may report either constipation or having several semisolid bowel movements daily. These symptoms have been attributed to megaloblastic changes of the cells of the intestinal mucosa.
Nonspecific gastrointestinal symptoms are not unusual and include anorexia, nausea, vomiting, heartburn, pyrosis, flatulence, and a sense of fullness 127. Rarely, patients present with severe abdominal pain associated with abdominal rigidity; this has been attributed to spinal cord pathology. Venkatesh and colleagues 128 report the case of a patient who presented with epigastric pain, diarrhea, and vomiting and was found to have thrombosis of the portal, superior mesenteric, and splenic veins due to hyperhomocysteinemia secondary to pernicious anemia.
Neurologic symptoms
The most common neurologic symptoms in vitamin B12 deficiency include paresthesias, weakness, clumsiness, and an unsteady gait. The last two symptoms are exacerbated in dark environments due to the loss of visual cues that patients often rely on, in concert with the loss of proprioception. These neurologic symptoms are due to myelin degeneration and loss of nerve fibers in the dorsal and lateral columns of the spinal cord and cerebral cortex (subacute combined degeneration).
Neurologic symptoms and findings may be present in the absence of anemia. This is more common in patients taking folic acid or on a high-folate diet.
Older patients may present with symptoms suggesting senile dementia or Alzheimer disease; memory loss, irritability, and personality changes are commonplace 116. Common psychiatric manifestations include depression, mania, chronic fatigue syndrome, and psychosis 95. Cognitive symptoms include memory impairment, attention deficit, and dementia 95. So-called megaloblastic madness—delusions, hallucinations, outbursts, and paranoid schizophrenic ideation—is less common. Identifying the cause is important because significant reversal of these symptoms and findings can occur with vitamin B12 administration.
While neurologic symptoms usually occur in the elderly, they can rarely occur in the young 129. Kocaoglu et al. 130 reported a case of vitamin B12 deficiency and cerebral atrophy in a 12-month-old infant whose development had slowed since 6 months of age; the infant was exclusively breastfed and his mother was a long-time vegetarian. Neurologic recovery began within days after the infant received an intramuscular cobalamin injection.
Genitourinary symptoms
Urinary retention and impaired micturition may occur because of spinal cord damage. This can predispose patients to urinary tract infections.
Symptoms of thrombotic complications
A study of four patients revealed that pernicious anemia can lead to hyperhomocysteinemia that is significant enough to lead to venous thrombosis, even in the absence of any other risk factors for thromboembolism 131.
Pernicious anemia complications
One of the most dreaded complications of pernicious anemia is the development of gastric cancer 105. A 2013 systematic review of over 22,000 patients with pernicious anemia found a pooled gastric cancer incidence of 0.27% per person-year, with a nearly sevenfold increased risk of gastric cancer in these patients 132. The same study showed a pooled gastric cancer recurrence rate of 6.8 132. For this reason, an upper gastrointestinal endoscopy is recommended when pernicious anemia is diagnosed 115. Repeat endoscopies without any evidence of gastrointestinal symptoms are generally not recommended. Surveillance endoscopy every three years is recommended by some experts in patients with documented evidence of advanced chronic autoimmune atrophic gastritis 133.
According to a large United States population study based on a Surveillance, Epidemiology, and End Results (SEER) Medicare database, patients with pernicious anemia are at higher risk of 10 cancer types 105:
- Gastric adenocarcinoma
- Gastric carcinoid tumors
- Tonsillar cancer
- Hypopharyngeal cancer
- Esophageal squamous cell carcinoma
- Myeloma
- Acute myeloid leukemia
- Myelodysplastic syndrome
The authors state, “The most striking of our findings was an 11-fold increase in the risk of gastric carcinoid tumors for both men and women with pernicious anemia, a risk that was higher among cases occurring 6 or more years after the pernicious anemia report/diagnosis” 105. They also point out these are uncommon cancers with low absolute risk: “Of the 17,076 cancers in our study among people with pernicious anemia, just 83 (0.5%) were gastric carcinoid tumors” 105.
Pernicious anemia diagnosis
When pernicious anemia is suspected, the first step is usually a full blood panel to test for anemia and/or macrocytosis, together with testing for vitamin B12 deficiency and increased levels of homocysteine and/or methylmalonic acid (MMA). Next, the positivity of gastric autoantibodies towards parietal cells and/or intrinsic factor is commonly assessed. In any case, the hematological and/or serological suspicion of pernicious anemia always needs to be confirmed by histological assessment of gastric antral and corpus biopsies obtained during gastroscopy 95.
The workup for pernicious anemia may include the following 134:
- Complete blood cell count (CBC)
- Peripheral blood smear
- Indirect bilirubin and lactate dehydrogenase assays
- Evaluation of gastric secretions. Total gastric secretions are decreased to about 10% of the reference range. Most patients with pernicious anemia are achlorhydric, even with histamine stimulation. Intrinsic factor (IF) is either absent or markedly decreased.
- Serum vitamin B12 (cobalamin), folic acid, methylmalonic acid (MMA) and homocysteine assays.
- Serum cobalamin reference ranges may vary slightly among different laboratories, but are generally from 200–900 pg/mL. Values of 180-250 pg/mL are considered bordeline, while less than 150 pg/mL is considered diagnostic of vitamin B12 deficiency. In these cases, elevated levels of methylmalonic acid (MMA) and total homocysteine can confirm the diagnosis 33.
- The serum cobalamin level is usually low in patients with pernicious anemia. However, up to a third of patients can present with normal vitamin B12 levels and normocytic anemia, which often delays diagnosis 135. Certain patients with other forms of cobalamin deficiency, such as some inborn forms of cobalamin deficiency, transcobalamin 2 deficiency, and cobalamin deficiency due to nitrous oxide, can also present with normal serum cobalamin levels.
- Serum cobalamin levels may also be low in patients with no clinical or identifiable metabolic abnormality 38. Causes of falsely low serum cobalamin levels inclue the following:
- Pregnancy
- Oral contraceptives and hormone replacement therapy
- Multiple myeloma
- Transcobalamin 1 (TC1) deficiency
- Severe folic acid deficiency
- Ascorbic acid in high doses
- A serum folic acid assay is useful for ruling out folic acid deficiency. The reference range is 2.5-20 ng/mL. Blood should be drawn before patients have a single hospital meal since food can restore serum folic acid levels to normal. Red blood cell folic acid level is not influenced by food.
- Levels of antibodies against intrinsic factor (IF) or the cells which make intrinsic factor (anti-parietal cell antibodies [PCAs]).
- Schilling test (no longer available in most medical centers)
- A clinical trial of vitamin B12
- Patients with diagnosis of pernicious anemia should undergo gastroscopy with biopsies to ascertain the presence of autoimmune gastritis 95. Biopsies should be collected following the updated Sydney system 136: two biopsies of the antrum and two biopsies from the corpus should be obtained and sent in separate vials. Another biopsy should be performed from incisura angularis and sent in the same vial of antrum biopsies.
- Bone marrow aspiration and biopsy (only needed if diagnosis is unclear)
Complete blood cell count (CBC) and peripheral blood smear may show the mean corpuscular volume (MCV) and mean cell hemoglobin (MCH) are increased, with a mean corpuscular hemoglobin concentration (MCHC) within the reference range 134. However, up to 30% of patients with pernicious anemia may lack macrocytosis 95. A normal MCV (mean corpuscular volume) does not rule out megaloblastic anemia, and pathognomonic megaloblasts are rarely seen. The hematocrit must fall by 20% before megaloblasts appear in the blood 125. Anisocytosis and an increase in the red cell distribution width is the earliest measurable change in red cell indices to hint toward the diagnosis 125.
The peripheral blood usually shows a macrocytic anemia with a mild leukopenia and thrombocytopenia. The leukopenia and thrombocytopenia usually parallel the severity of the anemia. The peripheral smear shows oval macrocytes, hypersegmented granulocytes, and anisopoikilocytosis. In severe anemia, red blood cell inclusions may include Howell-Jolly bodies, Cabot rings, and punctate basophilia. The macrocytosis can be obscured by the coexistence of iron deficiency, thalassemia minor, or inflammatory
The indirect bilirubin level may be elevated because pernicious anemia is a hemolytic disorder associated with increased turnover of bilirubin 134. The serum lactate dehydrogenase (LDH) concentration usually is markedly increased 134. Increased values for other red blood cells, enzymes, and serum iron saturation also are observed. The serum potassium, cholesterol, and skeletal alkaline phosphatase often are decreased.
A significantly decreased serum cobalamin level along with a typical clinical presentation, a characteristic peripheral smear, and an increased indirect bilirubin and LDH level is sufficient evidence for the diagnosis of a megaloblastic anemia.
Serum methylmalonic acid and homocysteine tests are important confirmatory tests but are not first-line tests. Elevated serum methylmalonic acid and homocysteine levels are found in patients with pernicious anemia. They probably are the most reliable test for cobalamin deficiency in patients who do not have a congenital metabolism disorder. In the absence of an inborn error of methylmalonic acid metabolism, methylmalonic aciduria is a sign of cobalamin deficiency.
Table 5. Serum methylmalonic acid (MMA) and homocysteine values used in differentiating between vitamin B12 deficiency and folic acid deficiency
| Patient Condition | Methylmalonic Acid | Homocysteine |
|---|---|---|
| Healthy | Normal | Normal |
| Vitamin B12 deficiency | Elevated | Elevated |
| Folate deficiency | Normal | Elevated |
Testing for B12 Deficiency
A B12 level below 200 pg/mL (ng/L) is consistent with vitamin B12 deficiency 123. Levels between 200 to 400 pg/mL are considered borderline 116. Serum B12 measurement alone has poor sensitivity and specificity for detecting B12 deficiency 125. In patients with pernicious anemia, this level will be falsely elevated in 22 to 35% of the patients due to the interaction of IF antibody (IFA) with the “IF reagent” used to detect B12 levels in current assays 116. Falsely low serum vitamin B12 levels can occur in patients with underlying multiple myeloma and pregnancy 38, 116.
Methylmalonic acid (MMA) and homocysteine levels can be obtained in patients when vitamin B12 levels are borderline or nondiagnostic to confirm the diagnosis of B12 deficiency 138. These assays are considered more sensitive and specific for detecting B12 deficiency when compared to serum B12 levels 125. Methylmalonic acid (MMA) can also help differentiate between vitamin B12 and folate deficiency, as it is elevated in vitamin B12 deficiency but not in folate deficiency 125. Homocysteine levels are elevated in folate deficiency, vitamin B6 deficiency, and patients with hypothyroidism 38. MMA level can be falsely elevated in patients with bacterial overgrowth, especially when there are blind loops of the bowel (following gastric surgery) 125. Both levels can be falsely elevated in patients with renal failure 125, 38.
Serum holotranscobalamin (holoTC) level measures the metabolically active fraction of serum vitamin B12 and is considered a more accurate test for detecting B12 deficiency 38. Transcobalamin is a transport protein that binds only 10 to 30% of the total plasma B12; however, this constitutes all of the “active fraction” used for metabolic activity 125. Limitations of this test include a large window with indeterminate values 138. In addition, according to one study, approximately 63% of patients with low holoTC levels had normal methylmalonic acid levels, raising concerns regarding the utility of this test as a true measure of B12 deficiency 138. A 2013 study measuring the utility of biomarkers for B12 deficiency compared serum B12 levels to holotranscobalamin and recommended holotranscobalamin as the initial screening test for the detection of B12 deficiency, followed by MMA levels 139. They also suggested that an indeterminate holotranscobalamin level between 23 and 75 pmol should be followed by methylmalonic acid testing. Of note, this study was conducted in patients with normal renal function.
Definitive Testing for Pernicious Anemia
Traditionally, vitamin B12 absorption was measured using the Schilling test. This test is now considered obsolete, and there is no available assay for detecting B12 absorption at this time 125. In the absence of reliable B12 absorption assays, definitive testing for pernicious anemia relies on the detection of circulating antibodies to intrinsic factors (IFA) and gastric parietal cells (PCA).
Demonstration of circulating intrinsic factor autoantibodies is almost diagnostic of type A (autoimmune) gastritis and pernicious anemia. Intrinsic factor (IF) antibodies are specific for this disorder and can be used to confirm the diagnosis 125. There are two types of IF antibodies (IFA). Type 1 IF antibodies block binding of vitamin B12 to intrinsic factor and are found in 70% to 90% of patients with pernicious anemia. Type 2 IF antibodies prevent attachment of the vitamin B12–IF complex to ileal receptors and are present in approximately 35% to 50% of patients with pernicious anemia; they rarely occur in the absence of type 1 IF antibodies. Both type 1 and type 2 antibodies are detected more often in gastric juice than in the serum 140.
In one case report, the presence of antibodies to intrinsic factors (IFA) was used to diagnose vitamin B12 deficiency in a patient with severe leukoencephalopathy 141. Interestingly, serum vitamin B12, homocysteine, and methylmalonic acid levels were normal. The patient responded to intensive cobalamin therapy 141.
Parietal cell antibodies occurs in 90% of patients with pernicious anemia. However, antibodies to parietal cells (PCA) are not specific for pernicious anemia 116. Some experts advise against routine testing for antibodies to parietal cells (PCA); others recommend routine testing with anti-IF antibodies (IFA) because the combined sensitivity for pernicious anemia approaches 73% 94, 38. Dual testing for intrinsic factors antibodies (IFA) and parietal cell antibodies (PCA) with proof of atrophic gastritis is 100% specific for pernicious anemia 116.
In ambiguous cases, a bone marrow biopsy showing megaloblastic erythropoiesis and arrested maturation of myeloid precursor cells will establish the diagnosis 94. An alternative approach in difficult cases is to establish the presence of atrophic gastritis with endoscopic evaluation and biopsy and/or showing the presence of hypergastrinemia 94. In rare situations, an empiric trial of vitamin B12 replacement can be used to make the diagnosis 94. In this scenario, a rise in the reticulocyte count (which occurs within 5 to 14 days) confirms the diagnosis.
Alternative and new approaches to the diagnosis of pernicious anemia are under evaluation. One of these is a newer cobalamin absorption test, which has its basis in measuring the change in serum holotranscobalamin following oral ingestion of non-radiolabeled cobalamin. Another approach has been described using accelerator mass spectrometry to quantify 14C in the blood following an orally administered dose of [14C]-cyanocobalamin 125. Recently an ELISA test measuring serum concentration of human IF has been developed and may prove to be an alternate measure of impaired IF production/absorption 142.
Once the diagnosis of pernicious anemia is established, confirmatory testing with gastroscopy and histologic assessment of the gastric mucosa to assess for the presence of atrophic gastritis is indicated 95. Pernicious anemia is recognized as a late-stage complication of autoimmune gastritis, with an increased risk of gastric cancers in this population 95. Therefore, a new diagnosis of pernicious anemia warrants endoscopy with biopsies to detect the presence of atrophic gastritis and to rule out gastric cancers 133. The presence of intestinal metaplasia on gastric biopsy confers a diagnosis of atrophic gastritis 133. Pale gastric mucosa and increased visibility of vasculature are typical endoscopic features of atrophic gastritis. With metaplasia, light-blue crests and white opaque fields are present 133.
Recent advances in endoscopic techniques have led to the development of an endoscopic grading of gastric intestinal metaplasia (EGGIM) using noninvasive techniques to assess the presence of metaplasia during endoscopy without any need for biopsies. This system has shown acceptable sensitivity and specificity compared to biopsies and can be used when evaluating patients with pernicious anemia 95. In a cross-sectional study of 210 patients with atrophic gastritis, endoscopic grading of gastric intestinal metaplasia (EGGIM) was found to reliably identify more than 90% of patients with gastric corpus intestinal metaplasia. This method was shown to overestimate intestinal metaplasia when pseudopyloric metaplasia was present 95.
Additional testing
Testing for iron deficiency is indicated for all patients with pernicious anemia 95. Up to 20% of the patients with pernicious anemia have concomitant iron deficiency anemia and, in severe cases, may have microcytic red blood cells 94. Serum levels of iron, transferrin, and ferritin should be measured in patients with pernicious anemia, especially when macrocytosis is not present. It is important to remember that patients with pernicious anemia and associated megaloblastic anemia may also develop severe thrombocytopenia 125. Platelet production can be reduced by around 10%, and patients may also have abnormal platelet function 125. Leukopenia may be present but rarely causes any clinical issues 125. Indirect bilirubin and lactate dehydrogenase levels are usually elevated due to the rapid breakdown of red blood cells and intramedullary hemolysis. It is imperative to remember that vitamin B12 and folate levels should be tested simultaneously in patients with macrocytic anemia to ensure both deficiencies are diagnosed if present 38.
Pernicious anemia treatment
Doctors treat pernicious anemia by replacing the missing vitamin B12 in the body. People who have pernicious anemia will need lifelong vitamin B12 treatment 38. Lifelong treatment for patients with confirmed pernicious anemia starts with an intramuscular (IM) injection of 1000 micrograms of B12 (hydroxocobalamin in Europe or cyanocobalamin in the United States) administered daily or every other day for 1 to 2 weeks, followed by weekly injections for 1 to 2 months, then a monthly injection (cyanocobalamin) or every 2 to 3 months (hydroxocobalamin) 33, 20, 9, 143, 78, 144.
An alternate approach is an initial dose of 1000 mcg IM injection every other day for 1 to 2 weeks, followed by weekly injections for one month and then monthly injections thereafter 125. Response should be monitored by reticulocyte counts, lactic dehydrogenase (LDH), and an appropriate rise in hemoglobin levels. LDH levels decrease and hemoglobin levels increase by about 1 g/dL/week. A rise in LDH might indicate a relapse.
Following the initial intensive treatment phase, patients can continue IM injections, or they can be offered high-dose oral vitamin B12 supplementation for the lifelong maintenance phase. In a 2016 review of oral vitamin B12 replacement for treating pernicious anemia, the authors concluded that “oral vitamin B12 is an effective alternative to vitamin B12 IM injections” 145. High-dose cyanocobalamin (1000–2000 micrograms) is most commonly taken daily as an oral tablet. Alternate formulations include sublingual and intranasal, but they are not routinely recommended 33, 20, 9, 143.
Recent data have suggested that high-dose oral replacement is as effective as IM replacement because passive absorption of vitamin B12 can occur in the absence of intrinsic factor (IF) 146. Even with a total absence of intrinsic factor (IF), about 1% of an oral dose is absorbed, and the daily requirement for vitamin B12 is 1 µg/day. A study by Zhang and colleagues 147 found evidence that using orally ingested soy protein isolate (SPI) nanoparticles as a carrier can improve the intestinal transport and absorption of vitamin B12. A 2018 Cochrane review reported oral route was as effective as IM vitamin B12 replacement; however, this was supported by very low-quality evidence 23. Therefore, current guidelines advise against the use of oral replacement in the initial phase of treatment 38. High-dose oral replacement (with 1000 to 2000 mcg of vitamin B12 daily) can be considered in patients with pernicious anemia for maintenance therapy 38.
The oral route may be necessary in the rare patients who have allergic reactions to parenteral administration, or in patients receiving anticoagulant or antiplatelet agent therapy, in whom intramuscular injections are contraindicated 148. If the oral route is used, obtain serum cobalamin measurements at periodic intervals to ensure that adequate quantities of cobalamin have been absorbed. Oral cobalamin therapy should not be used in patients with neurologic symptoms 38.
A randomized, placebo-controlled trial of oral cobalamin therapy in 50 patients with borderline serum vitamin B12 levels (125-200 pg/mL) and nonspecific symptoms compatible with subtle vitamin B12 deficiency found that after 1 month, serum methylmalonic acid (MMA) levels were corrected more often in patients receiving oral cobalamin than in those receiving placebo. However, the benefit to the MMA level disappeared after 3 additional months without cobalamin therapy 149.
A study found that oral cobalamine was more effective than parenteral therapy in some circumstances 149.
The earliest sign of treatment response is an increase in reticulocyte count that occurs within 5 to 14 days of treatment 94. A decrease in methylmalonic acid (MMA) and plasma homocysteine levels has also been observed in the first five days of treatment. Sustained normalization of serum cobalamin subsequently follows. Neuropsychiatric symptoms take a longer time to recover. As noted before, some neurologic symptoms may be irreversible.
Alternate formulations of vitamin B12 have been approved and include sublingual and intranasal formulations. However, data regarding their clinical efficacy is still limited, and they are not routinely recommended.
Patients whose vitamin B12 deficiency is due to underlying diseases involving the intestine or pancreas may require additional therapy 150. Examples of additional therapy are surgical correction of anatomic abnormalities of the gut that produce small bowel bacterial overgrowth, or the treatment of fish tapeworm anemia or pancreatitis. Elderly patients who also have hypokalemia should receive oral potassium supplements, to prevent severe hypokalemia and possible arrhythmias.
Blood transfusions are rarely required in patients with a megaloblastic anemia that is due to vitamin B12 deficiency 151. The likelihood of obtaining a dramatic response to cobalamin therapy within a few days of initiating treatment makes it unnecessary to subject the patient to the hazards of blood transfusion. Usually, mild-to-moderate congestive heart failure secondary to anemia abates with bed rest and low-dosage diuretic therapy. However, if the congestive heart failure is severe or the patient has coronary insufficiency, transfusion of packed red blood cells may be necessary 151. Transfuse the blood slowly because patients who are transfused for severe anemia often develop circulatory overload. For this reason, low-dose diuretic therapy is often employed with the blood transfusion 151.
Management Guidelines
British Society of Gastroenterology (2019): “We suggest that a baseline endoscopy with biopsies should be considered in individuals aged ≥50 years, with laboratory evidence of pernicious anemia, defined by vitamin B12 deficiency and either positive gastric parietal cell or intrinsic factor antibodies. As gastric adenocarcinoma affects the corpus in pernicious anemia, biopsies should be taken from the greater and lesser curves (evidence level: low quality; grade of recommendation: weak; level of agreement: 93%)” 152.
European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) (2019): “Patients with autoimmune gastritis (includes those with pernicious anemia) may benefit from endoscopic follow-up every 3 to 5 years. Low-quality evidence, weak recommendation (82% agree [76% strongly or moderately agree])” 153.
American Gastroenterological Association (2021): “Providers should recognize pernicious anemia as a late-stage manifestation of autoimmune gastritis that is characterized by vitamin B-12 deficiency and macrocytic anemia. Patients with a new diagnosis of pernicious anemia who have not had a recent endoscopy should undergo endoscopy with topographical biopsies to confirm corpus-predominant atrophic gastritis for risk stratification and to rule out prevalent gastric neoplasia, including neuroendocrine tumors” 133.
Endoscopic Follow-Up
Due to the risk of developing gastric cancer and type 1 gastric neuroendocrine tumors, endoscopic surveillance is the mainstay of the follow-up in pernicious anemia, as the early detection of neoplastic lesions at follow-up could permit a curative resection. European guidelines 154 suggest a 3-year follow-up in patients with metaplastic atrophic gastritis only in the antrum or only in the corpus, if risk factors, namely autoimmune gastritis, first-degree family history of gastric cancer, incomplete intestinal metaplasia, or persistent H. pylori infection, are present. In case of atrophic gastritis or intestinal metaplasia involving both antrum and corpus, a 3-year follow-up is recommended unless a first-degree family history is present. In this case, endoscopy should be performed every 1–2 years. The 3-year follow-up was shown to be cost-effective in intermediate-risk gastric cancer countries 155 and was confirmed in another Italian cost-effective study 156. However, only a few studies were performed to investigate the best interval to follow-up patients harboring this condition. In two studies conducted proposing a 2-year interval, the development of neoplastic lesions was present earlier than the 3-year interval 157, 158. However, other studies showed that even in patients with non-extensive atrophic gastritis, namely OLGA I-II/OLGIM I-II, neoplastic lesions could develop 159, 160, 161, 162. Furthermore, a recent longitudinal cohort study, conducted on 122 patients with AAG and 38 patients with multifocal atrophic gastritis in a follow-up program with a 3-year interval, showed the presence of 16 gastric neoplastic lesions at follow-up: 18.7% gastric cancers, 25.0% low-grade dysplasia, 12.5% low-grade dysplasia adenomas and 43.7% type-1 neuroendocrine tumors 163. All the diagnosed lesions were endoscopically (87.5%) or surgically (12.5%) treated with favorable outcomes 163.
The management of type 1 neuroendocrine tumors and resection strategy have still not been clarified 164. The European Neuroendocrine Tumor Society guidelines suggest removing tumors larger than 10 mm as they represent neuroendocrine tumors with potentially more aggressive behavior 165. In a recent prospective study conducted on 80 patients presenting 127 gastric type 1 neuroendocrine tumors, the authors concluded that resection strategy could be planned based on the tumor size. Neuroendocrine tumors smaller than 5 mm could be surveilled, and could be removed by cold snare polypectomy when the size was between 5 and 10 mm and by endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) when bigger than 10 mm, even if with low evidence 166.
European guidelines suggest that surveillance in patients with gastric precancerous conditions should be performed with high-definition electronic chromoendoscopy to better recognize areas at risk for gastric cancer and to perform gastric biopsies. Three meta-analyses showed the high accuracy of conventional and virtual chromoendoscopy for the diagnosis of early gastric cancer and dysplasia in patients harboring precancerous conditions 167, 168, 169. Moreover, in pilot studies, virtual chromoendoscopy seemed to be useful for the characterization of type-1 neuroendocrine tumors 170.
Pernicious anemia prognosis
Most people with pernicious anemia do well with treatment, except for patients diagnosed with subacute combined degeneration (SCD) 171. It is important to start treatment early. Nerve damage can be permanent if treatment does not start within 6 months of symptoms. Although B12 supplementation stops progression and improves neurologic deficits in most patients with subacute combined degeneration, evidence shows complete resolution only occurs in a small percentage of them 172. A 2006 observational study evaluating 57 patients with subacute combined degeneration reported only 14% clinical resolution after B12 treatment 172. Still, the study reported that of these patients, 86% had at least some clinical improvement. Subgroup analysis revealed that the absence of sensory dermatomal deficit, negative Romberg and Babinski signs, age less than 50 years, and less than or equal to 7-segment involvement on magnetic resonance imaging correlated with complete resolution of neurologic symptoms 172. This study highlights the importance of early diagnosis and treatment of vitamin B12 deficiency, as patients with severe or prolonged neurological symptoms tend to have persistent symptoms despite treatment.
After treatment initiation for pernicious anemia, reticulocytosis begins approximately 5 days later, followed by red blood cell count normalization within 4 to 6 weeks 33. Typically, neurological symptom improvement is slower than hematological improvement, and the degree of neurological recovery is inversely proportional to the severity and duration of symptoms before treatment. Psychiatric symptoms such as emotional lability and psychosis may rapidly improve 173.
With ongoing care and proper treatment, most people who have pernicious anemia can recover, feel well, and live normal lives.
Without treatment, pernicious anemia can lead to serious problems with the heart, nerves, and other parts of the body. Some of these problems may be permanent.
Although vitamin B12 therapy resolves the anemia, it will not cure atrophic gastritis, and patients with pernicious anemia remain at higher risk of gastric cancers throughout their life 105. There is an increased risk of gastric adenocarcinoma in these patients 133. A longitudinal study from China reported that patients with pernicious anemia and anti-IF or anti-parietal cell antibodies had an unsatisfactory neurologic response to treatment and, over time, developed newly diagnosed hypothyroidism as well as alimentary canal malignancies 174. Twenty percent of the cancers noted in this study were gastric cancers. This study reported a mean survival of 64 months for patients who developed a malignancy compared to 129 months for those without malignancy. The mortality rate was reported as 31%, with cancer-related deaths representing 37%. Interestingly, the authors reported a higher risk of cancer in patients who were positive for anti-IF antibodies compared to those without these antibodies 174.
Vitamin B12 deficiency causes
Vitamin B-12 deficiency can result from:
- Inadequate intake
- Inadequate absorption
- Decreased utilization
- Use of certain drugs
Inadequate vitamin B12 intake is possible in general malnutrition, chronic alcohol abuse, and vegan or strict vegetarian diets but is otherwise unlikely. Breastfed babies of vegan mothers may develop vitamin B12 deficiency by age 4 to 6 months because in these babies, liver stores (which are normally extensive in other babies) are limited and their rapid growth rate results in high demand. Vitamin B12 malabsorption and deficiency due to inadequate dietary intake are common in the elderly. In the elderly, inadequate absorption most commonly results from decreased acid secretion in the stomach. In such cases, crystalline vitamin B-12 (such as that available in vitamin supplements) can be absorbed, but food-bound vitamin B12 is not liberated and absorbed normally.
Inadequate Vitamin B-12 absorption is the most common cause of vitamin B12 deficiency 175. Absorption of vitamin B12 from food requires normal function of the stomach, pancreas, and small intestine. Stomach acid and enzymes free vitamin B12 from food, allowing it to bind to R-protein (also known as transcobalamin-1 or haptocorrin), found in saliva and gastric fluids. In the alkaline environment of the small intestine, R-proteins are degraded by pancreatic enzymes, freeing vitamin B12 to bind to intrinsic factor (IF), a protein secreted by specialized cells in the stomach. Receptors on the surface of the ileum (final part of the small intestine) take up the IF-B12 complex only in the presence of calcium, which is supplied by the pancreas 175. Vitamin B12 can also be absorbed by passive diffusion, but this process is very inefficient—only about 1% absorption of the vitamin B12 dose is absorbed passively 52. The prevalent causes of vitamin B12 deficiency are (1) an autoimmune condition known as pernicious anemia, and (2) a disorder called food-bound vitamin B12 malabsorption. Both conditions have been associated with a chronic inflammatory disease of the stomach known as atrophic gastritis. Atrophic gastritis (an autoimmune disease characterized by the presence of antibodies directed against gastric parietal cells and intrinsic factor [IF]). Immune-mediated destruction of gastric parietal cells, gastric mucosal atrophy, hypochlorhydria, decreased IF production, subsequent vitamin B12 malabsorption, vitamin B12 deficiency and pernicious anemia (a type of megaloblastic anemia)
Inadequate absorption may occur in blind loop syndrome (with overgrowth of bacteria) or fish tapeworm infestation; in these cases, bacteria or parasites use ingested vitamin B12 so that less is available for absorption.
- Bacterial overgrowth syndromes, ileal resection or gastrointestinal diseases such as terminal ileitis, celiac disease, inflammatory bowel disease, Crohn’s disease and tropical sprue Altered absorption of the IF-vitamin B12 complex in the terminal ileum; intestinal villous atrophy and mucosal injury (celiac disease, Crohn’s disease and tropical sprue) 176
- Intestinal parasitic infestations (often accompanied by eosinophilia) caused by the protozoan Giardia lamblia or the fish tapeworm Diphyllobothrium latum 176. Vitamin B12 malabsorption through vitamin B12 trapping by the parasites
Vitamin B12 absorption may be inadequate if ileal absorptive sites are destroyed by inflammatory bowel disease or are surgically removed.
Disorders of the exocrine pancreas or pancreatectomy. Insufficient pancreatic enzyme activity leads to a reduction in the proteolytic degradation of haptocorrin (mediated by pancreatic proteases in the small intestine); as a consequence, vitamin B12 remains bound to haptocorrin, cannot form the IF-vitamin B12 complex and is not available for absorption by the enterocytes in the distal ileum 176.
Less common causes of inadequate vitamin B12 absorption include chronic pancreatitis, gastric bypass, partial or complete gastrectomy, gastric reduction, weight loss surgery and chronic gastritis due to Helicobacter pylori infection, malabsorption syndromes, AIDS, use of certain drugs (eg, antacids, metformin), repeated exposure to nitrous oxide (N2O), and a genetic disorder causing malabsorption in the ileum (Imerslund-Graesbeck syndrome).
- Long-term use (≥ 12 months) of drugs altering gastric acid secretion or gastric pH (e.g., proton-pump inhibitors, H2 receptor blockers and antacids) cause vitamin B-12 deficiency. These drugs reduce the production of hydrochloric acid by gastric parietal cells; as a consequence, vitamin B12 is not adequately released from the food matrix due to insufficient hydrochloric acid and low pepsin activity.
- The underlying mechanism accounting for metformin-induced vitamin B12 deficiency is not fully understood, although it may involve one or more of the following 176:
- Interference with the calcium-dependent binding of the IF-vitamin B12 complex to the cubilin receptor on enterocytes at the ileum level;
- Interaction with the cubilin endocytic receptor;
- Alteration in small intestine motility leading to small intestinal bacterial overgrowth and subsequent inhibition of IF-vitamin B12 complex absorption in the distal ileum;
- Alteration in bile acid metabolism and reabsorption;
- Increased liver accumulation of vitamin B12; and (6) Reduced IF secretion by gastric parietal cells.
- According to the British Society for Haematology guidelines for diagnosis and treatment of vitamin B12 deficiency, no recommendations can be currently given on prophylactic administration with oral vitamin B12 in patients using metformin 143. Despite the lack of definitive guidelines or recommendations on treatment of metformin-induced vitamin B12 deficiency, patients using metformin with concomitant vitamin B12 deficiency should receive cobalamin supplementation aimed to correct this deficiency and prevent the related risk of peripheral nerve damage and/or other clinical consequences 176. Importantly, prompt vitamin B12 administration should be considered, particularly in metformin-treated patients with vitamin B12 deficiency accompanied by neurologic and/or hematologic manifestations such as peripheral neuropathy and megaloblastic anemia.
- Nitrous oxide anesthesia or recreational use of nitrous oxide. Irreversible oxidation and inactivation of the coenzyme form of vitamin B12 (methylcobalamin) at the active site of the vitamin B12-dependent methionine synthase reaction, resulting in increased levels of MMA and homocysteine
Less commonly, decreased utilization of vitamin B12 or use of medications that affect vitamin B12 absorption or metabolism including the bile acid resin cholestyramine (used to treat hypercholesterolemia), colchicine (used for acute gout) and many antibiotics such as neomycin and the anti-tuberculosis drug para-aminosalicylic acid. Unlike long-term use of proton-pump inhibitors, histamine H2-receptor antagonists or metformin, the frequency or duration of use of these drugs is usually insufficient to result in clinical vitamin B12 deficiency 176. Cholestyramine can chelate IF; colchicine and antibiotics can inhibit endocytosis of the IF-vitamin B12 complex.
Lastly, inherited disorders affecting the sequential steps in the assimilation, transport and intracellular processing and metabolism of vitamin B12 (Imerslund-Gräsbeck syndrome). Reduced expression, binding activity or affinity of receptors and proteins involved in transport, intracellular processing and metabolism of vitamin B12.
Known risk factors for vitamin B12 deficiency include 177:
- Age older than 75 years
- Strict vegetarianism or a plant-based diet
- Alcohol abuse
- Atrophic gastritis
- Crohn’s disease
- Ileal resection
- Pernicious anemia
- Postgastrectomy syndrome
- Tapeworm infection
- Transcobalamin 2 deficiency
Atrophic gastritis
Atrophic gastritis is a histopathologic entity characterized by chronic inflammation of the gastric mucosa with loss of the gastric glandular cells and replacement by intestinal-type epithelium, pyloric-type glands, and fibrous tissue as a response to chronic injury 178. Atrophy of the gastric mucosa is the endpoint of chronic processes, such as chronic gastritis associated with Helicobacter pylori infection, other unidentified environmental factors, and autoimmunity directed against gastric glandular cells (autoimmune gastritis) 178. Atrophic gastritis represents the end stage of chronic gastritis, both infectious and autoimmune. In both cases, the clinical manifestations of atrophic gastritis are those of chronic gastritis, but pernicious anemia is observed specifically in patients with autoimmune gastritis and not in those with Helicobacter pylori–associated atrophic gastritis.
Atrophic gastritis is thought to affect 10%-30% of people over 60 years of age 179. Atrophic gastritis is frequently associated with the presence of autoantibodies directed toward stomach cells (see pernicious anemia) and/or infection by the bacteria, Helicobacter pylori (H. pylori) 180. Helicobacter pylori (H. pylori) infection induces chronic inflammation of the stomach, which may progress to peptic ulcer disease, atrophic gastritis, and/or gastric cancer in some individuals 181. Diminished gastric function in individuals with atrophic gastritis can result in bacterial overgrowth in the small intestine and cause food-bound vitamin B12 malabsorption. Vitamin B12 levels in serum, plasma, and gastric fluids are significantly decreased in individuals with H. pylori infection, and eradication of the bacteria has been shown to significantly improve vitamin B12 serum concentrations 182.
Pernicious anemia
Pernicious anemia has been estimated to be present in approximately 2% of individuals over 60 years of age 108. Although anemia is often a symptom, pernicious anemia is actually the end stage of an autoimmune inflammation of the stomach known as autoimmune atrophic gastritis, resulting in destruction of stomach cells by one’s own antibodies (autoantibodies). Progressive destruction of the cells that line the stomach causes decreased secretion of acid and enzymes required to release food-bound vitamin B12. Antibodies to intrinsic factor (IF) bind to IF preventing formation of the IF-B12 complex, further inhibiting vitamin B12 absorption. About 20% of the relatives of pernicious anemia patients also have the condition, suggesting a genetic predisposition. It is also thought that H. pylori infection could be involved in initiating the autoimmune response in a subset of individuals 109. Furthermore, co-occurrence of autoimmune atrophic gastritis with other autoimmune conditions, especially autoimmune thyroiditis and type 1 diabetes mellitus, has been reported 183, 110.
Treatment of pernicious anemia generally requires injections of vitamin B12 to bypass intestinal absorption. High-dose oral supplementation is another treatment option, because consuming 1,000 μg (1 mg)/day of vitamin B12 orally should result in the absorption of about 10 μg/day (1% of dose) by passive diffusion. In fact, high-dose oral therapy is considered to be as effective as intramuscular injection 9.
Food-bound vitamin B12 malabsorption
Food-bound vitamin B12 malabsorption is defined as an impaired ability to absorb food- or protein-bound vitamin B12; individuals with this condition can fully absorb the free form 184. While the condition is the major cause of poor vitamin B12 status in the elderly population, it is usually associated with atrophic gastritis, a chronic inflammation of the lining of the stomach that ultimately results in the loss of glands in the stomach (atrophy) and decreased stomach acid production (see atrophic gastritis). Because stomach acid is required for the release of vitamin B12 from the proteins in food, vitamin B12 absorption is diminished. Decreased stomach acid production also provides an environment conducive to the overgrowth of anaerobic bacteria in the stomach, which further interferes with vitamin B12 absorption 66. Because vitamin B12 in supplements is not bound to protein, and because intrinsic factor (IF) is still available, the absorption of supplemental vitamin B12 is not reduced as it is in pernicious anemia. Thus, individuals with food-bound vitamin B12 malabsorption do not have an increased requirement for vitamin B12; they simply need it in the crystalline form found in fortified foods and dietary supplements.
Inherited disorders of vitamin B12 absorption
Rare cases of inborn errors of vitamin B12 metabolism have been reported in the literature 175. Imerslund-Gräsbeck syndrome is an inherited vitamin B12 malabsorption syndrome that causes megaloblastic anemia and neurologic disorders of variable severity in affected subjects. Similar clinical symptoms are found in individuals with hereditary IF deficiency (also called congenital pernicious anemia) in whom the lack of IF results in the defective absorption of vitamin B12. Additionally, mutations affecting vitamin B12 transport in the body have been identified 185.
Other causes of vitamin B12 deficiency
Other causes of vitamin B12 deficiency include surgical resection of the stomach or portions of the small intestine where receptors for the IF-B12 complex are located. Conditions affecting the small intestine, such as malabsorption syndromes (celiac disease and tropical sprue), may also result in vitamin B12 deficiency. Because the pancreas provides critical enzymes, as well as calcium required for vitamin B12 absorption, pancreatic insufficiency may contribute to vitamin B12 deficiency. Since vitamin B12 is found only in foods of animal origin, a strict vegetarian (vegan) diet has resulted in cases of vitamin B12 deficiency. Moreover, alcoholics may experience reduced intestinal absorption of vitamin B12 52 and individuals with acquired immunodeficiency syndrome (AIDS) appear to be at increased risk of deficiency, possibly related to a failure of the IF-B12 receptor to take up the IF-B12 complex 66. Furthermore, long-term use of acid-reducing drugs has also been implicated in vitamin B12 deficiency (see drug interactions below).
Drug interactions
A number of drugs reduce the absorption of vitamin B12. Proton-pump inhibitors (e.g., omeprazole and lansoprazole), used for therapy of Zollinger-Ellison syndrome and gastroesophageal reflux disease (GERD), markedly decrease stomach acid secretion required for the release of vitamin B12 from food but not from supplements 46. Long-term use of proton-pump inhibitors has been found to decrease blood vitamin B12 levels. However, vitamin B12 deficiency does not generally develop until after at least three years of continuous therapy 186, 187. Another class of gastric acid inhibitors known as histamine2 (H2)-receptor antagonists (e.g., cimetidine, famotidine, and ranitidine), often used to treat peptic ulcer disease, has also been found to decrease the absorption of vitamin B12 from food 46. It is not clear whether the long-term use of H2-receptor antagonists could cause overt vitamin B12 deficiency 188, 189. Individuals taking drugs that inhibit gastric acid secretion should consider taking vitamin B12 in the form of a supplement because gastric acid is not required for its absorption.
Other drugs found to inhibit vitamin B12 absorption from food include cholestyramine (a bile acid-binding resin used in the treatment of high cholesterol), chloramphenicol and neomycin (antibiotics), and colchicine (medicine for gout treatment) 46. Metformin, a medication for individuals with type 2 diabetes, was found to decrease vitamin B12 absorption by tying up free calcium required for absorption of the IF-B12 complex 176, 190. However, the clinical significance of this is unclear 191. It is not known whether calcium supplementation can reverse vitamin B12 malabsorption; therefore, calcium supplementation is not currently prescribed for the prevention or treatment of metformin-induced vitamin B12 deficiency 192. Previous reports that megadoses of vitamin C destroy vitamin B12 have not been supported 193 and may have been an artifact of the assay used to measure vitamin B12 levels 46.
Nitrous oxide, a commonly used anesthetic, oxidizes and inactivates vitamin B12, thus inhibiting both of the vitamin B12-dependent enzymes, and can produce many of the clinical features of vitamin B12 deficiency, such as megaloblastic anemia or neuropathy 46. Since nitrous oxide is commonly used for surgery in the elderly and in childbirth, some experts feel vitamin B12 deficiency should be ruled out prior to its use 179, 194.
Large doses of folic acid given to an individual with an undiagnosed vitamin B12 deficiency could correct megaloblastic anemia without correcting the underlying vitamin B12 deficiency, leaving the individual at risk of developing irreversible neurologic damage 46. For this reason, the Food and Nutrition Board of the US Institute of Medicine advises that all adults limit their intake of folic acid (supplements and fortification) to 1,000 mcg (1 mg) daily 195.
Groups at risk of vitamin B12 deficiency
The main causes of Vitamin B-12 deficiency include Vitamin B-12 malabsorption from food, pernicious anemia, postsurgical malabsorption, and dietary deficiency 196. However, in many cases, the cause of Vitamin B-12 deficiency is unknown.
The following groups are among those most likely to be Vitamin B-12 deficient.
Older adults
Depending on the definition used, between 3% and 43% of community-dwelling older adults, especially those with atrophic gastritis (chronic inflammation and thinning of your stomach), have vitamin B12 deficiency based on serum vitamin B12 levels 74, 75. The vitamin B12 deficiency rate at a cutoff of less than 211 mcg/L (156 pmol/L) at admission to a long-term care facility, according to one study, was 14%, and 38% of these older adults had levels lower than 407 pg/mL (300 pmol/L) 75.
Conditions associated with vitamin B12 deficiency include pernicious anemia, present in about 15% to 25% of older adults with vitamin B12 deficiency 42. Atrophic gastritis, an autoimmune condition affecting 2% of the general population but 8–9% of adults aged 65 and older, decreases production of intrinsic factor and secretion of hydrochloric acid in the stomach and thus decreases absorption of vitamin B12 42, 76. A third condition associated with vitamin B12 deficiency in older adults is Helicobacter pylori infection, possibly because this bacterium causes inflammation that leads to malabsorption of vitamin B12 from food 77.
Individuals with pernicious anemia
Pernicious anemia is an irreversible auto-immune disease that affects the gastric mucosa and results in gastric atrophy 78. This disease leads to attacks on parietal cells in the stomach, resulting in failure to produce intrinsic factor (IF) and malabsorption of dietary vitamin B12, recycled biliary vitamin B12, and free vitamin B12 79, 60. Therefore, without treatment, pernicious anemia causes vitamin B12 deficiency, even in the presence of adequate vitamin B12 intakes.
Pernicious anemia refers to one of the hematologic manifestations of chronic auto-immune gastritis, in which the immune system targets the parietal cells of the stomach or intrinsic factor itself, leading to decreased absorption of vitamin B12. Asymptomatic autoimmune gastritis likely precedes gastric atrophy by 10 to 20 years, followed by the onset of iron-deficiency anemia that occurs as early as 20 years before vitamin B12 deficiency pernicious anemia.
In rare cases, pernicious anemia is passed down through families. This is called congenital pernicious anemia. Babies with this type of anemia do not make enough intrinsic factor. Or they cannot properly absorb vitamin B12 in the small intestine.
Pernicious anemia is the most common cause of clinically evident vitamin B12 deficiency around the world 79, 78. The incidence of pernicious anemia in the United States is an estimated 151 per 100,000, and this condition is more common in women and in people of European ancestry 78.
Individuals with gastrointestinal disorders
Individuals with stomach and small intestine disorders, such as celiac disease and Crohn’s disease, may be unable to absorb enough vitamin B12 from food to maintain healthy body stores 80. But although rates of vitamin B12 deficiency are higher in people with celiac disease than other people 81, the evidence for whether rates of vitamin B12 deficiency are higher in people with Crohn’s disease is mixed 82, 83. Vitamin B12 deficiency in people with Crohn’s disease is typically treated with intramuscular cobalamin injections, but high doses of oral cyanocobalamin therapy (e.g., 1,000 mcg/day) might be equally effective 84.
Individuals who have had gastrointestinal surgery
Surgical procedures in the gastrointestinal tract, such as for weight loss (bariatric surgery) or to remove all or part of the stomach (gastrectomy), can cause a complete or partial loss of cells that secrete hydrochloric acid and cells that secrete intrinsic factor (IF) 85, 86. Thus, these procedures reduce the amount of vitamin B12, particularly food-bound vitamin B12, that the body absorbs 85, 86. High doses (1,000 mcg/day) of oral methylcobalamin supplements appear to be as effective as hydroxycobalamin injections in normalizing vitamin B12 values in patients who have undergone Roux-en-Y gastric bypass surgery 87.
Vegetarians
Vegans who consume no animal products and vegetarians who consume some animal products (e.g., dairy products, eggs, or both) but not meat have a higher risk of developing vitamin B12 deficiency because natural food sources of vitamin B12 are limited to animal foods 88. Consumption of foods fortified with vitamin B12 (such as fortified nutritional yeasts) as well as vitamin B12 supplements can substantially reduce the risk of deficiency 88.
Infants of vegan women
Exclusively breastfed infants of women who consume no animal products might have very limited reserves of vitamin B12 and can develop vitamin B12 deficiency, sometimes very early in life 89. The infant’s vitamin B12 deficiency can be severe, especially if the mother’s vitamin B12 deficiency is severe or caused by pernicious anemia; sometimes, the mother’s own vitamin B12 deficiency is clinically mild and not recognized. Undetected and untreated vitamin B12 deficiency in infants can result in neurological damage, failure to thrive, developmental delays, and anemia 89, 90. The reasons include the small amounts of vitamin B12 in the breast milk of vegan mothers as well as the limited amounts of vitamin B12 crossing the placenta in these women during fetal development.
Vitamin B12 deficiency prevention
Because of potential interactions from prolonged medication use, healthcare providers should consider screening patients for vitamin B12 deficiency if they have been taking proton pump inhibitors or H2 blockers for more than 12 months, or metformin for more than four months 13. The average intake of vitamin B12 in the United States is 3.4 mcg per day, and the recommended dietary allowance is 2.4 mcg per day for adult men and nonpregnant women, and 2.6 mcg per day for pregnant women 51. Patients older than 50 years may not be able to adequately absorb dietary vitamin B12 and should consume food fortified with vitamin B12 51. Vegans and strict vegetarians should consume fortified cereals or supplements to prevent vitamin B12 deficiency. The American Society for Metabolic and Bariatric Surgery recommends that patients who have had weight loss surgery take 1 mg of oral vitamin B12 per day indefinitely 197.
Vitamin B12 deficiency signs and symptoms
Vitamin B12 deficiency affects multiple systems, and signs and symptoms vary in severity from mild fatigue to severe neurologic impairment 13. The substantial liver storage of vitamin B12 can delay signs and symptoms for up to 10 years after the onset of Vitamin B12 deficiency 198.
The signs and symptoms of vitamin B12 deficiency include 199:
- anaemia resulting from impaired red blood cell production
- loss of peripheral nerve function that can result in impaired sensation, movement or organ function
- visual disturbance
- memory loss
- psychiatric abnormalities
- temporary infertility in women
- vitamin B12 deficiency during pregnancy can result in fetal abnormalities, such as neural tube defects 200, 201, 202.
Vitamin B12 deficiency is generally characterized by a specific type of anemia called megaloblastic anemia. Anemia usually develops insidiously. It can cause fatigue (easily fatigued with exertion), palpitations, pale skin, weakness, constipation, loss of appetite, and weight loss 12, 33, 34, 12, 15. Megaloblastic anemia is often more severe than its symptoms indicate because its slow evolution allowing physiologic adaptation.
Skin hyperpigmentation, glossitis (swollen inflamed tongue) and infertility have also been reported 12, 33, 34. Neurologic signs and symptoms are caused by progressive demyelination and can include peripheral neuropathy, absence of normal neurologic reflexes (areflexia), and the loss of proprioception and vibratory sense. Areflexia (absence of normal neurologic reflexes) can be permanent if neuronal death occurs in the posterior and lateral spinal cord tracts 12, 33, 34, 203. Dementia-like disease, including episodes of psychosis, is possible with more severe and chronic vitamin B12 deficiency 12, 203. Clinical evaluation seems to show an inverse relationship between the severity of megaloblastic anemia and the degree of neurologic impairment 33.
Maternal vitamin B12 deficiency during pregnancy or while breastfeeding may lead to neural tube defects, developmental delay, failure to thrive, hypotonia, ataxia, and anemia 30, 204, 205, 206, 207. Women at high risk or with known deficiency should supplement with vitamin B12 during pregnancy or while breastfeeding 30, 204, 205, 206, 207.
Symptoms of vitamin B12 deficiency can take decades to develop, and can usually only be diagnosed by a medical professional 12, 13.
Vitamin B12 deficiency symptoms can include:
- Diarrhea or constipation
- Nausea
- Vomiting
- Fatigue, lack of energy, or lightheadedness when standing up or with exertion
- Loss of appetite
- Pale skin (mild jaundice)
- Shortness of breath, mostly during exercise
- Heartburn
- Swollen, red tongue or bleeding gums
General symptoms of anemia may include:
- extreme tiredness (fatigue)
- lack of energy (lethargy)
- breathlessness
- feeling faint
- headaches
- pale skin
- noticeable heartbeats (palpitations)
- hearing sounds coming from inside the body, rather than from an outside source (tinnitus)
- loss of appetite and weight loss
If you have anemia caused by a vitamin B12 deficiency, you may have other symptoms, such as 30, 208:
- a pale yellow tinge to your skin. In advanced anemia, severe pale skin with jaundice (due to hemolysis) produces a “peculiar lemon-yellow” skin color 125.
- vitiligo
- skin hyperpigmentation
- a sore and red tongue (glossitis)
- mouth ulcers
- pins and needles (paresthesia)
- changes in the way that you walk and move around (gait abnormalities)
- disturbed vision
- irritability
- depression
- changes in the way you think, feel and behave
- a decline in your mental abilities, such as memory, understanding and judgement (dementia)
- acute psychosis
- areflexia
- loss of proprioception and vibratory sense
- impaired sense of smell
If you have a low vitamin B12 level for a long time, you can have nervous system damage. Symptoms can include 209:
- Confusion
- Short-term memory loss
- Depression
- Loss of balance
- Numbness and tingling in the hands and feet
- Problems concentrating
- Irritability
- Hallucinations
- Delusions
- Optic nerve atrophy
Some of these symptoms can also happen in people who have a vitamin B12 deficiency but have not developed anemia.
Anemia usually develops insidiously. It is often more severe than its symptoms indicate because its slow evolution allows physiologic adaptation.
Occasionally, splenomegaly and hepatomegaly occur. Various gastrointestinal symptoms, including weight loss and poorly localized abdominal pain, may occur. Glossitis, usually described as burning of the tongue, is uncommon.
Neurologic symptoms develop independently from and often without hematologic abnormalities.
Subacute combined degeneration refers to degenerative changes in the nervous system due to Vitamin B12 deficiency; they affect mostly brain and spinal cord white matter, including the dorsal columns, the lateral corticospinal tracts, and the spinocerebellar tracts 210, 211. Demyelinating or axonal peripheral neuropathies can occur 212, 210.
In early stages, decreased position (proprioception) and vibratory sensation in the extremities is accompanied by mild to moderate weakness and hyporeflexia. In later stages, spasticity, extensor plantar responses, greater loss of position and vibratory sensation in the lower extremities, and ataxia emerge 213, 42. These deficits may develop in a stocking-glove distribution. Tactile, pain, and temperature sensations are usually spared but may be difficult to assess in the elderly. Areflexia can be permanent if neuronal death occurs in the posterior and lateral spinal cord tracts 203, 34.
Some patients are also irritable and mildly depressed. Dementia-like disease, including episodes of psychosis, paranoia (megaloblastic madness), poor memory, delirium, depression, confusion, and, at times, postural hypotension may occur in advanced cases 203, 12. The confusion may be difficult to differentiate from age-related dementias, such as Alzheimer disease.
Neurologic symptoms may develop independently from and often without hematologic abnormalities. Clinical evaluation seems to show an inverse relationship between the severity of megaloblastic anemia and the degree of neurologic impairment 15.
Megaloblastic anemia
Diminished activity of methionine synthase in vitamin B12 deficiency inhibits the regeneration of tetrahydrofolate (THF) and traps folate in a form that is not usable by the body, resulting in symptoms of folate deficiency even in the presence of adequate folate levels. Thus, in both folate and vitamin B12 deficiencies, folate is unavailable to participate in DNA synthesis. This impairment of DNA synthesis affects the rapidly dividing cells of the bone marrow earlier than other cells, resulting in the production of large, immature, hemoglobin-poor red blood cells. The resulting anemia is known as megaloblastic anemia and is the symptom for which the disease, pernicious anemia, was named 66. Supplementation with folic acid will provide enough usable folate to restore normal red blood cell formation. However, if vitamin B12 deficiency is the cause, it will persist despite the resolution of the anemia. Thus, megaloblastic anemia should not be treated with folic acid until the underlying cause has been determined 214.
Neurologic symptoms
The neurologic symptoms of vitamin B12 deficiency include numbness and tingling of the hands and, more commonly, the feet; difficulty walking; memory loss; disorientation; and dementia with or without mood changes. Although the progression of neurologic complications is generally gradual, such symptoms may not be reversed with treatment of vitamin B12 deficiency, especially if they have been present for a long time. The most common initial sign and symptom of vitamin B12 deficiency is burning or prickling sensation that is usually felt in the hands, arms, legs, or feet (paresthesia), present in 70% of patients with neurological symptoms 215. Paresthesias are described as tingling or numbness, and, in contrast with other neuropathies, typically start in hands or both distal extremities 215, 216. Other neurological manifestations may include subacute combined degeneration characterized by lesion of the posterior and lateral columns of the spinal cord leading to asthenia, spasticity, impaired vibratory and proprioceptive sensation with ataxia and extensor plantar responses 216; autonomic dysfunction (erectile and bladder dysfunction) 217; optic neuropathy with progression to visual loss (characterized by central and centrocecal scotomas) 218, and memory and mood involvement, up to dementia 95.
Neurologic complications are not always associated with megaloblastic anemia and are the only clinical symptom of vitamin B12 deficiency in about 25% of cases 65. Although vitamin B12 deficiency is known to damage the myelin sheath covering cranial, spinal, and peripheral nerves, the biochemical processes leading to neurological damage in vitamin B12 deficiency are not yet fully understood 219.
Gastrointestinal symptoms
Tongue soreness, appetite loss, and constipation have also been associated with vitamin B12 deficiency. The origins of these symptoms are unclear, but they may be related to the stomach inflammation underlying some cases of vitamin B12 deficiency and to the progressive destruction of the lining of the stomach 65.
Hyperhomocysteinemia
High levels of homocysteine in the blood (hyperhomocysteinemia) has been linked to heart disease and stroke 10. Hyperhomocysteinemia can be caused by a deficiency of either vitamin B12 or folate, and in human subjects mild (13–24 µM) and moderate (25–60 µM) hyperhomocysteinemia are also associated with mutations of MTHFR genes.
Vitamin B12 deficiency hyperhomocysteinemia may be associated with osteoporosis, depression, cognitive decline, and some forms of dementia in the elderly 10. More recently, vitamin B12 deficiency has been reported as common among patients with hyperhomocysteinemia and thrombosis 220, although the presence of a direct effect of vitamin B12 deficiency rather than mediated by hyperhomocysteinemia or other factors is uncertain. In fact, lifestyle-related factors, such as smoking status, body mass index (BMI), and physical activity, could interfere between hyperhomocysteinemia and the thromboembolism relationship 221. Moreover, the effect of lowering homocysteine levels in patients with intermediate (total homocysteine 30–100 µmol/L) or severe hyperhomocysteinemia (total homocysteine > 100 µmol/L) remains unknown 222. The cases described below report examples of vitamin B12 deficiency and hyperhomocysteinemia related to different causes.
A case of cerebral venous thrombosis secondary to hyperhomocysteinemia caused by vitamin B12 deficiency in a 32-year-old Indo-Aryan man who followed a strict vegetarian diet is reported by Kapur 223. The preliminary blood examination revealed macrocytic anemia with hemoglobin of 11.4 g/dL and mean corpuscular volume (MCV) of 110 fL 223. Peripheral blood film showed macrocytes and macro-ovalocytes with hypersegmented neutrophils; low serum cobalamin levels 68 pg/mL (200–600) with normal folate levels and total serum homocysteine
levels of 36 μmol/L (5.0–13.9) were observed 223. In addition to other treatments, the patient received parenteral cyanocobalamin 1000 μg once daily for seven days. Gradually, he regained sensorium, his power improved, and he was discharged on orally administered sodium valproate, warfarin, and methylcobalamin. Repeated investigations undertaken at six months after stopping anticoagulants showed normal serum cobalamin 364 pg/mL (200–600) and fasting total homocysteine levels 8.4 μmol/L. The authors conclude that hyperhomocysteinemia is an independent risk factor for cerebral venous thrombosis in patients with cobalamin deficiency, especially those who follow a strict vegetarian diet, and that hyperhomocysteinemia can be easily reversed with vitamin supplementation, cobalamin, and folic acid 223.
The cases of four Moroccan patients with acute vein thrombosis of different sites are reported by Ammouri 224. Three men and one woman of different ages (a 34-year-old man, a 60-year-old man, a 58-year-old man, and a 47-year-old woman) were selected. All patients presented low hemoglobin level (from 8.6 g/dL to 9.5 g/dL), low MCV (mean corpuscular volume), low cobalamin plasma level (about 60 pg/mL; normal >120 pg/mL), and high levels of plasma homocysteine (50 to 200 μmol/L; normal range <15 µmol/L) with normal folate plasma levels. For all, pernicious anemia and venous thrombosis secondary to hyperhomocysteinemia were evident. First, the authors speculated that normal folate levels may have contributed to the delay in the diagnosis of pernicious anemia, leading to severe hyperhomocysteinemia and the consequent development of vascular injury 224.
Hyperhomocysteinemia could lead to venous thrombosis by several pathways. For example, the toxic effect of homocysteine on the vascular endothelium and on the dotting cascade, as well procoagulant properties of homocysteine, including the decrease of antithrombin III binding to endothelial heparan sulfate, an increase of affinity between lipoprotein(a) and fibrin, induction of tissue factor activity in endothelial cells, and inhibition of inactivation of factor V by activated protein. In all patients, clinical and biological abnormalities disappeared upon vitamin B12 supplementation. The authors concluded that vitamin B12 supplements can rapidly correct hyperhomocysteinemia avoiding and preventing thrombotic events 224.
Tanaka et al. 222 reported a case of a 39-year-old man with inferior vena cava (IVC) thrombus. The analysis of risk factors of venous thromboembolism shown hyperhomocysteinemia (total homocysteine 83.1 µmol/L; normal range 5–15 µmol/L) due to an unbalanced diet with a deficiency of folic acid and vitamin B12. The patient was treated with both folic acid and vitamin B6/vitamin B12 supplementation in association with warfarin, inducing a significant resolution of thrombus after four weeks and no evidence of recurrent IVC thrombus at six months. The authors concluded that B vitamins and folic acid therapy might be effective in patients with severe hyperhomocysteinemia 222.
An interesting case of a 43-year-old man presenting with a two-week history of painless ascending sensory disturbances, suspected to be suffering from acute inflammatory polyneuropathy, is reported by Ulrich et al. 225. On clinical examination, deep tendon reflexes were preserved, muscle strength was 5/5 everywhere, and gait was ataxic. Initial laboratory assessment showed nearly normal holotranscobalamin (43 pmol/L; pmol/L normal >50 pmol/L), suggesting no vitamin B12 deficiency. Surprisingly, further investigation showed high homocysteine (48.5 µmol/L; normal <10 µmol/L), suggesting an impairment of vitamin B12-dependent metabolism leading to the diagnosis of subacute combined degeneration. The patient remembered having taken tablets containing cobalamin for three days before hospitalization. The authors concluded that holotranscobalamin can be rapidly normalized during supplementation and the analysis of methylmalonic acid (MMA) and homocysteine might help to detect B12 deficiency in patients who recently started supplementation.
A case of a 24-year-old male with unprovoked bilateral submassive pulmonary emboli with a high level of homocysteine without anemia is reported by Kovalenko et al. 226. Complete blood count showed a MCV of 104fL without anemia, and homocysteine level was 41.3 μmol/L (normal 4.0–13.7 μmol/L). Workup for macrocytosis was notable for low vitamin B12 (72 pg/mL) and folate (2.1 ng/mL) levels. After vitamin B12 supplementation, serum homocysteine levels did not decrease to normal values. The authors speculated that a poor absorption of B vitamins due to a small bowel resection two years before and excessive alcohol consumption could have impaired the results. Another case associated with alcoholism was previously described by Goette et al. 227. The authors described a rare case of a 32-year-old man with severe hyperhomocysteinemia underlying a probable cause of thromboembolic complications 227. The patient did not have a history of cardiovascular disease, but he had at least a six-month history of alcohol abuse at least six months before hospital admission. Laboratory assays showed abnormalities in liver functions, vitamin B12 (226 pg/mL; normal range 150–675 pg/mL) and folate (1.6 μg/L; normal range 1.4–11.8 μg/L) were low but within normal range, while serum homocysteine was at least 12 times higher than normal (173 μmol/L). The patient was treated with 5 mg oral folic acid and 20 mg oral vitamin B6 daily. Vitamin supplementation was then adapted and integrated with other drugs, such as weight-adapted low molecular weight heparin and L-arginine. For some patients, the authors suggested the screening for hyperhomocysteinemia in association with endothelial dysfunction markers as appropriate 227.
Elevated plasma homocysteine is involved in cognitive decline, including Alzheimer’s disease, mild cognitive impairment, and dementia, especially in elderly subjects. McCaddon 228 reported seven cases of older patients (four women aged 78 years, 84 years, 77 years and 87 years, 84 years old, and two men 71 and 75 years old). They presented with cognitive impairment and/or depression and dementia 228. Each had different vitamin B12 status with hyperhomocysteinemia. Treatment with N-acetylcysteine, together with B vitamin supplements, improves cognitive status in hyperhomocysteinemic patients. The authors concluded that it could be important to evaluate inadequate vitamin B12 and folate metabolism in subjects with cognitive diseases, underlining the importance of clinical trials to evaluate the beneficial effects of a synergistic approach to cognitively impaired hyperhomocysteinaemic patients 228.
Vitamin B12 deficiency complications
As most cases of vitamin B12 deficiency can be easily and effectively treated, complications are rare. But complications can occasionally develop, particularly if you have been vitamin B12 deficient for some time.
Vitamin B12 deficiency complications can include 229:
- Heart failure due to the anemia
- Severe disabling neurological deficits
- Risk of gastric cancer
- Risk of developing an autoimmune disorder like type 1 diabetes, myasthenia gravis, Hashimoto disease, or rheumatoid arthritis.
Anemia complications
All types of anaemia, regardless of the cause, can lead to heart and lung complications as the heart struggles to pump oxygen to the vital organs. A lack of vitamin B12 with or without anemia can cause complications.
Adults with severe anemia are at risk of developing:
- an abnormally fast heartbeat (tachycardia)
- heart failure, where the heart fails to pump enough blood around the body at the right pressure
Neurological problems
A lack of vitamin B12 can cause neurological problems, which affect your nervous system, such as:
- vision problems
- memory loss
- pins and needles (paraesthesia)
- loss of physical co-ordination (ataxia), which can affect your whole body and cause difficulty speaking or walking
- damage to parts of the nervous system (peripheral neuropathy), particularly in the legs
If neurological problems do develop, they may be irreversible.
Stomach cancer
If you have a vitamin B12 deficiency caused by pernicious anemia, a condition where your immune system attacks healthy cells in your stomach, your risk of developing stomach cancer is increased.
Neural tube defects
If you’re pregnant, not having enough vitamin B12 can increase the risk of your baby developing a serious birth defect known as a neural tube defect. The neural tube is a narrow channel that eventually forms the brain and spinal cord.
Examples of neural tube defects include:
- Spina bifida – where the baby’s spine does not develop properly
- Anencephaly – where a baby is born without parts of the brain and skull
- Encephalocele – where a membrane or skin-covered sac containing part of the brain pushes out of a hole in the skull
Infertility
Vitamin B12 deficiency can sometimes lead to temporary infertility, an inability to conceive. Infertility usually improves with appropriate vitamin B12 treatment.
Effects of nitrous oxide
Nitrous oxide (N2O), commonly known as ‘laughing gas’, is a type of anesthetic used in dental treatments and childbirth. Using nitrous oxide can reduce the levels of vitamin B12 in your body. Nitrous oxide oxidizes and inactivates vitamin B12, thus inhibiting both of the vitamin B12-dependent enzymes, and can produce many of the clinical features of vitamin B12 deficiency, such as megaloblastic anemia or neuropathy 46. Since nitrous oxide is commonly used for surgery and childbirth, some experts feel vitamin B12 deficiency should be ruled out prior to its use 194, 179. If you are pregnant and have vitamin B12 deficiency, discuss with your doctor or midwife whether you will be able to use nitrous oxide during labor.
Vitamin B12 deficiency diagnosis
Your health care provider will perform a physical exam. This may reveal problems with your reflexes. It is important to remember that severe neurologic disease may occur without anemia or macrocytosis. Figure 5 presents an approach to diagnosing vitamin B12 deficiency and pernicious anemia 143.
- To screen for vitamin B12 deficiency, your doctor may order blood tests to see whether you have low hemoglobin or vitamin B12 levels. Complete blood test checking for anemia and vitamin B-12 and folate levels 33, 230, 35, 231. Bone marrow suppression is common and potentially affects all cell lines, with megaloblastic anemia being most common 12, 33, 34. The resultant abnormal erythropoiesis can trigger other notable abnormal laboratory findings, such as decreased haptoglobin levels, high lactate dehydrogenase levels, and elevated reticulocyte count 12, 33, 34.
- Vitamin B12 deficiency results in impairment of the activities of vitamin B12-requiring enzymes. Impaired activity of methionine synthase results in elevated homocysteine levels, while impaired activity of L-methylmalonyl-CoA mutase results in increased levels of a metabolite of methylmalonyl-CoA called methylmalonic acid (MMA). While individuals with mild vitamin B12 deficiency may not experience symptoms, blood levels of homocysteine and/or methylmalonic acid (MMA) may be elevated 194. The Schilling test, which was once the diagnostic standard for pernicious anemia, is no longer available in the United States.
- Patients diagnosed with vitamin B12 deficiency whose history and physical examination do not suggest an obvious dietary or malabsorptive etiology should be tested for pernicious anemia with anti-intrinsic factor antibodies, particularly if other autoimmune disorders are present 12, 33, 34, 143. Patients with pernicious anemia may have hematologic findings consistent w ith normocytic anemia 12. If anti-intrinsic factor results are negative but suspicion for pernicious anemia remains, an elevated serum gastrin level is consistent with the diagnosis 33.
To date, there is no consensus about the exact definition of vitamin B12 deficiency 232. There is still a significant debate within the scientific community about the specific cut-off values that should be applied to define a low vitamin B12 status and about the definition of the best biomarker or combination of biomarkers to assess vitamin B12 status 232, 21. Varying cut-off values invariably lead to underestimating or overestimating the incidence of vitamin B12 deficiency 176. With regard to the definition of an optimal vitamin B12 status, a low vitamin B12 status (frank vitamin B12 deficiency) is generally defined as total serum vitamin B12 levels of < 148 pmol/L, with levels between 148 and 221 pmol/L being considered as “borderline” or suggestive of “marginal deficiency” 20.
In light of the above remarks, measurement of functional biomarkers of vitamin B12 status (homocysteine and methylmalonic acid [MMA]) may be useful to confirm the diagnosis of true vitamin B12 deficiency, particularly in the presence of low-normal total serum vitamin B12 levels and/or clinical suspicion of vitamin B12 deficiency 232. Therefore, total vitamin B12, its bioactive protein-bound form holotranscobalamin (HoloTC), homocysteine and methylmalonic acid (MMA) are the preferred serum biomarkers to accurately assess vitamin B12 status 21. However, it is worth noting that serum levels of homocysteine and methylmalonic acid (MMA) can be elevated even in the presence of folate deficiency, which can also be associated with macrocytic anemia and thereby confused with vitamin B12 deficiency 176. Therefore, measurement of serum folate, MMA and homocysteine levels can help to distinguish vitamin B12 deficiency from folate deficiency. Serum levels of both homocysteine and MMA are often elevated in the presence of true vitamin B12 deficiency. Conversely, homocysteine levels are elevated but MMA levels are normal in the presence of folate deficiency 233. Yet, it is also worth remembering that both homocysteine and MMA levels can be elevated in the presence of kidney disease 232.
Figure 6. Vitamin B12 deficiency diagnosis
Footnote: Suggested approach to the patient with suspected vitamin B12 deficiency.
[Source 13 ]Table 5 lists the relative sensitivities and specificities of various laboratory tests 234
Table 5. Vitamin B12 deficiency laboratory tests sensitivities and specificities
[Source 13 ]The diagnosis of vitamin B12 deficiency is based mainly on complete blood count and vitamin B-12 and folate levels. Complete blood count usually detects megaloblastic anemia. Tissue deficiency and macrocytic indexes may precede the development of anemia. The diagnosis of vitamin B12 deficiency is based mainly on blood measurements of serum vitamin B12 level less than 200 pg/mL (148 pmol/L), complemented with second‐line tests including total homocysteine and methylmalonic acid levels, which are metabolic indicators of vitamin B12 deficiency 235. A serum vitamin B12 level less than 150 pg/mL (< 111 pmol/L) is diagnostic for vitamin B-12 deficiency 12, 33. Serum vitamin B12 levels may be artificially elevated in patients with alcoholism, liver disease, or cancer because of decreased hepatic clearance of transport proteins and resultant higher circulating levels of vitamin B12; physicians should use caution when interpreting laboratory results in these patients 36, 37. In patients with a normal or low-normal serum vitamin B12 level, complete blood count results demonstrating macrocytosis, or suspected clinical manifestations, a serum methylmalonic acid (MMA) level is an appropriate next step and is a more direct measure of vitamin B12’s physiologic activity 143, 34, 12, 33. Although not clinically validated or available for widespread use, measurement of holotranscobalamin, the metabolically active form of vitamin B12, is an emerging method of detecting deficiency 143.
The folate level is also measured because vitamin B12 deficiency must be differentiated from folate deficiency as a cause of megaloblastic anemia; folate supplementation can mask vitamin B12 deficiency and may alleviate megaloblastic anemia but allow the neurologic deficits to progress or even accelerate.
Studies have indicated that an estimated 20% of people can present with neuropsychiatric symptoms in the absence of hematological abnormalities 236.
When clinical judgment suggests vitamin B12 deficiency but the vitamin B12 level is low-normal (200 to 350 pg/mL [145 to 260 pmol/L]) or hematologic indexes are normal, other tests can be done. They include measuring the following:
- Serum methylmalonic acid (MMA) levels: An elevated MMA level supports vitamin B12 deficiency but may be due to renal failure. Methylmalonic acid (MMA) levels can also be used to monitor the response to treatment. Methylmalonic acid levels remain normal in folate deficiency.
- Homocysteine levels: Levels may be elevated with either vitamin B12 or folate deficiency.
- Less commonly, holotranscobalamin 2 (transcobalamin 2–B12 complex) content: When holotranscobalamin 2 is < 40 pg/mL (< 30 pmol/L), Vitamin B-12 is deficient.
After Vitamin B-12 deficiency is diagnosed, additional tests (eg, Schilling test) may be indicated for younger adults but usually not for the elderly. Unless dietary Vitamin B-12 is obviously inadequate, serum gastrin levels or autoantibodies to intrinsic factor may be measured; sensitivity and specificity of these tests may be poor.
- Schilling test
The Schilling test is useful only if diagnosing intrinsic factor deficiency is important, as in classic pernicious anemia. This test is not necessary for most elderly patients. The Schilling test measures absorption of free radiolabeled Vitamin B-12. Radiolabeled Vitamin B-12 is given orally, followed in 1 to 6 h by 1000 mcg (1 mg) of parenteral Vitamin B-12, which reduces uptake of radiolabeled Vitamin B-12 by the liver. Absorbed radiolabeled Vitamin B-12 is excreted in urine, which is collected for 24 h. The amount excreted is measured, and the percentage of total radiolabeled Vitamin B-12 is determined. If absorption is normal, ≥ 9% of the dose given appears in the urine. Reduced urinary excretion (< 5% if kidney function is normal) indicates inadequate Vitamin B-12 absorption. Improved absorption with the subsequent addition of intrinsic factor to radiolabeled Vitamin B-12 confirms the diagnosis of pernicious anemia.
The test is often difficult to do or interpret because of incomplete urine collection or renal insufficiency. In addition, because the Schilling test does not measure absorption of protein-bound Vitamin B-12, the test does not detect defective liberation of Vitamin B-12 from foods, which is common among the elderly. The Schilling test repletes Vitamin B-12 and can mask deficiency, so it should be done only after all other diagnostic tests and therapeutic trials.
If malabsorption is identified, the Schilling test can be repeated after a 2-wk trial of an oral antibiotic. If antibiotic therapy corrects malabsorption, the likely cause is intestinal overgrowth of bacteria (eg, blind-loop syndrome).
Vitamin B12 deficiency test
Diagnosis of Vitamin B-12 deficiency is based on complete blood count and Vitamin B-12 and folate levels. Complete blood count usually detects megaloblastic anemia. Tissue deficiency and macrocytic indexes may precede the development of anemia. A Vitamin B-12 level < 200 pg/mL (< 145 pmol/L) indicates Vitamin B-12 deficiency. The folate level is measured because Vitamin B-12 deficiency must be differentiated from folate deficiency as a cause of megaloblastic anemia; folate supplementation can mask Vitamin B-12 deficiency and may alleviate megaloblastic anemia but allow the neurologic deficits to progress or even accelerate.
When clinical judgment suggests Vitamin B-12 deficiency but the Vitamin B-12 level is low-normal (200 to 350 pg/mL [145 to 260 pmol/L]) or hematologic indexes are normal, other tests can be done. They include measuring the following:
- Serum methylmalonic acid (MMA) levels: An elevated MMA level supports Vitamin B-12 deficiency but may be due to renal failure. Methylmalonic acid (MMA) levels can also be used to monitor the response to treatment. Methylmalonic acid levels remain normal in folate deficiency.
- Homocysteine levels: Levels may be elevated with either Vitamin B-12 or folate deficiency.
- Less commonly, holotranscobalamin II (transcobalamin II–B12 complex) content: When holotranscobalamin II is < 40 pg/mL (< 30 pmol/L), Vitamin B-12 is deficient.
After Vitamin B-12 deficiency is diagnosed, additional tests (eg, Schilling test) may be indicated for younger adults but usually not for the elderly. Unless dietary Vitamin B-12 is obviously inadequate, serum gastrin levels or autoantibodies to intrinsic factor may be measured; sensitivity and specificity of these tests may be poor.
Schilling test
The Schilling test is useful only if diagnosing intrinsic factor deficiency is important, as in classic pernicious anemia. This test is not necessary for most elderly patients. The Schilling test measures absorption of free radiolabeled Vitamin B-12. Radiolabeled Vitamin B-12 is given orally, followed in 1 to 6 h by 1000 mcg (1 mg) of parenteral Vitamin B-12, which reduces uptake of radiolabeled Vitamin B-12 by the liver. Absorbed radiolabeled Vitamin B-12 is excreted in urine, which is collected for 24 h. The amount excreted is measured, and the percentage of total radiolabeled Vitamin B-12 is determined. If absorption is normal, ≥ 9% of the dose given appears in the urine. Reduced urinary excretion (< 5% if kidney function is normal) indicates inadequate Vitamin B-12 absorption. Improved absorption with the subsequent addition of intrinsic factor to radiolabeled Vitamin B-12 confirms the diagnosis of pernicious anemia.
The test is often difficult to do or interpret because of incomplete urine collection or renal insufficiency. In addition, because the Schilling test does not measure absorption of protein-bound Vitamin B-12, the test does not detect defective liberation of Vitamin B-12 from foods, which is common among the elderly. The Schilling test repletes Vitamin B-12 and can mask deficiency, so it should be done only after all other diagnostic tests and therapeutic trials.
If malabsorption is identified, the Schilling test can be repeated after a 2-week trial of an oral antibiotic. If antibiotic therapy corrects malabsorption, the likely cause is intestinal overgrowth of bacteria (eg, blind-loop syndrome).
Vitamin B12 deficiency treatment
Vitamin B12 deficiency can be treated with intramuscular injections of cyanocobalamin or hydroxocobalamin or oral vitamin B12 therapy. However, depending on the cause of the B12 deficiency, the duration and route of treatment vary. In patients who are B12 deficient due to a strict vegan diet, an oral supplement of B12 is adequate for repletion 39. Vitamin B12 1000 to 2000 mcg (1 to 2 mg) orally can be given once/day to patients who do not have severe deficiency or neurologic symptoms or signs. A 2018 Cochrane review included three randomized controlled trials (RCTs) that compared very high doses (1,000–2,000 mcg) of oral with intramuscular vitamin B12 for vitamin B12 deficiency in a total of 153 participants 23. The evidence from these studies, although of low quality, showed that the ability of high oral doses of vitamin B12 supplements to normalize serum vitamin B12 was similar to that of intramuscular vitamin B12. The British Society for Haematology recommends intramuscular vitamin B12 for severe deficiency and malabsorption syndromes, whereas oral replacement may be considered for patients with asymptomatic, mild disease with no absorption or compliance concerns 38.
For more severe deficiency, vitamin B12 1 mg IM (intramuscularly) is usually given 1 to 4 times/week for several weeks until hematologic abnormalities are corrected; then it is given once/month. Approximately 10% of the standard injectable dose of 1 mg is absorbed, which allows for rapid replacement in patients with severe deficiency or severe neurologic sy mptoms 33. Guidelines from the British Society for Haematology recommend injections three times per week for two weeks in patients without neurologic deficits 143. If neurologic deficits are present, injections should be given every other day for up to three weeks or until no further improvement is noted. Table 4 lists the usual times until improvement for abnormalities associated with vitamin B12 deficiency 9. In general, patients with an irreversible cause should be treated indefinitely, whereas those with a reversible cause should be treated until the deficiency is corrected and symptoms resolve 12. If vitamin B12 deficiency coexists with folate deficiency, vitamin B12 should be replaced first to prevent subacute combined degeneration of the spinal cord 12. The British Society for Haematology does not recommend retesting vitamin B12 levels after treatment has been initiated, and no guidelines address the optimal interval for screening high-risk patients 143.
Although hematologic abnormalities are usually corrected within 6 week (reticulocyte count should improve within 1 week), resolution of neurologic symptoms may take much longer. Neurologic symptoms that persist for months or years become irreversible. In most elderly people with vitamin B-12 deficiency and dementia, cognition does not improve after treatment.
There are 2 types of vitamin B12 injections:
- Hydroxocobalamin
- Cyanocobalamin
Typically, vitamin B12 deficiency is treated with intramuscular injections of cyanocobalamin or hydroxocobalamin, because this method bypasses any barriers to absorption. Hydroxocobalamin is usually the recommended option as it stays in the body for longer. Approximately 10% of the standard injectable dose of 1 mg is absorbed, which allows for rapid replacement in patients with severe deficiency or severe neurologic symptoms 15. Guidelines from the British Society for Haematology recommend injections three times per week for two weeks in patients without neurologic deficits 38. If neurologic deficits are present, injections should be given every other day for up to three weeks or until no further improvement is noted.
If vitamin B12 deficiency coexists with folate deficiency, vitamin B12 should be replaced first to prevent subacute combined degeneration of the spinal cord 12.
Although hematologic abnormalities are usually corrected within 6 week (reticulocyte count should improve within 1 week), resolution of neurologic symptoms may take much longer. Neurologic symptoms that persist for months or years become irreversible. In most elderly people with Vitamin B-12 deficiency and dementia, cognition does not improve after treatment. Table 6 lists the usual times until improvement for abnormalities associated with vitamin B12 deficiency 9.
Vitamin B-12 treatment must be continued for life unless the pathophysiologic mechanism for the deficiency is corrected.
Infants of vegan mothers should receive supplemental Vitamin B-12 from birth.
In patients with a deficiency in intrinsic factor (IF), either due to pernicious anemia or gastric bypass surgery, a parenteral dose of vitamin B12 is recommended, as oral B12 will not be fully absorbed due to the lack of intrinsic factor. A dose of 1000 mcg of B12 via the intramuscular route is recommended once a month 229. In newly diagnosed patients, 1000 mcg of vitamin B12 is given intramuscularly once a week for four weeks to replenish stores before switching to once-monthly dosing 229. Studies have shown that at doses high enough to fully saturate intestinal B12 receptors, oral B12 is also effective, despite a lack of intrinsic factor 229.
In anyone at risk of developing a B12 deficiency, such as patients with Crohn’s disease or celiac disease, routine monitoring of B12 should be performed. If the severity of the disease worsens and B12 levels begin to decline, treatment is then started. However, prophylactic treatment before B12 levels fall is not indicated 237, 238, 239.
Table 6. Usual times until improvement for abnormalities associated with vitamin B12 deficiency
[Source 13 ]If your vitamin B12 deficiency is caused by a lack of the vitamin B12 in your diet, you may be advised to take vitamin B12 tablets every day between meals. Or you may need to have an vitamin B12 injection of hydroxocobalamin twice a year.
People who find it difficult to get enough vitamin B12 in their diets, such as those following a vegan diet, may need vitamin B12 tablets for life.
Although it’s less common, people with vitamin B12 deficiency caused by a prolonged poor diet may be advised to stop taking the tablets once their vitamin B12 levels have returned to normal and their diet has improved.
Good sources of vitamin B12 include:
- meat
- salmon and cod
- milk and other dairy products
- eggs
If you’re a vegetarian or vegan, or are looking for alternatives to meat and dairy products, there are other foods that contain vitamin B12, such as yeast extract (including Marmite), as well as some fortified breakfast cereals and soy products.
Check the nutrition labels while food shopping to see how much vitamin B12 different foods contain.
If your vitamin B12 deficiency is not caused by a lack of vitamin B12 in your diet, you’ll usually need to have an injection of hydroxocobalamin every 2 to 3 months for the rest of your life 240.
If you have had neurological symptoms that affect your nervous system, such as numbness or tingling in your hands and feet, caused by a vitamin B12 deficiency, you’ll be referred to a hematologist and may need to have vitamin B12 injections every 2 months. Your hematologist will advise on how long you need to keep taking the vitamin B12 injections.
For injections of vitamin B12 given in the UK, hydroxocobalamin is preferred to an alternative called cyanocobalamin 240. This is because hydroxocobalamin stays in the body for longer.
Monitoring your condition
It is essential for your healthcare provider to confirm vitamin B12 deficiency before starting therapy and a follow-up plan for the monitoring your response 241. To ensure your treatment is working, you may need to have further blood tests. A blood test is often carried out around 7 to 10 days after starting treatment to assess whether treatment is working. If you have severe anemia associated with vitamin B12 deficiency, your blood response should lead to a marked increase in reticulocytes (precursors of red blood cells) by one-to-two weeks 241. In mild vitamin B12 deficiency, this is less important, and follow-up should be done at two-to-three months after initiation of hydroxocobalamin 241. These measurements should include vitamin B12 levels as well as homocysteine and methylmalonic acid (MMA) levels 242. Both homocysteine and methylmalonic acid (MMA) are indicators for vitamin B12 levels and demonstrate your response to hydroxocobalamin 243. Most people who have had a vitamin B12 or folate deficiency will not need further monitoring unless their symptoms return or their treatment is ineffective 244.
Vitamin B12 deficiency prognosis
For patients who are promptly treated with vitamin B12, the prognosis is good. In general, younger patients have better outcomes compared to older individuals. The best response is obtained in people with the absence of severe neurological deficits. Therefore, it is important to start vitamin B12 treatment early. Nerve damage can be permanent if vitamin B12 treatment does not start within 6 months of symptoms. Although vitamin B12 supplementation stops progression and improves neurologic deficits in most patients with subacute combined degeneration, evidence shows complete resolution only occurs in a small percentage of them 172. A 2006 observational study evaluating 57 patients with subacute combined degeneration reported only 14% clinical resolution after B12 treatment 172. Still, the study reported that of these patients, 86% had at least some clinical improvement. Subgroup analysis revealed that the absence of sensory dermatomal deficit, negative Romberg and Babinski signs, age less than 50 years, and less than or equal to 7-segment involvement on magnetic resonance imaging correlated with complete resolution of neurologic symptoms 172. This study highlights the importance of early diagnosis and treatment of vitamin B12 deficiency, as patients with severe or prolonged neurological symptoms tend to have persistent symptoms despite treatment.
References- Herbert V. Vitamin B-12 in Present Knowledge in Nutrition. 17th ed. Washington, DC: International Life Sciences Institute Press, 1996.
- Combs G. Vitamin B-12 in The Vitamins. New York: Academic Press, Inc., 1992.
- Bernard MA, Nakonezny PA, Kashner TM. The effect of vitamin B12 deficiency on older veterans and its relationship to health. J Am Geriatr Soc. 1998 Oct;46(10):1199-206. doi: 10.1111/j.1532-5415.1998.tb04534.x
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B-12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press, 1998.
- Healton EB, Savage DG, Brust JC, Garrett TF, Lindenbaum J. Neurological aspects of cobalamin deficiency. Medicine 1991;70:229-44.
- Bottiglieri T. Folate, vitamin B12, and neuropsychiatric disorders. Nutr Rev. 1996 Dec;54(12):382-90. doi: 10.1111/j.1753-4887.1996.tb03851.x
- Clarke R. B-vitamins and prevention of dementia. Proc Nutr Soc. 2008 Feb;67(1):75-81. doi: 10.1017/S0029665108006046
- Bjørke Monsen AL, Ueland PM. Homocysteine and methylmalonic acid in diagnosis and risk assessment from infancy to adolescence. Am J Clin Nutr. 2003 Jul;78(1):7-21. doi: 10.1093/ajcn/78.1.7
- Carmel R. How I treat cobalamin (vitamin B12) deficiency. Blood. 2008 Sep 15;112(6):2214-21. doi: 10.1182/blood-2008-03-040253
- Azzini E, Raguzzini A, Polito A. A Brief Review on Vitamin B12 Deficiency Looking at Some Case Study Reports in Adults. Int J Mol Sci. 2021 Sep 7;22(18):9694. doi: 10.3390/ijms22189694
- U.S. Department of Agriculture, Agricultural Research Service . What We Eat in America, 2017–2018. External Link Disclaimer. U.S. Department of Agriculture, Agricultural Research Service; Beltsville, MD, USA: 2020.
- Hunt A, Harrington D, Robinson S. Vitamin B12 deficiency. BMJ. 2014 Sep 4;349:g5226. doi: 10.1136/bmj.g5226
- Langan RC, Goodbred AJ. Vitamin B12 Deficiency: Recognition and Management. Am Fam Physician. 2017 Sep 15;96(6):384-389. https://www.aafp.org/pubs/afp/issues/2017/0915/p384.html
- Carmel R. Cobalamin (vitamin B12). In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:369-89.
- Stabler SP. Vitamin B12. In: Marriott BP, Birt DF, Stallings VA, Yates AA, eds. Present Knowledge in Nutrition. 11th ed. Washington, DC: Elsevier; 2020:257-71.
- Clarke R. B-vitamins and prevention of dementia. Plenary Lecture. Proceedings of the Nutrition Society 2008 Feb;67(1):75-81. doi:10.1017/S0029665108006046
- Laird E, O’Halloran AM, Molloy AM, Healy M, Hernandez B, O’Connor D, Kenny RA, Briggs R. Low vitamin B12 but not folate is associated with incident depressive symptoms in community-dwelling older adults: a 4 year longitudinal study. Br J Nutr. 2021 Dec 13:1-22. doi: 10.1017/S0007114521004748
- Mikkelsen K, Stojanovska L, Apostolopoulos V. The Effects of Vitamin B in Depression. Curr Med Chem. 2016;23(38):4317-4337. doi: 10.2174/0929867323666160920110810
- Yanjun Wu, Liming Zhang, Suyun Li, Dongfeng Zhang, Associations of dietary vitamin B1, vitamin B2, vitamin B6, and vitamin B12 with the risk of depression: a systematic review and meta-analysis, Nutrition Reviews, Volume 80, Issue 3, March 2022, Pages 351–366, https://doi.org/10.1093/nutrit/nuab014
- Green R, Allen LH, Bjørke-Monsen AL, Brito A, Guéant JL, Miller JW, Molloy AM, Nexo E, Stabler S, Toh BH, Ueland PM, Yajnik C. Vitamin B12 deficiency. Nat Rev Dis Primers. 2017 Jun 29;3:17040. doi: 10.1038/nrdp.2017.40. Erratum in: Nat Rev Dis Primers. 2017 Jul 20;3:17054.
- Hannibal L, Lysne V, Bjørke-Monsen AL, Behringer S, Grünert SC, Spiekerkoetter U, Jacobsen DW, Blom HJ. Biomarkers and Algorithms for the Diagnosis of Vitamin B12 Deficiency. Front Mol Biosci. 2016 Jun 27;3:27. doi: 10.3389/fmolb.2016.00027. Erratum in: Front Mol Biosci. 2017 Aug 08;4:53.
- Bailey RL, Carmel R, Green R, Pfeiffer CM, Cogswell ME, Osterloh JD, Sempos CT, Yetley EA. Monitoring of vitamin B-12 nutritional status in the United States by using plasma methylmalonic acid and serum vitamin B-12. Am J Clin Nutr. 2011 Aug;94(2):552-61. doi: 10.3945/ajcn.111.015222
- Wang H, Li L, Qin LL, Song Y, Vidal-Alaball J, Liu TH. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency. Cochrane Database Syst Rev. 2018 Mar 15;3(3):CD004655. doi: 10.1002/14651858.CD004655.pub3
- Watanabe F, Yabuta Y, Tanioka Y, Bito T. Biologically active vitamin B12 compounds in foods for preventing deficiency among vegetarians and elderly subjects. J Agric Food Chem. 2013 Jul 17;61(28):6769-75. doi: 10.1021/jf401545z
- Pawlak R, Parrott SJ, Raj S, Cullum-Dugan D, Lucus D. How prevalent is vitamin B(12) deficiency among vegetarians? Nutr Rev. 2013 Feb;71(2):110-7. doi: 10.1111/nure.12001
- Pawlak R. Is vitamin B12 deficiency a risk factor for cardiovascular disease in vegetarians? Am J Prev Med. 2015 Jun;48(6):e11-26. doi: 10.1016/j.amepre.2015.02.00
- Sakyi S.A., Laing E.F., Mantey R., Kwarteng A., Owiredu E.-W., Dadzie R.E., Amoani B., Opoku S., Afranie B.O., Boakye D. Profiling immuno-metabolic mediators of vitamin B12 deficiency among metformin-treated type 2 diabetic patients in Ghana. PLoS ONE. 2021;16:e0249325. doi: 10.1371/journal.pone.0249325
- Green R., Allen L.H., Bjørke-Monsen A.L., Britto A., Guéant J.L., Miller J.W., Molloy A.M., Nexo E., Stabler S., Toh B.H., et al. Vitamin B12 deficiency. Nat. Rev. Dis. Primers. 2017;3:17040. doi: 10.1038/nrdp.2017.40
- Pawlak R., E Lester S., Babatunde T. The prevalence of cobalamin deficiency among vegetarians assessed by serum vitamin B12: A review of literature. Eur. J. Clin. Nutr. 2014;68:541–548. doi: 10.1038/ejcn.2014.46
- Langan RC, Zawistoski KJ. Update on vitamin B12 deficiency. Am Fam Physician. 2011 Jun 15;83(12):1425-30. https://www.aafp.org/pubs/afp/issues/2011/0615/p1425.html
- de Jager J, Kooy A, Lehert P, Wulffelé MG, van der Kolk J, Bets D, Verburg J, Donker AJ, Stehouwer CD. Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. BMJ. 2010 May 20;340:c2181. doi: 10.1136/bmj.c2181
- Lam JR, Schneider JL, Zhao W, Corley DA. Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. JAMA. 2013 Dec 11;310(22):2435-42. doi: 10.1001/jama.2013.280490
- Stabler SP. Clinical practice. Vitamin B12 deficiency. N Engl J Med. 2013 Jan 10;368(2):149-60. doi: 10.1056/NEJMcp1113996
- Dali-Youcef N, Andrès E. An update on cobalamin deficiency in adults. QJM. 2009 Jan;102(1):17-28. doi: 10.1093/qjmed/hcn138
- Kaferle J, Strzoda CE. Evaluation of macrocytosis. Am Fam Physician. 2009 Feb 1;79(3):203-8. https://www.aafp.org/pubs/afp/issues/2009/0201/p203.html
- Arendt JF, Nexo E. Cobalamin related parameters and disease patterns in patients with increased serum cobalamin levels. PLoS One. 2012;7(9):e45979. doi: 10.1371/journal.pone.0045979
- Andrès E, Serraj K, Zhu J, Vermorken AJ. The pathophysiology of elevated vitamin B12 in clinical practice. QJM. 2013 Jun;106(6):505-15. doi: 10.1093/qjmed/hct051
- Devalia, V., Hamilton, M.S., Molloy, A.M. and (2014), Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol, 166: 496-513. https://doi.org/10.1111/bjh.12959
- Vitamin B12. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional
- https://calgaryguide.ucalgary.ca/vitamin-b12-deficiency/
- Stoopler ET, Kuperstein AS. Glossitis secondary to vitamin B12 deficiency anemia. CMAJ. 2013 Sep 3;185(12):E582. doi: 10.1503/cmaj.120970
- Cavalcoli F, Zilli A, Conte D, Massironi S. Micronutrient deficiencies in patients with chronic atrophic autoimmune gastritis: A review. World J Gastroenterol. 2017 Jan 28;23(4):563-572. doi: 10.3748/wjg.v23.i4.563
- Chanarin I. Adverse effects of increased dietary folate. Relation to measures to reduce the incidence of neural tube defects. Clin Invest Med 1994;17:244-52. https://www.ncbi.nlm.nih.gov/pubmed/7924000?dopt=Abstract
- Clarke R. B-vitamins and prevention of dementia. Proc Nutr Soc 2008;67:75-81. https://www.ncbi.nlm.nih.gov/pubmed/18234134?dopt=Abstract
- Johnson MA. If high folic acid aggravates Vitamin B-12 deficiency what should be done about it? Nutr Rev 2007;65:451-8. https://www.ncbi.nlm.nih.gov/pubmed/17972439?dopt=Abstract
- Vitamin B12. https://lpi.oregonstate.edu/mic/vitamins/vitamin-B12
- Herbert V, Das K. Vitamin B-12 in Modern Nutrition in Health and Disease. 8th ed. Baltimore, MD: Williams & Wilkins, 1994.
- Zittoun J, Zittoun R. Modern clinical testing strategies in cobalamin and folate deficiency. Semin Hematol. 1999 Jan;36(1):35-46.
- Thakkar K, Billa G. Treatment of vitamin B12 deficiency-methylcobalamine? Cyancobalamine? Hydroxocobalamin?-clearing the confusion. Eur J Clin Nutr. 2015 Jan;69(1):1-2. doi: 10.1038/ejcn.2014.165
- Brody T. Nutritional Biochemistry. 2nd ed. San Diego: Academic Press; 1999.
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B(6), Folate, Vitamin B(12), Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academies Press; 1998. Available from: https://www.ncbi.nlm.nih.gov/books/NBK114310/ doi: 10.17226/6015
- Carmel R. Cobalamin (Vitamin B-12). In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, eds. Modern Nutrition in Health and Disease. Philadelphia: Lippincott Williams & Wilkins; 2006:482-497.
- Paul C, Brady DM. Comparative Bioavailability and Utilization of Particular Forms of B12 Supplements With Potential to Mitigate B12-related Genetic Polymorphisms. Integr Med (Encinitas). 2017 Feb;16(1):42-49. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5312744
- Al Amin ASM, Gupta V. Vitamin B12 (Cobalamin) [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559132
- Klee GG. Cobalamin and folate evaluation: measurement of methylmalonic acid and homocysteine vs vitamin B(12) and folate. Clin Chem. 2000 Aug;46(8 Pt 2):1277-83.
- Guéant JL, Safi A, Aimone-Gastin I, Rabesona H, Bronowicki JP, Plénat F, Bigard MA, Haertlé T. Autoantibodies in pernicious anemia type I patients recognize sequence 251-256 in human intrinsic factor. Proc Assoc Am Physicians. 1997 Sep;109(5):462-9.
- Kapadia CR. Vitamin B12 in health and disease: part I–inherited disorders of function, absorption, and transport. Gastroenterologist. 1995 Dec;3(4):329-44.
- Johnson MA. If high folic acid aggravates vitamin B12 deficiency what should be done about it? Nutr Rev. 2007 Oct;65(10):451-8. doi: 10.1111/j.1753-4887.2007.tb00270.x
- Hall CA. Transcobalamins I and II as natural transport proteins of vitamin B12. J Clin Invest. 1975 Nov;56(5):1125-31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC301974/pdf/jcinvest00173-0061.pdf
- Allen LH, Miller JW, de Groot L, Rosenberg IH, Smith AD, Refsum H, Raiten DJ. Biomarkers of Nutrition for Development (BOND): Vitamin B-12 Review. J Nutr. 2018 Dec 1;148(suppl_4):1995S-2027S. doi: 10.1093/jn/nxy201
- Maruvada P, Stover PJ, Mason JB, Bailey RL, Davis CD, Field MS, Finnell RH, Garza C, Green R, Gueant JL, Jacques PF, Klurfeld DM, Lamers Y, MacFarlane AJ, Miller JW, Molloy AM, O’Connor DL, Pfeiffer CM, Potischman NA, Rodricks JV, Rosenberg IH, Ross SA, Shane B, Selhub J, Stabler SP, Trasler J, Yamini S, Zappalà G. Knowledge gaps in understanding the metabolic and clinical effects of excess folates/folic acid: a summary, and perspectives, from an NIH workshop. Am J Clin Nutr. 2020 Nov 11;112(5):1390-1403. doi: 10.1093/ajcn/nqaa259
- Mineva EM, Sternberg MR, Zhang M, Aoki Y, Storandt R, Bailey RL, Pfeiffer CM. Age-specific reference ranges are needed to interpret serum methylmalonic acid concentrations in the US population. Am J Clin Nutr. 2019 Jul 1;110(1):158-168. doi: 10.1093/ajcn/nqz045
- Allen LH. Vitamin B-12. Adv Nutr. 2012 Jan;3(1):54-5. doi: 10.3945/an.111.001370
- Allen LH. Vitamin B12. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:812-20.
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate, Other B Vitamins, and Choline. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington (DC): National Academies Press (US); 1998. Available from: https://www.ncbi.nlm.nih.gov/books/NBK114310
- Shane B. Folic acid, vitamin B-12, and vitamin B-6. In: Stipanuk M, ed. Biochemical and Physiological Aspects of Human Nutrition. Philadelphia: W.B. Saunders Co.; 2000:483-518.
- National Institute of Health. Vitamin B-12. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- Damayanti D, Jaceldo-Siegl K, Beeson WL, Fraser G, Oda K, Haddad EH. Foods and Supplements Associated with Vitamin B12 Biomarkers among Vegetarian and Non-Vegetarian Participants of the Adventist Health Study-2 (AHS-2) Calibration Study. Nutrients. 2018 Jun 4;10(6):722. doi: 10.3390/nu10060722
- Henjum S, Manger M, Hampel D, Brantsæter AL, Shahab-Ferdows S, Bastani NE, Strand TA, Refsum H, Allen LH. Vitamin B12 concentrations in milk from Norwegian women during the six first months of lactation. Eur J Clin Nutr. 2020 May;74(5):749-756. doi: 10.1038/s41430-020-0567-x
- U.S. Food and Drug Adminstration. Code of Federal Regulations Title 21 § 107 – Infant Formula. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=107.100
- Doets EL, In ‘t Veld PH, Szczecińska A, Dhonukshe-Rutten RA, Cavelaars AE, van ‘t Veer P, Brzozowska A, de Groot LC. Systematic review on daily vitamin B12 losses and bioavailability for deriving recommendations on vitamin B12 intake with the factorial approach. Ann Nutr Metab. 2013;62(4):311-22. doi: 10.1159/000346968
- Allen LH. Bioavailability of vitamin B12. Int J Vitam Nutr Res. 2010 Oct;80(4-5):330-5. doi: 10.1024/0300-9831/a000041
- U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 27. Nutrient Data Laboratory home page, 2014. https://ndb.nal.usda.gov/ndb/
- Wong CW. Vitamin B12 deficiency in the elderly: is it worth screening? Hong Kong Med J. 2015 Apr;21(2):155-64. doi: 10.12809/hkmj144383
- Pfisterer KJ, Sharratt MT, Heckman GG, Keller HH. Vitamin B12 status in older adults living in Ontario long-term care homes: prevalence and incidence of deficiency with supplementation as a protective factor. Appl Physiol Nutr Metab. 2016 Feb;41(2):219-22. doi: 10.1139/apnm-2015-0565
- WECK, M.N., STEGMAIER, C., ROTHENBACHER, D. and BRENNER, H. (2007), Epidemiology of chronic atrophic gastritis: population-based study among 9444 older adults from Germany. Alimentary Pharmacology & Therapeutics, 26: 879-887. https://doi.org/10.1111/j.1365-2036.2007.03430.x
- Kalkan, Ç., Karakaya, F., Tüzün, A., Gençtürk, Z. Bıı., and Soykan, I. (2016) Factors related to low serum vitamin B12 levels in elderly patients with non-atrophic gastritis in contrast to patients with normal vitamin B12 levels. Geriatr Gerontol Int, 16: 686– 692. doi: 10.1111/ggi.12537
- Rojas Hernandez CM, Oo TH. Advances in mechanisms, diagnosis, and treatment of pernicious anemia. Discov Med. 2015 Mar;19(104):159-68. https://www.discoverymedicine.com/Cristhiam-M-Rojas-Hernandez/2015/03/advances-in-mechanisms-diagnosis-and-treatment-of-pernicious-anemia
- Green R, Allen LH, Bjørke-Monsen AL, Brito A, Guéant JL, Miller JW, Molloy AM, Nexo E, Stabler S, Toh BH, Ueland PM, Yajnik C. Vitamin B12 deficiency. Nat Rev Dis Primers. 2017 Jun 29;3:17040. doi: 10.1038/nrdp.2017.40. Erratum in: Nat Rev Dis Primers. 2017 Jul 20;3:17054
- Ao M, Tsuji H, Shide K, Kosaka Y, Noda A, Inagaki N, Nakase H, Tanaka K. High prevalence of vitamin B-12 insufficiency in patients with Crohn’s disease. Asia Pac J Clin Nutr. 2017;26(6):1076-1081. doi: 10.6133/apjcn.022017.13
- Bledsoe AC, King KS, Larson JJ, Snyder M, Absah I, Choung RS, Murray JA. Micronutrient Deficiencies Are Common in Contemporary Celiac Disease Despite Lack of Overt Malabsorption Symptoms. Mayo Clin Proc. 2019 Jul;94(7):1253-1260. doi: 10.1016/j.mayocp.2018.11.036
- Mark G. Ward, MBBS, Viraj C. Kariyawasam, MBBS, Sathis B. Mogan, MBBS, Kamal V. Patel, BSc, MBBS, Maria Pantelidou, MBBS, BSc, DPMSA, Agata Sobczyńska-Malefora, MSc, PhD, François Porté, MBBS, BSc, Nyree Griffin, MBChB, MD, Simon H. C. Anderson, MD, Jeremy D. Sanderson, MD, Dominic J. Harrington, BSc, MSc, PhD, Peter M. Irving, MA, MD, Prevalence and Risk Factors for Functional Vitamin B12 Deficiency in Patients with Crohn’s Disease, Inflammatory Bowel Diseases, Volume 21, Issue 12, 1 December 2015, Pages 2839–2847, https://doi.org/10.1097/MIB.0000000000000559
- Pan Y, Liu Y, Guo H, Jabir MS, Liu X, Cui W, Li D. Associations between Folate and Vitamin B12 Levels and Inflammatory Bowel Disease: A Meta-Analysis. Nutrients. 2017 Apr 13;9(4):382. doi: 10.3390/nu9040382
- Gomollón F, Gargallo CJ, Muñoz JF, Vicente R, Lue A, Mir A, García-Alvarado M, Gracia M, García-López S. Oral Cyanocobalamin is Effective in the Treatment of Vitamin B12 Deficiency in Crohn’s Disease. Nutrients. 2017 Mar 20;9(3):308. doi: 10.3390/nu9030308
- Kornerup LS, Hvas CL, Abild CB, Richelsen B, Nexo E. Early changes in vitamin B12 uptake and biomarker status following Roux-en-Y gastric bypass and sleeve gastrectomy. Clin Nutr. 2019 Apr;38(2):906-911. doi: 10.1016/j.clnu.2018.02.007
- Dogan K, Aarts EO, Koehestanie P, Betzel B, Ploeger N, de Boer H, Aufenacker TJ, van Laarhoven KJHM, Janssen IMC, Berends FJ. Optimization of vitamin suppletion after Roux-en-Y gastric bypass surgery can lower postoperative deficiencies: a randomized controlled trial. Medicine (Baltimore). 2014 Nov;93(25):e169. doi: 10.1097/MD.0000000000000169
- Wendy Schijns, Jens Homan, Leah van der Meer, Ignace M Janssen, Cees J van Laarhoven, Frits J Berends, Edo O Aarts, Efficacy of oral compared with intramuscular vitamin B-12 supplementation after Roux-en-Y gastric bypass: a randomized controlled trial, The American Journal of Clinical Nutrition, Volume 108, Issue 1, July 2018, Pages 6–12, https://doi.org/10.1093/ajcn/nqy072
- Pawlak R, Lester SE, Babatunde T. The prevalence of cobalamin deficiency among vegetarians assessed by serum vitamin B12: a review of literature. Eur J Clin Nutr. 2014 May;68(5):541-8. doi: 10.1038/ejcn.2014.46. Epub 2014 Mar 26. Erratum in: Eur J Clin Nutr. 2016 Jul;70(7):866.
- Dror DK, Allen LH. Vitamin B-12 in Human Milk: A Systematic Review. Adv Nutr. 2018 May 1;9(suppl_1):358S-366S. doi: 10.1093/advances/nmx019
- Piccoli, GB, Clari, R, Vigotti, FN, Leone, F, Attini, R, Cabiddu, G, Mauro, G, Castelluccia, N, Colombi, N, Capizzi, I, Pani, A, Todros, T, Avagnina, P. Vegan–vegetarian diets in pregnancy: danger or panacea? A systematic narrative review. BJOG 2015; 122: 623– 633. https://doi.org/10.1111/1471-0528.13280
- Annibale B., Lahner E., Fave G.D. Diagnosis and management of pernicious anemia. Curr. Gastroenterol. Rep. 2011;13:518–524. doi: 10.1007/s11894-011-0225-5
- Stabler SP. Clinical practice. Vitamin B12 deficiency. N Engl J Med 2013;368:149–60. http://www.nejm.org/doi/full/10.1056/NEJMcp1113996
- Annibale B., Lahner E., Fave G.D. Diagnosis and management of pernicious anemia. Curr. Gastroenterol. Rep. 2011;13:518–524. doi: 10.1007/s11894-011-0225-5
- Oo TH. Diagnostic difficulties in pernicious anemia. Discov Med. 2019 Nov-Dec;28(155):247-253. https://www.discoverymedicine.com/Thein-H-Oo/2019/12/diagnostic-difficulties-in-pernicious-anemia
- Esposito G, Dottori L, Pivetta G, Ligato I, Dilaghi E, Lahner E. Pernicious Anemia: The Hematological Presentation of a Multifaceted Disorder Caused by Cobalamin Deficiency. Nutrients. 2022 Apr 17;14(8):1672. doi: 10.3390/nu14081672
- Hershko C, Ronson A, Souroujon M, et al. Variable hematologic presentation of autoimmune gastritis: age‐related progression from iron deficiency to cobalamin depletion. Blood 2006;107:1673. http://www.bloodjournal.org/content/107/4/1673.long
- Amedai A, Bergman MP, Appelmelk BJ, et al. Molecular mimicry between Helicobacter pylori antigens and H+, K+‐adenosine triphosphatase in human gastric autoimmunity. J Exp Med 2003;198:1147–56. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2194239
- Lenti M.V., Rugge M., Lahner E., Miceli E., Toh B.H., Genta R.M., De Block C., Hershko C., Di Sabatino A. Autoimmune gastritis. Nat. Rev. Dis. Primers. 2020;6:56. doi: 10.1038/s41572-020-0187-8
- Nagao T, Hirokawa M. Diagnosis and treatment of macrocytic anemias in adults. Journal of General and Family Medicine. 2017;18(5):200-204. doi:10.1002/jgf2.31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5689413
- Lenti M.V., Miceli E., Cococcia S., Klersy C., Staiani M., Guglielmi F., Giuffrida P., Vanoli A., Luinetti O., De Grazia F., et al. Determinants of diagnostic delay in autoimmune atrophic gastritis. Aliment. Pharmacol. Ther. 2019;50:167–175. doi: 10.1111/apt.15317
- Toh B.H., van Driel I.R., Gleeson P.A. Pernicious anemia. N. Engl. J. Med. 1997;337:1441–1448. doi: 10.1056/NEJM199711133372007
- Carabotti M., Annibale B., Lahner E. Common Pitfalls in the Management of Patients with Micronutrient Deficiency: Keep in Mind the Stomach. Nutrients. 2021;13:208. doi: 10.3390/nu13010208
- Loukili NH, Noel E, Blaison G, et al. Update of pernicious anemia. A retrospective study of 49 cases. Rev Med Interne 2004;25:556–61. https://www.ncbi.nlm.nih.gov/pubmed/15276287
- Stabler SP, Allen RH. Vitamin B12 deficiency as a worldwide problem. Annu Rev Nutr 2004;24:299–326. https://www.ncbi.nlm.nih.gov/pubmed/15189123
- Murphy G, Dawsey SM, Engels EA, Ricker W, Parsons R, Etemadi A, Lin SW, Abnet CC, Freedman ND. Cancer Risk After Pernicious Anemia in the US Elderly Population. Clin Gastroenterol Hepatol. 2015 Dec;13(13):2282-9.e1-4. doi: 10.1016/j.cgh.2015.05.040
- Pernicious Anemia. https://emedicine.medscape.com/article/204930-overview#a6
- Chan JC, Liu HS, Kho BC, Lau TK, Li VL, Chan FH, Leong IS, Pang HK, Lee CK, Liang YS. Longitudinal study of Chinese patients with pernicious anaemia. Postgrad Med J. 2008 Dec;84(998):644-50. doi: 10.1136/pgmj.2007.06742
- Carmel R. Megaloblastic anemias. Curr Opin Hematol. 1994 Mar;1(2):107-12.
- Banka S, Ryan K, Thomson W, Newman WG. Pernicious anemia – genetic insights. Autoimmun Rev. 2011 Jun;10(8):455-9. doi: 10.1016/j.autrev.2011.01.009
- Checchi S, Montanaro A, Ciuoli C, Brusco L, Pasqui L, Fioravanti C, Sestini F, Pacini F. Prevalence of parietal cell antibodies in a large cohort of patients with autoimmune thyroiditis. Thyroid. 2010 Dec;20(12):1385-9. doi: 10.1089/thy.2010.0041
- Carmel R. How I treat cobalamin (vitamin B12) deficiency. Blood 2008;112:2214–21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2532799
- Andrès E, Loukili NH, Noel E, et al. Vitamin B12 (cobalamin) deficiency in elderly patients. CMAJ 2004;171:251–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC490077
- Hirokawa M. Recent progress of diagnosis and treatment for immune‐mediated hematological diseases. Topics: III. Diagnosis and treatment: 3. Pernicious anemia. Nihon Naika Gakkai Zasshi. 2014;103:1609–12. https://www.ncbi.nlm.nih.gov/pubmed/25154255
- Park JY, Lam‐Himlin D, Vemulapalli R. Review of autoimmune metaplastic atrophic gastritis. Gastrointest Endosc 2013;77:284–92. https://www.ncbi.nlm.nih.gov/pubmed/23199649
- Lahner E, Annibale B. Pernicious anemia: new insights from a gastroenterological point of view. World J Gastroenterol. 2009 Nov 7;15(41):5121-8. doi: 10.3748/wjg.15.5121
- Htut, TW, Thein, KZ, Oo, TH. Pernicious anemia: pathophysiology and diagnostic difficulties. J Evid Based Med. 2021; 14: 161- 169. https://doi.org/10.1111/jebm.12435
- Bunn H.F. Vitamin B12 and pernicious anemia–the dawn of molecular medicine. N. Engl. J. Med. 2014;370:773–776. doi: 10.1056/NEJMcibr1315544
- Conn DA. Detection of type I and type II antibodies to intrinsic factor. Med Lab Sci. 1986 Apr;43(2):148-51.
- Toh B.H., Chan J., Kyaw T., Alderuccio F. Cutting edge issues in autoimmune gastritis. Clin. Rev. Allergy Immunol. 2012;42:269–278. doi: 10.1007/s12016-010-8218-y
- Amedei A, Bergman MP, Appelmelk BJ, Azzurri A, Benagiano M, Tamburini C, van der Zee R, Telford JL, Vandenbroucke-Grauls CM, D’Elios MM, Del Prete G. Molecular mimicry between Helicobacter pylori antigens and H+, K+ –adenosine triphosphatase in human gastric autoimmunity. J Exp Med. 2003 Oct 20;198(8):1147-56. doi: 10.1084/jem.20030530
- Chmiela M, Gonciarz W. Molecular mimicry in Helicobacter pylori infections. World J Gastroenterol. 2017 Jun 14;23(22):3964-3977. doi: 10.3748/wjg.v23.i22.3964
- Castoro C, Le Moli R, Arpi ML, Tavarelli M, Sapuppo G, Frittitta L, Squatrito S, Pellegriti G. Association of autoimmune thyroid diseases, chronic atrophic gastritis and gastric carcinoid: experience from a single institution. J Endocrinol Invest. 2016 Jul;39(7):779-84. doi: 10.1007/s40618-016-0445-5
- Vaqar S, Shackelford K. Pernicious Anemia. [Updated 2022 Nov 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK540989
- Pernicious Anemia Treatment & Management. https://emedicine.medscape.com/article/204930-treatment#d12
- Green R. Vitamin B12 deficiency from the perspective of a practicing hematologist. Blood. 2017 May 11;129(19):2603-2611. doi: 10.1182/blood-2016-10-569186
- Carabotti M, Lahner E, Esposito G, Sacchi MC, Severi C, Annibale B. Upper gastrointestinal symptoms in autoimmune gastritis: A cross-sectional study. Medicine (Baltimore). 2017 Jan;96(1):e5784. doi: 10.1097/MD.0000000000005784
- Pernicious Anemia Clinical Presentation. https://emedicine.medscape.com/article/204930-clinical
- Venkatesh P, Shaikh N, Malmstrom MF, Kumar VR, Nour B. Portal, superior mesenteric and splenic vein thrombosis secondary to hyperhomocysteinemia with pernicious anemia: a case report. J Med Case Rep. 2014 Aug 25;8:286. doi: 10.1186/1752-1947-8-286
- Ekabe CJ, Kehbila J, Abanda MH, Kadia BM, Sama CB, Monekosso GL. Vitamin B12 deficiency neuropathy; a rare diagnosis in young adults: a case report. BMC Res Notes. 2017 Jan 28;10(1):72. doi: 10.1186/s13104-017-2393-3
- Kocaoglu C, Akin F, Caksen H, Böke SB, Arslan S, Aygün S. Cerebral atrophy in a vitamin B12-deficient infant of a vegetarian mother. J Health Popul Nutr. 2014 Jun;32(2):367-71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4216972
- Ammouri W, Tazi ZM, Harmouche H, Maamar M, Adnaoui M. Venous thromboembolism and hyperhomocysteinemia as first manifestation of pernicious anemia: a case series. J Med Case Rep. 2017 Sep 2;11(1):250. doi: 10.1186/s13256-017-1415-z
- Vannella, L., Lahner, E., Osborn, J. and Annibale, B. (2013), Systematic review: gastric cancer incidence in pernicious anaemia. Aliment Pharmacol Ther, 37: 375-382. https://doi.org/10.1111/apt.12177
- Shah SC, Piazuelo MB, Kuipers EJ, Li D. AGA Clinical Practice Update on the Diagnosis and Management of Atrophic Gastritis: Expert Review. Gastroenterology. 2021 Oct;161(4):1325-1332.e7. doi: 10.1053/j.gastro.2021.06.078
- Pernicious Anemia Workup. https://emedicine.medscape.com/article/204930-workup#c8
- Mohamed M, Thio J, Thomas RS, Phillips J. Pernicious anaemia. BMJ. 2020 Apr 24;369:m1319. doi: 10.1136/bmj.m1319
- Dixon M.F., Genta R.M., Yardley J.H., Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am. J. Surg. Pathol. 1996;20:1161–1181. doi: 10.1097/00000478-199610000-00001
- Pernicious Anemia Workup. https://emedicine.medscape.com/article/204930-workup#c12
- Wolffenbuttel BHR, Wouters HJCM, Heiner-Fokkema MR, van der Klauw MM. The Many Faces of Cobalamin (Vitamin B12) Deficiency. Mayo Clin Proc Innov Qual Outcomes. 2019 May 27;3(2):200-214. doi: 10.1016/j.mayocpiqo.2019.03.002
- Utility and limitations of biochemical markers of vitamin B12 deficiency. Eur J Clin Invest 2013; 43 ( 3): 231– 237. https://doi.org/10.1111/eci.12034
- Toh BH, van Driel IR, Gleeson PA. Pernicious anemia. N Engl J Med. 1997 Nov 13;337(20):1441-8. doi: 10.1056/NEJM199711133372007
- Graber JJ, Sherman FT, Kaufmann H, Kolodny EH, Sathe S. Vitamin B12-responsive severe leukoencephalopathy and autonomic dysfunction in a patient with “normal” serum B12 levels. J Neurol Neurosurg Psychiatry. 2010 Dec;81(12):1369-71. doi: 10.1136/jnnp.2009.178657
- Greibe E, Nexo E. Development of a Sensitive ELISA for Gastric Intrinsic Factor and Detection of Intrinsic Factor Immunoreactivity in Human Serum. Nutrients. 2022 Sep 28;14(19):4043. doi: 10.3390/nu14194043
- Devalia V, Hamilton MS, Molloy AM; British Committee for Standards in Haematology. Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol. 2014 Aug;166(4):496-513. doi: 10.1111/bjh.12959
- Erkurt MA, Aydogdu I, Dikilitaş M, Kuku I, Kaya E, Bayraktar N, Ozhan O, Ozkan I, Sonmez A. Effects of cyanocobalamin on immunity in patients with pernicious anemia. Med Princ Pract. 2008;17(2):131-5. doi: 10.1159/000112967
- Chan CQ, Low LL, Lee KH. Oral Vitamin B12 Replacement for the Treatment of Pernicious Anemia. Front Med (Lausanne). 2016 Aug 23;3:38. doi: 10.3389/fmed.2016.00038
- Christopher C Butler, Josep Vidal-Alaball, Rebecca Cannings-John, Andrew McCaddon, Kerenza Hood, Alexandra Papaioannou, Ian Mcdowell, Andrew Goringe, Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: a systematic review of randomized controlled trials, Family Practice, Volume 23, Issue 3, June 2006, Pages 279–285, https://doi.org/10.1093/fampra/cml008
- Zhang J, Field CJ, Vine D, Chen L. Intestinal uptake and transport of vitamin B12-loaded soy protein nanoparticles. Pharm Res. 2015 Apr;32(4):1288-303. doi: 10.1007/s11095-014-1533-x
- Andres E, Serraj K. Optimal management of pernicious anemia. J Blood Med. 2012;3:97-103. doi: 10.2147/JBM.S25620
- Favrat B, Vaucher P, Herzig L, Burnand B, Ali G, Boulat O, Bischoff T, Verdon F. Oral vitamin B12 for patients suspected of subtle cobalamin deficiency: a multicentre pragmatic randomised controlled trial. BMC Fam Pract. 2011 Jan 13;12:2. doi: 10.1186/1471-2296-12-2
- Pernicious Anemia Treatment & Management. https://emedicine.medscape.com/article/204930-treatment
- Pernicious Anemia Treatment & Management. https://emedicine.medscape.com/article/204930-treatment#d10
- Banks M, Graham D, Jansen M, Gotoda T, Coda S, di Pietro M, Uedo N, Bhandari P, Pritchard DM, Kuipers EJ, Rodriguez-Justo M, Novelli MR, Ragunath K, Shepherd N, Dinis-Ribeiro M. British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019 Sep;68(9):1545-1575. doi: 10.1136/gutjnl-2018-318126
- Pimentel-Nunes P, Libânio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, Garrido M, Kikuste I, Megraud F, Matysiak-Budnik T, Annibale B, Dumonceau JM, Barros R, Fléjou JF, Carneiro F, van Hooft JE, Kuipers EJ, Dinis-Ribeiro M. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019 Apr;51(4):365-388. doi: 10.1055/a-0859-1883
- Pimentel-Nunes P, Libânio D, Marcos-Pinto R, et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019 Apr;51(4):365-388. doi: 10.1055/a-0859-1883
- Areia M., Dinis-Ribeiro M., Goncalves F.R. Cost-utility analysis of endoscopic surveillance of patients with gastric premalignant conditions. Helicobacter. 2014;19:425–436. doi: 10.1111/hel.12150
- Lahner E., Hassan C., Esposito G., Carabotti M., Zullo A., Dinis-Ribeiro M., Annibale B. Cost of detecting gastric neoplasia by surveillance endoscopy in atrophic gastritis in Italy: A low risk country. Dig. Liver. Dis. 2017;49:291–296. doi: 10.1016/j.dld.2016.12.004
- Rugge M., Meggio A., Pravadelli C., Barbareschi M., Fassan M., Gentilini M., Zorzi M., Pretis G., Graham D.Y., Genta R.M. Gastritis staging in the endoscopic follow-up for the secondary prevention of gastric cancer: A 5-year prospective study of 1755 patients. Gut. 2019;68:11–17. doi: 10.1136/gutjnl-2017-314600
- Zullo A., Hassan C., Repici A., Annibale B. Intestinal metaplasia surveillance: Searching for the road-map. World J. Gastroenterol. 2013;19:1523–1526. doi: 10.3748/wjg.v19.i10.1523
- Lahner E., Esposito G., Pilozzi E., Purchiaroni F., Corleto V.D., Di Giulio E., Annibale B. Occurrence of gastric cancer and carcinoids in atrophic gastritis during prospective long-term follow up. Scand. J. Gastroenterol. 2015;50:856–865. doi: 10.3109/00365521.2015.1010570
- Rugge M., Genta R.M., Fassan M., Valentini E., Coati I., Guzzinati S., Savarino E., Zorzi M., Farinati F., Malfertheiner P. OLGA Gastritis Staging for the Prediction of Gastric Cancer Risk: A Long-term Follow-up Study of 7436 Patients. Am. J. Gastroenterol. 2018;113:1621–1628. doi: 10.1038/s41395-018-0353-8
- de Vries A.C., van Grieken N.C., Looman C.W., Casparie M.K., de Vries E., Meijer G.A., Kuipers E.J. Gastric cancer risk in patients with premalignant gastric lesions: A nationwide cohort study in the Netherlands. Gastroenterology. 2008;134:945–952. doi: 10.1053/j.gastro.2008.01.071
- Cho S.J., Choi I.J., Kook M.C., Nam B.H., Kim C.G., Lee J.Y., Ryu K.W., Kim Y.W. Staging of intestinal- and diffuse-type gastric cancers with the OLGA and OLGIM staging systems. Aliment. Pharmacol. Ther. 2013;38:1292–1302. doi: 10.1111/apt.12515
- Esposito G., Dilaghi E., Cazzato M., Pilozzi E., Conti L., Carabotti M., Di Giulio E., Annibale B., Lahner E. Endoscopic surveillance at 3 years after diagnosis, according to European guidelines, seems safe in patients with atrophic gastritis in a low-risk region. Dig. Liver Dis. 2021;53:467–473. doi: 10.1016/j.dld.2020.10.038
- Panzuto F., Magi L., Esposito G., Rinzivillo M., Annibale B. Comparison of Endoscopic Techniques in the Management of Type I Gastric Neuroendocrine Neoplasia: A Systematic Review. Gastroenterol. Res. Pract. 2021;2021:6679397. doi: 10.1155/2021/6679397
- Fave G.D., O’Toole D., Sundin A., Taal B., Ferolla P., Ramage J.K., Ferone D., Ito T., Weber W., Zheng-Pei Z., et al. ENETS Consensus Guidelines Update for Gastroduodenal Neuroendocrine Neoplasms. Neuroendocrinology. 2016;103:119–124. doi: 10.1159/000443168
- Esposito G., Cazzato M., Rinzivillo M., Pilozzi E., Lahner E., Annibale B., Panzuto F. Management of type-I gastric neuroendocrine neoplasms: A 10-years prospective single centre study. Dig. Liver Dis. 2021 doi: 10.1016/j.dld.2021.11.012
- Kikuste I., Marques-Pereira R., Monteiro-Soares M., Pimentel-Nunes P., Areia M., Leja M., Dinis-Ribeiro M. Systematic review of the diagnosis of gastric premalignant conditions and neoplasia with high-resolution endoscopic technologies. Scand. J. Gastroenterol. 2013;48:1108–1117. doi: 10.3109/00365521.2013.825315
- Zhao Z., Yin Z., Wang S., Wang J., Bai B., Qiu Z., Zhao Q. Meta-analysis: The diagnostic efficacy of chromoendoscopy for early gastric cancer and premalignant gastric lesions. J. Gastroenterol. Hepatol. 2016;31:1539–1545. doi: 10.1111/jgh.13313
- Rodriguez-Carrasco M., Esposito G., Libânio D., Pimentel-Nunes P., Dinis-Ribeiro M. Image-enhanced endoscopy for gastric preneoplastic conditions and neoplastic lesions: A systematic review and meta-analysis. Endoscopy. 2020;52:1048–1065. doi: 10.1055/a-1205-0570
- Esposito G., Angeletti S., Cazzato M., Galli G., Conti L., Di Giulio E., Annibale B., Lahner E. Narrow band imaging characteristics of gastric polypoid lesions: A single-center prospective pilot study. Eur. J. Gastroenterol. Hepatol. 2020;32:701–705. doi: 10.1097/MEG.0000000000001697
- Vaqar S, Shackelford K. Pernicious Anemia. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK540989
- Vasconcelos OM, Poehm EH, McCarter RJ, Campbell WW, Quezado ZM. Potential outcome factors in subacute combined degeneration: review of observational studies. J Gen Intern Med. 2006 Oct;21(10):1063-8. doi: 10.1111/j.1525-1497.2006.00525.x
- Kumar N. Neurologic aspects of cobalamin (B12) deficiency. Handb Clin Neurol. 2014;120:915-26. doi: 10.1016/B978-0-7020-4087-0.00060-7
- Chan JC, Liu HS, Kho BC, Lau TK, Li VL, Chan FH, Leong IS, Pang HK, Lee CK, Liang YS. Longitudinal study of Chinese patients with pernicious anaemia. Postgrad Med J. 2008 Dec;84(998):644-50. doi: 10.1136/pgmj.2007.067421
- Kozyraki R, Cases O. Vitamin B12 absorption: mammalian physiology and acquired and inherited disorders. Biochimie. 2013 May;95(5):1002-7. doi: 10.1016/j.biochi.2012.11.004
- Infante M, Leoni M, Caprio M, Fabbri A. Long-term metformin therapy and vitamin B12 deficiency: An association to bear in mind. World J Diabetes. 2021 Jul 15;12(7):916-931. doi: 10.4239/wjd.v12.i7.916
- Vitamin B-12 Associated Neurological Diseases. https://emedicine.medscape.com/article/1152670-overview
- Crafa P, Russo M, Miraglia C, et al. From Sidney to OLGA: an overview of atrophic gastritis. Acta Biomed. 2018 Dec 17. 89(8-S):93-9.
- Baik HW, Russell RM. Vitamin B12 deficiency in the elderly. Annu Rev Nutr. 1999;19:357-77. doi: 10.1146/annurev.nutr.19.1.357
- Neumann WL, Coss E, Rugge M, Genta RM. Autoimmune atrophic gastritis–pathogenesis, pathology and management. Nat Rev Gastroenterol Hepatol. 2013 Sep;10(9):529-41. doi: 10.1038/nrgastro.2013.101
- Raza M, Bhatt H. Atrophic Gastritis. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563275
- Lahner, E., Persechino, S. and Annibale, B. (2012), Micronutrients (Other than iron) and Helicobacter pylori Infection: A Systematic Review. Helicobacter, 17: 1-15. https://doi.org/10.1111/j.1523-5378.2011.00892.x
- Lam-Tse WK, Batstra MR, Koeleman BP, Roep BO, Bruining MG, Aanstoot HJ, Drexhage HA. The association between autoimmune thyroiditis, autoimmune gastritis and type 1 diabetes. Pediatr Endocrinol Rev. 2003 Sep;1(1):22-37.
- Ho C, Kauwell GP, Bailey LB. Practitioners’ guide to meeting the vitamin B-12 recommended dietary allowance for people aged 51 years and older. J Am Diet Assoc. 1999 Jun;99(6):725-7. doi: 10.1016/S0002-8223(99)00174-1
- Watkins D, Rosenblatt DS. Lessons in biology from patients with inborn errors of vitamin B12 metabolism. Biochimie. 2013 May;95(5):1019-22. doi: 10.1016/j.biochi.2013.01.013
- Dharmarajan TS, Kanagala MR, Murakonda P, Lebelt AS, Norkus EP. Do acid-lowering agents affect vitamin B12 status in older adults? J Am Med Dir Assoc. 2008 Mar;9(3):162-7. doi: 10.1016/j.jamda.2007.10.004
- Wilhelm SM, Rjater RG, Kale-Pradhan PB. Perils and pitfalls of long-term effects of proton pump inhibitors. Expert Rev Clin Pharmacol. 2013 Jul;6(4):443-51. doi: 10.1586/17512433.2013.811206
- Valuck RJ, Ruscin JM. A case-control study on adverse effects: H2 blocker or proton pump inhibitor use and risk of vitamin B12 deficiency in older adults. J Clin Epidemiol. 2004 Apr;57(4):422-8. doi: 10.1016/j.jclinepi.2003.08.015
- Termanini B, Gibril F, Sutliff VE, Yu F, Venzon DJ, Jensen RT. Effect of long-term gastric acid suppressive therapy on serum vitamin B12 levels in patients with Zollinger-Ellison syndrome. Am J Med. 1998 May;104(5):422-30. doi: 10.1016/s0002-9343(98)00087-4
- Bauman WA, Shaw S, Jayatilleke E, Spungen AM, Herbert V. Increased intake of calcium reverses vitamin B12 malabsorption induced by metformin. Diabetes Care. 2000 Sep;23(9):1227-31. doi: 10.2337/diacare.23.9.1227
- Obeid R. Metformin causing vitamin B12 deficiency: a guilty verdict without sufficient evidence. Diabetes Care. 2014 Feb;37(2):e22-3. doi: 10.2337/dc13-2278
- Mazokopakis EE, Starakis IK. Recommendations for diagnosis and management of metformin-induced vitamin B12 (Cbl) deficiency. Diabetes Res Clin Pract. 2012 Sep;97(3):359-67. doi: 10.1016/j.diabres.2012.06.001
- Simon JA, Hudes ES. Relation of serum ascorbic acid to serum vitamin B12, serum ferritin, and kidney stones in US adults. Arch Intern Med. 1999 Mar 22;159(6):619-24. doi: 10.1001/archinte.159.6.619
- Weir DG, Scott JM. Vitamin B12 “Cobalamin.” In: Shils M, ed. Nutrition in Health and Disease. 9th ed. Baltimore: Williams & Wilkins; 1999:447-458.
- Food and Nutrition Board, Institute of Medicine. Vitamin B12. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, D.C.: National Academy Press; 1998:306-356. https://nap.nationalacademies.org/read/6015/chapter/1
- Andrès E, Federici L, Affenberger S, Vidal-Alaball J, Loukili NH, Zimmer J, et al. B12 deficiency: a look beyond pernicious anemia. J Fam Pract 2007;56:537-42. https://www.ncbi.nlm.nih.gov/pubmed/17605945?dopt=Abstract
- Mechanick JI, Youdim A, Jones DB, Timothy Garvey W, Hurley DL, Molly McMahon M, Heinberg LJ, Kushner R, Adams TD, Shikora S, Dixon JB, Brethauer S. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013 Mar-Apr;9(2):159-91. doi: 10.1016/j.soard.2012.12.010
- Carmel R. Current concepts in cobalamin deficiency. Annu Rev Med. 2000;51:357-75. doi: 10.1146/annurev.med.51.1.357
- Active B12 assay for diagnosing vitamin B12 deficiency. https://www.nice.org.uk/advice/mib40/resources/active-b12-assay-for-diagnosing-vitamin-b12-deficiency-pdf-63499159342789
- Mills JL, Scott JM, Kirke PN, McPartlin JM, Conley MR, Weir DG, Molloy AM, Lee YJ. Homocysteine and neural tube defects. J Nutr. 1996 Mar;126(3):756S-760S. doi: 10.1093/jn/126.suppl_3.756S
- Imbard A, Benoist JF, Blom HJ. Neural tube defects, folic acid and methylation. Int J Environ Res Public Health. 2013 Sep 17;10(9):4352-89. doi: 10.3390/ijerph10094352
- Wang ZP, Shang XX, Zhao ZT. Low maternal vitamin B(12) is a risk factor for neural tube defects: a meta-analysis. J Matern Fetal Neonatal Med. 2012 Apr;25(4):389-94. doi: 10.3109/14767058.2011.580800
- Reynolds E. Vitamin B12, folic acid, and the nervous system. Lancet Neurol. 2006 Nov;5(11):949-60. doi: 10.1016/S1474-4422(06)70598-1
- Molloy AM, Kirke PN, Troendle JF, Burke H, Sutton M, Brody LC, Scott JM, Mills JL. Maternal vitamin B12 status and risk of neural tube defects in a population with high neural tube defect prevalence and no folic Acid fortification. Pediatrics. 2009 Mar;123(3):917-23. doi: 10.1542/peds.2008-1173
- Dror DK, Allen LH. Effect of vitamin B12 deficiency on neurodevelopment in infants: current knowledge and possible mechanisms. Nutr Rev. 2008 May;66(5):250-5. doi: 10.1111/j.1753-4887.2008.00031.x
- Centers for Disease Control and Prevention (CDC). Neurologic impairment in children associated with maternal dietary deficiency of cobalamin–Georgia, 2001. MMWR Morb Mortal Wkly Rep. 2003 Jan 31;52(4):61-4. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5204a1.htm
- Hay G, Johnston C, Whitelaw A, Trygg K, Refsum H. Folate and cobalamin status in relation to breastfeeding and weaning in healthy infants. Am J Clin Nutr. 2008 Jul;88(1):105-14. doi: 10.1093/ajcn/88.1.105
- How to Cite this Article: Derin, S, Koseoglu, S, Sahin, C, Sahan, M. Effect of vitamin B12 deficiency on olfactory function. Int Forum Allergy Rhinol. 2016; 6: 1051– 1055. https://doi.org/10.1002/alr.21790
- Pernicious anemia. https://medlineplus.gov/ency/article/000569.htm
- Hemmer B., Glocker F.X., Schumacher M., Deuschl G., Lücking C.H. Subacute combined degeneration: Clinical, electrophysiological, and magnetic resonance imaging findings. J. Neurol. Neurosurg. Psychiatry. 1998;65:822–827. doi: 10.1136/jnnp.65.6.822
- Maamar M., Mezalek Z.T., Harmouche H., Adnaoui M., Aouni M., Maaouni A. Contribution of spinal MRI for unsuspected cobalamin deficiency in isolated sub-acute combined degeneration. Eur. J. Intern. Med. 2008;19:143–145. doi: 10.1016/j.ejim.2007.03.017
- Merck Sharp & Dohme Corp., Merck Manual. Vitamin B 12. https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency,-dependency,-and-toxicity/vitamin-b-12
- Oo TH, Rojas-Hernandez CM. Challenging clinical presentations of pernicious anemia. Discov Med. 2017 Sep;24(131):107-115. https://www.discoverymedicine.com/Thein-H-Oo/2017/09/challenging-clinical-presentations-of-pernicious-anemia
- Herbert V. Vitamin B-12. In: Ziegler EE, Filer LJ, eds. Present Knowledge in Nutrition. 7th ed. Washington D.C.: ILSI Press; 1996:191-205.
- Healton E.B., Savage D.G., Brust J.C., Garrett T.J., Lindenbaum J. Neurologic aspects of cobalamin deficiency. Medicine. 1991;70:229–245. doi: 10.1097/00005792-199107000-00001
- Gwathmey K.G., Grogan J. Nutritional neuropathies. Muscle Nerve. 2020;62:13–29. doi: 10.1002/mus.26783
- Kumar N. Nutritional neuropathies. Neurol. Clin. 2007;25:209–255. doi: 10.1016/j.ncl.2006.11.001
- Briani C., Dalla Torre C., Citton V., Manara R., Pompanin S., Binotto G., Adami F. Cobalamin deficiency: Clinical picture and radiological findings. Nutrients. 2013;5:4521–4539. doi: 10.3390/nu5114521
- Scalabrino G. The multi-faceted basis of vitamin B12 (cobalamin) neurotrophism in adult central nervous system: Lessons learned from its deficiency. Prog Neurobiol. 2009 Jul;88(3):203-20. doi: 10.1016/j.pneurobio.2009.04.004
- Remacha A.F., Souto J.C., Piñana J.L., Sardà M.P., Queraltó J.M., Martí-Fàbregas J., Garcia-Moll X., Fernández C., Rodríguez Á., Cuesta J. Vitamin B12 deficiency, hyperhomocysteinemia and thrombosis: A case and control study. Int. J. Hematol. 2011;93:458–464. doi: 10.1007/s12185-011-0825-8
- Ospina-Romero M., Cannegieter S.C., Heijer M.D., Doggen C.J.M., Rosendaal F.R., Lijfering W.M. Hyperhomocysteinemia and Risk of First Venous Thrombosis: The Influence of (Unmeasured) Confounding Factors. Am. J. Epidemiol. 2018;187:1392–1400. doi: 10.1093/aje/kwy004
- Tanaka M., Taniguchi T., Saito N., Kimura T. Inferior vena cava thrombus due to hyperhomocysteinemia. J. Cardiol. Cases. 2018;18:168–170. doi: 10.1016/j.jccase.2018.07.003
- Kapur V., D’Cruz S., Kaur R. An uncommon presentation of hyperhomocysteinemia and vitamin B12 deficiency: A case report. J. Med. Case Rep. 2019;13:36. doi: 10.1186/s13256-019-1988-9
- Ammouri W., Tazi Z.M., Harmouche H., Maamar M., Adnaoui M. Venous thromboembolism and hyperhomocysteinemia as first manifestation of pernicious anemia: A case series. J. Med. Case Rep. 2017;11:250. doi: 10.1186/s13256-017-1415-z
- Ulrich A., Muller D., Linnebank M., Tarnutzer A.A. Pitfalls in the diagnostic evaluation of subacute combined degeneration. BMJ Case Rep. 2015;2015:bcr2014208622. doi: 10.1136/bcr-2014-208622
- Kovalenko O., Kassem A.N., Jenkins M. Hyperhomocysteinemia and Pulmonary Embolism in a Young Male. Cureus. 2020;12:e7818. doi: 10.7759/cureus.7818
- Goette A., Hammwöhner M., Dierkes J., Lachmuth J., Frölich J.C., Klein H., Bode-Böger S.M. Aortic thrombus and pulmonary embolism in a patient with hyperhomocysteinemia. Nat. Clin. Pr. Neurol. 2006;3:396–399. doi: 10.1038/ncpcardio0601
- McCaddon A. Homocysteine and cognitive impairment; a case series in a General Practice setting. Nutr. J. 2006;5:6. doi: 10.1186/1475-2891-5-6
- Ankar A, Kumar A. Vitamin B12 Deficiency. [Updated 2022 Oct 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441923
- Carmel R, Green R, Rosenblatt DS, Watkins D. Update on cobalamin, folate, and homocysteine. Hematology Am Soc Hematol Educ Program. 2003:62-81. doi: 10.1182/asheducation-2003.1.62
- Stabler SP, Allen RH. Megaloblastic anemias. In: Cecil RL, Goldman L, Ausiello DA, eds. Cecil Textbook of Medicine. 22nd ed. Philadelphia, Pa.: Saunders; 2004:1050–1057.
- Obeid R, Heil SG, Verhoeven MMA, van den Heuvel EGHM, de Groot LCPGM, Eussen SJPM. Vitamin B12 Intake From Animal Foods, Biomarkers, and Health Aspects. Front Nutr. 2019 Jun 28;6:93. doi: 10.3389/fnut.2019.00093
- Ankar A, Kumar A. Vitamin B12 Deficiency. [Updated 2022 Oct 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441923
- Oberley, M.J. and Yang, D.T. (2013), Laboratory testing for cobalamin deficiency in megaloblastic anemia. Am. J. Hematol., 88: 522-526. https://doi.org/10.1002/ajh.23421
- Oberley MJ, Yang DT. Laboratory testing for cobalamin deficiency in megaloblastic anemia. Am J Hematol. 2013 Jun;88(6):522-6. doi: 10.1002/ajh.23421
- Quadros EV. Advances in the understanding of cobalamin assimilation and metabolism. Br J Haematol. 2010 Jan;148(2):195-204. doi: 10.1111/j.1365-2141.2009.07937.x
- Bromage S, Ganmaa D, Rich-Edwards JW, Rosner B, Bater J, Fawzi WW. Projected effectiveness of mandatory industrial fortification of wheat flour, milk, and edible oil with multiple micronutrients among Mongolian adults. PLoS One. 2018 Aug 2;13(8):e0201230. doi: 10.1371/journal.pone.0201230
- Homan J, Schijns W, Aarts EO, Janssen IMC, Berends FJ, de Boer H. Treatment of Vitamin and Mineral Deficiencies After Biliopancreatic Diversion With or Without Duodenal Switch: a Major Challenge. Obes Surg. 2018 Jan;28(1):234-241. doi: 10.1007/s11695-017-2841-0
- Freedberg DE, Kim LS, Yang YX. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017 Mar;152(4):706-715. doi: 10.1053/j.gastro.2017.01.031
- BSH Guidance on B12 Replacement during the COVID-19 Pandemic, British Society for Haematology. https://b-s-h.org.uk/media/18275/bsh-guidance-b12-replacement-covid-1901052020finalv.pdf
- Ramezanpour Ahangar E, Annamaraju P. Hydroxocobalamin. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557632
- Oh R, Brown DL. Vitamin B12 deficiency. Am Fam Physician. 2003 Mar 1;67(5):979-86. https://www.aafp.org/pubs/afp/issues/2003/0301/p979.html
- O’Leary F, Samman S. Vitamin B12 in health and disease. Nutrients. 2010 Mar;2(3):299-316. doi: 10.3390/nu2030299
- Vitamin B12 or folate deficiency anaemia treatment. https://www.nhs.uk/conditions/vitamin-b12-or-folate-deficiency-anaemia/treatment