Xanthochromia
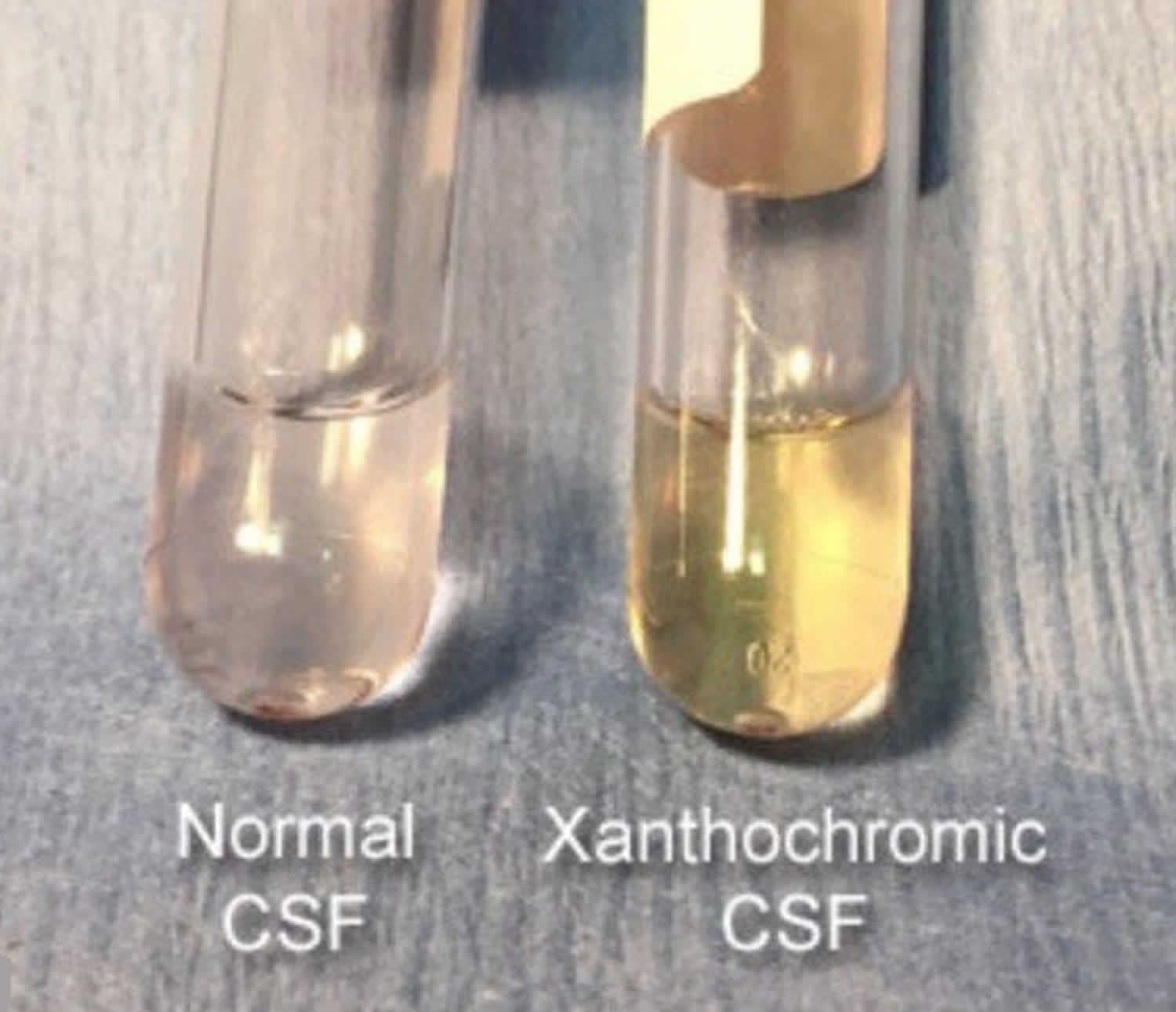
Xanthochromia is the orange, or pink discoloration of the cerebrospinal fluid (CSF) most often caused by the lysis of red blood cells resulting in hemoglobin breakdown to oxyhemoglobin, methemoglobin, and bilirubin the and is used by some doctors to differentiate in vivo hemorrhage from a traumatic lumbar puncture 1. The term xanthochromia now is more widely accepted to represent the yellow color created by the presence of bilirubin in the CSF 2. The presence of bilirubin resulting in yellow discoloration of the CSF is the contemporary definition of xanthochromia 3.
CSF discoloration begins after red blood cells have been in spinal fluid for about two hours, and remains for two to four weeks 4. Xanthochromia is present in more than 90 percent of patients within 12 hours of subarachnoid hemorrhage onset 5 and in patients with serum bilirubin levels between 10 to 15 mg per dL (171 to 256.5 μmol per L). CSF protein levels of at least 150 mg per dL (1.5 g per L) as seen in many infectious and inflammatory conditions, or as a result of a traumatic tap that contains more than 100,000 red blood cells per mm³ also will result in xanthochromia 5. Newborn CSF is often xanthochromic because of the frequent elevation of bilirubin and protein levels in this age group 1.
The rupture of an intracerebral aneurysm most commonly causes subarachnoid hemorrhages. The incidence of subarachnoid hemorrhage (SAH) is anywhere from 9 to 15 people per 100,000 in the United States with rates that vary by geography. Risk factors include hypertension, cigarette smoking, alcohol use, some sympathomimetic drugs, and some genetic causes that increase the risk of a cerebral aneurysm 6.
Once a cerebral aneurysm has ruptured or started to leak, blood may be found in the CSF in varying quantities. Over time this blood is degraded by macrophages and broken down into its byproducts containing bilirubin. The process of conversion from heme to bilirubin in the CSF takes 6 to 12 hours and can only happen in vivo. Therefore, xanthochromia is best identified 6 to 12 hours after the onset of a bleed.
There are currently 2 different methods to identify xanthochromia in the CSF. In the United States, visual detection is still the method of choice. A CSF sample is spun down in a centrifuge, and the supernatant is visually inspected with the naked eye for a yellow color. This is accomplished by holding a vial of water next to a vial of supernatant against a white backdrop. The second and perhaps a more reliable way to test for xanthochromia is the use of spectrophotometry. A spectrophotometer measures the absorption of light of material and identifies that material based on the wavelength of light it absorbs. Bilirubin itself has a narrow window of detection with a wavelength of ∼440 to 460 nm with peaks at 415 nm, indicating the presence of hemoglobin (Hb) and bilirubin, respectively 7. The problem with this test is that it is not known which CSF bilirubin absorbance indicates a clinically significant bleed 8. Multiple studies show the superiority of spectrophotometry when compared to visual inspection. There are several factors that can interfere with the appearance of xanthochromia on visual inspection alone. For instance, the presence of proteins or pigments such as carotenoids can obscure the color change associated with the presence of xanthochromia. The presence of oxyhemoglobin with an acute bleed or traumatic lumbar puncture appears pink or orange and can hide the yellow discoloration of xanthochromia leading to a false negative result. Furthermore, unlike spectrophotometry, visual inspection cannot detect low concentrations of bilirubin and cannot distinguish bilirubin from oxyhemoglobin 9.
Non-contrast computed tomography of the head (NCHCT) is still the initial test of choice in the diagnosis of subarachnoid hemorrhage. The sensitivity of this test is greatest within the first 6 hours of onset of symptoms. The current standard of care is to obtain an non-contrast computed tomography of the head followed by a lumbar puncture to evaluate for xanthochromia if the non-contrast computed tomography of the head is negative. The finding of xanthochromia in the CSF is helpful in that it is 93% sensitive and 95% specific with a positive predictive value of 72% and a negative predictive value of 99% 10. Xanthochromia is typically present in the CSF within 6 to 12 hours after the onset of symptoms. Unlike CT, xanthochromia is present in the CSF in all patients up to 2 weeks postictus and is still present in 70% of patients Up to three weeks later 11. Furthermore, sensitivity for detecting a bleed by CT decreases from up to 95% on day 1 to less than 10% in 3 weeks, with the sensitivity of CSF analysis remaining constant near 100% over this time 12. Because the production of bilirubin is a process that happens only in vivo, the presence of xanthochromia in the CSF is the only way to differentiate between a true hemorrhage and a traumatic tap as both can contain large amounts of red blood cells 13.
Xanthochromia key points
- Xanthochromia is the presence of bilirubin in the CSF.
- Xanthochromia can be the only positive marker that a patient is suffering an acute subarachnoid hemorrhage.
- Xanthochromia is an important finding in distinguishing between a traumatic tap and a subarachnoid hemorrhage.
- Visual inspection of the CSF is the most common method of detection.
- Spectrophotometry has been shown to be superior when evaluating for xanthochromia.
Xanthochromia causes
Bilirubin is the byproduct of the degradation of oxyhemoglobin by the enzyme oxygenase. There are many causes of xanthochromia such as acute intracerebral hemorrhage, brain tumors, infection, increased protein and severe systemic jaundice. The finding of xanthochromia in the CSF is most commonly used in the diagnosis of subarachnoid hemorrhage (SAH) in the presence of a normal head computed tomography 14. Table 1 lists CSF colors associated with various conditions.
Subarachnoid hemorrhage is a rare but significant disease which can lead to sudden death and disability if not diagnosed and treated properly. Patients often present complaining of the worst headache of their life. A sudden onset at a maximal intensity or within the first hour of onset often characterizes headache. There can be associated with meningismus, nausea, vomiting, photophobia, and/or phonophobia but rarely with acute neurologic deficits. It can be difficult to distinguish between a non-traumatic headache associated with subarachnoid hemorrhage or another less serious cause.
Table 1. CSF colors and associated conditions or causes
| Color of CSF supernatant | Conditions or causes |
|---|---|
Yellow | Blood breakdown products |
Hyperbilirubinemia | |
CSF protein ≥150 mg per dL (1.5 g per L) >100,000 red blood cells per mm3 | |
Orange | Blood breakdown products |
High carotenoid ingestion | |
Pink | Blood breakdown products |
Green | Hyperbilirubinemia |
Purulent CSF | |
Brown | Meningeal melanomatosis |
Xanthochromic CSF differential diagnosis
The finding of xanthochromia on a spinal tap can be the only evidence to suggest the presence of a subarachnoid hemorrhage. There are many causes of xanthochromia such as acute intracerebral hemorrhage, brain tumors, infection, increased protein and severe systemic jaundice. The finding of xanthochromia in the CSF is most commonly used in the diagnosis of subarachnoid hemorrhage (SAH) in the presence of a normal head computed tomography 14. Table 1 lists CSF colors associated with various conditions.
It is very difficult to determine the pretest probability of subarachnoid hemorrhage based on presentation alone. There is no one factor that could determine the need for further testing for an acute non-traumatic headache. Lumbar puncture is an invasive procedure, and often results are misleading and non-diagnostic. There is a very specific subset of patients in whom a lumbar puncture with the finding of xanthochromia will correctly diagnose a subarachnoid hemorrhage. The majority of patients with negative head CT will not be diagnosed with subarachnoid hemorrhage. However, the over the use of CT angiography (CTA) exposes patients to unnecessary radiation and contrast. Furthermore, the use of CT angiography leads to the finding of incidental aneurysms which may or may not be clinically significant. This, in turn, may expose the patient to even more unnecessary testing and intervention. In this case, lumbar puncture has a high diagnostic yield, eliminating the need for neurosurgical consultation or intervention in the majority of cases 15. The test is both cost effective and time efficient and reduces the number of patients exposed to the radiation and contrast associated with angiography 15.
Xanthochromia treatment
Xanthochromia treatment involves treating the underlying cause.
Once the patient is diagnosed with a subarachnoid hemorrhage based on the findings of xanthochromia in the CSF, they may be sent for magnetic resonance imaging (MRI), CT angiography, or taken directly for treatment. The next step in management is to find the location of an aneurysm and thus the cause of the subarachnoid hemorrhage.
References- Cerebrospinal Fluid Analysis. Am Fam Physician. 2003 Sep 15;68(6):1103-1109. https://www.aafp.org/afp/2003/0915/p1103.html
- Dugas C, Bollu PC. Xanthochromia. [Updated 2019 Feb 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526048
- Gill HS, Marcolini EG, Barber D, Wira CR. The Utility of Lumbar Puncture After a Negative Head CT in the Emergency Department Evaluation of Subarachnoid Hemorrhage. Yale J Biol Med. 2018 Mar;91(1):3-11.
- Dougherty JM, Roth RM. Cerebral spinal fluid. Emerg Med Clin North Am. 1986;4:281–97.
- Fishman RA. Cerebrospinal fluid in diseases of the nervous system. 2d ed. Philadelphia: Saunders, 1992.
- Yu SD, Chen MY, Johnson AJ. Factors associated with traumatic fluoroscopy-guided lumbar punctures: a retrospective review. AJNR Am J Neuroradiol. 2009 Mar;30(3):512-5.
- Van Gijn J, van Dongen KJ. Time course of aneurysmal haemorrhage on computed tomograms. Neuroradiology 1982;23:153-156.
- Detection of Xanthochromia in Cerebrospinal Fluid. Ainsley H. Chalmers, Michelle Kiley. Clinical Chemistry Aug 1998, 44 (8) 1740-1742; http://clinchem.aaccjnls.org/content/44/8/1740
- Chu KH, Bishop RO, Brown AF. Spectrophotometry, not visual inspection for the detection of xanthochromia in suspected subarachnoid haemorrhage: A debate. Emerg Med Australas. 2015 Jun;27(3):267-72.
- Dupont SA, Wijdicks EF, Manno EM, Rabinstein AA. Thunderclap headache and normal computed tomographic results: value of cerebrospinal fluid analysis. Mayo Clin. Proc. 2008 Dec;83(12):1326-31.
- Vermeulen M, Hasan D, Blijenberg BG, Hijdra A, van Gijn J. Xanthochromia after subarachnoid haemorrhage needs no revisitation. J. Neurol. Neurosurg. Psychiatry. 1989 Jul;52(7):826-8.
- Petzold A, Keir G, Sharpe TL. Why human color vision cannot reliably detect cerebrospinal fluid xanthochromia. Stroke. 2005 Jun;36(6):1295-7.
- Mark DG, Kene MV, Offerman SR, Vinson DR, Ballard DW., Kaiser Permanente CREST Network. Validation of cerebrospinal fluid findings in aneurysmal subarachnoid hemorrhage. Am J Emerg Med. 2015 Sep;33(9):1249-52.
- Ichiba T, Hara M, Nishikawa K, Tanabe T, Urashima M, Naitou H. Comprehensive Evaluation of Diagnostic and Treatment Strategies for Idiopathic Spinal Subarachnoid Hemorrhage. J Stroke Cerebrovasc Dis. 2017 Dec;26(12):2840-2848.
- Martin SC, Teo MK, Young AM, Godber IM, Mandalia SS, St George EJ, McGregor C. Defending a traditional practice in the modern era: The use of lumbar puncture in the investigation of subarachnoid haemorrhage. Br J Neurosurg. 2015;29(6):799-803.